ATI Maternity Exam
Total Questions : 44
Showing 25 questions, Sign in for moreA nurse is collecting data from a client who is postpartum. Which of the following findings should alert the nurse to the possibility of a postpartum complication?
Explanation
Choice A reason:
A urinary output of 2,000 mL/12 hr is normal for a postpartum client, as the body eliminates excess fluid accumulated during pregnancy.
Choice B reason:
A temperature of 100.4 F for two days indicates a possible infection, such as endometritis or mastitis, and requires further evaluation and treatment.
Choice C reason:
Chills shortly following delivery are common and benign and are caused by hormonal changes and fluid shifts.
Choice D reason:
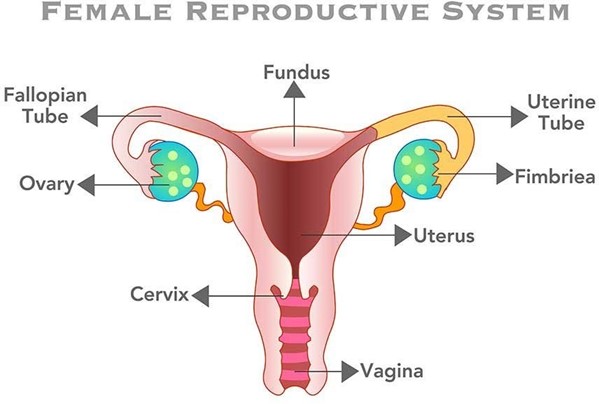
A fundus at the umbilicus level is expected for a postpartum client and indicates that the uterus is involuting properly.
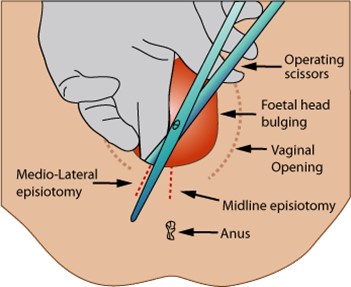
A nurse is caring for a client who has unrelieved episiotomy pain 8 hr following delivery. Which of the following actions should the nurse take?
Explanation
Choice A reason:
A warm sitz bath can promote healing and comfort, but it is not recommended until 24 hr after delivery, as it can increase swelling and bleeding.
Choice B reason:
An ice pack can reduce inflammation and pain by causing vasoconstriction and numbing the area. It should be applied for 20 minutes at a time, with a cloth barrier between the skin and the ice.
Choice C reason:
A soft pillow under the client's butocks can increase pressure on the perineum and worsen the pain. The client should be encouraged to lie on her side or sit in a semi-Fowler's position.
Choice D reason:
A heating lamp can dry out the wound and delay healing. It can also cause burns and discomfort. It should be avoided for episiotomy care.
A nurse is assisting with the care of a client who is multigravid and in active labor with 7 cm of cervical dilation and 100% effacement. The fetus is at +1 station, and the client's amniotic membranes are intact. The client suddenly states that she needs to push. Which of the following is the appropriate nursing response?
Explanation
Choice A reason:
Panting can help prevent premature pushing and reduce the risk of cervical edema or laceration. The client should be instructed to take short, shallow breaths through her mouth during contractions until she reaches 10 cm of dilation.
Choice B reason:
Assessing the perineum for signs of crowning is not a priority at this stage, as the fetus is not yet at a low enough station to be visible. Crowning usually occurs when the fetus is at +4 or +5 station.
Choice C reason:
Assisting the client into a comfortable position is important, but it does not address the urge to push. The client should be encouraged to change positions frequently to promote fetal descent and comfort.
Choice D reason:
Helping the client to the bathroom to empty her bladder is not advisable, as it can increase the risk of cord prolapse or rupture of membranes. The client should have an indwelling catheter inserted if she is unable to void spontaneously.
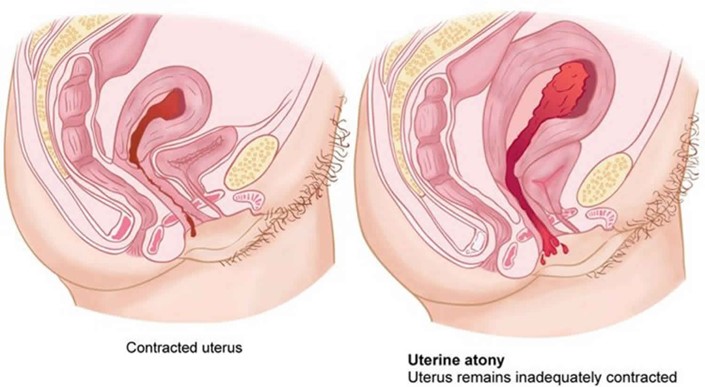
A nurse is caring for a client 2 hr following a spontaneous vaginal delivery and notes that the client has saturated two perineal pads with blood in a 30-min period. Which of the following actions should the nurse take first?
Explanation
Choice A reason:
Checking the consistency of the client's uterine fundus is the first action the nurse should take, as it can indicate the cause of excessive bleeding. A boggy or soft fundus indicates uterine atony, which is the most common cause of postpartum hemorrhage. The nurse should massage the fundus until it becomes firm and contracted.
Choice B reason:
Having the client use the bedpan to urinate is an important action, as a full bladder can displace the uterus and prevent it from contracting properly. However, this is not the first action the nurse should take, as it does not address the immediate source of bleeding.
Choice C reason:
Increasing the client's fluid intake is an important action, as it can help replace fluid loss and prevent hypovolemia and shock. However, this is not the first action the nurse should take, as it does not stop the bleeding.
Choice D reason:
Preparing to administer oxytocic medication is an important action, as it can stimulate uterine contractions and reduce bleeding. However, this is not the first action the nurse should take, as it requires a provider's prescription and may not be necessary if fundal massage is effective.
A nurse is caring for a client who is 12 hr postpartum. The nurse recognizes the client is in the dependent, taking-in phase of maternal postpartum adjustment. Which of the following is an expected finding during this period?
Explanation
Expressions of excitement are typical during the dependent, taking-in phase, which lasts for the first 24 to 48 hr after delivery. The client may relive and review her labor and delivery experience, and may need reassurance and validation from others.
Choice B reason:
Lack of appetite is not an expected finding during the dependent, taking-in phase, as the client may have increased hunger and thirst after delivery. The nurse should encourage adequate nutrition and hydration to promote healing and lactation.
Choice C reason:
Eagerness to learn newborn care skills is more characteristic of the dependent-independent, taking-hold phase, which begins around the third day postpartum. During this phase, the client becomes more confident and interested in caring for herself and her newborn.
ChoiceD reason:
Focus on the family unit and its members is more characteristic of the interdependent, letting-go phase, which occurs after the first week postpartum. During this phase, the client redefines her role within the family and society, and integrates the newborn into her life.
A nurse is caring for a client following a cesarean birth. The client tells the nurse that she is hungry. Which of the following actions should the nurse take first?
Explanation
Choice B reason:
Auscultating the client's abdomen is the first action the nurse should take, as it can assess the return of bowel function after surgery. The nurse should listen for bowel sounds in all four quadrants, and note their frequency and quality.
Offering clear liquids is an important action, as it can provide hydration and nutrition for the client. However, this is not the first action the nurse should take, as it may cause nausea and vomiting if the client's bowel function has not returned.
Choice C reason:
Checking the client's chart for a diet prescription is an important action, as it can ensure that the client follows the provider's orders and does not consume anything contraindicated. However, this is not the first action the nurse should take, as it does not address the client's hunger or bowel function.
Choice D reason:
Giving the client soda crackers is an important action, as it can provide a bland and easily digestible food for the client. However, this is not the first action the nurse should take, as it may be too solid for the client's stomach if her bowel function has not returned.
A nurse is assessing a client who is 8 hr postpartum and multiparous. Which of the following findings should alert the nurse to the client's need to urinate?
Explanation
Choice B reason:
A fundus that is elevated and displaced from the midline indicates a full bladder, which can interfere with uterine contraction and increase the risk of hemorrhage. The nurse should assist the client to void or catheterize her if necessary.
Choice A reason:
Moderate swelling of the labia is a normal finding after vaginal delivery, and does not indicate a need to urinate. The nurse should apply ice packs and perineal pads to reduce edema and discomfort.
Choice C reason:
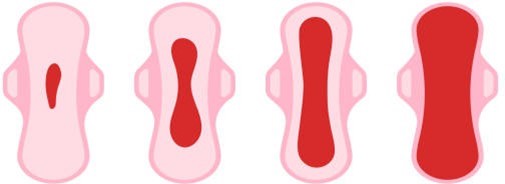
Moderate lochia rubra is a normal finding during the first 24 hr postpartum, and does not indicate a need to urinate. The nurse should monitor the amount and color of lochia, and change the perineal pads as needed.
Choice D reason:
A blood pressure of 130/84 mm Hg is within the normal range for a postpartum client, and does not indicate a need to urinate. The nurse should monitor the blood pressure for signs of hypertension or hypotension, which can indicate complications such as preeclampsia or hemorrhage.
A nurse is caring for a postpartum client following a vaginal birth of a newborn weighing 4252 g (9 lb 6 oz). The nurse should identify that this client is at risk for which of the following postpartum complications?
Explanation
Choice B reason:
Uterine atony is the failure of the uterus to contract and retract after delivery, which can lead to excessive bleeding and hemorrhage. The client is at risk for uterine atony due to delivering a large newborn, which can overstretch the uterine muscles and reduce their tone.
Choice A reason:
Puerperal infection is an infection of the reproductive tract that occurs within six weeks after delivery. The client is not at increased risk for puerperal infection due to delivering a large newborn, unless there are other factors such as prolonged labor, multiple vaginal exams, or episiotomy.
Choice C reason:
Thrombophlebitis is an inflammation of a vein with a blood clot formation. The client is not at increased risk for thrombophlebitis due to delivering a large newborn, unless there are other factors such as immobility, dehydration, or trauma.
Choice D reason:
Retained placental fragments are pieces of the placenta that remain in the uterus after delivery, which can cause bleeding and infection. The client is not at increased risk for retained placental fragments due to delivering a large newborn, unless there are other factors such as abnormal placental atachment, manual removal, or incomplete separation.
A nurse is assisting with the care of a client who had an epidural anesthesia block during the early stages of labor. The client's blood pressure is 80/40 mm Hg and the fetal heart recording is 140/min. Which of the following actions should the nurse take first?
Explanation
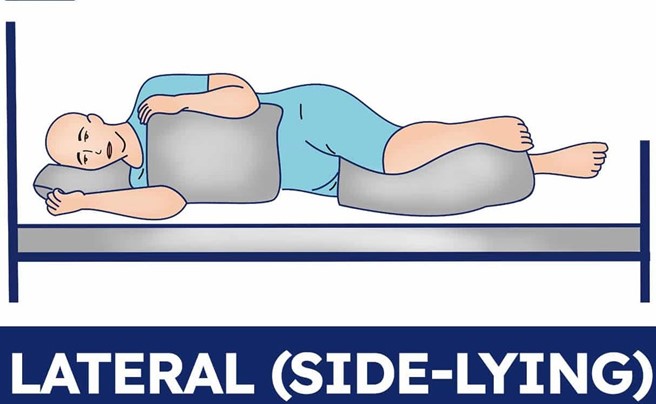
Choice A reason:
Placing the client in a lateral position is the first action the nurse should take, as it can improve maternal and fetal circulation by relieving pressure on the inferior vena cava. The client's blood pressure is low, which can indicate hypotension due to epidural anesthesia or supine hypotension syndrome.
Choice B reason:
Notifying the provider is an important action, as it can facilitate further interventions and monitoring for the client and the fetus. However, this is not the first action the nurse should take, as it does not address the immediate problem of hypotension.
Choice C reason:
Increasing IV fluid rate is an important action, as it can expand blood volume and increase blood pressure. However, this is not the first action the nurse should take, as it may not be effective if the client is in a supine position.
Choice D reason:
Elevating the legs is an important action, as it can enhance venous return and increase blood pressure. However, this is not the first action the nurse should take, as it may worsen supine hypotension syndrome by increasing pressure on the inferior vena cava.
A nurse is assisting with the care of a client who is in the first stage of labor. The nurse observes the umbilical cord protruding from the vagina. Which of the following actions should the nurse take first?
Explanation
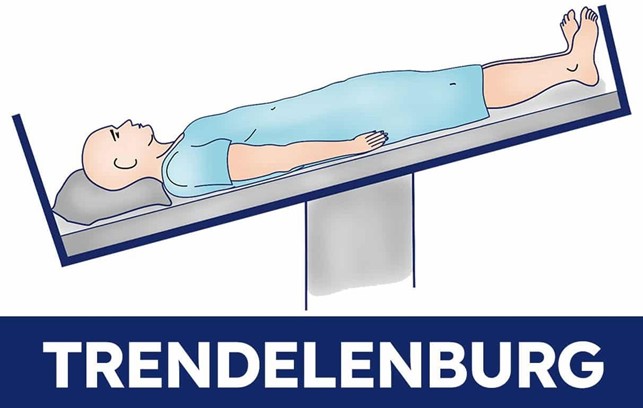
Choice D reason:
Placing the client in a knee-chest or Trendelenburg position is the first action the nurse should take, as it can relieve pressure on the cord and prevent compression and fetal hypoxia. The nurse should also use a sterile gloved hand to hold the presenting part off the cord.
Choice A reason:
Preparing the client for an emergency cesarean birth is an important action, as it can facilitate prompt delivery and prevent fetal compromise. However, this is not the first action the nurse should take, as it does not address the immediate problem of cord prolapse.
Choice B reason:
Covering the cord with a sterile, moist saline dressing is an important action, as it can prevent drying and infection of the cord. However, this is not the first action the nurse should take, as it does not address the immediate problem of cord compression.
Choice C reason:
Explaining to the client what is happening is an important action, as it can provide emotional support and education for the client. However, this is not the first action the nurse should take, as it does not address the immediate problem of cord prolapse.
A nurse is caring for a group of clients on an intrapartum unit. Which of the following findings should be reported to the RN immediately?
Explanation
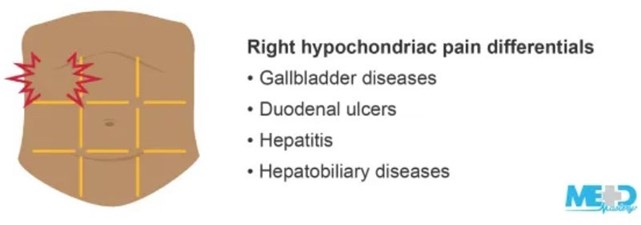
Choice D reason: A client who has preeclampsia and reports epigastric pain and unresolved headache should be reported to the RN immediately, as these are signs of severe preeclampsia and impending eclampsia, which can lead to seizures, coma, and death. The client may need anticonvulsant medication, magnesium sulfate infusion, and delivery of the fetus.
Choice A reason: A client who is at 32 weeks of gestation and is experiencing irregular, frequent contractions is tearful may have preterm labor, which should be monitored and treated accordingly. However, this is not as urgent as choice D, as the contractions may subside with hydration, rest, or tocolytic medication.
Choice B reason: A client who has preeclampsia has 2+ patellar reflexes and 2+ proteinuria may have mild preeclampsia, which should be managed with antihypertensive medication, bed rest, and fetal monitoring. However, this is not as urgent as choice D, as the reflexes and proteinuria are not indicative of severe preeclampsia or eclampsia.
Choice C reason: A client who is at 28 weeks of gestation and receiving terbutaline reports fine tremors may have a common side effect of terbutaline, which is a beta-adrenergic agonist that relaxes uterine smooth muscle and inhibits contractions. However, this is not as urgent as choice D, as the tremors are usually transient and benign. The nurse should monitor the client's vital signs, blood glucose, and fetal heart rate.
A nurse is collecting data from a postpartum client and finds a large amount of lochia rubra with several clots on the client's perineal pad. Which of the following actions should the nurse take first?
Explanation
Choice A reason:
Feeling for a full bladder is not the first action the nurse should take, although it is important to assess for bladder distension and urinary retention in postpartum clients. A full bladder can displace the uterus and increase the risk of uterine atony and hemorrhage.
Choice B reason:
Checking the client's fundus is the first action the nurse should take, as it can indicate the tone and position of the uterus. A firm and midline fundus indicates adequate uterine contraction and prevents excessive bleeding. A boggy or deviated fundus indicates uterine atony or retained placental fragments, which can cause hemorrhage.
Choice C reason:
Measuring the client's vital signs is not the first action the nurse should take, although it is important to monitor for signs of shock and infection in postpartum clients. Vital signs can be affected by various factors and do not provide a direct assessment of uterine status.
Choice D reason:
Requesting the provider perform a vaginal examination is not the first action the nurse should take, as it can introduce infection and trauma to the perineum. A vaginal examination is only indicated if there is suspicion of cervical or vaginal lacerations or retained placenta.
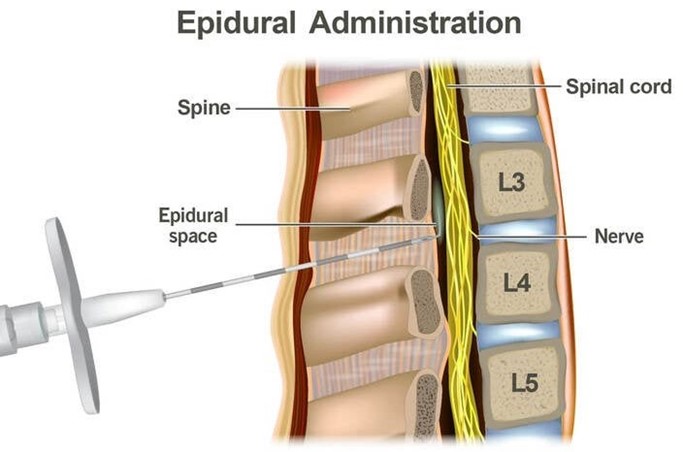
A nurse is reinforcing teaching with a client who is in labor about why epidural anesthesia is not initiated until a good labor patern has been established. Which of the following explanations should the nurse include?
Explanation
Choice A reason:
Given too soon, epidural anesthesia can cause fetal depression is incorrect, as epidural anesthesia does not cross the placenta and does not affect the fetal status.
Choice B reason:
Given too soon, epidural anesthesia will delay rupture of fetal membranes is incorrect, as epidural anesthesia does not interfere with the rupture of membranes. The rupture of membranes depends on the cervical dilation and effacement, the position of the presenting part, and the strength of contractions.
Choice C reason:
Given too soon, epidural anesthesia can cause maternal hypertension is incorrect, as epidural anesthesia can cause maternal hypotension due to vasodilation and decreased venous return. The nurse should monitor the client's blood pressure and administer fluids and vasopressors as needed.
Choice D reason:
Given too soon, epidural anesthesia can prolong labor is correct, as epidural anesthesia can decrease the strength and frequency of contractions and reduce the urge to push. The nurse should ensure that the client has a good labor patern before administering epidural anesthesia and monitor the progress of labor afterwards.
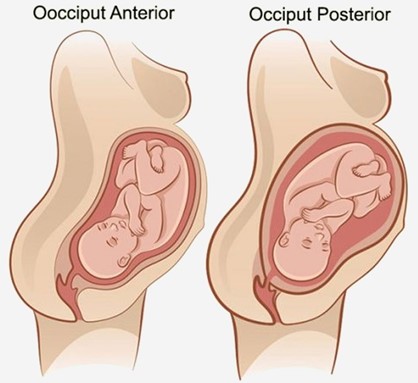
A nurse is assisting with the care of a client who is in labor. The client's labor is difficult and prolonged and she reports a severe backache. Which of the following factors is a contributing cause of difficult, prolonged labor?
Explanation
Choice A reason:
Fetal position is persistent occiput posterior is correct, as this position can cause difficult, prolonged labor and severe backache. The occiput posterior position means that the back of the fetal head is facing the maternal sacrum, which can result in poor alignment and descent, increased pressure on the maternal sacrum and nerves, and increased risk of perineal trauma. The nurse should encourage the client to change positions frequently, use pelvic rocking exercises, apply counterpressure to the sacrum, and administer analgesics as needed.
Choice B reason:
Fetal attitude is in general flexion is incorrect, as this attitude can facilitate normal labor and delivery. The fetal attitude refers to the degree of flexion or extension of the fetal head and limbs in relation to the fetal trunk. General flexion means that the fetal head is flexed on the chest, the arms are crossed over the chest, and the legs are flexed at the knees. This attitude allows the smallest diameter of the fetal head to pass through the birth canal.
Choice C reason:
Fetal lie is longitudinal is incorrect, as this lie can facilitate normal labor and delivery. The fetal lie refers to the relationship between the long axis of the fetus and the long axis of the mother. Longitudinal lie means that both axes are parallel, which allows for either a vertex (head-first) or a breech (butocks-first) presentation.
Choice D reason:
Maternal pelvis is gynecoid is incorrect, as this pelvis can facilitate normal labor and delivery. The maternal pelvis refers to the shape and size of the bony pelvis that affects the passage of the fetus. Gynecoid pelvis is the most common and favorable type for vaginal birth, as it has a rounded inlet, a wide pubic arch, and adequate outlet dimensions.
A nurse is assisting in the care of a client who is in the second stage of labor. Which of the following findings should the nurse report to the provider?
Explanation
Choice A reason:
Bloody show from the vagina is incorrect, as this finding is normal and expected in the second stage of labor. Bloody show refers to the passage of mucus and blood from the cervix, which indicates cervical dilation and effacement.
Choice B reason:
Early decelerations in the FHR is incorrect, as this finding is normal and benign in the second stage of labor. Early decelerations are symmetrical decreases in the FHR that mirror the contractions, which indicate fetal head compression and vagal stimulation. The nurse should continue to monitor the FHR and document the findings.
Choice C reason:
Pelvic pressure with contractions is incorrect, as this finding is normal and expected in the second stage of labor. Pelvic pressure indicates that the fetus is descending into the birth canal and that the client is ready to push.
Choice D reason:
Uterine contraction lasting 2 min is correct, as this finding is abnormal and potentially dangerous in any stage of labor. Uterine contraction lasting 2 min can indicate uterine tetany or hyperstimulation, which can cause fetal distress, placental abruption, uterine rupture, or maternal hemorrhage. The nurse should report this finding to the provider immediately and prepare to intervene as ordered.

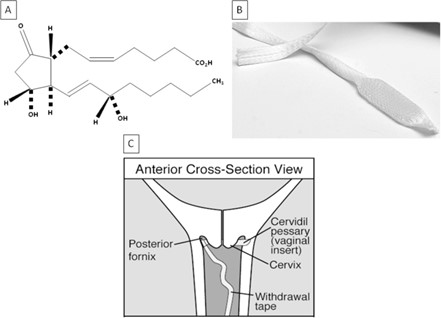
A nurse is preparing to administer dinoprostone gel to a client who is pregnant. The client asks the nurse about the purpose of the medication. Which of the following responses should the nurse make?
Explanation
Choice A reason:
Dinoprostone stimulates uterine contractions is incorrect, as this is not the primary purpose of the medication. Dinoprostone is a prostaglandin that can induce labor by ripening the cervix and enhancing uterine contractility, but it is not used solely for stimulating contractions.
Choice B reason:
Dinoprostone promotes softening of the cervix is correct, as this is the main purpose of the medication. Dinoprostone is used to prepare the cervix for labor by increasing its softness, dilation, and effacement. This can facilitate the descent of the fetus and shorten the duration of labor.
Choice C reason:
Dinoprostone relaxes uterine contractions is incorrect, as this is the opposite effect of the medication. Dinoprostone can increase uterine tone and frequency, which can help initiate or augment labor. The nurse should monitor the client for signs of uterine hyperstimulation or fetal distress.
Choice D reason:
Dinoprostone assists with ending the pregnancy is incorrect, as this is not the intended use of the medication. Dinoprostone can be used to terminate a pregnancy in some cases, such as fetal demise or missed abortion, but it is not routinely used for this purpose. The nurse should explain to the client that dinoprostone is used to induce labor and not to end a pregnancy.
A nurse is assisting with the monitoring of a client who is in the first stage of labor, with an external fetal monitor in place and IV fluids infusing. Which of the following factors will cause variable decelerations in the fetal heart rate?
Explanation
Choice A reason:
Maternal opioid administration is incorrect, as this factor can cause late decelerations in the fetal heart rate. Late decelerations are symmetrical decreases in the FHR that begin after the peak of the contraction and return to baseline after the contraction ends, which indicate uteroplacental insufficiency. Maternal opioid administration can reduce maternal blood pressure and placental perfusion, leading to fetal hypoxia.
Choice B reason:
Fetal head compression is incorrect, as this factor can cause early decelerations in the fetal heart rate. Early decelerations are symmetrical decreases in the FHR that mirror the contractions, which indicate fetal head compression and vagal stimulation. Fetal head compression occurs as the fetus descends into the birth canal and does not pose a threat to the fetal well-being.
Choice C reason:
Uteroplacental insufficiency is incorrect, as this factor can cause late decelerations in the fetal heart rate. Uteroplacental insufficiency refers to a reduced blood flow and oxygen delivery to the fetus through the placenta, which can result from maternal hypotension, uterine hyperstimulation, placental abruption, or other conditions. Uteroplacental insufficiency can cause fetal hypoxia and acidosis.
Choice D reason:
Umbilical cord compression is correct, as this factor can cause variable decelerations in the fetal heart rate. Variable decelerations are abrupt decreases in the FHR that vary in onset, duration, and depth, which indicate umbilical cord compression and reduced blood flow to the fetus. Umbilical cord compression can occur due to cord prolapse, nuchal cord, short cord, or other causes. The nurse should reposition the client, administer oxygen, and prepare for delivery if indicated.
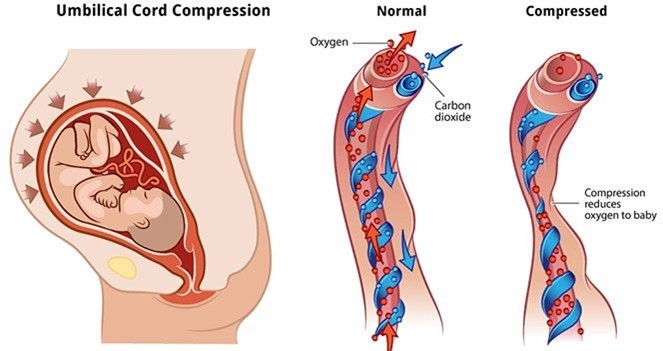
A nurse is assisting in the care of a client who is in active labor. The nurse notes variable decelerations of the FHR. The nurse should identify which of the following as a cause of variable decelerations?
Explanation
Choice A reason:
Fetal head compression is incorrect, as this factor can cause early decelerations in the fetal heart rate. Early decelerations are symmetrical decreases in the FHR that mirror the contractions, which indicate fetal head compression and vagal stimulation. Fetal head compression occurs as the fetus descends into the birth canal and does not pose a threat to the fetal well-being.
Choice B reason:
Polyhydramnios is incorrect, as this factor can cause variable or late decelerations in the fetal heart rate, depending on the underlying cause. Polyhydramnios refers to an excessive amount of amniotic fluid, which can result from fetal anomalies, maternal diabetes, multiple gestation, or other conditions. Polyhydramnios can cause umbilical cord prolapse, uterine overdistension, or placental abruption, leading to reduced blood flow and oxygen delivery to the fetus.
Choice C reason:
Maternal fever is incorrect, as this factor can cause late decelerations in the fetal heart rate. Late decelerations are symmetrical decreases in the FHR that begin after the peak of the contraction and return to baseline after the contraction ends, which indicate uteroplacental insufficiency. Maternal fever can increase maternal and fetal metabolism and oxygen demand, leading to fetal hypoxia and acidosis.
Choice D reason:
Umbilical cord compression is correct, as this factor can cause variable decelerations in the fetal heart rate. Variable decelerations are abrupt decreases in the FHR that vary in onset, duration, and depth, which indicate umbilical cord compression and reduced blood flow to the fetus. Umbilical cord compression can occur due to cord prolapse, nuchal cord, short cord, or other causes. The nurse should reposition the client, administer oxygen, and prepare for delivery if indicated.
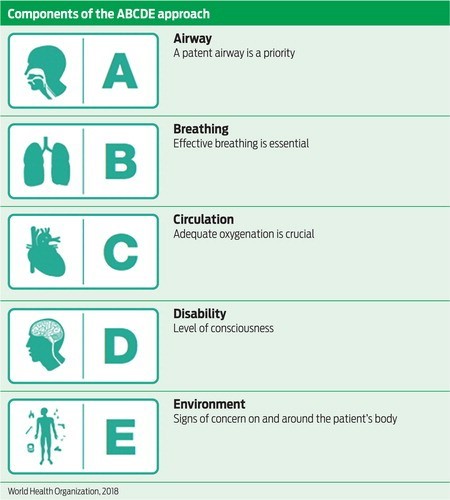
A nurse is caring for a postpartum client who saturates a perineal pad in 10 min. Which of the following actions should the nurse take first?
Explanation
Choice A reason: Massage the client's fundus is correct, as this is the first action the nurse should take according to the ABCDE priority framework. Saturating a perineal pad in 10 min indicates excessive bleeding and possible postpartum hemorrhage, which can compromise the client's airway, breathing, and circulation. Massaging the fundus can stimulate uterine contraction and reduce blood loss.
Choice B reason: Check the client's blood pressure is incorrect, as this is not the first action the nurse should take, although it is important to monitor for signs of shock. Checking the blood pressure does not address the cause of bleeding or prevent further blood loss.
Choice C reason: Administer oxytocin is incorrect, as this is not the first action the nurse should take, although it may be indicated later. Administering oxytocin requires a provider's order and may have adverse effects such as nausea,
vomiting, headache, or water intoxication. The nurse should first atempt to control bleeding by massaging the fundus and then administer oxytocin as ordered.
Choice D reason: Observe for pooling of blood under the butocks is incorrect, as this is not the first action the nurse should take, although it can help estimate blood loss. Observing for pooling of blood does not address the cause of bleeding or prevent further blood loss. The nurse should first atempt to control bleeding by massaging the fundus and then assess for other signs of hemorrhage.
A nurse is assisting in the care of a client who is in labor. The doctor documents the vaginal examination as: 3 cm, 30%, and -1. The nurse evaluates this documentation to mean which of the following?
Explanation
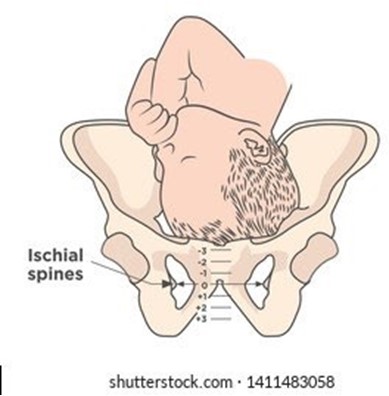
Choice A reason: The cervix is effaced 3 cm, it is dilated 30%, and the presenting part is 1 cm above the ischial spines is incorrect, as this does not follow the correct order and measurement of cervical assessment. Cervical effacement is measured in percentage, not in centimeters, and it indicates the thinning or shortening of the cervix. Cervical dilation is measured in centimeters, not in percentage, and it indicates the opening or widening of the cervix.
Choice B reason: The cervix is dilated 3 cm, it is effaced 30%, and the presenting part is 1 cm above the ischial spines is correct, as this follows the correct order and measurement of cervical assessment. Cervical dilation, effacement, and station are recorded in that order to describe the progress of labor. Station refers to the relationship between the presenting part of the fetus and the maternal pelvis, measured by the level of the ischial spines. A negative station means that the presenting part is above the spines, while a positive station means that it is below.
Choice C reason: The cervix is effaced 3 cm, it is dilated 30%, and the presenting part is 1 cm below the ischial spines is incorrect, as this does not follow the correct order and measurement of cervical assessment. Cervical effacement is measured in percentage, not in centimeters, and it indicates the thinning or shortening of the cervix. Cervical dilation is measured in centimeters, not in percentage, and it indicates the opening or widening of the cervix.
Choice D reason: The cervix is dilated 3 cm, it is effaced 30%, and the presenting part is 1 cm below the ischial spines is incorrect, as this does not match the documentation of station. A negative station means that the presenting part is above the spines, while a positive station means that it is below.
A nurse is caring for a client who is 4 hr postpartum. The nurse finds a small amount of lochia rubra on the client's perineal pad. The fundus is midline and firm at the umbilicus. Which of the following actions should the nurse take?
Explanation
Choice A reason: Perform fundal massage is incorrect, as this action is not indicated for a client who has a firm and midline fundus. Fundal massage is used to stimulate uterine contraction and prevent hemorrhage in clients who have a boggy or deviated fundus.
Choice B reason: Assist the client to ambulate is correct, as this action can promote lochia drainage and prevent pooling of blood in the vagina. The nurse should encourage the client to ambulate early and frequently after birth, as long as there are no contraindications. The nurse should also monitor the client for signs of orthostatic hypotension and provide assistance as needed.
Choice C reason: Check for blood under the client's butock is incorrect, as this action is not necessary for a client who has a small amount of lochia rubra on the perineal pad. Lochia rubra is normal and expected in the first few days after birth, and it indicates that the placental site is healing. The nurse should check for blood under the butock only if there is suspicion of excessive bleeding or concealed hemorrhage.
Choice D reason: Increase the rate of the IV fluids is incorrect, as this action is not indicated for a client who has a small amount of lochia rubra on the perineal pad. Increasing the rate of IV fluids can cause fluid overload and electrolyte imbalance in the client. The nurse should maintain the IV fluids at the prescribed rate and monitor the client's intake and output.
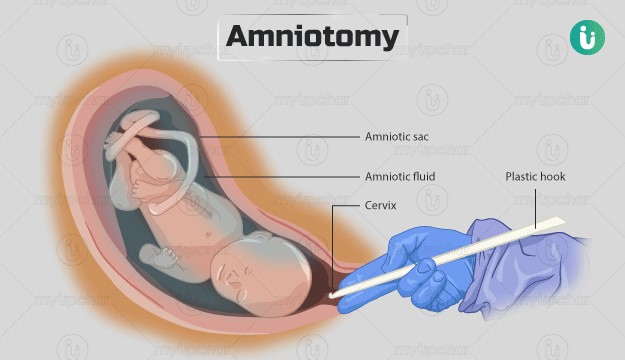
A nurse is assisting in the care of a client following an amniotomy who is now in the active phase of the first stage of labor. Which of the following actions should the nurse take?
Explanation
Choice A reason: Check the client's temperature every 4 hr is incorrect, as this action is not frequent enough for a client who had an amniotomy. The nurse should check the client's temperature every 2 hr after an amniotomy, as there is an increased risk of infection due to the rupture of membranes. The nurse should also monitor for signs of chorioamnionitis, such as foul-smelling amniotic fluid, maternal tachycardia, or fetal tachycardia.
Choice B reason: Remind the client to bear down with each contraction is incorrect, as this action is not appropriate for a client who is in the active phase of the first stage of labor. The nurse should instruct the client to avoid bearing down or pushing until they are in the second stage of labor, when the cervix is fully dilated and effaced. Bearing down too early can cause cervical edema, lacerations, or exhaustion.
Choice C reason: Maintain the client in the lithotomy position is incorrect, as this action is not optimal for a client who is in the active phase of the first stage of labor. The lithotomy position is a supine position with the legs elevated and abducted, which can reduce blood flow to the uterus and placenta, increase perineal edema, and limit pelvic outlet diameter. The nurse should encourage the client to change positions frequently and use upright or lateral positions that can enhance uterine contractility, fetal descent, and maternal comfort.
Choice D reason: Encourage the client to empty the bladder every 2 hr is correct, as this action can promote labor progress and prevent bladder distension and infection. The nurse should assist the client to void every 2 hr after an amniotomy, as there may be decreased sensation of bladder fullness due to pressure from the fetal head. A full bladder can interfere with uterine contractions, fetal descent, and cervical dilation.
A nurse is collecting data from a client who is 12 hr postpartum following a spontaneous vaginal delivery. The nurse should expect to find the uterine fundus at which of the following positions on the client's abdomen?
Explanation
Choice A reason: Three fingerbreadths above the umbilicus is incorrect, as this position indicates a higher than expected fundal height for a client who is 12 hr postpartum. The fundus is normally at the level of the umbilicus immediately after birth and then descends about one fingerbreadth per day. A high fundal height can indicate uterine atony, retained placental fragments, or bladder distension.
Choice B reason: One fingerbreadth above the symphysis pubis is incorrect, as this position indicates a lower than expected fundal height for a client who is 12 hr postpartum. The fundus is normally at the level of the umbilicus immediately after birth and then descends about one finger-breadth per day. A low fundal height can indicate uterine inversion, which is a rare but life-threatening complication.
Choice C reason: At the level of the umbilicus is correct, as this position indicates a normal and expected fundal height for a client who is 12 hr postpartum. The fundus is normally at the level of the umbilicus immediately after birth and then descends about one finger-breadth per day. A midline and firm fundus indicates adequate uterine contraction and involution.
Choice D reason: To the right of the umbilicus is incorrect, as this position indicates a deviated fundus for a client who is 12 hr postpartum. The fundus should be midline and not displaced to either side. A deviated fundus can indicate bladder distension, which can interfere with uterine contraction and involution. The nurse should assist the client to empty their bladder and reassess the fundal position.

A nurse is assisting a client who is postpartum with her first breastfeeding experience. When the client asks how much of the nipple she should put into the baby's mouth, which of the following responses by the nurse is appropriate?
Explanation
Choice A reason: "Babies know instinctively exactly how much of the nipple to take into their mouth." is incorrect, as this response does not provide adequate guidance or support for the client. Babies may not always latch on correctly or effectively, especially in the first few atempts. The nurse should teach the client how to position and latch the baby properly and observe for signs of effective breastfeeding.
Choice B reason: "Your baby's mouth is rather small so she will only take part of the nipple." is incorrect, as this response can lead to ineffective breastfeeding and nipple trauma. Taking only part of the nipple can cause poor milk transfer, inadequate milk production, and nipple soreness or cracking. The nurse should teach the client how to ensure that the baby takes enough of the nipple and areola into their mouth.
Choice C reason: "Try to place the nipple, the entire areola, and some breast tissue beyond the areola into her mouth." is correct, as this response provides accurate and helpful information for the client. Placing the nipple, the entire areola, and some breast tissue beyond the areola into the baby's mouth can facilitate optimal milk transfer, stimulate milk production, and prevent nipple injury. The nurse should demonstrate and assist the client with this technique and provide positive feedback.
Choice D reason: "You should place your nipple and some of the areola into her mouth." is incorrect, as this response does not provide enough detail or specificity for the client. Placing only some of the areola into the baby's mouth may not be sufficient for effective breastfeeding and may cause nipple damage. The nurse should teach the client how to ensure that the baby takes enough of the nipple and areola into their mouth.
A nurse is assisting with the admission of a client who is at 39 weeks of gestation and has a history of genital herpes. Which of the following actions should the nurse take?
Explanation
Choice A reason: Request the RN perform a cervical examination is incorrect, as this action is not indicated for a client who has a history of genital herpes. A cervical examination can introduce infection and trauma to the cervix and increase the risk of viral shedding and transmission to the fetus. The nurse should avoid performing or requesting a cervical examination unless absolutely necessary.
Choice B reason: Initiate fetal monitoring for baseline and changes is correct, as this action is appropriate for any client who is in labor. Fetal monitoring can provide information about the fetal heart rate, variability, accelerations, decelerations, and contractions. The nurse should monitor the fetal status continuously and report any abnormal findings to the provider.
Choice C reason: Prepare for a vaginal birth is incorrect, as this action may not be possible for a client who has a history of genital herpes. A vaginal birth can expose the fetus to the herpes virus and cause neonatal infection, which can be life-threatening. The nurse should assess the client for signs of active lesions or prodromal symptoms and prepare for a cesarean birth if indicated.
Choice D reason: Administer antibiotics is incorrect, as this action is not effective for a client who has a history of genital herpes. Genital herpes is caused by a virus, not a bacteria, and antibiotics have no effect on viral infections. The nurse should administer antiviral medications as prescribed to reduce viral shedding and transmission to the fetus.
Sign Up or Login to view all the 44 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

