ATI Maternity Exam - Exam 2
Total Questions : 68
Showing 25 questions, Sign in for moreA nurse is teaching a group of clients who are in their first trimester about exercise during pregnancy. Which of the following statements should the nurse include in the teaching?
Explanation
A. Incorrect. Weightbearing exercises should be avoided or limited during pregnancy, as they can increase the risk of injury, joint pain, and fatigue.
B. Correct. Moderate exercise can improve circulation, reduce swelling, and prevent varicose veins during pregnancy.
C. Incorrect. Resting for 30 minutes before each new exercise is not necessary and may reduce the benefits of physical activity.
D. Incorrect. Stretching exercises can help prevent muscle cramps, improve flexibility, and reduce back pain during pregnancy.
A nurse on the labor and delivery unit is caring for a patient who is having induction of labor with oxytocin administered through a secondary IV line. Uterine contractions occur every 2
minutes, last 90 seconds, and are strong to palpation. The baseline fetal heart rate is 150/minute, with uniform decelerations beginning at the peak of the contraction and a return to baseline after the contraction is over.
Which of the following actions should the nurse take?
Explanation
A. Incorrect. Increasing the rate of infusion of the IV oxytocin would worsen the uterine hyperstimulation and fetal distress that are indicated by the frequent, long, and strong contractions and uniform decelerations.
B. Correct. Discontinuing the infusion of the IV oxytocin would stop the uterine hyperstimulation and allow the fetus to recover from hypoxia.
C. Incorrect. Decreasing the rate of infusion of the maintenance IV solution would not affect the uterine hyperstimulation or fetal distress, as they are caused by the oxytocin, not by the fluid volume.
D. Incorrect. Slowing the client's rate of breathing would not help with the uterine hyperstimulation or fetal distress, as they are not related to maternal hyperventilation or respiratory alkalosis.
A nurse is providing teaching about expected gestational changes to a client who is at 12 weeks of gestation. Which of the following statements by the client indicates a need for further teaching?
Explanation
A. "I will monitor my weight gain during the remaining months."
Correct: Monitoring weight gain during pregnancy is an appropriate action as it helps to ensure the baby's growth and overall health.
B. "I will use only nonprescription medications while pregnant."
Incorrect: This statement indicates a need for further teaching. Nonprescription medications may not be safe during pregnancy, as some overthecounter drugs can potentially harm the
fetus. It's essential for pregnant women to consult their healthcare provider before taking any medications.
C. "I will tell my doctor before using home remedies for nausea."
Correct: This statement shows the client's understanding that it's important to consult with their healthcare provider before using any home remedies during pregnancy, as some
remedies may not be safe for the developing fetus.
D. "I will reduce my stress level."
Correct: Managing stress during pregnancy is beneficial for both the mother and the baby. It indicates a good understanding of selfcare during pregnancy.
A nurse is instructing a woman who is contemplating pregnancy about nutritional needs. To reduce the risk of giving birth to a newborn who has a neural tube defect, which of the following information should the nurse include in the teaching?
Explanation
A. "Increase your intake of ironrich foods and take a prenatal vitamin."
Important, but not directly related to reducing the risk of neural tube defects. Ironrich foods and prenatal vitamins are essential for overall maternal and fetal health, but they do not specifically target neural tube defect prevention.
B. "Avoid any alcohol consumption."
Important advice during pregnancy to prevent fetal alcohol spectrum disorders, but not directly related to reducing the risk of neural tube defects.
C. "Take a folic acid supplement for at least 3 months before you get pregnant."
Correct: Adequate folic acid intake before conception and during early pregnancy can significantly reduce the risk of neural tube defects in newborns.
D. "Avoid all foods containing aspartame."Aspartame is an artificial sweetener that has been studied for safety in pregnancy, and there is currently no strong evidence linking it to neural tube defects. However, it's still a good idea
to limit the intake of artificial sweeteners during pregnancy and focus on a balanced diet.
A nurse in a prenatal clinic is instructing a client about an amniocentesis, which is scheduled at 15 weeks of gestation. Which of the following should be included in the teaching?
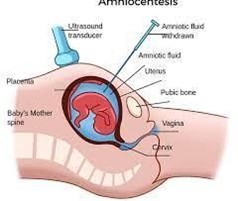
Explanation
A. "The test will be performed if your baby's heartbeat is heard."
Incorrect: Amniocentesis is not typically performed based on whether the baby's heartbeat is heard. It is done for specific diagnostic purposes, such as genetic testing or assessing certain fetal conditions.
B. "This test will determine if your baby's lungs are mature."
Incorrect: Amniocentesis does not determine fetal lung maturity. The test involves the extraction of a small amount of amniotic fluid to analyze fetal chromosomes and identify genetic conditions.
C. "After the test, you will be given Rh immune globulin since you are Rh positive."
Incorrect: Rh immune globulin (Rhogam) is given to Rhnegative pregnant women to prevent Rh sensitization, which occurs when an Rhnegative mother is exposed to
Rhpositive fetal blood. Rhogam is not directly related to amniocentesis.
D. "This test requires the presence of an adequate volume of amniotic fluid."
Correct: Amniocentesis requires a sufficient amount of amniotic fluid around the fetus for safe and accurate testing. If there is not enough amniotic fluid, the procedure may be postponed or canceled.
A nurse is preparing to measure the fundal height of a client who is at 22 weeks of gestation.
At which location should the nurse expect to palpate the fundus?
Explanation
A. 1 cm below the umbilicus: This is too low for a client at 22 weeks of gestation.
B. 3 cm below the umbilicus: This is also too low for a client at 22 weeks of gestation.
C. 2 cm above the umbilicus: At 22 weeks of gestation, the fundus should be palpated about 2 cm above the umbilicus, which is at approximately the level of the maternal belly button.
D. 3 cm above the umbilicus: This is too high for a client at 22 weeks of gestation.
A nurse is caring for a client who is at 6 weeks of gestation with her first pregnancy and asks the nurse when she can expect to experience quickening. Which of the following responses should the nurse make?
Explanation
A. "This always happens by the end of the first trimester of pregnancy.": Quickening typically occurs later in pregnancy, not by the end of the first trimester.
B. "This will occur during the last trimester of pregnancy.": Quickening occurs much earlier than the last trimester.
C. "This usually happens between the fourth and fifth months of pregnancy.": Quickening, which is the first perception of fetal movements by the mother, generally occurs between 16 to 20 weeks of gestation.
D. "This will happen once the uterus begins to rise out of the pelvis.": Quickening does not directly correlate with the rising of the uterus out of the pelvis.
A nurse in a prenatal clinic is caring for a client who is at 39 weeks of gestation and who asks about the signs that precede the onset of labor. Which of the following should the nurse identify as a sign that precedes labor?
Explanation
A. A surge of energy: Some women experience a sudden burst of energy, often referred to as a "nesting" instinct, shortly before the onset of labor.
B. Urinary retention: Urinary frequency and urgency are more common before labor, not urinary retention.
C. Decreased vaginal discharge: Before labor, there might be an increase in vaginal discharge, often thick and pinkish, known as the "bloody show."
D. Weight gain of 0.5 to 1.5 kg: Weight gain is not typically associated with the onset of labor.
A nurse is caring for a client following an amniotomy who is now in the active phase of the first stage of labor. Which of the following actions should the nurse implement with this client?
Explanation
A. Maintain the client in the lithotomy position: The lithotomy position is not typically
maintained during the active phase of labor. It is used during the pushing stage (second stage) of labor.
B. Encourage the client to empty her bladder every 2 hr: A full bladder can impede fetal descent and progress during labor, so encouraging the client to empty her bladder regularly is essential.
C. Remind the client to bear down with each contraction: Bearing down during the active phase of labor is not appropriate, as it may lead to premature pushing and cervical swelling.
D. Perform vaginal examinations frequently: Frequent vaginal examinations can increase the risk of infection and should be minimized during labor.
A nurse is caring for a client who is gravida 3, para 2, and is in active labor. The fetal head is at 3+ station after a vaginal examination. Which of the following actions should the nurse take?
Explanation
A. Observe for the presence of a nuchal cord: While this is important, it is not specifically related to the finding of the fetal head at a certain station.
B. Prepare to administer oxytocin: Oxytocin is a hormone used to induce or augment labor, but there is no indication for its use based solely on the fetal head station.
C. Observe for crowning: The fetal head at 3+ station indicates significant descent, and crowning may occur soon. Crowning is the appearance of the fetal head at the vaginal opening and indicates that delivery is imminent.
D. Apply fundal pressure: Fundal pressure is not appropriate at this stage of labor and could cause harm.
A nurse on the labor and delivery unit is caring for a client who is having a difficult, prolonged labor with severe backache. Which of the following contributing causes should the nurse identify?
Explanation
A. Fetal position is persistent occiput posterior: The occiput posterior position (the back of
the baby's head facing the mother's back) can lead to a more challenging and prolonged labor with intense back pain.
B. Fetal attitude is in general flexion: Flexion is the normal fetal attitude for birth and does not contribute to a difficult labor with backache.
C. Fetal lie is longitudinal: Longitudinal lie refers to the baby's position along the mother's spine, but it doesn't specify the position of the baby's back, so it is not directly related to backache.
D. Maternal pelvis is gynecoid: Gynecoid pelvis is the most favorable pelvis shape for childbirth, so it is not likely to cause difficult labor with severe backache.
A nurse is caring for a client who is in active labor and notes late decelerations on the fetal monitor. Which of the following is the priority nursing action?
Explanation
A. Position the client on her side: Late decelerations are often associated with uteroplacental insufficiency, which may be improved by changing the maternal position to improve blood flow to the placenta.
B. Elevate the client's legs: Elevating the client's legs would not directly address the cause of late decelerations.
C. Increase the infusion rate of the IV fluid: While ensuring adequate hydration is important, it is not the priority action when late decelerations are noted.
D. Administer oxygen via a face mask: Oxygen administration may be necessary, but it is not the priority action. Positioning the client on her side to improve blood flow is the priority.
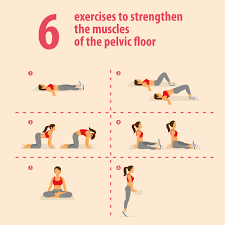
A nurse is providing teaching about Kegel exercises to a group of clients who are in the third trimester of pregnancy. Which of the following statements by a client indicates understanding of the teaching?
Explanation
Choice A: Kegel exercises are specifically designed to strengthen the pelvic floor muscles, which play a crucial role during childbirth. Strengthening these muscles can aid in better control during labor and delivery, facilitating stretching and reducing the risk of injury.
Choice B: Kegel exercises do not have a direct impact on preventing constipation during pregnancy. However, they may help improve bowel control and prevent fecal incontinence.
Choice C: While Kegel exercises can improve posture and core strength, their primary benefit lies in strengthening the pelvic muscles, not directly reducing backaches throughout pregnancy.
Choice D: Kegel exercises are not intended to prevent stretch marks on the abdomen. Stretch marks are caused by the stretching of the skin during pregnancy and are not related to pelvic muscle exercises.
A nurse is teaching a client who is at 23 weeks of gestation and will return to the facility in 2 days for an amniocentesis. Which of the following instructions should the nurse give the client?
Explanation
Choice A: Bowel prep protocols are not required for an amniocentesis procedure, as it involves sampling amniotic fluid from the uterus, not the bowel.
Choice B: Emptying the bladder before the procedure is important to improve comfort and minimize the risk of accidental puncture during the amniocentesis.
Choice C: It is essential to have a full bladder for some ultrasound procedures, but it is not necessary for an amniocentesis. A full bladder can help push the uterus upward and make it easier to visualize the fetus during the ultrasound, but it is not relevant to the amniocentesis procedure.
Choice D: Washing the abdomen with soap and water is not a required step for an amniocentesis procedure. The procedure involves sterile preparation of the abdomen using an antiseptic
solution.
A nurse in a provider's office is caring for a client who is at 36 weeks of gestation and scheduled for an amniocentesis. The client asks why she is having an ultrasound prior to the procedure. Which of the following is an appropriate response by the nurse?
Explanation
Choice A: An ultrasound can indeed determine the number of fetuses if a client is carrying multiples, but this is not the primary reason for performing an ultrasound before amniocentesis.
Choice B: An ultrasound is typically done before an amniocentesis to visualize the location of the placenta and fetus. This information is important to ensure that the amniocentesis needle is safely inserted away from the placenta and the fetus.
Choice C: The primary purpose of an amniocentesis is to obtain a sample of amniotic fluid to screen for genetic conditions, not specifically for spina bifida.
Choice D: Fetal age can be estimated through an ultrasound, but this is not the primary reason for performing an ultrasound before an amniocentesis. The main goal of the procedure is to obtain a sample of amniotic fluid for genetic testing.
A nurse is caring for a client who is in active labor and has just been examined as being at 7 cm of cervical dilation and 100% effacement. The fetus is at 1+ station, and the client's amniotic membranes are intact. The client suddenly states that she needs to push. Which of the following actions should the nurse take?
Explanation
Choice A: At 7 cm dilation, the client is in active labor, and assisting her into a more comfortable position may not be appropriate at this stage. It is essential to observe for signs of impending birth and assess the progress of labor.
Choice B: Feeling the urge to push may indicate that the baby is descending and the cervix is fully dilated. The nurse should immediately observe the perineum for signs of crowning (when the baby's head starts to appear at the vaginal opening) to prepare for delivery.
Choice C: If the client is feeling the urge to push and the cervix is fully dilated, panting or blowing through contractions will not be effective. It is important to allow the client to follow her body's natural urges to push.
Choice D: While emptying the bladder is generally recommended during labor to provide more room for the baby to descend, the client's current urge to push suggests that the baby is likely in a lower position, and it might not be safe or feasible to move the client to the bathroom.
A nurse is caring for a client who has a positive pregnancy test. The nurse is teaching the client about common discomforts in the first trimester of pregnancy as well as warning signs of potential danger. The nurse should instruct the client to call the clinic if she experiences which of the following manifestations?
Explanation
Choice A: Leukorrhea, which refers to an increase in vaginal discharge, is a common discomfort during pregnancy and is generally not a cause for concern.
Choice B: Painful and tender areas on the leg may be a sign of deep vein thrombosis (DVT), a potentially dangerous condition. During pregnancy, there is an increased risk of developing blood clots, and DVT can be a serious complication that requires immediate medical attention.
Choice C: Nausea and vomiting are common in early pregnancy and are usually associated with morning sickness. While it can be uncomfortable, it is generally not considered a dangerous symptom unless it leads to severe dehydration.
Choice D: Urinary frequency is a common discomfort during pregnancy, especially in the first and third trimesters. Although it can be bothersome, it is not typically a sign of immediate danger.
A nurse is caring for a client who is in the first stage of labor and is using patternpaced breathing. The client says she feels lightheaded, and her fingers are tingling. Which of the following actions should the nurse take?
Explanation
Choice A: The client's symptoms of lightheadedness and tingling fingers indicate that she may be hyperventilating, which can occur when patternpaced breathing is too rapid. Breathing into a paper bag can help the client rebreathe some of the exhaled carbon dioxide, which can help correct the respiratory alkalosis caused by hyperventilation.
Choice B: Administering oxygen via nasal cannula may not address the underlying issue of hyperventilation. It is more appropriate to assist the client in slowing down her breathing pattern.
Choice C: Tucking the chin to the chest is not relevant to the client's symptoms of hyperventilation.
Choice D: Instructing the client to increase her respiratory rate would exacerbate the hyperventilation, leading to more symptoms of respiratory alkalosis.
A nurse is providing teaching to a client who is at 30 weeks of gestation and is to have a nonstress test (NST). Which of the following statements by the client indicates a need for further teaching?
Explanation
Choice A: The client should not lie on her back during the NST because the supine position can compress the vena cava and reduce blood flow to the placenta and the baby. The NST is typically done with the client in a semireclined or left lateral position to ensure optimal blood flow to the baby.
Choice B: Monitoring the baby's heart rate is a correct statement and a standard part of the NST procedure.
Choice C: The duration mentioned (20 to 30 minutes) is accurate for the average NST timeframe.
Choice D: Scheduling the NST when the baby is usually active is also a correct statement, as fetal movement during the test is an important aspect of evaluating fetal wellbeing.
A nurse is teaching about fetal development to a group of clients in the antenatal clinic.
Which of the following statements should the nurse include in the teaching?
Explanation
Choice A: Fetal movements, also known as quickening, are usually felt by the mother between weeks 18 and 25 of pregnancy, not specifically at week 24.
Choice B: While the sex of the baby is determined at conception, it is not visually identifiable on ultrasound until around week 16 to 20, depending on the fetus's position and the quality of the ultrasound images.
Choice C: The baby's heartbeat can be visualized on ultrasound as early as 6 weeks of pregnancy. It becomes audible using a Doppler stethoscope around 8 to 9 weeks of pregnancy.
Choice D: Lanugo, the fine hair covering the baby's body, usually appears around weeks 20 to 24 of pregnancy and begins to diminish later in pregnancy, not specifically at week 36.
A nurse in a family planning clinic is caring for a 17 year old female client who is requesting oral contraceptives. The client states that she is nervous because she has never had a pelvic examination. Which of the following responses should the nurse make?
Explanation
Choice A: While relaxation can be helpful during a pelvic examination, it is not the most comprehensive response to address the client's concerns.
Choice B: A pelvic examination is not always required for prescribing birth control pills. In many cases, a healthcare provider can prescribe oral contraceptives based on the client's medical history and other factors without a pelvic exam.
Choice C: This response encourages the client to express her specific concerns and fears related to the examination, allowing the nurse to address them directly and provide appropriate support and reassurance.
Choice D: Although offering support during the exam is important, it does not address the client's nervousness and concerns about the examination itself.
A nurse is caring for a client who is in active labor and notes late decelerations in the FHR. Which of the following actions should the nurse take first?
Explanation
Choice A: Late decelerations in the fetal heart rate are often associated with uteroplacental insufficiency, and one of the first interventions is to improve uterine blood flow by changing the client's position. Placing the client in a left lateral position can help relieve pressure on the vena cava and improve blood flow to the placenta and the baby.
Choice B: Administering oxygen is a correct intervention for late decelerations, but it should follow the position change. Oxygen administration helps increase oxygen levels in the maternal blood, which can improve fetal oxygenation.
Choice C: Applying a fetal scalp electrode can provide continuous fetal heart rate monitoring, but it does not address the immediate concern of late decelerations. Position change and oxygen administration should be the priority.
Choice D: Increasing the rate of the IV infusion might not have an immediate effect on resolving late decelerations. Position change and oxygen administration should be the initial interventions.
A nurse is teaching a client who is at 18 weeks of gestation and is to undergo an amniocentesis. The nurse should explain that the purpose of this test is to identify which of the following? (Select all that apply.)
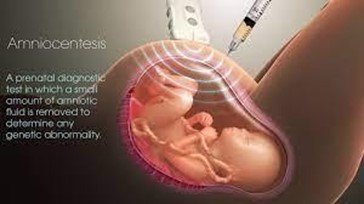
Explanation
Choice A: Amniocentesis is not primarily performed to determine the gender of the fetus. The main indication for this procedure is to detect genetic abnormalities or chromosomal disorders.
Choice B: The primary purpose of an amniocentesis is to detect chromosomal abnormalities such as Down syndrome (trisomy 21), trisomy 18, and trisomy 13, among others.
Choice C: Rh incompatibility is assessed through blood tests, not amniocentesis. It involves determining the Rh factor of the mother's blood and monitoring for potential Rh sensitization.
Choice D: Cephalopelvic disproportion refers to a situation where the baby's head is too large or the mother's pelvis is too small to allow for a vaginal delivery. It is not related to amniocentesis.
Choice E: While detecting neural tube defects can be done through amniocentesis, it is not the primary indication for the procedure. Neural tube defects can also be screened for through blood tests and ultrasound examinations. Amniocentesis is more commonly used for chromosomal analysis.
A nurse midwife is examining a client who is a primigravida at 42 weeks of gestation and states that she believes she is in labor. Which of the following findings confirm to the nurse that the client is in labor?
Explanation
Choice A: Pain above the umbilicus may be associated with various conditions during pregnancy, but it is not a definitive sign of labor.
Choice B: The presence of amniotic fluid in the vaginal vault (rupture of membranes or "water breaking") can be a sign of labor, but it is not the most specific indicator.
Choice C: Brownish vaginal discharge may indicate the passage of old blood or "bloody show," which can be a sign of impending labor. However, it is not as reliable as cervical dilation.
Choice D: Cervical dilation is one of the most definitive signs of labor. As the cervix opens and thins (effaces), it allows for the baby's passage through the birth canal. Cervical dilation is an essential indicator of active labor.
A nurse is creating the plan of care for a client who is at 39 weeks of gestation and in active labor. Which of the following actions should the nurse include in the plan of care?
Explanation
Choice A: While it is important to ensure the client has a voiding schedule during labor, routinely inserting an indwelling urinary catheter is not necessary for maintaining an empty bladder.
Choice B: Strict bedrest with all four side rails up is not appropriate during active labor, as it limits the client's movement and can be uncomfortable.
Choice C: Monitoring the fetal heart rate hourly during active labor is essential to assess the wellbeing of the baby and detect any signs of fetal distress.
Choice D: Checking the cervix to determine how close the time of delivery may be is not a standard action to take before administering analgesics. Analgesic administration should be based on the client's pain level and medical indications.
Sign Up or Login to view all the 68 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

