ATI Maternity Exam 3
Total Questions : 55
Showing 25 questions, Sign in for moreThe primary factor that differentiates eclampsia from preeclampsia is:
Select one:
Explanation
Choice A Reason: Pulmonary edema is a condition where fluid accumulates in the lungs, causing shortness of breath and difficulty breathing. It can occur in preeclampsia due to increased blood pressure and fluid retention, but it is not a definitive sign of eclampsia.
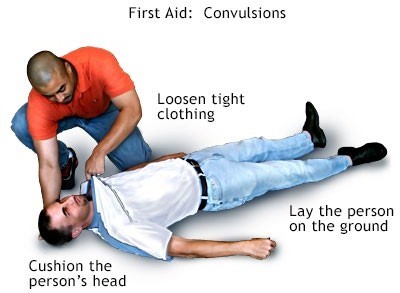
Choice B Reason: Convulsion (seizure) is a sudden, involuntary contraction of muscles that can cause loss of consciousness, shaking, and twitching. It is the main symptom of eclampsia and distinguishes it from preeclampsia.
Choice C Reason: Renal failure is a condition where the kidneys fail to filter waste products from the blood, resulting in high levels of creatinine and urea. It can occur in preeclampsia due to reduced blood flow to the kidneys, but it is not a specific indicator of eclampsia.
Choice D Reason: Retinal edema is a condition where fluid leaks into the retina, causing blurred vision and flashes of light. It can occur in preeclampsia due to increased blood pressure and damage to the blood vessels in the eye, but it is not a characteristic feature of eclampsia.
The nurse at a shelter is counseling a group of women experiencing domestic violence. What is most important for the nurse to emphasize?
Select one:
Explanation
Choice A Reason: About 1 of every 5 women will experience abuse in her lifetime is a statistic that shows the prevalence of domestic violence, but it does not address the question of what the nurse should emphasize to the group of women.
Choice B Reason: When women go back to the situation after the abuser has calmed down, things will be beter is a false statement that reflects the cycle of abuse, where the abuser may apologize and promise to change after a violent episode, but then repeat the same behavior later. This does not help the women understand their situation or seek help.
Choice C Reason: The victimized woman can easily leave the situation is a false statement that ignores the many barriers and challenges that women face when trying to escape from domestic violence, such as fear, isolation, financial dependence, lack of support, legal issues, and threats from the abuser. This does not empower the women or provide them with realistic options.
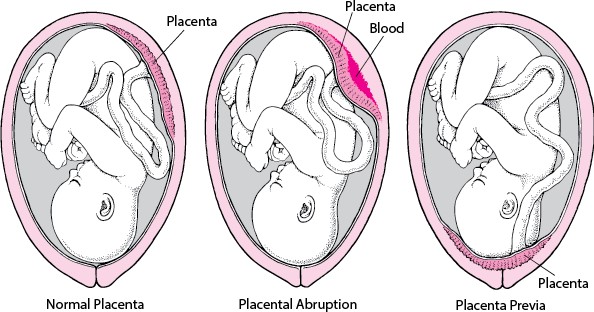
Choice D Reason: The violence will not stop or decrease if the woman becomes pregnant is a true statement that highlights the danger of staying in an abusive relationship during pregnancy. Domestic violence can increase the risk of miscarriage, preterm birth, low birth weight, placental abruption, fetal injury, and maternal death. This may motivate the women to seek safety and protection for themselves and their unborn children.
At 22 weeks' gestation, a client is diagnosed with placenta previa. The doctor tells the client that the placenta may move away from the cervix as the pregnancy progresses. This is classified as what type of previa?
Explanation
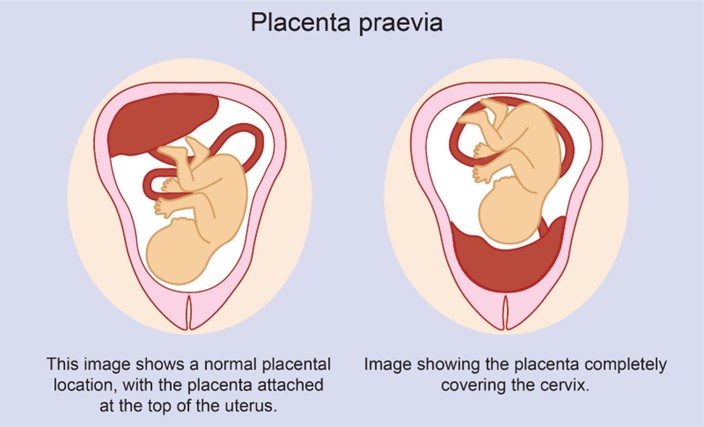
Choice A Reason: Partial placenta previa is a condition where the placenta partially covers the cervix. It usually does not resolve and may cause bleeding and complications during labor and delivery.
Choice B Reason: Complete placenta previa is a condition where the placenta completely covers the cervix. It is a serious condition that requires cesarean delivery and may cause life-threatening hemorrhage.
Choice C Reason: Marginal placenta previa is a condition where the edge of the placenta reaches the margin of the cervix. It may also cause bleeding and complications during labor and delivery.
Choice D Reason: Low-lying placenta previa is a condition where the placenta is near the cervix, but not covering it. It may resolve spontaneously as the uterus grows and the placenta moves upward.
A client who is breastfeeding her newborn tells the nurse, "I notice that when I feed him, I feel fairly strong contraction-like pain. Labor is over. Why am I having contractions now?" Which response by the nurse would be most appropriate?
Select one:
Explanation
Choice A Reason: "Your body is responding to the events of labor, just like after a tough workout." This is an inaccurate statement that does not explain the cause of the contractions or reassure the client.
Choice B Reason: "This could be a sign that your body is trying to get rid of retained placental fragments." This is an alarming statement that may scare the client and imply that something is wrong. Retained placental fragments are rare and usually cause heavy bleeding, fever, and infection.
Choice C Reason: "Let me check your vaginal discharge just to make sure everything is fine." This is an unnecessary statement that does not answer the client's question or provide any information.
Choice D Reason:"The baby's sucking releases oxytocin which causes your uterus to contract." This is a correct statement that explains the physiological mechanism of the contractions and reassures the client that they are normal and beneficial.
A couple who has had difficulty conceiving confides in the nurse at the infertility clinic that they feel overwhelmed with the decisions that face them. Which of the following nursing strategies would be most appropriate and therapeutic?
Select one:
Explanation
Choice A Reason: Provide compassionate and accurate information throughout the process and support them to make their own decisions. This is a therapeutic strategy that demonstrates empathy, honesty, and advocacy for the couple. It also helps them understand their options, risks, benefits, and alternatives, and encourages them to participate in their care.
Choice B Reason: Inquire about the names they have chosen for their baby to get their mind off their stress. This is a non-therapeutic strategy that avoids addressing the couple's concerns, minimizes their feelings, and may create false hope or unrealistic expectations.
Choice C Reason: Express sympathy and provide directive advice to the couple about what they should do. This is a non-therapeutic strategy that shows pity, imposes personal values, and undermines the couple's self-determination.
Choice D Reason: Refer them to a marriage counselor in the same building to help them with the decisions. This is a non-therapeutic strategy that implies that the couple has marital problems, shifts responsibility, and may create resentment or resistance.
The nurse administers vitamin K intramuscularly as prophylaxis to the newborn based on which of the following rationales?
Select one:
Explanation
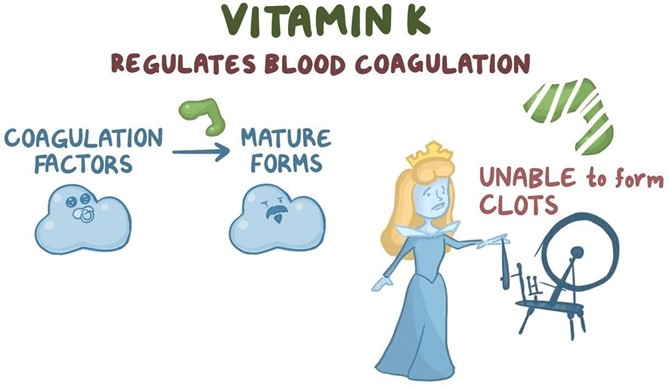
Choice A Reason: Vitamin K will increase erythropoiesis. This is an incorrect statement that confuses vitamin K with erythropoietin. Erythropoietin is a hormone that stimulates red blood cell production in the bone marrow. Vitamin K does not affect erythropoiesis.
Choice B Reason: Vitamin K will enhance bilirubin breakdown. This is an incorrect statement that confuses vitamin K with phototherapy. Phototherapy is a treatment that exposes the newborn's skin to light, which converts bilirubin into water-soluble forms that can be excreted by the liver and kidneys. Bilirubin is a yellow pigment that results from the breakdown of red blood cells. High levels of bilirubin can cause jaundice and brain damage in newborns. Vitamin K does not affect bilirubin metabolism.
Choice C Reason: Vitamin K will stop Rh sensitization. This is an incorrect statement that confuses vitamin K with Rh immune globulin. Rh immune globulin is an injection given to Rh-negative mothers who deliver Rh-positive babies, to prevent them from developing antibodies against Rh-positive blood cells in future pregnancies. Rh sensitization is a condition where the mother's immune system atacks the baby's blood cells, causing hemolytic disease of the newborn. Vitamin K does not affect Rh sensitization.
Choice D Reason: Vitamin K will promote blood clotting ability. This is a correct statement that explains the rationale for administering vitamin K as prophylaxis to newborns. Vitamin K is essential for the synthesis of clotting factors in the liver. Newborns have low levels of vitamin K at birth due to poor placental transfer and lack of intestinal bacteria that produce vitamin K. Therefore, they are at risk of bleeding disorders such as hemorrhagic disease of the newborn.
The nurse, working in labor and delivery, performs a sterile vaginal exam on a laboring woman. During the exam, she feels a loop of pulsating cord in the vagina. The nurse would anticipate:
Select one:
Explanation
Choice A Reason: Continuing to monitor and document fetal heart rate. This is an inadequate response that does not address the urgency of the situation or intervene to prevent fetal distress or demise.
Choice B Reason: Changing the mother's position to left lateral and giving oxygen by nasal cannula. This is a partial response that may improve maternal-fetal blood flow and oxygenation, but it does not resolve the cord compression or facilitate delivery.
Choice C Reason: With a sterile glove, maintaining pressure to lift the presenting part and emergently notifying the provider for a STAT C-section. This is an appropriate response that aims to reduce the cord compression by elevating the fetal head away from the cord and prepare for an immediate cesarean delivery.
Choice D Reason: Bolusing the patient with 1000cc lactated ringers. This is an irrelevant response that does not address the cause of the problem or improve fetal outcome.
The nurse at a shelter is counseling a group of women experiencing domestic violence. What is most important for the nurse to emphasize?
Select one:
Explanation
Choice A Reason: About 1 of every 5 women will experience abuse in her lifetime is a statistic that shows the prevalence of domestic violence, but it does not address the question of what the nurse should emphasize to the group of women.
Choice B Reason: When women go back to the situation after the abuser has calmed down, things will be beter is a false statement that reflects the cycle of abuse, where the abuser may apologize and promise to change after a violent episode, but then repeat the same behavior later. This does not help the women understand their situation or seek help.
Choice C Reason: The victimized woman can easily leave the situation is a false statement that ignores the many barriers and challenges that women face when trying to escape from domestic violence, such as fear, isolation, financial dependence, lack of support, legal issues, and threats from the abuser. This does not empower the women or provide them with realistic options.
Choice D Reason: The violence will not stop or decrease if the woman becomes pregnant is a true statement that highlights the danger of staying in an abusive relationship during pregnancy. Domestic violence can increase the risk of miscarriage, preterm birth, low birth weight, placental abruption, fetal injury, and maternal death. This may motivate the women to seek safety and protection for themselves and their unborn children.
Obstetrical risks to consider for a pregnant teenager would be all of the following, EXCEPT: Select one:
Explanation
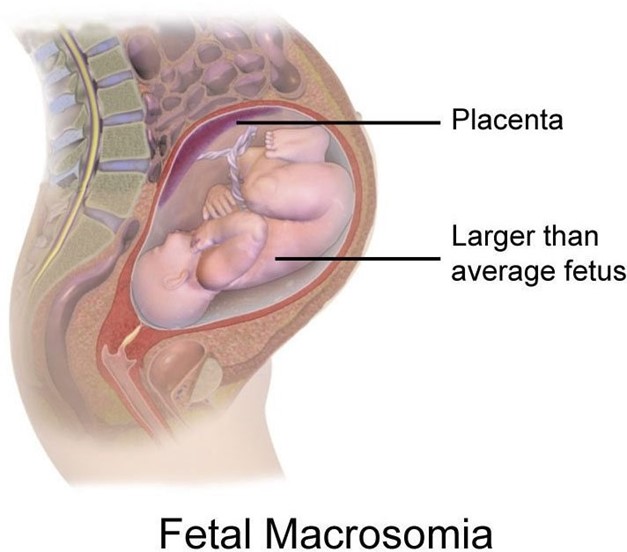
Choice A Reason: Macrosomic fetus is a fetus that weighs more than 4000 grams or 8 pounds 13 ounces at birth. It is not a common complication of teenage pregnancy, but rather of maternal diabetes, obesity, or a history of large babies.
Choice B Reason: Preeclampsia is a condition characterized by high blood pressure and proteinuria in pregnancy. It can cause serious complications for both the mother and the baby, such as seizures, organ damage, growth restriction, and placental abruption. Teenage pregnancy is a risk factor for preeclampsia, especially if the mother is younger than 15 years old.
Choice C Reason: Inadequate nutritional status of mother is a condition where the mother does not consume enough calories, protein, vitamins, minerals, or fluids during pregnancy. It can affect the growth and development of the baby and increase the risk of low birth weight, preterm birth, and birth defects. Teenage pregnancy is a risk factor for inadequate nutritional status of mother, as teenagers may have poor dietary habits, eating disorders, or limited access to food.
Choice D Reason: Cephalopelvic disproportion is a condition where the size or shape of the baby's head or body is too large to fit through the mother's pelvis. It can prevent normal vaginal delivery and require cesarean section. Teenage pregnancy is a risk factor for cephalopelvic disproportion, as teenagers may have smaller or immature pelvises that are not fully developed.
The parents of a newborn who is being treated for bacterial septicemia ask the nurse why their baby didn't seem very ill. The best response of the nurse is:
Select one:
Explanation
Choice A Reason: "You would have seen more symptoms if you had been looking more closely at your baby." This is an inappropriate response that blames the parents for missing the signs of sepsis and does not explain the Reason for the subtle symptoms.
Choice B Reason: "A newborn's immune system isn't mature, so symptoms are subtle and can be hard to recognize." This is an appropriate response that educates the parents about the immunological basis of sepsis in newborns and reassures them that they are not at fault for not noticing the symptoms.
Choice C Reason: "A high fever will always be present in sick newborns, including your baby." This is an incorrect response that contradicts the fact that newborns may not develop fever in response to infection due to their immature immune systems.
Choice D Reason: "A mother's immunity usually protects the infant from illness, but not in this case." This is an inaccurate response that implies that the mother failed to provide adequate immunity to her baby and does not address the question of why the baby did not seem very ill.
A woman has just entered the third stage of labor. The nurse would focus care on which of the following? Select one:
Explanation
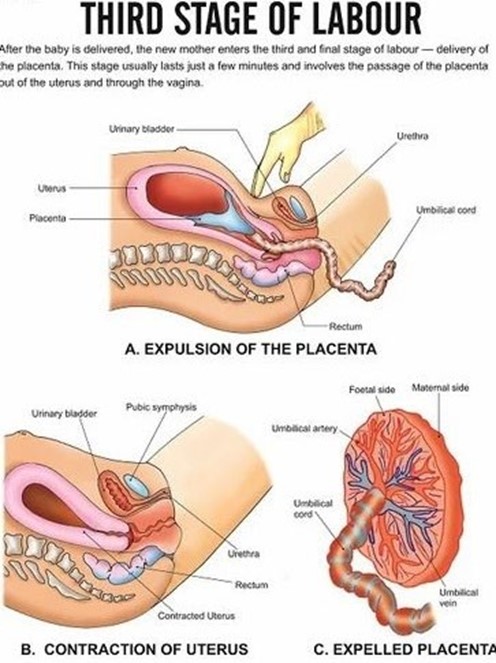
Choice A Reason: Assisting with the delivery of the placenta and ensuring that the fundus is contracted afterward. This is an appropriate action for the nurse to perform during the third stage of labor, as it helps complete the process of labor and prevent complications.
Choice B Reason: Palpating the woman's fundus for position and firmness. This is an action that is done after the delivery of the placenta, not during. It is important to monitor the fundal height, location, and consistency to assess uterine involution and bleeding.
Choice C Reason: Encouraging the woman to push with her contractions. This is an action that is done during the second stage of labor, not the third. The second stage of labor is the period from full cervical dilation to the birth of the baby. The nurse's role is to support and coach the woman to push effectively with her contractions.
Choice D Reason: Alleviating perineal discomfort with the application of ice packs. This is an action that is done after the delivery of the placenta, not during. It is a comfort measure that can reduce swelling, pain, and inflammation in the perineal area.
During an observational experience in labor and delivery, the student nurse recognizes that thick meconium is present in the amniotic fluid. Upon delivery of the newborn, the student nurse understands that there are signs that indicate that the newborn will need resuscitation. These signs are:
Select one:
Explanation
Choice A Reason: Central cyanosis and poor tone. These are signs of hypoxia and asphyxia in newborns, which indicate a need for resuscitation. Central cyanosis means bluish discoloration of the skin or mucous membranes around the mouth, nose, or eyes. Poor tone means limpness or lack of muscle activity.
Choice B Reason: Heart rate of 160 beats per minute and spitting up mucus. These are not signs of hypoxia or asphyxia in newborns, but rather normal findings or minor issues. A normal heart rate for a newborn ranges from 120 to 160 beats per minute. Spitting up mucus may be due to excess secretions or swallowing amniotic fluid, which can be cleared by suctioning or burping.
Choice C Reason: Crying with respirations of greater than 60 breaths per minute. These are not signs of hypoxia or asphyxia in newborns, but rather normal or expected findings. Crying indicates that the newborn has a patent airway and adequate lung expansion. Respirations of greater than 60 breaths per minute may be normal for a newborn in transition or due to transient tachypnea, which usually resolves within a few hours.
Choice D Reason: Blue hands and feet but lips that are slowly pinking up. These are not signs of hypoxia or asphyxia in newborns, but rather a common condition called acrocyanosis. Acrocyanosis means bluish discoloration of the hands and feet due to poor peripheral circulation in response to cold exposure or stress. It does not affect oxygenation or ventilation and usually disappears within 24 to 48 hours after birth.
Why is it important for the nurse to assess the bladder regularly and encourage the laboring client to void every 2 hours?
Select one:
Explanation
Choice A Reason: Frequent voiding encourages sphincter control. This is an incorrect statement that has no relevance to labor and delivery. Sphincter control refers to the ability to contract and relax the muscles that control urination and defecation. It is not affected by frequent voiding.
Choice B Reason: A full bladder impedes oxygen flow to the fetus. This is an incorrect statement that confuses a full bladder with a prolapsed cord. A prolapsed cord is a condition where the umbilical cord slips through the cervix before the baby and becomes compressed by the fetal head, which can reduce oxygen flow to the fetus. A full bladder does not affect oxygen flow to the fetus.
Choice C Reason: Frequent voiding prevents bruising of the bladder. This is an incorrect statement that exaggerates the effect of a full bladder on the bladder wall. A full bladder may cause some pressure or discomfort on the bladder, but it does not cause bruising or damage.
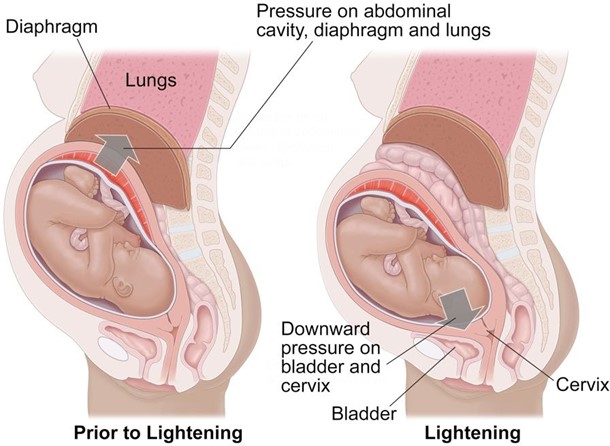
Choice D Reason: A full bladder can impede fetal descent. This is a correct statement that explains why it is important for the nurse to assess the bladder regularly and encourage the laboring client to void every 2 hours.
The nurse assesses a newborn at 36 weeks' gestation, and the following behaviors are noted: nasal flaring, labored breathing, and excessive mucus. The nurse is most concerned about:
Select one:
Explanation
Choice A Reason: Possible Meconium Aspiration Syndrome (MAS). This is an unlikely condition for this newborn, as MAS occurs when fetal stool (meconium) enters into the lungs before or during birth, causing airway obstruction, inflammation, and infection. MAS usually affects term or post-term infants who experience fetal distress or hypoxia in utero.
Choice B Reason: Possible polycythemia. This is an unrelated condition for this newborn, as polycythemia refers to an abnormally high number of red blood cells in the blood, which can increase blood viscosity and impair circulation.
Polycythemia may occur in infants who have delayed cord clamping, intrauterine growth restriction, maternal diabetes, or high altitude exposure.
Choice C Reason: Possible Transient Tachypnea of the Newborn (TTN). This is a less serious condition than RDS, as TTN is a mild respiratory problem that results from delayed clearance of fetal lung fluid after birth. TTN causes rapid breathing, nasal flaring, grunting, and mild cyanosis. It usually resolves within 24 to 48 hours after birth.
Choice D Reason: Possible Respiratory Distress Syndrome (RDS). This is a serious condition that requires immediate intervention and treatment, as RDS can lead to life-threatening complications such as pulmonary hemorrhage, pneumothorax, or bronchopulmonary dysplasia. RDS causes respiratory distress, nasal flaring, retractions, grunting, and central cyanosis. It usually occurs within minutes to hours after birth.
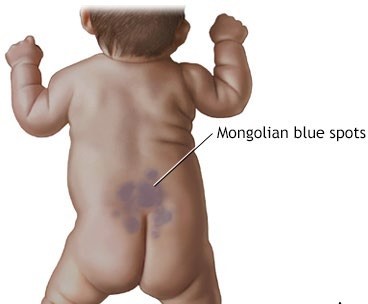
During a physical assessment of a newborn, the nurse observes bluish markings across the newborn's lower back. The nurse interprets this finding as:
Select one:
Explanation
Choice A Reason: Milia. This is an incorrect answer that describes a different skin condition. Milia are tiny white or yellow cysts that appear on the nose, chin, or cheeks of newborns. They are caused by the retention of keratin in the sebaceous glands or hair follicles. They usually disappear within a few weeks without treatment.
Choice B Reason: Dermal melanosis. This is a correct answer that explains the finding of bluish markings across the newborn's lower back. Dermal melanosis. This is because dermal melanosis, also known as Mongolian spots, is a common benign skin condition that affects newborns of Asian, African, or Hispanic descent. It is characterized by bluish-gray or brown patches of pigmentation on the lower back, butocks, or extremities. It is caused by the migration of melanocytes from the neural crest to the dermis during embryonic development. It usually fades by 2 to 4 years of age.
Choice C Reason: Stork bites. This is an incorrect answer that refers to another skin condition. Stork bites, also known as salmon patches or nevus simplex, are flat pink or red marks that appear on the forehead, eyelids, nose, upper lip, or nape of the neck of newborns. They are caused by dilated capillaries in the superficial dermis. They usually fade by 18 months of age.
Choice D Reason: Birth trauma. This is an incorrect answer that implies an injury or damage to the newborn's skin or tissues during labor and delivery. Birth trauma can cause bruises, abrasions, lacerations, fractures, or nerve injuries. It is not related to bluish markings on the lower back.
Post-term fetal risks include all of the following, EXCEPT: Select one:
Explanation
Choice A Reason: Macrosomic newborn. This is a correct answer that describes a possible complication of post-term pregnancy. A macrosomic newborn is a newborn that weighs more than 4000 grams or 8 pounds 13 ounces at birth. It can occur in post-term pregnancies due to prolonged exposure to maternal glucose and insulin. It can increase the risk of birth injuries, shoulder dystocia, cesarean delivery, and hypoglycemia.
Choice B Reason: Intrauterine growth restriction (IUGR). This is a correct answer that indicates a potential problem of post-term pregnancy. IUGR is a condition where the fetal growth is slower than expected for gestational age. It can occur in post-term pregnancies due to placental insufficiency, aging, or calcification, which can impair nutrient and oxygen delivery to the fetus. It can increase the risk of fetal distress, hypoxia, acidosis, and stillbirth.
Choice C Reason: Umbilical cord prolapse. This is an incorrect answer that does not reflect a risk of post-term pregnancy, but rather a risk of other factors such as prematurity, low birth weight, breech presentation, multiple gestation, polyhydramnios, or artificial rupture of membranes.
Choice D Reason: Meconium Aspiration Syndrome (MAS). This is a correct answer that denotes a possible complication of post-term pregnancy. MAS occurs when fetal stool (meconium) enters into the lungs before or during birth, causing airway obstruction, inflammation, and infection. MAS usually affects term or post-term infants who experience fetal distress or hypoxia in utero. It can cause respiratory distress syndrome (RDS), persistent pulmonary hypertension (PPHN), or chronic lung disease (CLD).
A woman with a history of crack cocaine use is admited to the Labor and Birthing Unit. While caring for the patient, the nurse notes a sudden onset of fetal bradycardia. The patient also complains of acute abdominal pain that is continuous and she has dark red vaginal bleeding. Which of the following would the nurse suspect?
Select one:
Explanation
Choice A Reason: Shoulder dystocia. This is an incorrect answer that describes a different obstetric complication. Shoulder dystocia is a condition where the baby's shoulder gets stuck behind the mother's pubic bone during delivery, which can cause nerve injury, fracture, or asphyxia to the baby. Shoulder dystocia does not cause fetal bradycardia, abdominal pain, or vaginal bleeding.
Choice B Reason: Placental abruption. This is a correct answer that explains the symptoms of fetal bradycardia, abdominal pain, and vaginal bleeding in a woman with a history of crack cocaine use. Placental abruption. This is because placental abruption is a condition where the placenta separates from the uterine wall before delivery, which can cause fetal distress, maternal hemorrhage, and shock. Placental abruption can be triggered by maternal hypertension, trauma, or substance abuse, such as crack cocaine.
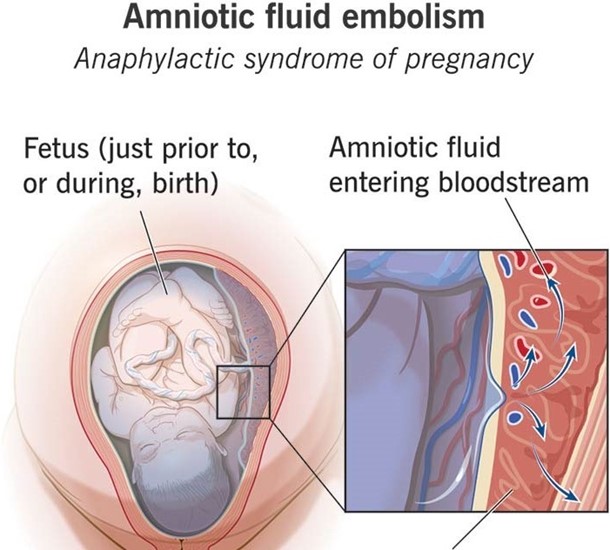
Choice C Reason: Anaphylactoid syndrome of pregnancy. This is an incorrect answer that refers to a rare and fatal condition also known as amniotic fluid embolism. Anaphylactoid syndrome of pregnancy is a condition where amniotic fluid enters into the maternal bloodstream and causes an allergic reaction, which can lead to respiratory failure, cardiac arrest, coagulopathy, and coma. Anaphylactoid syndrome of pregnancy does not cause fetal bradycardia or vaginal bleeding.
Choice D Reason: Placenta previa. This is an incorrect answer that indicates another placental disorder. Placenta previa is a condition where the placenta covers or is near the cervix, which can cause painless bright red bleeding during pregnancy or labor. Placenta previa does not cause fetal bradycardia or abdominal pain.
The nurse assesses a 1-day-old newborn. Which finding indicates that the newborn's oxygenation needs are not being met?
Select one:
Explanation
Choice A Reason: Grunting and nasal flaring. These are signs of respiratory distress in newborns, which indicate that their oxygenation needs are not being met. Grunting and nasal flaring. This is because grunting and nasal flaring are signs of respiratory distress in newborns, which indicate inadequate oxygenation and ventilation. Grunting is a noise made by the newborn when exhaling, which reflects an atempt to keep the alveoli open and increase lung volume.
Nasal flaring is a widening of the nostrils when inhaling, which reflects an effort to reduce airway resistance and increase airflow.
Choice B Reason: Acrocyanosis. This is not a sign of respiratory distress in newborns, but rather a common condition called acrocyanosis. Acrocyanosis means bluish discoloration of the hands and feet due to poor peripheral circulation in response to cold exposure or stress. It does not affect oxygenation or ventilation and usually disappears within 24 to 48 hours after birth.
Choice C Reason: Abdominal breathing. This is not a sign of respiratory distress in newborns, but rather a normal patern of breathing for them. Abdominal breathing means that the newborn's abdomen rises and falls with each breath, which reflects the use of the diaphragm as the primary respiratory muscle.
Choice D Reason: Respiratory rate of 54 breaths/minute. This is not a sign of respiratory distress in newborns, but rather a normal range of respiratory rate for them. A normal respiratory rate for a newborn ranges from 40 to 60 breaths per minute.
A woman who is 12 hours postpartum had a pulse rate around 80 beats per minute during pregnancy. Now, the nurse finds a pulse of 60 beats per minute. Which of these actions should the nurse take?
Select one:
Explanation
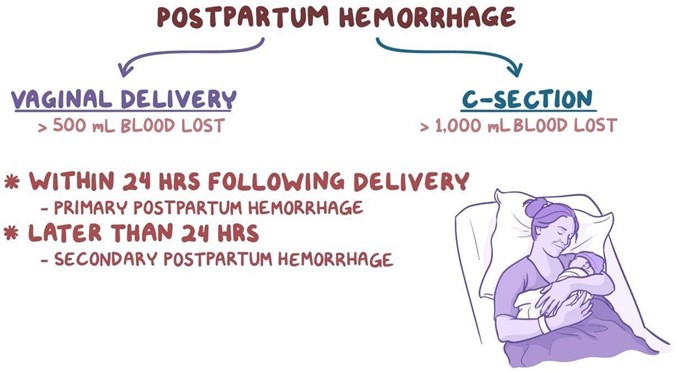
Choice A Reason: Contact the physician, as it indicates early DIC. This is an incorrect answer that confuses a low pulse rate with a high pulse rate. DIC stands for disseminated intravascular coagulation, which is a life-threatening condition where abnormal clotting and bleeding occur simultaneously in the body. DIC can occur as a complication of postpartum hemorrhage, infection, or placental abruption. DIC can cause tachycardia (high pulse rate), not bradycardia (low pulse rate).
Choice B Reason: Contact the physician, as it is a first sign of postpartum eclampsia. This is an incorrect answer that misinterprets a low pulse rate as a sign of hypertension. Postpartum eclampsia is a condition where seizures occur in a woman who has preeclampsia or eclampsia after delivery. Preeclampsia and eclampsia are characterized by high blood pressure and proteinuria in pregnancy. Postpartum eclampsia can cause hypertension (high blood pressure), not hypotension (low blood pressure).
Choice C Reason: Document the finding as it is a normal finding at this time. This is because a pulse rate of 60 beats per minute is within the normal range for an adult and may reflect a physiological adaptation to the postpartum period. During pregnancy, the maternal blood volume and cardiac output increase, which can elevate the pulse rate. After delivery, these parameters gradually return to pre-pregnancy levels, which can lower the pulse rate.
Choice D Reason: Obtain an order for a CBC, as it suggests postpartum anemia. This is an incorrect answer that assumes that a low pulse rate is caused by anemia. Anemia is a condition where the red blood cell count or hemoglobin level is lower than normal, which can impair oxygen delivery to the tissues. Anemia can occur in the postpartum period due to blood loss during delivery or poor nutritional intake during pregnancy. Anemia can cause tachycardia (high pulse rate), not bradycardia (low pulse rate).

A woman is at 32 weeks' gestation. Her fundal height measurement at this clinic appointment is 26 centimeters. After reviewing her ultrasound results, the health care provider asks the nurse to schedule the client for a series of ultrasounds to be done every 2 weeks. The nurse should ensure that the client understands that the main purpose for this is to:
Select one:
Explanation
Choice A Reason: Rule out a suspected hydatidiform mole. This is an incorrect answer that describes an unlikely condition for this client. A hydatidiform mole is a type of gestational trophoblastic disease where abnormal placental tissue develops instead of a normal fetus. A hydatidiform mole can cause vaginal bleeding, hyperemesis gravidarum (severe nausea and vomiting), preeclampsia, and hyperthyroidism. A hydatidiform mole usually causes a fundal height measurement that is larger than expected for gestational age, not smaller.
Choice B Reason: Assess for congenital anomalies. This is an incorrect answer that implies that the client has not had a previous ultrasound to screen for fetal anomalies. Congenital anomalies are structural or functional defects that are present at birth, such as cleft lip, spina bifida, or Down syndrome. Ultrasound can detect some congenital anomalies by visualizing the fetal anatomy and morphology. However, ultrasound screening for fetal anomalies is usually done between 18 and 22 weeks of gestation, not at 32 weeks.
Choice C Reason: Determine fetal presentation. This is an incorrect answer that suggests that the client has an uncertain fetal presentation. Fetal presentation is the part of the fetus that is closest to the cervix, such as vertex (head), breech (butocks or feet), or transverse (shoulder). Fetal presentation can affect the mode and outcome of delivery. Ultrasound can determine fetal presentation by locating the fetal head and spine. However, fetal presentation can also be assessed by abdominal palpation or vaginal examination, which are simpler and less invasive methods.
Choice D Reason: Monitor fetal growth. This is because fundal height measurement is a method of estimating fetal size and gestational age by measuring the distance from the pubic symphysis to the top of the uterus (fundus) in centimeters. A fundal height measurement that is significantly smaller or larger than expected for gestational age may indicate intrauterine growth restriction (IUGR) or macrosomia, respectively. IUGR means that the fetal growth is slower than expected for gestational age, which can increase the risk of fetal distress, hypoxia, acidosis, and stillbirth. Macrosomia means that the fetal weight is higher than expected for gestational age, which can increase the risk of birth injuries, shoulder dystocia, cesarean delivery, and hypoglycemia. Ultrasound is a more accurate way of assessing fetal size and growth by measuring various parameters such as biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC), and femur length (FL). Ultrasound can also detect other factors that may affect fetal growth such as placental function, amniotic fluid volume, umbilical cord blood flow, and fetal anomalies.
The nurse's initial action when caring for an otherwise stable, full term infant with a slightly decreased temperature is to:
Select one:
Explanation
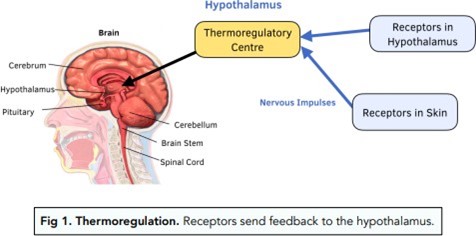
Choice A Reason: Place the infant skin to skin with the mother and re-check temperature in 30 minutes. This is because skin-to-skin contact is an effective and safe method of increasing the infant's temperature and promoting thermoregulation. Skin-to-skin contact also has other benefits such as enhancing bonding, breastfeeding, and maternal-infant attachment.
Choice B Reason: Check the infant's CBC and blood cultures, as this is a sign of probable sepsis. This is an unnecessary action that may cause undue stress and discomfort to the infant and the mother. A slightly decreased temperature in a full-term infant is not a sign of probable sepsis, but rather a common finding that may be due to environmental factors, such as exposure to cold air or wet linens.
Choice C Reason: Return the infant to the nursery for close observation under warming lights. This is an undesirable action that may interfere with the early initiation of breastfeeding and bonding between the mother and the infant. Warming lights are not recommended for routine use in healthy newborns, as they may cause dehydration, hyperthermia, or eye damage.
Choice D Reason: Notify the physician immediately and suggest orders for placement in an incubator. This is an excessive action that may indicate a lack of knowledge or confidence on the part of the nurse. An incubator is not indicated for a stable, full term infant with a slightly decreased temperature, as it may expose the infant to unnecessary interventions, infections, or separation from the mother.
The client at 42 weeks' pregnancy is admited for induction of her labor. Which statement indicates that she understands the Reasons for the induction?
Select one:
Explanation
Choice A Reason: "If I go too long overdue, the amniotic fluid volume can become too low for my baby to be safe." This is a correct answer that indicates that the client understands one of the Reasons for induction of labor at 42 weeks' pregnancy.
Choice B Reason: "My baby took longer to grow, and now she's ready to be born." This is an incorrect answer that shows a misconception about fetal growth and development. Fetal growth does not depend on gestational age alone, but also on genetic, maternal, placental, and environmental factors. A post-term fetus does not necessarily grow faster or larger than a term fetus. In fact, some post-term fetuses may experience intrauterine growth restriction (IUGR), which means slower than expected growth for gestational age.
Choice C Reason: "I don't really need this induction, my baby will come whenever he wants to." This is an incorrect answer that reveals a lack of awareness or acceptance of the need for induction of labor at 42 weeks' pregnancy. Induction of labor is recommended for post-term pregnancies to prevent potential complications such as fetal distress, stillbirth, or maternal hemorrhage.
Choice D Reason: "Since I am so tired of being pregnant, I am being induced." This is an incorrect answer that implies that induction of labor is based on maternal preference or convenience rather than medical indication. Induction of labor should not be done without a valid Reason or informed consent, as it carries some risks such as failed induction, prolonged labor, infection, uterine rupture, or cesarean delivery.
When the nurse is assessing a postpartum client approximately 6 hours after delivery, which finding would warrant further investigation?
Select one:
Explanation
Choice A Reason: Moderate amounts of deep red lochia. This is not a finding that would warrant further investigation, but rather a normal finding for the early postpartum period. Lochia is the vaginal discharge that occurs after delivery, which consists of blood, mucus, and tissue from the uterus. Lochia is usually deep red in color and moderate in amount for the first few days after delivery.
Choice B Reason: Sweating while afebrile. This is not a finding that would warrant further investigation, but rather a common occurrence in the postpartum period. Sweating is a mechanism of thermoregulation that helps the body eliminate excess fluid and electrolytes that were retained during pregnancy. Sweating does not necessarily indicate fever or infection.
Choice C Reason: Voiding 350 mL of blood-tinged urine. This is not a finding that would warrant further investigation, but rather an expected outcome for the postpartum period. Voiding large amounts of urine is normal in the postpartum period, as the body eliminates the excess fluid that was accumulated during pregnancy. Blood-tinged urine may be due to trauma or irritation of the urinary tract during labor or delivery, which usually resolves within a few days.
Choice D Reason: Heart rate of 115 beats/minute. This is because a heart rate of 115 beats/minute is higher than the normal range for an adult, which is 60 to 100 beats/minute. A high heart rate may indicate postpartum hemorrhage, infection, pain, anxiety, or dehydration. The nurse should further assess the client for other signs and symptoms of these conditions and notify the physician if necessary.
An adolescent patient at 20 weeks gestation states that it is important not to have a baby that weighs too much. She states this has been her rationale for limiting calories. Her weight has decreased from 110 pounds to 106 pounds.
What would be the best nursing response? Select one:
Explanation
Choice A Reason: "It's okay to want a small baby when you're a teen." This is an incorrect answer that validates the patient's misconception and reinforces her unhealthy behavior. It also implies that there is something wrong with having a normal-sized baby or being a teen mother.
Choice B Reason: "You shouldn't be worrying about your figure." This is an incorrect answer that dismisses the patient's feelings and concerns and may make her defensive or resistant to change. It also does not address the underlying issues or provide any guidance or support.
Choice C Reason: ""Your baby needs adequate nutrition to develop and to be healthy." This is because this response provides factual information and education to the patient about the importance of nutrition during pregnancy. It also conveys empathy and concern for both the mother and the baby without being judgmental or accusatory.
Choice D Reason: "You are causing harm to your baby." This is an incorrect answer that blames and criticizes the patient and may make her feel guilty or ashamed. It also does not offer any help or solutions for her situation.
Following a normal spontaneous vaginal delivery (NSVD), a 28 year old G3 now P3 mother develops sudden onset shortness of breath, hypoxia and cyanosis. The delivery room nurse quickly recognizes these symptoms as possible:
Select one:
Explanation
Choice A Reason: Manifestations of uteroplacental insufficiency. This is an incorrect answer that describes a different condition that affects the fetus, not the mother. Uteroplacental insufficiency is a condition where the placenta fails to deliver adequate oxygen and nutrients to the fetus, which can result in fetal growth restriction, distress, or demise. Uteroplacental insufficiency does not cause shortness of breath, hypoxia, or cyanosis in the mother.
Choice B Reason: Manifestations of prolapsed cord. This is an incorrect answer that refers to another condition that affects the fetus, not the mother. Prolapsed cord is a condition where the umbilical cord slips through the cervix before the baby and becomes compressed by the fetal head, which can reduce oxygen flow to the fetus. Prolapsed cord does not cause shortness of breath, hypoxia, or cyanosis in the mother.
Choice C Reason: Manifestations of anaphylactoid syndrome of pregnancy. This is because anaphylactoid syndrome of pregnancy, also known as amniotic fluid embolism, is a rare and fatal condition where amniotic fluid enters into the maternal bloodstream and causes an allergic reaction, which can lead to respiratory failure, cardiac arrest, coagulopathy, and coma. Anaphylactoid syndrome of pregnancy can occur during or after labor and delivery, especially in cases of NSVD, multiparity, advanced maternal age, or placental abruption.
Choice D Reason: Manifestations of an acute asthmatic episode. This is an incorrect answer that assumes that the mother has a history of asthma or an allergic trigger. Asthma is a chronic inflammatory disorder of the airways that causes wheezing, coughing, chest tightness, and dyspnea. Asthma can be exacerbated by pregnancy or labor, but it is not a common cause of sudden onset respiratory distress in the postpartum period.
Sign Up or Login to view all the 55 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

