ATI Maternity Exam 2
Total Questions : 45
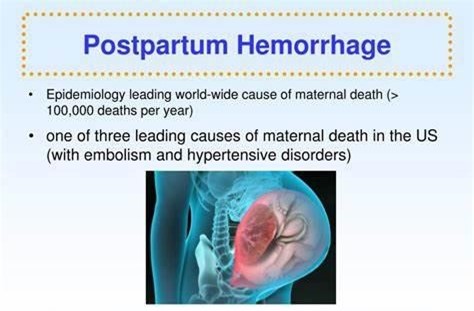
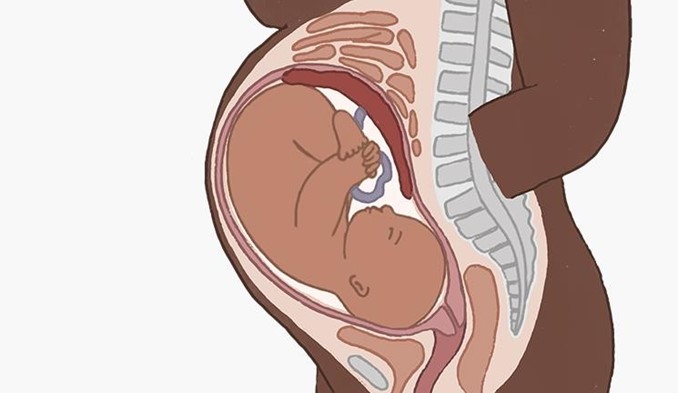
Showing 25 questions, Sign in for moreAdllent, 1 day postpartum, is being monitored after a postpartum hemorrhage. Which of the following should the nurse report to the obstetrician?
Explanation
Choice a) Urine output of 200 mL for the past 8 hours is incorrect because this is a normal finding for a postpartum woman. The average urine output for a healthy adult is about 800 to 2000 mL per day, which means about 100 to 250 mL per hour. Therefore, a urine output of 200 mL for the past 8 hours is within the normal range and does not indicate any complications.
Choice b) Weight decrease of 2 pounds since delivery is incorrect because this is also a normal finding for a postpartum woman. The weight loss is due to the expulsion of the placenta, amniotic fluid, and blood during delivery. A postpartum woman can expect to lose about 10 to 12 pounds immediately after giving birth, and another 5 pounds in the following weeks due to fluid loss. Therefore, a weight decrease of 2 pounds since delivery is not a cause for concern and does not need to be reported to the obstetrician.
Choice c) Pulse rate of 65 beats per minute is incorrect because this is also a normal finding for a postpartum woman. The normal resting pulse rate for an adult ranges from 60 to 100 beats per minute, and it may decrease slightly after delivery due to blood loss and reduced cardiac output. Therefore, a pulse rate of 65 beats per minute is not indicative of any problems and does not require any intervention.
Choice d) Drop in hematocrit of 6% since admission is correct because this is an abnormal finding for a postpartum woman and suggests that she has developed anemia due to excessive blood loss. Hematocrit is the percentage of red blood cells in the blood, and it reflects the oxygen-carrying capacity of the blood. The normal hematocrit range for an adult female is 37% to 47%, and it may decrease slightly after delivery due to hemodilution. However, a drop in hematocrit of more than 10% from the baseline or below 30% indicates severe anemia and requires immediate treatment. Therefore, a drop in hematocrit of 6% since admission is a significant change that should be reported to the obstetrician as soon as possible.
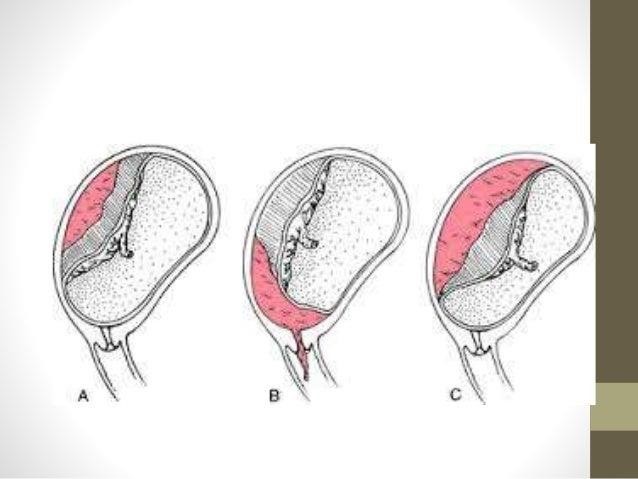
A woman who is 8 months pregnant is brought to the emergency department after a serious motor vehicle crash. Although she has no apparent injuries, she is admitted to the hospital for observation for which complication?
Explanation
Choice a) Placenta previa is incorrect because this is a condition where the placenta partially or completely covers the cervix, which can cause painless vaginal bleeding in the third trimester. It is not related to trauma and does not require hospitalization unless bleeding occurs.
Choice b) Dehydration is incorrect because this is a condition where the body loses more fluid than it takes in, which can cause symptoms such as thirst, dry mouth, headache, fatigue, and dizziness. It is not a complication of pregnancy and can be prevented by drinking enough water and avoiding caffeine and alcohol.
Choice c) Gestational hypertension is incorrect because this is a condition where the blood pressure rises above 140/90 mmHg after 20 weeks of pregnancy, which can cause complications such as preeclampsia, eclampsia, and fetal growth restriction. It is not caused by trauma and can be managed by regular antenatal care and medication if needed.
Choice d) Abruptio placentae is correct because this is a condition where the placenta separates from the uterine wall before delivery, which can cause severe vaginal bleeding, abdominal pain, uterine contractions, and fetal distress. It is a life-threatening emergency that can be triggered by trauma and requires immediate delivery of the baby and treatment of shock and blood loss. Therefore, a woman who is 8 months pregnant and involved in a serious motor vehicle crash should be admitted to the hospital for observation for this complication.
Which is true about newborns classified as small for gestational age (SGA)?
Explanation
Choice a) They are born before 38 weeks of gestation is incorrect because this is not the definition of SGA. SGA refers to newborns who have a birth weight or length that is significantly lower than expected for their gestational age, regardless of when they are born. Therefore, a newborn can be SGA even if they are born at term or post-term.
Choice b) Placental malfunction is the only recognized cause of this condition is incorrect because this is not the only factor that can contribute to SGA. Placental malfunction can cause fetal growth restriction due to insufficient blood supply and nutrients to the fetus, but there are other possible causes such as maternal factors (e.g.,
hypertension, diabetes, smoking, malnutrition), fetal factors (e.g., chromosomal abnormalities, infections, congenital anomalies), and environmental factors (e.g., altitude, pollution, stress).
Choice c) They weigh less than 2500 g is incorrect because this is not the criterion for SGA. SGA is based on the comparison of the newborn's weight or length with the expected values for their gestational age, not on an absolute cutoff. Therefore, a newborn can be SGA even if they weigh more than 2500 g, as long as they are below the 10th percentile for their gestational age.
Choice d) They are below the 10th percentile on gestational growth charts is correct because this is the most commonly used definition of SGA. Gestational growth charts are tools that plot the expected weight or length of a fetus or newborn according to their gestational age and sex. They are based on population data and can vary
depending on the ethnicity and region of origin of the mother and the baby. A newborn who falls below the 10th percentile on these charts is considered SGA, meaning that they have grown less than 90% of their peers .

The nurse is observing a parent holding a preterm infant. The infant is sneezing, yawning, and extending the arms and legs. What action by the nurse is best?
Explanation
Choice a) Have the parent fold the infant's arms across the chest is incorrect because this is not a helpful way to calm a preterm infant. Folding the arms across the chest can restrict the infant's breathing and movement, and may increase their stress and discomfort. Preterm infants need gentle and supportive touch, not restraint or pressure.
Choice b) Encourage the parent to place the infant back in the warmer is incorrect because this is not a necessary or beneficial action for a preterm infant who is showing signs of overstimulation. Placing the infant back in the warmer can interrupt the bonding and attachment process between the parent and the infant, and may make the infant feel more isolated and insecure. Preterm infants need close and frequent contact with their parents, not separation or detachment.
Choice c) Encourage the parent to do kangaroo care is correct because this is an effective and evidence-based method of soothing and stabilizing a preterm infant who is experiencing overstimulation. Kangaroo care is a technique where the parent holds the infant skin-to-skin on their chest, providing warmth, comfort, and security. Kangaroo care can reduce the infant's stress hormones, lower their heart rate and blood pressure, improve their oxygenation and breathing, enhance their growth and development, and strengthen their bond with their parent.
Choice d) Cover the infant with a warm bed blanket is incorrect because this is not a sufficient or optimal way to comfort a preterm infant who is displaying signs of overstimulation. Covering the infant with a warm bed blanket can provide some warmth and protection, but it does not offer the same benefits as kangaroo care. A warm bed blanket cannot mimic the parent's heartbeat, voice, smell, and movement, which are essential for the infant's emotional and physiological well-being. Preterm infants need human touch and interaction, not just physical warmth.
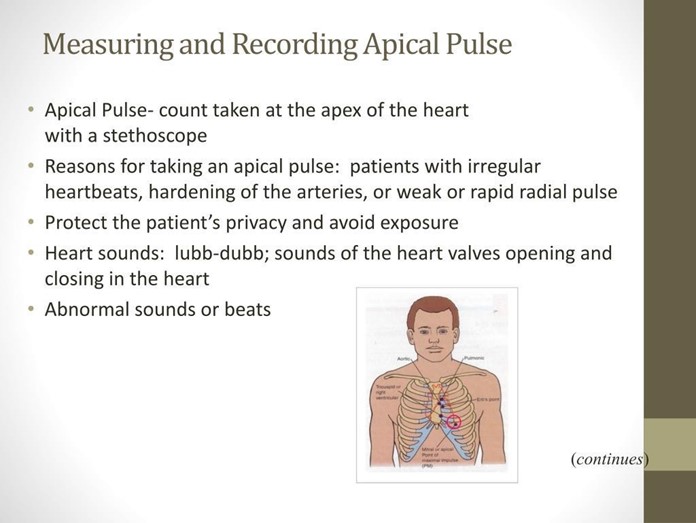
While assessing the newborn, the nurse should be aware that the average expected apical pulse range of a full-term, quiet, alert newborn is __ beats/min.
Explanation
Choice a) 100 to 120 is incorrect because this is too low for a normal newborn's heart rate. The heart rate of a newborn is influenced by factors such as gestational age, activity level, temperature, and health status. A full-term, quiet, alert newborn should have a heart rate between 120 and 160 beats per minute, which reflects their high metabolic rate and oxygen demand. A heart rate below 100 beats per minute may indicate bradycardia, which can be caused by hypoxia, hypothermia, or cardiac problems.
Choice b) 120 to 160 is correct because this is the normal range for a full-term, quiet, alert newborn's heart rate. The apical pulse is the best way to measure the heart rate of a newborn, as it reflects the actual contractions of the heart. The apical pulse can be auscultated at the fourth intercostal space on the left side of the chest, just below the nipple line. The nurse should count the apical pulse for a full minute, as it may vary with the respiratory cycle.
Choice c) 80 to 100 is incorrect because this is also too low for a normal newborn's heart rate. A full-term, quiet, alert newborn should have a heart rate between 120 and 160 beats per minute, which is higher than that of an adult or an older child. A heart rate below 100 beats per minute may indicate bradycardia, which can be caused by hypoxia, hypothermia, or cardiac problems.
Choice d) 150 to 180 is incorrect because this is too high for a normal newborn's heart rate. A full-term, quiet, alert newborn should have a heart rate between 120 and 160 beats per minute, which is lower than that of a preterm or a crying newborn. A heart rate above 160 beats per minute may indicate tachycardia, which can be caused by fever, infection, anemia, or hyperthyroidism.
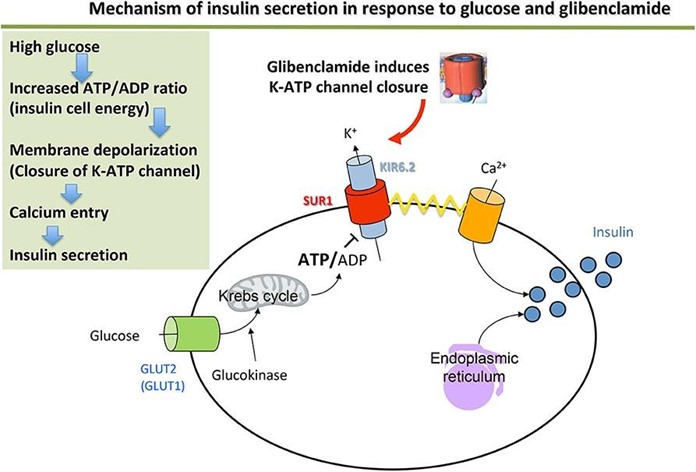
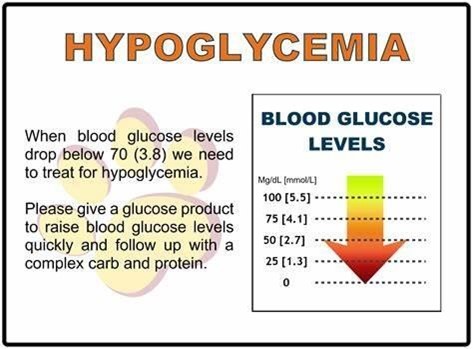
Four hours after delivery of a healthy neonate of an insulin-dependent diabetic woman, the baby appears jittery, irritable, and has a high-pitched cry. Which nursing action has top priority?
Explanation
Choice a) Document the event in the nurses' notes is incorrect because this is not a priority action for a neonate who is showing signs of hypoglycemia. Hypoglycemia is a condition where the blood glucose level is lower than normal, which can cause neurological and metabolic problems in newborns. Neonates of diabetic mothers are at higher risk of developing hypoglycemia due to increased insulin production and decreased glycogen stores.
Documenting the event in the nurses' notes is an important step, but it should be done after assessing and treating the neonate's condition.
Choice b) Test for blood glucose level is correct because this is the most important action for a neonate who is exhibiting symptoms of hypoglycemia. The nurse should use a heel stick or a cord blood sample to measure the blood glucose level of the neonate as soon as possible, as hypoglycemia can lead to serious complications such as seizures, coma, brain damage, or death if left untreated. The normal blood glucose range for a full-term neonate is 40 to 60 mg/dL in the first hour of life, and 50 to 90 mg/dL thereafter. A blood glucose level below 40 mg/dL indicates hypoglycemia and requires immediate intervention.
Choice c) Notify the clinician stat is incorrect because this is not the most urgent action for a neonate who is suffering from hypoglycemia. The nurse should notify the clinician after confirming the diagnosis of hypoglycemia and initiating treatment, such as feeding or administering intravenous glucose. The clinician may order further tests or treatments depending on the severity and cause of the hypoglycemia, but the nurse should not delay the initial management of the neonate's condition.
Choice d) Start an intravenous line with D5W is incorrect because this is not the first-line treatment for a neonate who has hypoglycemia. D5W stands for dextrose 5% in water, which is a solution that contains glucose and water. It can be used to treat hypoglycemia by providing a source of energy and fluid to the neonate. However, before starting an intravenous line with D5W, the nurse should first attempt to feed the neonate with breast milk or formula, as this can also raise the blood glucose level and provide other nutrients and antibodies. If feeding is unsuccessful or contraindicated, then the nurse should start an intravenous line with D5W as ordered by the clinician.
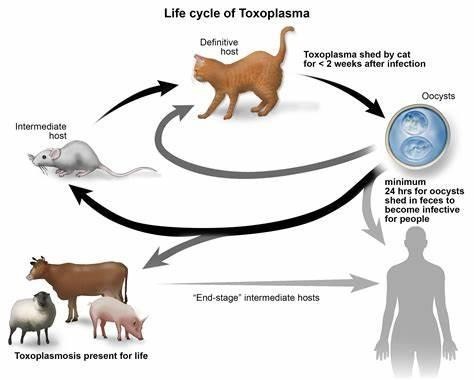
A nurse has taught a pregnant woman about toxoplasmosis. What statement by the patient indicates a need for further instruction?
Explanation
Choice a) I will be certain to empty the litter boxes regularly is incorrect because this is a risky behavior for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis is an infection caused by a parasite called Toxoplasma gondii, which can be found in the feces of cats and other animals. If a pregnant woman gets infected with toxoplasmosis, she can pass it to her unborn baby, which can cause serious problems such as miscarriage, stillbirth, or birth defects. Therefore, a pregnant woman should avoid contact with cat litter and let someone else handle the litter boxes, or wear gloves and wash her hands thoroughly if she has to do it herself.
Choice b) I have to wash all of my fruits and vegetables is correct because this is a good practice for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis can also be transmitted through contaminated soil or water, which can adhere to fruits and vegetables. Therefore, a pregnant woman should wash all of her fruits and vegetables before eating them, and peel or cook them if possible, to remove any traces of the parasite.
Choice c) I won't eat raw eggs is correct because this is another good practice for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis can also be acquired through eating undercooked or raw meat or eggs that contain the parasite. Therefore, a pregnant woman should avoid eating raw eggs or any foods that contain them, such as mayonnaise, mousse, or homemade ice cream, and cook all of her meat and eggs thoroughly until they are no longer pink or runny.
Choice d) I need to be cautious when cooking meat is correct because this is also an important practice for a pregnant woman who wants to prevent toxoplasmosis. Toxoplasmosis can also be spread through handling raw meat that contains the parasite. Therefore, a pregnant woman should be careful when cooking meat and use separate utensils and cutting boards for raw and cooked meat, wash her hands and surfaces after touching raw meat, and avoid tasting raw meat while cooking it.
The student nurse asks why gloves are needed when handling a newborn because the newborn "hasn't been exposed to anything". What response by the nurse is best?
Explanation
Choice a) We are protecting the infant from our bacteria is incorrect because this is not the main reason why gloves are needed when handling a newborn. While it is true that newborns have immature immune systems and are susceptible to infections, gloves are not only used to protect the infant from our bacteria but also to protect ourselves from the infant's body fluids and secretions, which may contain pathogens or blood-borne diseases.
Therefore, this response is incomplete and misleading.
Choice b) Amniotic fluid and maternal blood pose risks to us is incorrect because this is also not the primary reason why gloves are needed when handling a newborn. While it is true that amniotic fluid and maternal blood may contain harmful microorganisms or viruses that can infect us, gloves are not only used to protect ourselves from these substances but also to protect the infant from our skin flora and potential contaminants, which may cause skin irritation or infection. Therefore, this response is also incomplete and misleading.
Choice c) It is hospital policy is incorrect because this is not a sufficient or satisfactory reason why gloves are needed when handling a newborn. While it is true that wearing gloves may be a hospital policy or protocol, this response does not explain the rationale or evidence behind this policy and may imply that the nurse does not understand or agree with it. Therefore, this response is vague and unprofessional.
Choice d) It is part of standard precautions is correct because this is the best and most accurate reason why gloves are needed when handling a newborn. Standard precautions are a set of guidelines and practices that aim to prevent the transmission of infections in healthcare settings. They include wearing gloves, gowns, masks, and eye protection when there is a risk of exposure to blood or body fluids, as well as washing hands before and after patient contact, cleaning and disinfecting equipment and surfaces, and disposing of waste properly. Standard precautions apply to all patients, regardless of their diagnosis or infection status, and are based on the principle that all blood and body fluids are potentially infectious. Therefore, this response is clear and appropriate.
A nurse in a hospital is caring for a client who is at 38 weeks of gestation and has a large amount of painless, bright red vaginal bleeding. The client is placed on a fetal monitor indicating a regular fetal heart rate of 138/min and no uterine contractions. The client's vital signs are: blood pressure 98/52 mm Hg, heart rate 118/min, respiratory rate 24/min, and temperature 36.4°C (97.6°F). Which of the following is the priority nursing action?
Explanation
Choice a) Insert an indwelling urinary catheter is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Inserting an indwelling urinary catheter can cause trauma to the cervix or the placenta, which can worsen the bleeding and endanger the mother and the fetus. Therefore, this action should be avoided unless absolutely necessary.
Choice b) Prepare the abdominal and perineal areas is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Preparing the abdominal and perineal areas can be done before performing a cesarean section, which is usually the preferred mode of delivery for placenta previa. However, this action should be done after stabilizing the client's condition and obtaining informed consent for surgery.
Choice c) Witness the signature for informed consent for surgery is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery.
Witnessing the signature for informed consent for surgery can be done before performing a cesarean section, which is usually the preferred mode of delivery for placenta previa. However, this action should be done after stabilizing the client's condition and explaining the risks and benefits of surgery.
Choice d) Initiate IV access is correct because this is the priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Initiating IV access can help to restore fluid volume, prevent hypovolemic shock, administer medications such as oxytocin or blood products if needed, and prepare for emergency cesarean section if indicated. Therefore, this action should be done as soon as possible to save the life of the mother and the fetus.
Which maternal condition always necessitates delivery by cesarean section?
Explanation
Choice a) Ectopic pregnancy is incorrect because this is not a condition that requires delivery by cesarean section. Ectopic pregnancy is a condition where the fertilized egg implants outside the uterus, usually in the fallopian tube. It is a life-threatening complication that can cause internal bleeding and rupture of the tube. Ectopic pregnancy cannot result in a viable baby and must be terminated as soon as possible, either by medication or surgery. Therefore, this response is irrelevant and inaccurate.
Choice b) Preeclampsia is incorrect because this is not a condition that always necessitates delivery by cesarean section. Preeclampsia is a condition where the blood pressure rises above 140/90 mmHg after 20 weeks of pregnancy, along with proteinuria and edema. It can cause complications such as eclampsia, HELLP syndrome, placental abruption, and fetal growth restriction. The only cure for preeclampsia is delivery of the baby and placenta, but the mode of delivery depends on several factors, such as the gestational age, the severity of the condition, the fetal status, and the maternal preference. Therefore, some women with preeclampsia may deliver vaginally, while
others may need a cesarean section.
Choice c) Partial abruptio placentae is incorrect because this is not a condition that always necessitates delivery by cesarean section. Abruptio placentae is a condition where the placenta separates from the uterine wall before delivery, causing vaginal bleeding, abdominal pain, uterine contractions, and fetal distress. It can be classified as partial or complete, depending on the extent of the separation. The mode of delivery for abruptio placentae depends on several factors, such as the degree of bleeding, the fetal viability, the cervical dilation, and the fetal position.
Therefore, some women with partial abruptio placentae may deliver vaginally, while others may need a cesarean section.
Choice d) Total placenta previa is correct because this is the only condition that always necessitates delivery by cesarean section. Placenta previa is a condition where the placenta covers part or all of the cervix, preventing normal delivery. It can be classified as marginal, partial, or total, depending on the degree of overlap. The mode of delivery for placenta previa depends on several factors, such as the type of previa, the amount of bleeding, the gestational age, and the fetal status. However, women with total placenta previa have no chance of delivering vaginally, as the placenta completely blocks the birth canal. Therefore, they must have a cesarean section to avoid hemorrhage and fetal compromise.
What documentation on a woman's chart on postpartum day 14 indicates a normal involution process?
Explanation
Choice a) Breasts firm and tender is incorrect because this is not a sign of normal involution, but rather a sign of breast engorgement, which is a common problem in the first few weeks of breastfeeding. Breast engorgement occurs when thE breasts become overfilled with milk, causing them to feel hard, swollen, painful, and warm. It can be prevented or relieved by frequent and effective breastfeeding, applying warm or cold compresses, massaging the breasts, expressing some milk, and wearing a supportive bra.
Choice b) Episiotomy slightly red and puffy is incorrect because this is not a sign of normal involution, but rather a sign of inflammation or infection of the perineal wound. An episiotomy is a surgical cut made in the perineum (the area between the vagina and the anus) to enlarge the vaginal opening during delivery. It can take several weeks to heal and may cause pain, swelling, bruising, bleeding, or discharge. It can be cared for by keeping the area clean and dry, applying ice packs or witch hazel pads, taking painkillers or sitz baths, and avoiding constipation or straining.
Choice c) Fundus below the symphysis and not palpable is correct because this is a sign of normal involution, which is the process of the uterus returning to its pre-pregnancy size and shape after delivery. The fundus is the upper part of the uterus that can be felt through the abdomen. Immediately after delivery, the fundus is about the size of a grapefruit and can be felt at or above the umbilicus (the navel). It gradually descends about one fingerbreadth per day until it reaches the level of the symphysis pubis (the joint where the two pubic bones meet) by about 10 days postpartum. By 14 days postpartum, the fundus should be below the symphysis and not palpable.
Choice d) Moderate bright red lochial flow is incorrect because this is not a sign of normal involution, but rather a sign of excessive or prolonged bleeding after delivery. Lochia is the vaginal discharge that consists of blood, mucus, and tissue from the lining of the uterus. It changes in color and amount over time, from red to pink to brown to yellow to white. The normal lochia flow should be scant to moderate in amount, dark red to brown in color, and last for about 4 to 6 weeks postpartum. A moderate bright red lochial flow on day 14 postpartum may indicate that the uterus is not contracting well or that there is an infection or retained placental tissue in the uterus.

The infant of a mother with diabetes is hypoglycemic. What type of feeding should be instituted first?
Explanation
Choice a) D5W intravenously is incorrect because this is not the preferred method of feeding for a hypoglycemic infant. D5W stands for dextrose 5% in water, which is a solution that contains glucose and water. It can be used to treat hypoglycemia by providing a source of energy and fluid to the infant. However, it has several disadvantages, such as requiring an invasive procedure, increasing the risk of infection, causing fluid overload or electrolyte imbalance, and stimulating insulin secretion, which can lead to rebound hypoglycemia. Therefore, D5W intravenously should be reserved for severe cases of hypoglycemia that do not respond to oral or enteral feeding.
Choice b) Formula via nasogastric tube is incorrect because this is not the first-line option of feeding for a hypoglycemic infant. Formula is an artificial substitute for breast milk that contains nutrients and calories to support the infant's growth and development. It can be given via nasogastric tube, which is a tube that passes through the nose and into the stomach, when the infant cannot suck or swallow effectively. However, formula has several disadvantages, such as being less digestible, less immunogenic, and less adaptable than breast milk, as well as increasing the risk of necrotizing enterocolitis, allergy, or infection. Therefore, formula via nasogastric tube should be used only when breast milk is unavailable or contraindicated.
Choice c) Breast milk is correct because this is the best and most recommended type of feeding for a hypoglycemic infant. Breast milk is the natural and optimal food for infants that contains all the nutrients and antibodies they need to grow and thrive. It can be given directly from the breast or expressed and fed by bottle or cup. Breast milk has several advantages, such as being easily digestible, enhancing immune function, promoting bonding, and adjusting to the infant's needs. Breast milk also contains lactose, which is a natural sugar that can raise the blood glucose level of the infant without causing a spike in insulin secretion. Therefore, breast milk should be offered to the hypoglycemic infant as soon as possible after birth and at regular intervals thereafter.
Choice d) Glucose water in a bottle is incorrect because this is not an appropriate type of feeding for a hypoglycemic infant. Glucose water is a solution that contains glucose and water. It can be given by bottle or cup to provide a quick source of energy to the infant. However, it has several disadvantages, such as providing no other nutrients or calories, interfering with breastfeeding, causing diarrhea or dehydration, and stimulating insulin secretion, which can lead to rebound hypoglycemia. Therefore, glucose water in a bottle should be avoided or used sparingly for mild cases of hypoglycemia that do not respond to breast milk.
A baby is grunting in the neonatal nursery. Which of the following actions by the nurse is appropriate?
Explanation
Choice a) Check the baby's diaper is incorrect because this is not a priority action for a baby who is grunting in the neonatal nursery. Grunting is a sign of respiratory distress, which means that the baby is having difficulty breathing and is trying to keep air in the lungs by making a low-pitched sound with each expiration. Checking the baby's diaper may be part of routine care, but it does not address the underlying cause of the grunting or improve the baby's oxygenation. Therefore, this action should be done after assessing and treating the baby's respiratory status.
Choice b) Place a pacifier in the baby's mouth is incorrect because this is not an appropriate action for a baby who is grunting in the neonatal nursery. Grunting is a sign of respiratory distress, which means that the baby is having difficulty breathing and is trying to keep air in the lungs by making a low-pitched sound with each expiration. Placing a pacifier in the baby's mouth may interfere with the baby's breathing and worsen the grunting, as it can obstruct the airway, increase the work of breathing, or cause aspiration. Therefore, this action should be avoided or used with caution for babies who are grunting.
Choice c) Have the mother feed the baby is incorrect because this is not a safe action for a baby who is grunting in the neonatal nursery. Grunting is a sign of respiratory distress, which means that the baby is having difficulty breathing and is trying to keep air in the lungs by making a low-pitched sound with each expiration. Having the mother feed the baby may increase the risk of choking or aspiration, as the baby may not be able to coordinate sucking, swallowing, and breathing. Therefore, this action should be delayed or modified until the baby's respiratory status improves.
Choice d) Assess the respiratory rate is correct because this is the most important action for a baby who is grunting in the neonatal nursery. Grunting is a sign of respiratory distress, which means that the baby is having difficulty breathing and is trying to keep air in the lungs by making a low-pitched sound with each expiration. Assessing the respiratory rate can help to determine the severity and cause of the respiratory distress, as well as guide further interventions such as oxygen therapy, suctioning, or medication. The normal respiratory rate for a newborn ranges from 30 to 60 breaths per minute, and it may vary with sleep or activity. A respiratory rate above 60 breaths per minute or below 30 breaths per minute indicates abnormality and requires immediate attention. Therefore, this action should be done as soon as possible for babies who are grunting.
A nurse is caring for a pregnant woman at 30 weeks of gestation in preterm labor. The woman's physician orders
Explanation
Choice a) Consult the physician, because the dose is too high is incorrect because this is not a necessary or appropriate action for a nurse who is following a valid order for betamethasone. Betamethasone is a corticosteroid that can be used to accelerate fetal lung maturation and reduce the risk of respiratory distress syndrome and other complications in preterm infants. The recommended dose for betamethasone is 12 mg IM every 24 hours for two doses, which is exactly what the physician ordered. Therefore, there is no reason to question or consult the physician about the dose, as it is within the normal range and based on evidence-based practice.
Choice b) Schedule the second dose for 11 am on the next day is incorrect because this is not a correct or accurate way to implement the order for betamethasone. Betamethasone should be given at least 24 hours apart, but not more than 48 hours apart, to achieve optimal fetal lung development and neonatal outcomes. Scheduling the second dose for 11 am on the next day would result in a 24-hour interval between the doses, which is acceptable, but not ideal. The best time to schedule the second dose would be between 24 and 48 hours after the first dose, such as at 11 pm on the same day or at 7 am on the next day.
Choice c) Prepare to administer the medication intramuscularly between contractions is correct because this is the best and most appropriate way to implement the order for betamethasone. Betamethasone should be given by intramuscular injection in a large muscle mass, such as the deltoid or gluteus, using a 21-gauge needle and a syringe with an air lock. The injection site should be cleaned with alcohol and aspirated before injecting. The medication should be administered between contractions, when the uterine blood flow is maximal and the fetal absorption is optimal. The nurse should also monitor the woman and the fetus for any adverse effects of betamethasone, such as maternal hyperglycemia, hypertension, infection, or edema, or fetal tachycardia, hypoglycemia, or infection.
Choice d) Explain to the woman that this medication will reduce her heart rate and help her to breathe easier is incorrect because this is not a true or relevant statement about betamethasone. Betamethasone does not have any direct effect on the maternal heart rate or respiratory function, as it is mainly intended to improve the fetal lung maturation and reduce the risk of respiratory distress syndrome and other complications in preterm infants.
Betamethasone may cause some side effects such as increased blood pressure, blood sugar, or fluid retention in the mother, which may affect her cardiovascular or respiratory status indirectly. However, these effects are usually transient and mild, and do not outweigh the benefits of betamethasone for the fetus. Therefore, this statement is misleading and inaccurate.
Which condition seen in the postpartum period is likely to require careful medical assessment?
Explanation
Choice a) Headaches is correct because this is a condition that can indicate a serious problem in the postpartum period and may require careful medical assessment. Headaches are common in the first few weeks after giving birth, but they can also be a sign of complications such as preeclampsia, eclampsia, cerebral venous thrombosis, meningitis, or aneurysm. Preeclampsia and eclampsia are conditions that cause high blood pressure, proteinuria, and seizures in pregnant or postpartum women. Cerebral venous thrombosis is a blood clot in the brain that can cause stroke-like symptoms. Meningitis is an infection of the membranes that cover the brain and spinal cord. Aneurysm is a bulge or rupture in a blood vessel that can cause bleeding in the brain. These conditions can be life-threatening and require immediate treatment. Therefore, women who experience severe, persistent, or unusual headaches in the postpartum period should seek medical attention as soon as possible.
Choice b) Varicosities of the legs is incorrect because this is not a condition that usually requires careful medical assessment in the postpartum period. Varicosities are enlarged or swollen veins that appear blue or purple under the skin. They are common in pregnancy due to increased blood volume, hormonal changes, and pressure from the growing uterus. They usually improve after delivery, but may persist or worsen in some women. Varicosities are usually harmless and do not cause any symptoms, but they may cause cosmetic concerns, discomfort, itching, or bleeding. They can also increase the risk of superficial thrombophlebitis, which is inflammation of a vein near the skin surface. However, these complications are rare and mild, and can be managed with conservative measures such as compression stockings, elevation of the legs, exercise, and painkillers. Therefore, women who have varicosities of the legs in the postpartum period do not need to worry too much, unless they have signs of infection or deep vein thrombosis, which is a more serious condition that involves a blood clot in a deep vein that can travel to the lungs and cause pulmonary embolism.
Choice c) Carpal tunnel syndrome is incorrect because this is not a condition that typically requires careful medical assessment in the postpartum period. Carpal tunnel syndrome is a condition that causes numbness, tingling, pain, or weakness in the hand and wrist due to compression of the median nerve that runs through a narrow passage called the carpal tunnel. It can occur in pregnancy due to fluid retention, hormonal changes, or repetitive movements. It usually resolves after delivery, but may persist or recur in some women. Carpal tunnel syndrome is usually mild and does not cause any serious complications, but it may interfere with daily activities or quality of life. It can be treated with conservative measures such as splinting, icing, massage, stretching, or painkillers. In severe cases, surgery may be needed to release the pressure on the nerve. Therefore, women who have carpal tunnel syndrome in the postpartum period do not need to seek medical attention urgently, unless they have signs of nerve damage or infection.
Choice d) Periodic numbness and tingling of the fingers is incorrect because this is not a condition that generally requires careful medical assessment in the postpartum period. Periodic numbness and tingling of the fingers can be caused by various factors such as cold exposure, poor circulation, nerve compression, vitamin deficiency, or anxiety.
It can also occur in pregnancy due to fluid retention or hormonal changes. It usually goes away after delivery, but may linger or come back in some women. Periodic numbness and tingling of the fingers is usually harmless and does not indicate any serious problem, but it may cause discomfort or annoyance. It can be relieved with simple measures such as warming up, moving around, shaking out the hands, taking supplements, or relaxing. Therefore, women who experience periodic numbness and tingling of the fingers in the postpartum period do not need to worry too much, unless they have signs of infection or neurological disorder.
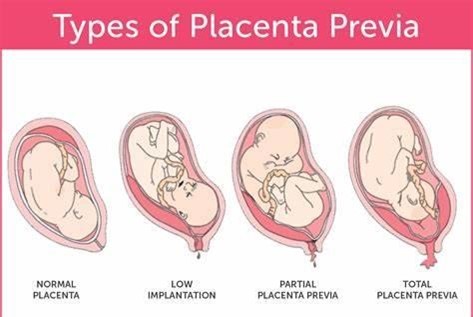
A nurse is caring for a client who is at 37 weeks of gestation and has placenta previa. The client asks the nurse why the provider does not do an internal examination. Which of the following explanations of the primary reason should the nurse provide?
Explanation
Choice a) This could result in profound bleeding is correct because this is the primary reason why an internal examination should be avoided for a client who has placenta previa. Placenta previa is a condition where the placenta covers part or all of the cervix, preventing normal delivery. An internal examination involves inserting a gloved finger or a speculum into the vagina and cervix to assess their dilation, effacement, position, and station. This can cause trauma to the cervix or the placenta, which can trigger severe hemorrhage and endanger the mother and the fetus. Therefore, this explanation is accurate and appropriate.
Choice b) This could initiate preterm labor is incorrect because this is not the main reason why an internal examination should be avoided for a client who has placenta previa. Placenta previa is a condition where the placenta covers part or all of the cervix, preventing normal delivery. An internal examination may stimulate uterine contractions, which can lead to preterm labor and delivery. However, this is not the most serious or likely complication of an internal examination for a client who has placenta previa, as the bleeding risk is much higher and more urgent. Therefore, this explanation is incomplete and misleading.
Choice c) There is an increased risk of introducing infection is incorrect because this is not a specific reason why an internal examination should be avoided for a client who has placenta previa. Placenta previa is a condition where the placenta covers part or all of the cervix, preventing normal delivery. An internal examination may introduce bacteria or other microorganisms into the vagina or cervix, which can cause infection and inflammation. However, this is a general risk that applies to any pregnant woman who undergoes an internal examination, not just those who have placenta previa. Therefore, this explanation is irrelevant and inaccurate.
Choice d) There is an increased risk of rupture of the membranes is incorrect because this is not a relevant reason why an internal examination should be avoided for a client who has placenta previa. Placenta previa is a condition where the placenta covers part or all of the cervix, preventing normal delivery. An internal examination may cause rupture of the membranes, which are the sacs that contain the amniotic fluid and the fetus. However, this is not a significant or common complication of an internal examination for a client who has placenta previa, as the membranes are usually located above or away from the placenta and cervix. Therefore, this explanation is improbable and inaccurate.
The priority nursing intervention when admitting a pregnant woman who has experienced a bleeding episode in late pregnancy is:
Explanation
Choice A) Monitor uterine contractions is incorrect because this is not the most urgent intervention for a pregnant woman who has experienced a bleeding episode in late pregnancy. Uterine contractions can indicate labor or placental abruption, which are possible causes of bleeding in late pregnancy. However, they are not the only or the most reliable indicators of these conditions, as some women may have painless bleeding or contractions without bleeding. Moreover, monitoring uterine contractions does not address the immediate needs of the mother and the fetus, such as oxygenation, circulation, and perfusion. Therefore, this intervention should be done after assessing and stabilizing the vital signs and FHR.
Choice B) Assess fetal heart rate (FHR) and maternal vital signs is correct because this is the most important and essential intervention for a pregnant woman who has experienced a bleeding episode in late pregnancy. Bleeding in late pregnancy can be caused by various conditions, such as placenta previa, placental abruption, uterine rupture, or vasa previa, which can compromise the blood supply and oxygen delivery to the mother and the fetus. Assessing FHR and maternal vital signs can help to determine the severity and cause of the bleeding, as well as guide further
interventions such as fluid resuscitation, oxygen therapy, blood transfusion, or emergency delivery. The normal FHR range for a fetus is 110 to 160 beats per minute, and it may vary with fetal activity or maternal position. The normal maternal vital signs are: blood pressure 120/80 mm Hg or lower, heart rate 60 to 100 beats per minute, respiratory rate 12 to 20 breaths per minute, and temperature 36.5°C to 37.5°C (97.7°F to 99.5°F). Any deviation from these ranges may indicate hypoxia, hypovolemia, shock, infection, or distress. Therefore, this intervention should be done as soon as possible for women who have bleeding in late pregnancy.
Choice c) Perform a venipuncture for hemoglobin and hematocrit levels is incorrect because this is not a priority intervention for a pregnant woman who has experienced a bleeding episode in late pregnancy. Hemoglobin and hematocrit are blood tests that measure the amount of red blood cells and their percentage in the blood volume.
They can help to evaluate the extent of blood loss and the need for blood transfusion. However, they are not
immediate or accurate indicators of bleeding in late pregnancy, as they may take time to reflect the changes in blood volume or be affected by other factors such as hydration or hemodilution. Moreover, performing a venipuncture does not address the immediate needs of the mother and the fetus, such as oxygenation, circulation, and perfusion.
Therefore, this intervention should be done after assessing and stabilizing the vital signs and FHR.
Choice d) Place clean disposable pads to collect any drainage is incorrect because this is not a priority intervention for a pregnant woman who has experienced a bleeding episode in late pregnancy. Placing clean disposable pads can help to keep the perineal area clean and dry, as well as to estimate the amount and type of bleeding. However, it does not address the immediate needs of the mother and the fetus, such as oxygenation, circulation, and perfusion. Moreover, it does not provide any information about the cause or severity of the bleeding, as it may be affected by factors such as gravity or pooling. Therefore, this intervention should be done after assessing and stabilizing the vital signs and FHR.
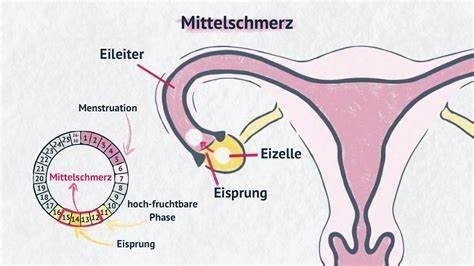
What is the correct definition of Mittelschmerz?
Explanation
Choice a) A phase of the female menstrual cycle that involves the release of an egg (ovum) from one of the ovaries is incorrect because this is not the definition of Mittelschmerz, but rather the definition of ovulation. Ovulation is the process by which one or more eggs are released from the ovaries and travel to the fallopian tubes, where they can be fertilized by sperm. Ovulation usually occurs around the middle of the menstrual cycle, which is typically 28 days long, but can vary from person to person. Ovulation can be detected by changes in basal body temperature, cervical mucus, or hormone levels. Therefore, this response is inaccurate and misleading.
Choice B) A female reproductive organ in which ova or eggs are produced is incorrect because this is not the definition of Mittelschmerz, but rather the definition of ovary. The ovary is a paired organ that is located on either side of the uterus in the lower abdomen. The ovary contains thousands of follicles, which are sacs that contain immature eggs. Each month, one or more follicles mature and release an egg during ovulation. The ovary also produces hormones such as estrogen and progesterone, which regulate the menstrual cycle and pregnancy. Therefore, this response is irrelevant and inaccurate.
Choice C) The regular discharge of blood and mucosal tissue from the inner lining of the uterus through the vagina is incorrect because this is not the definition of Mittelschmerz, but rather the definition of menstruation. Menstruation is the process by which the endometrium, which is the tissue that lines the uterus and prepares for implantation of a fertilized egg, is shed and expelled through the vagina if pregnancy does not occur. Menstruation usually occurs once a month and lasts for about 3 to 7 days, but can vary from person to person. Menstruation can be accompanied by symptoms such as cramps, bloating, mood swings, or headaches. Therefore, this response is irrelevant and inaccurate.
Choice D) One-sided, lower belly pain associated with normal ovulation. Usually occurs about 14 days before the next menstrual period is correct because this is the definition of Mittelschmerz. Mittelschmerz is a German word that means "middle pain". It refers to a mild to moderate pain or discomfort that some women experience in their lower abdomen around the time of ovulation. The pain may last for a few minutes to a few hours and may switch sides from month to month depending on which ovary releases an egg. The pain may be caused by irritation or stretching of the ovarian or abdominal wall by the maturing follicle or by fluid or blood released during ovulation.
Mittelschmerz is not a sign of any disease or problem and does not require any treatment. However, it can be confused with other conditions that cause pelvic pain, such as appendicitis, ectopic pregnancy, or ovarian cysts. Therefore, women who have severe or persistent pain should consult their doctor for diagnosis and treatment. Therefore, this response is clear and accurate.
The nurse is teaching the parents of a newborn who is going to receive phototherapy. What other measure does the nurse teach to help reduce the bilirubin?
Explanation
Choice A) Increase oral intake of water between feedings is incorrect because this is not a helpful or recommended measure to help reduce the bilirubin in a newborn who is receiving phototherapy. Bilirubin is a yellow pigment that is produced when red blood cells are broken down. It is normally excreted by the liver into bile and then eliminated by the intestines. However, some newborns have high levels of bilirubin in their blood, which can cause jaundice, a condition that makes the skin and eyes look yellow. Phototherapy is a treatment that uses blue light to help break down the bilirubin and make it easier for the liver to process. Increasing oral intake of water between feedings does not have any effect on the bilirubin level, as water does not contain any nutrients or calories that can stimulate the liver or bowel function. Moreover, giving water to a newborn can cause hyponatremia, which is a low level of sodium in the blood that can lead to seizures, brain damage, or death. Therefore, this measure should be avoided or used with caution for newborns who are receiving phototherapy.
Choice B) Wrap the infant in triple blankets to prevent cold stress during phototherapy is incorrect because this is not a safe or appropriate measure to help reduce the bilirubin in a newborn who is receiving phototherapy. Cold stress is a condition that occurs when a newborn loses too much heat and has difficulty maintaining a normal body temperature. It can cause complications such as hypoglycemia, hypoxia, acidosis, or bleeding. Wrapping the infant in triple blankets may seem like a good way to prevent cold stress, but it can actually cause overheating, dehydration, or hyperthermia, which are equally dangerous for the newborn. Moreover, wrapping the infant in blankets can reduce the effectiveness of phototherapy, as it blocks the exposure of the skin to the blue light. Therefore, this measure should be avoided or used with caution for newborns who are receiving phototherapy.
Choice C) How to prepare the newborn for an exchange transfusion is incorrect because this is not a relevant or necessary measure to help reduce the bilirubin in a newborn who is receiving phototherapy. An exchange transfusion is a procedure that involves replacing some of the newborn's blood with donor blood to lower the bilirubin level and prevent brain damage. It is usually reserved for severe cases of jaundice that do not respond to phototherapy or other treatments. Preparing the newborn for an exchange transfusion involves obtaining informed consent from the parents, placing an umbilical venous catheter, monitoring vital signs and blood tests, and administering medications and fluids. However, these steps are not part of routine care for newborns who are receiving phototherapy, and they do not help to reduce the bilirubin level by themselves. Therefore, this measure should be done only when indicated by the physician and explained by the nurse.
Choice D) Increase the frequency of feedings is correct because this is an effective and recommended measure to help reduce the bilirubin in a newborn who is receiving phototherapy. Feeding provides nutrients and calories that can stimulate the liver and bowel function, which are essential for processing and eliminating bilirubin from the body. Feeding also helps to prevent dehydration, which can worsen jaundice and increase the risk of complications.
Feeding can be done by breast milk or formula, depending on the mother's preference and availability. The frequency of feedings should be increased to at least every 2 to 3 hours or on demand, as long as the newborn shows signs of hunger and satisfaction. Therefore, this measure should be encouraged and supported by the nurse for newborns who are receiving phototherapy.
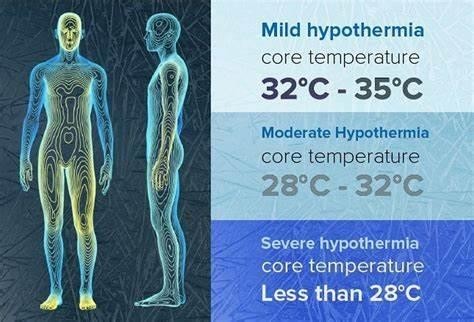
What is the result of hypothermia in the newborn?
Explanation
Choice A) Decreased metabolic rate is incorrect because this is not a result of hypothermia in the newborn, but rather a cause of it. Metabolic rate is the speed at which the body uses energy to perform its functions. Newborns have a high metabolic rate, which helps them to maintain a normal body temperature of 36.5°C to 37.5°C (97.7°F to 99.5°F). However, some factors can lower the metabolic rate of newborns, such as prematurity, low birth weight, infection, or hypoglycemia. A low metabolic rate can make the newborn more susceptible to heat loss and hypothermia, which is a condition that occurs when the body temperature drops below 36°C (96.8°F). Therefore, this response is inaccurate and misleading.
Choice B) Decreased oxygen demands is incorrect because this is not a result of hypothermia in the newborn, but rather a consequence of it. Oxygen demand is the amount of oxygen that the body needs to function properly.
Newborns have a high oxygen demand, which helps them to support their growth and development. However, some factors can decrease the oxygen demand of newborns, such as hypothermia, sedation, or asphyxia. A low oxygen demand can impair the oxygen delivery and utilization by the tissues and organs, leading to hypoxia, acidosis, or organ failure. Therefore, this response is irrelevant and inaccurate.
Choice C) Shivering to generate heat is incorrect because this is not a result of hypothermia in the newborn, but rather a mechanism that is absent in them. Shivering is an involuntary contraction of the muscles that produces heat and raises the body temperature. It is a common response to cold exposure in adults and older children, but not in newborns. Newborns do not have the ability to shiver, as their muscles are immature and lack glycogen stores.
Instead, they rely on other methods to generate heat, such as non-shivering thermogenesis, which involves burning brown fat in certain areas of the body. Therefore, this response is irrelevant and inaccurate.
Choice D) Increased glucose demands is correct because this is a result of hypothermia in the newborn that can cause complications. Glucose demand is the amount of glucose that the body needs to produce energy and maintain its functions. Newborns have a high glucose demand, which helps them to support their metabolic rate and thermoregulation. However, some factors can increase the glucose demand of newborns, such as hypothermia, stress, or infection. A high glucose demand can deplete the glucose stores and cause hypoglycemia, which is a low level of glucose in the blood that can lead to seizures, brain damage, or death. Therefore, this response is clear and accurate.
The nurse is caring for a neonate undergoing phototherapy. What action does the nurse include on the infant's care plan?
Explanation
Choice A) Dress the infant in only a T-shirt and diaper is correct because this is an appropriate and recommended action for a neonate undergoing phototherapy. Phototherapy is a treatment that uses blue light to help break down the bilirubin and make it easier for the liver to process. Bilirubin is a yellow pigment that is produced when red blood cells are broken down. It can cause jaundice, a condition that makes the skin and eyes look yellow. Dressing the infant in only a T-shirt and diaper can maximize the exposure of the skin to the light and increase the effectiveness of phototherapy. It can also prevent overheating, dehydration, or skin irritation that may occur if the infant is dressed too warmly or tightly. Therefore, this action should be included on the infant's care plan.
Choice B) Restrict parental and oral fluids is incorrect because this is not a helpful or recommended action for a neonate undergoing phototherapy. Fluids are essential for maintaining hydration, circulation, and perfusion in the body. They can also help to flush out the bilirubin from the blood and urine. Restricting fluids can cause dehydration, hypovolemia, shock, or kidney damage in the neonate. Moreover, fluids can provide nutrients and calories that can stimulate the liver and bowel function, which are important for processing and eliminating bilirubin. Therefore, this action should be avoided or used with caution for neonates undergoing phototherapy.
Choice C) Keep the infant supine at all times is incorrect because this is not a safe or appropriate action for a neonate undergoing phototherapy. Supine means lying on the back with the face up. Keeping the infant supine at all times can limit the exposure of the skin to the light and reduce the effectiveness of phototherapy. It can also increase the risk of aspiration, suffocation, or sudden infant death syndrome (SIDS), which are conditions that occur when the infant stops breathing due to obstruction of the airway or lack of oxygen. Therefore, this action should be avoided or used with caution for neonates undergoing phototherapy.
Choice D) Keep the infant's eyes covered under the light is incorrect because this is not a necessary or recommended action for a neonate undergoing phototherapy. The eyes are sensitive organs that can be damaged by exposure to bright or intense light. However, modern phototherapy devices use blue light that has a low intensity and wavelength that do not harm the eyes. Moreover, covering the eyes can interfere with bonding, feeding, or development of the neonate. Therefore, this action should be done only when indicated by the physician and explained by the nurse.
A nurse is teaching an assistive personnel to measure a newborn's respiratory rate. Which of the following statements indicates an understanding of why the respiratory rate should be counted for a complete minute?
Explanation
Choice A) Newborns are abdominal breathers is incorrect because this is not a reason why the respiratory rate should be counted for a complete minute, but rather a characteristic of how newborns breathe. Abdominal breathing means that the diaphragm and the abdominal muscles are the main muscles used for breathing, rather than the chest muscles. Newborns are abdominal breathers because their chest wall is more compliant and less stable than adults, and their intercostal muscles are not fully developed. Abdominal breathing does not affect the accuracy or duration of measuring the respiratory rate, as long as the abdomen is visible and palpable. Therefore, this response is irrelevant and inaccurate.
Choice B) Activity will increase the respiratory rate is incorrect because this is not a reason why the respiratory rate should be counted for a complete minute, but rather a factor that can influence the respiratory rate. Activity means any physical or mental exertion that requires more oxygen and energy from the body. Activity can increase the respiratory rate, as well as the heart rate and blood pressure, to meet the increased oxygen demand and carbon dioxide removal. However, activity does not affect the accuracy or duration of measuring the respiratory rate, as long as the newborn is calm and resting during the measurement. Therefore, this response is irrelevant and inaccurate.
Choice C) The rate and rhythm of breath are irregular in newborns is correct because this is a reason why the respiratory rate should be counted for a complete minute. The rate and rhythm of breath refer to how fast and how regularly one breathes. Newborns have an irregular rate and rhythm of breath, which means that they breathe at different speeds and intervals, sometimes pausing for a few seconds between breaths. This is normal and harmless for newborns, as long as they do not stop breathing for more than 20 seconds or show signs of distress. However, it can make it difficult to measure the respiratory rate accurately, as counting for a shorter period may not reflect the true average rate. Therefore, counting for a complete minute can ensure a more reliable measurement. Therefore, this response is clear and accurate.
Choice D) Newborns do not expand their lungs fully with each respiration is incorrect because this is not a reason why the respiratory rate should be counted for a complete minute, but rather a feature of how newborns breathe.
Lung expansion means how much air one inhales and exhales with each breath. Newborns do not expand their lungs fully with each respiration, because they have smaller lung volumes and capacities than adults, and they breathe more shallowly and rapidly. However, lung expansion does not affect the accuracy or duration of measuring the respiratory rate, as long as the chest or abdomen movement is visible and palpable. Therefore, this response is irrelevant and inaccurate.

A nurse is caring for a client who is postpartum and received methylergonovine (methergine). Which of the following findings indicates that the medication was effective?
Explanation
Choice A) Report of absent breast pain is incorrect because this is not a finding that indicates that the medication was effective, but rather a finding that indicates that the client does not have mastitis or engorgement. Mastitis is an infection of the breast tissue that causes pain, swelling, redness, and fever. Engorgement is a condition where the breasts become overfilled with milk, causing pain, hardness, and leakage. Both conditions are common in postpartum women who are breastfeeding, but they are not related to methylergonovine or uterine bleeding. Therefore, this response is irrelevant and inaccurate.
Choice B) Increase in lochia is incorrect because this is not a finding that indicates that the medication was effective, but rather a finding that indicates that the medication was ineffective or that the client has a complication. Lochia is the vaginal discharge that consists of blood, mucus, and tissue from the uterus after childbirth. It usually lasts for about 4 to 6 weeks and gradually decreases in amount and color. Methylergonovine is a medication that helps to control uterine bleeding by improving the tone and contractions of the uterus. An increase in lochia may mean that methylergonovine did not work well or that the client has a problem such as retained placenta, infection, or subinvolution. Therefore, this response is opposite and inaccurate.
Choice C) Increase in blood pressure is incorrect because this is not a finding that indicates that the medication was effective, but rather a finding that indicates that the client has a side effect or a risk factor. Blood pressure is the force of blood against the walls of the arteries. It is measured by two numbers: systolic (the pressure when the heart beats) and diastolic (the pressure when the heart rests). The normal range for blood pressure is 120/80 mm Hg or lower. Methylergonovine is a medication that can cause vasoconstriction, which means narrowing of the blood vessels and increasing of the blood pressure. This can lead to complications such as hypertension, stroke, or heart attack. Therefore, this response is adverse and inaccurate.
Choice D) Fundus firm to palpation is correct because this is a finding that indicates that the medication was effective and that the client has a good outcome. The fundus is the upper part of the uterus that can be felt through the abdomen after childbirth. It should be firm, midline, and at or below the level of the navel. A firm fundus means that the uterus has contracted well and stopped bleeding. Methylergonovine is a medication that helps to achieve this by improving the tone and contractions of the uterus. Therefore, this response is positive and accurate.

A nurse in the antepartum unit is caring for a client who is at 36 weeks of gestation and has gestational hypertension. Suddenly, the client reports continuous abdominal pain and vaginal bleeding. The nurse should suspect which of the following complications?
Explanation
Choice A) Placenta previa is incorrect because this is not a likely complication for a client who has gestational hypertension and reports continuous abdominal pain and vaginal bleeding. Placenta previa is a condition where the placenta covers part or all of the cervix, preventing normal delivery. It can cause painless, bright red bleeding in the third trimester, especially after intercourse or a pelvic exam. However, it does not cause abdominal pain, as the bleeding is not associated with uterine contractions or separation. Moreover, it is not related to gestational hypertension, which is a condition that causes high blood pressure during pregnancy. Therefore, this response is irrelevant and inaccurate.
Choice B) Incompetent cervix is incorrect because this is not a possible complication for a client who is at 36 weeks of gestation and has gestational hypertension and reports continuous abdominal pain and vaginal bleeding.
Incompetent cervix is a condition where the cervix is weak and unable to hold the pregnancy, leading to premature dilation and delivery. It can cause painless, watery vaginal discharge or spotting in the second trimester, followed by rupture of membranes and labor. However, it does not cause abdominal pain or heavy bleeding, as the cervix does not tear or detach from the uterus. Moreover, it is not related to gestational hypertension, which is a condition that causes high blood pressure during pregnancy. Therefore, this response is irrelevant and inaccurate.
Choice C) Prolapsed cord is incorrect because this is not a common complication for a client who has gestational hypertension and reports continuous abdominal pain and vaginal bleeding. Prolapsed cord is a condition where the umbilical cord slips through the cervix and into the vagina before the baby, compressing the cord and cutting off the blood supply and oxygen to the baby. It can cause variable or prolonged fetal heart rate decelerations, visible or palpable cord in the vagina, or fetal distress. However, it does not cause abdominal pain or bleeding, as the cord does not rupture or bleed. Moreover, it is not related to gestational hypertension, which is a condition that causes high blood pressure during pregnancy. Therefore, this response is irrelevant and inaccurate.
Choice D) Abruptio placentae is correct because this is a probable complication for a client who has gestational hypertension and reports continuous abdominal pain and vaginal bleeding. Abruptio placentae is a condition where the placenta separates from the uterine wall before delivery, causing hemorrhage and hypoxia for the mother and the baby. It can cause severe, constant abdominal pain, dark red bleeding, uterine tenderness or rigidity, fetal distress or demise, or maternal shock or coagulopathy. It can be triggered by gestational hypertension, which is a condition that causes high blood pressure during pregnancy and increases the risk of placental abruption by 25%. Therefore, this response is relevant and accurate.

A first-time father is changing the diaper of his 1-day-old daughter. He asks the nurse, "What is this black, sticky stuff in her diaper?" The nurse's best response is:
Explanation
Choice A) "Oh, don't worry about that. It's okay." is incorrect because this is not a helpful or informative response for a first-time father who is changing the diaper of his 1-day-old daughter. This response does not explain what the black, sticky stuff in the diaper is, why it is there, or how long it will last. It also does not address the father's concern or curiosity, and may make him feel dismissed or ignored. Therefore, this response is inadequate and inappropriate.
Choice B) "That's meconium, which is your baby's first stool. It's normal." is correct because this is a clear and accurate response for a first-time father who is changing the diaper of his 1-day-old daughter. This response explains what the black, sticky stuff in the diaper is, which is meconium. Meconium is a substance that consists of amniotic fluid, mucus, bile, and other waste products that accumulate in the baby's intestines before birth. It is usually passed within the first 24 to 48 hours after birth, and then replaced by transitional or regular stools. Meconium has a dark green or black color and a thick, sticky consistency. It does not have any odor or bacteria. It is normal and harmless for most babies, unless they inhale it during delivery, which can cause breathing problems or infection. Therefore, this response reassures and educates the father about his baby's condition.
Choice C) "That's transitional stool." is incorrect because this is not a true or complete response for a first-time father who is changing the diaper of his 1-day-old daughter. This response does not identify what the black, sticky stuff in the diaper is, which is meconium. Transitional stool is a type of stool that appears after meconium and before regular stools. It usually occurs between the second and fifth day after birth, and then changes to yellow or brown stools. Transitional stool has a greenish-brown color and a loose, seedy consistency. It may have some odor or bacteria. It indicates that the baby's digestive system is maturing and adapting to breast milk or formula. Therefore, this response confuses and misleads the father about his baby's condition.
Choice D) "That means your baby is bleeding internally." is incorrect because this is not a valid or appropriate response for a first-time father who is changing the diaper of his 1-day-old daughter. This response does not describe what the black, sticky stuff in the diaper is, which is meconium. Bleeding internally means that blood vessels are damaged or ruptured inside the body, causing blood loss and shock. This can be caused by various factors such as trauma, infection, clotting disorder, or medication. Bleeding internally can manifest as blood in the stool, urine, vomit, or saliva. However, it does not cause black, sticky stools like meconium. Moreover, this response scares and alarms the father without any evidence or reason. Therefore, this response is false and unethical.
Sign Up or Login to view all the 45 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

