ATI Med Surg 102
Total Questions : 50
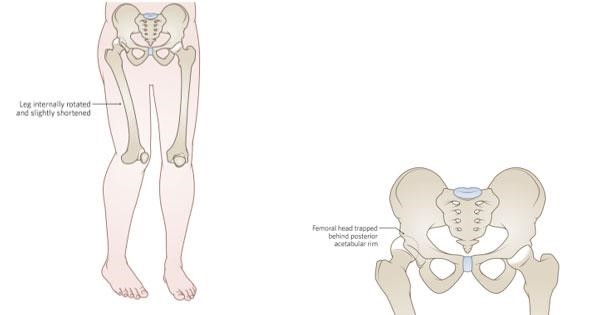
Showing 25 questions, Sign in for moreA client is brought to the emergency department by ambulance after stepping in a hole and falling. During the assessment, the nurse notes that the right leg is shorter than the left leg the right hip is noticeably deformed and acute pain is noted. Imaging does not reveal a fracture. What is the most likely explanation for this client's signs and symptoms?
Explanation
A. Right hip dislocation: In a hip dislocation, the head of the femur is forced out of the acetabulum, which is the socket in the pelvis. This can cause a noticeably shorter leg, hip deformity, and acute pain. Imaging might not show a fracture in the case of a dislocation.
B. Right hip contusion: A hip contusion is a bruise on the hip, usually caused by a direct blow or trauma. While it can cause pain and swelling, it typically does not result in a noticeably shorter leg or hip deformity.
C. Right hip strain: Hip strain refers to damage to the muscles or tendons around the hip joint due to overuse or sudden twisting movements. While it can cause pain, it does not typically lead to a noticeable leg shortening or hip deformity.
D. Right hip osteoarthritis: Osteoarthritis is a degenerative joint disease that can affect the hip joint. It leads to joint pain and stiffness but does not usually cause a noticeable leg shortening or acute deformity unless there are severe complications, which are not mentioned in the scenario.
A home health nurse is seeing an elderly male client for the first time. During the physical assessment of the skin on the lower legs the skin is pale and cool to touch. The nurse notes small circular ulcers on the soles of his feet. From these findings, the nurse knows that the client has a problem with circulation. Which of the circulation condition does the nurse suspect?

Explanation
The findings of pale and cool skin on the lower legs, along with small circular ulcers on the soles of the feet, are indicative of arterial insufficiency. Arterial insufficiency occurs when there is a decreased blood flow to the extremities, often due to conditions such as atherosclerosis or peripheral arterial disease. This reduced blood flow can result in pale and cool skin, as well as the development of ulcers, which are typically round and have well-defined borders. It is essential to assess and manage arterial insufficiency promptly to prevent complications like tissue necrosis and gangrene.
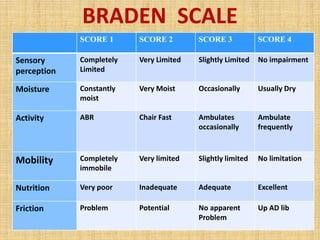
A nurse is completing a risk assessment on a new admission. Which standardized scale will the nurse use to calculate the client's risk for pressure ulcers?
Explanation
A. Morse Scale:
The Morse Scale, also known as the Morse Fall Scale, is used to assess a patient's risk of falling. It evaluates various factors such as history of falling, secondary diagnosis, ambulatory aids, IV therapy, gait, and mental status. It is primarily focused on assessing the risk of falls, not pressure ulcers.
B. Braden Scale:
As previously mentioned, the Braden Scale assesses a patient's risk for developing pressure ulcers. It takes into account sensory perception, moisture, activity, mobility, nutrition, and friction/shear. The scale helps healthcare providers determine the level of risk a patient has for developing pressure sores and guides interventions to prevent them.
C. Bristol Scale:
The Bristol Stool Scale is used to classify the form of human feces into seven categories. It is a medical aid designed to classify the form of human feces into seven categories. This scale is primarily used to assess bowel movements and is unrelated to pressure ulcers.
D. Hendrich II Scale:
The Hendrich II Fall Risk Model is a tool designed to identify patients at risk for falls. It includes factors such as confusion, symptomatic depression, altered elimination, dizziness, male gender, and the use of antiepileptics, benzodiazepines, or non-opioid analgesics. Similar to the Morse Scale, it focuses on assessing the risk of falls, not pressure ulcers.
A nurse is teaching an older adult client who has osteoporosis about beginning a program of regular physical activity. Which of the following recommendations should the nurse make?
Explanation
A. Stretching exercises:
Stretching exercises involve gently elongating muscles and tendons, promoting flexibility and range of motion. For individuals with osteoporosis, stretching exercises can improve balance and reduce the risk of falls, which is crucial as osteoporosis weakens bones and makes individuals more prone to fractures.
B. Riding a bicycle:
Bicycling is a low-impact cardiovascular exercise that is easy on the joints. It can help improve cardiovascular health, but it might not specifically address the balance and flexibility issues often associated with osteoporosis. However, it's a good option for overall fitness and joint health.
C. Walking briskly:
Brisk walking is an excellent low-impact aerobic exercise. It improves cardiovascular health, strengthens muscles, and aids in weight management. Walking can be adapted to various fitness levels, making it a suitable exercise for many older adults. While it doesn't specifically focus on flexibility, it promotes overall health and well-being.
D. High-impact aerobics:
High-impact aerobics involve activities like jumping, running, or intense dancing. These exercises can stress the bones and joints, potentially leading to injuries, especially for individuals with osteoporosis. High-impact exercises are generally discouraged for people with osteoporosis due to the increased risk of fractures.
A nurse educator is providing an in-service to nursing staff about urinary tract infections (UTP). Which statements made by the staff validate they understand the etiology and pathophysiology of UTIs? Select all that apply.
Explanation
A. "UTI’s can be caused by urethrovesical reflux which is the backward flow of urine from the urethra to the bladder after coughing, sneezing, or straining":
This statement is correct. Urethrovesical reflux can contribute to UTIs, especially in women, as it can introduce bacteria from the urethra back into the bladder.
B. "UTI’s are more common in women due to their longer urethras":
This statement is correct. Women have shorter urethras than men, which makes it easier for bacteria to travel into the bladder, increasing the risk of UTIs.
C. "Glycosaminoglycan (GAG) is a protein in the urinary tract that exerts a nonadherent protective effect against various bacteria":
This statement is correct. Glycosaminoglycan is a substance that lines the urinary tract and helps prevent bacterial adherence, thereby protecting against UTIs.
D. "The organism most often responsible for UTI's in older adults is staphylococcus":
This statement is incorrect. The most common bacteria responsible for UTIs are Escherichia coli (E. coli), not staphylococcus.
E. "The normal urinary tract is sterile above the urethra":
This statement is correct. Normally, the urinary tract above the urethra is sterile, devoid of bacteria. UTIs occur when bacteria enter and multiply in the urinary system, leading to infection.
A nurse is caring for an adolescent client who has pneumonia and a prescription for cefpodoxime 5 mg/kg PO for 5 days. The client weighs 88 lb. How many mg should the nurse administer? (Round the answer to the nearest whole number)
Explanation
To calculate the dose of cefpodoxime for the adolescent client, we first need to convert the weight from pounds to kilograms.
1 lb is approximately 0.45 kg.
88lb×0.45kg/lb=39.6kg88lb×0.45kg/lb=39.6kg (rounded to one decimal place).
The dose prescribed is 5 mg/kg. Now, multiply the weight in kilograms by the prescribed dose:
5mg/kg×39.6kg=198mg5mg/kg×39.6kg=198mg.
So, the nurse should administer 198 mg of cefpodoxime to the adolescent client.
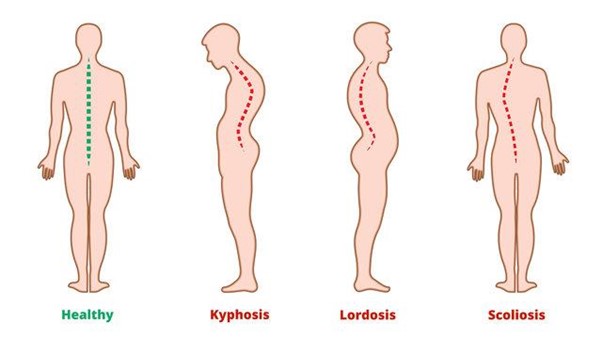
A nurse is assessing an older adult client who has osteoporosis. Which of the following spinal deformities should the nurse expect to find in this client?
Explanation
A. Lordosis: Lordosis is an inward curvature of the spine, commonly seen in the lower back (lumbar spine) or neck (cervical spine). It creates a swayback appearance. Lordosis is not typically associated with osteoporosis.
B. Scoliosis: Scoliosis is a sideways curvature of the spine, creating an "S" or "C" shape. While scoliosis can occur in people of all ages, it is not directly caused by osteoporosis.
C. Ankylosis: Ankylosis refers to the stiffening or fusion of joints, often due to inflammation and progressive loss of function. It is not a spinal deformity associated with osteoporosis.
D. Kyphosis: Kyphosis is a forward rounding of the back, leading to a hunched or humpbacked posture. It commonly affects the upper back (thoracic spine) and is associated with osteoporosis, especially in older adults. When the bones in the spine weaken due to osteoporosis, they can compress and collapse, leading to the development of kyphosis. This condition is sometimes referred to as a dowager's hump when it occurs in older women.
A nurse needs to infuse three 1L bags over 12 hours. At what rate should the nurse program the pump to run in millilitres per hour? Round to the nearest whole number.
Explanation
To calculate the infusion rate, you first need to determine the total volume to be infused and the total time over which the infusion will occur.
Three 1L bags need to be infused over 12 hours.
Total volume = 3 bags * 1000 mL/bag = 3000 mL
Total time = 12 hours
Now, to find the rate in milliliters per hour (mL/h), divide the total volume by the total time:
Infusion rate = Total volume / Total time
Infusion rate = 3000 mL / 12 hours = 250 mL/h
A nurse is caring for a client who has multiple long bone fractures caused by a motor-vehicle crash that happened 24 hr ago. The client tells the nurse he is short of breath and experiencing chest pain. The nurse should assess the client further for which of the following potential complications?
Explanation
A. Hypovolemic shock: Hypovolemic shock occurs when there is a significant loss of blood or fluids in the body, leading to insufficient blood volume to maintain normal circulation. Symptoms include rapid heart rate, low blood pressure, confusion, and cold, clammy skin. While hypovolemic shock is a concern in trauma patients, the symptoms described by the client (shortness of breath and chest pain) are not typical of hypovolemic shock.
B. Fat embolism syndrome: Fat embolism syndrome occurs when fat particles are released into the bloodstream, often after a long bone fracture or trauma. These fat particles can block small blood vessels, leading to symptoms such as respiratory distress, confusion, and petechial rash (small red or purple spots under the skin). While fat embolism syndrome is a concern in patients with long bone fractures, the symptoms described by the client are more suggestive of a pulmonary embolism.
C. Venous thromboembolism (VTE): VTE refers to the formation of blood clots in the veins. Deep vein thrombosis (DVT) occurs when a blood clot forms in a deep vein, usually in the legs, while pulmonary embolism (PE) occurs when a clot breaks loose and travels to the lungs. Symptoms of PE can include sudden chest pain, shortness of breath, rapid heart rate, and cough, which may produce bloody or blood-streaked sputum. Given the client's symptoms of shortness of breath and chest pain, VTE, specifically pulmonary embolism, is a significant concern.
D. Compartment syndrome: Compartment syndrome occurs when there is increased pressure within a muscle compartment, leading to reduced blood flow and potential nerve damage. Symptoms can include severe pain, swelling, and numbness or tingling. While compartment syndrome is a complication of fractures, the symptoms described by the client (shortness of breath and chest pain) are not characteristic of compartment syndrome.
A client is admitted to the orthopedic unit with a fractured femur after a motorcycle accident. The client has been placed in traction until his femur can be rodded in surgery. For what early complications should the nurse monitor this client? Select all that apply.
Explanation
A. Malunion: Malunion happens when a fractured bone heals in an improper position, leading to deformity and functional impairment. While it is a concern, it typically develops over time during the healing process and is not an immediate early complication that the nurse would monitor for in the acute phase following a fracture.
B. Compartment syndrome: Compartment syndrome is a serious condition that can occur after an injury, such as a fracture. When there is increased pressure within a muscle compartment, it can lead to reduced blood flow, potentially causing tissue damage and nerve injury. Prompt recognition and intervention are crucial to prevent complications.
C. Fat embolism: Fat embolism occurs when fat particles from the bone marrow or other sources enter the bloodstream, often after a long bone fracture or major trauma. These particles can travel to the lungs and other organs, causing respiratory distress, confusion, and other symptoms. Fat embolism is a significant concern in orthopedic trauma patients and requires careful monitoring.
D. Deep vein thrombosis (DVT): DVT is the formation of blood clots in deep veins, usually in the legs. Patients with fractures, especially those immobilized for extended periods, are at increased risk for DVT. If a clot dislodges and travels to the lungs, it can cause a pulmonary embolism, which is a life-threatening complication.
E. Pulmonary emboli: Pulmonary emboli occur when blood clots, often originating from DVT, travel to the lungs and block pulmonary arteries. This condition can lead to sudden difficulty breathing, chest pain, and even cardiac arrest. Pulmonary embolism is a medical emergency and requires immediate intervention.
A nurse is caring for a client started on Phenazopyridine (Pyridium). Which of the following indicates this medication is effective?
Explanation
A. Increased urinary output: Phenazopyridine (Pyridium) does not directly impact urinary output. Its primary function is to provide relief from urinary pain, burning, and discomfort associated with urinary tract infections (UTIs) or other urinary conditions. It does not affect the amount of urine a person produces.
B. Decreased WBC's: Phenazopyridine does not directly influence white blood cell count (WBCs). WBC count is an indicator of the body's immune response and is typically used to assess the presence of infection. Phenazopyridine provides symptomatic relief but does not affect the underlying infection or the body's immune response to it.
C. Increased uric acid: Phenazopyridine does not affect uric acid levels. Uric acid is a waste product that is excreted by the kidneys. Elevated uric acid levels can be associated with conditions like gout, but Phenazopyridine does not have any direct impact on these levels.
D. Decreased bladder pain/spasms: Phenazopyridine is intended to relieve symptoms such as bladder pain, spasms, burning sensation, and discomfort experienced during urination. Therefore, the effectiveness of Phenazopyridine is indicated by a reduction in these symptoms. If the patient reports a decrease in bladder pain and spasms, it suggests that the medication is working to alleviate the discomfort associated with urinary tract issues.
A nurse is caring for a client with acute pyelonephritis. Which area should the nurse percuss to assess for pain related to pyelonephritis?
Explanation
A. McBurney's point on the abdomen: McBurney's point is a location in the right lower quadrant of the abdomen that is significant in the assessment for appendicitis. It is not relevant to the assessment of pyelonephritis, which is a kidney infection.
B. Psoas sign at the knee: The psoas sign is a test for appendicitis, not pyelonephritis. It involves the patient lying on their back and lifting their right leg against resistance. If this movement causes pain in the lower right abdomen, it could indicate irritation of the psoas muscle due to an inflamed appendix.
C. Rovsing's Sign on the abdomen: Rovsing's sign is also a test for appendicitis. It involves palpating the left lower quadrant of the abdomen and observing if it causes pain in the right lower quadrant. The presence of pain in the right lower quadrant during palpation of the left lower quadrant can indicate appendicitis. This sign is not specific to pyelonephritis.
D. Costovertebral angle (CVA) on the back: The CVA is located on the back at the angle formed by the 12th rib and the spine. Percussion of the CVA is a common technique used to assess for kidney tenderness. In the case of acute pyelonephritis, infection and inflammation of the kidneys can cause tenderness and pain in the CVA area. Therefore, this area is assessed for pain related to kidney infections like pyelonephritis.
A client has come to the orthopedic clinic for a follow-up appointment 6 weeks after fracturing his ankle. Diagnostic imaging reveals that bone union is not taking place. What factor most likely contributed to this complication?
Explanation
A. Inadequate immobilization: Proper immobilization is essential for fractured bones to heal correctly. Immobilization, often achieved through casts, splints, or other orthopedic devices, stabilizes the broken bone fragments, allowing them to fuse back together. If the immobilization is not sufficient or if the patient doesn't follow the prescribed immobilization protocol, there can be excessive movement at the fracture site, hindering the healing process.
B. Venous thromboembolism: Venous thromboembolism (VTE) refers to the formation of blood clots in veins, usually in the legs (deep vein thrombosis) that can travel to the lungs (pulmonary embolism). While VTE is a potential complication after a fracture, it is not a direct cause of delayed bone union.
C. Inadequate vitamin D intake: Vitamin D is essential for bone health as it helps the body absorb calcium, which is crucial for bone formation and maintenance. Inadequate vitamin D levels can weaken bones and impair the healing process, but it's not a common cause of delayed bone union unless there are severe deficiencies or underlying medical conditions.
D. Bleeding at the injury site: Bleeding at the injury site occurs immediately after the fracture and is a natural part of the body's response to injury. While excessive bleeding can lead to complications, it is not a likely cause of delayed bone union six weeks after the injury. In the early stages of healing, bleeding is replaced by the formation of a hematoma, which eventually transforms into a callus and aids in the bone healing process.
A nurse is providing teaching to a client about measures to prevent urinary tract infections (UTIs). Which of the following client statements indicates a need for further teaching?
Explanation
A. "I will need to drink apple cider vinegar each day."
This statement is incorrect. Drinking apple cider vinegar is not a proven method to prevent urinary tract infections (UTIs). The client does not need to consume apple cider vinegar as a preventive measure for UTIs.
B. “I will need to wipe my perineal area from back to front after urination."
This statement is incorrect and indicates a need for further teaching. Proper hygiene is essential in preventing UTIs, and wiping from back to front can introduce bacteria from the anal area to the urethra, increasing the risk of UTIs. The correct technique is to wipe from front to back after urination to prevent the spread of bacteria.
C. “I need to drink 8 cups of liquid each day."
This statement is correct. Staying well-hydrated by drinking an adequate amount of fluids, such as 8 cups of liquid each day, can help flush out bacteria from the urinary tract and reduce the risk of UTIs. Proper hydration is a good preventive measure.
D. "I will need to empty my bladder regularly and completely.”
This statement is correct. Emptying the bladder regularly and completely helps prevent the accumulation of bacteria in the urinary tract. Incomplete emptying of the bladder can allow bacteria to multiply, increasing the risk of UTIs. Regular and thorough emptying of the bladder is an important preventive measure against UTIs.
A nurse is caring for an older adult client who is at risk for skin breakdown. Which of the following interventions should the nurse use to help maintain the integrity of the client's skin?
Explanation
A. Remove heel boots:
Heel boots are often used to protect the heels from pressure ulcers. However, it's important to assess the skin regularly and remove heel boots periodically to inspect the skin underneath. Leaving them on continuously without proper inspection can cause moisture buildup, leading to skin breakdown.
B. Reposition every 3 hours
Repositioning the client every 3 hours is a crucial intervention to prevent skin breakdown, especially in individuals at risk, such as older adults. Prolonged pressure on specific areas of the body can lead to pressure ulcers or bedsores. Regular repositioning helps relieve pressure on vulnerable areas, improving circulation and reducing the risk of skin breakdown.
C. Apply cornstarch to keep the skin dry:
While it's essential to keep the skin clean and dry, using cornstarch can sometimes lead to moisture retention, especially in skin folds. Excess moisture can contribute to skin breakdown and fungal infections. Instead, proper hygiene practices and the use of moisture-wicking products are recommended.
D. Provide high protein diet:
Adequate nutrition, including a high-protein diet, is essential for overall skin health and healing. Protein is necessary for tissue repair and regeneration. While a balanced diet is crucial for overall health, it is not a specific intervention solely focused on maintaining skin integrity.
A nurse is caring for a client who is postoperative following knee arthroplasty and has a new prescription for enoxaparin 1mg/kg subcutaneous. The client weighs 185 lb. How many mg should the nurse administer? (Round the answer to the nearest tenth. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
To calculate the dose of enoxaparin, first, you need to convert the client's weight from pounds to kilograms.
1 lb is approximately equal to 0.45 kg.
185 lb * 0.45 kg/lb = 83.25 kg (rounded to the nearest hundredth)
Now that you know the client's weight in kilograms, you can calculate the dose:
Dose = 1 mg/kg * 83.25 kg = 83.25 mg
Therefore, the nurse should administer 83.3 mg of enoxaparin
A nurse is teaching a group of clients about osteoarthritis. Which of the following recommendations should the nurse include in the teaching?
Explanation
A. Use Echinacea to manage joint pain:
Echinacea is a natural supplement, but its effectiveness in managing joint pain related to osteoarthritis is not well-established. It's important for individuals to consult their healthcare provider before using any supplements, as they may interact with medications or have other adverse effects.
B. Maintain a recommended body weight.
Maintaining a healthy body weight is an important recommendation for managing osteoarthritis. Excess weight puts additional stress on weight-bearing joints, such as knees and hips, which can worsen osteoarthritis symptoms. Losing weight, if necessary, or maintaining a healthy weight can help reduce joint pain and improve mobility in individuals with osteoarthritis.
C. Apply ice to the joint before exercising:
Applying ice can help reduce inflammation and provide pain relief, but it's typically used after exercising or during acute flare-ups, not necessarily before exercising. Heat is often recommended before exercise to warm up the joint and improve flexibility.
D. Reduce the amount of purine in the diet:
This recommendation is more relevant for managing gout, a different type of arthritis caused by the buildup of uric acid crystals in the joints. Purine-rich foods can trigger gout attacks but are not directly related to osteoarthritis. Osteoarthritis is primarily related to wear and tear of the joints over time.
A nurse is providing dietary teaching to a client who has a history of gout and recurring uric acid kidney stones. Which of the following instructions should the nurse include in the teaching?
Explanation
A. Restrict calcium intake to one serving per day:
This statement is not accurate. Adequate calcium intake is essential for bone health. Calcium-rich foods are important for maintaining strong bones and are not directly related to gout or uric acid kidney stones. It's crucial to differentiate between dietary recommendations for different health conditions.
B. Take 3,000 mg of vitamin C daily:
High doses of vitamin C can increase urinary oxalate and uric acid levels, which might contribute to the formation of kidney stones. It is generally not recommended for individuals with a history of uric acid kidney stones.
C. The nurse should instruct the client to limit foods high in purines.
Dietary changes are important in managing gout and preventing uric acid kidney stones. Purines are natural substances found in many foods, especially animal products, and purine-rich foods can contribute to increased uric acid levels, leading to gout attacks and kidney stones.
D. Eat 12 oz of animal protein daily:
Consuming excessive amounts of animal protein, particularly red meat, can lead to higher purine intake, which is not advisable for individuals prone to gout and uric acid kidney stones. High animal protein intake can increase uric acid production and may exacerbate these conditions. Moderation in protein intake, especially from animal sources, is recommended.
A nurse is caring for a 125 kg patient who is to receive 2.5-3.5 mg/kg of enoxaparin daily. How many milligrams will the patient receive if getting the high end of the dosage range? Round to the whole number.
Explanation
To calculate the high-end dosage for a 125 kg patient, you can multiply the weight in kilograms (125 kg) by the high-end dosage range (3.5 mg/kg):
High-end dosage = 125 kg * 3.5 mg/kg = 437.5 mg
An emergency department client is diagnosed with a hip dislocation. The client's family is relieved that the client has not suffered a hip fracture, but the nurse explains that this is still considered to be a medical emergency. What is the rationale for the nurse's statement?
Explanation
A. The longer the joint is displaced, the more difficult it is to get it back in place:
This statement is correct. Prompt reduction of a dislocated joint is important because the longer the joint remains out of place, the more difficult it becomes to realign it. Delayed reduction can lead to complications and makes the process more challenging for healthcare providers.
B. Avascular necrosis may develop at the site if it is not promptly resolved:
Avascular necrosis is a condition where bone tissue dies due to a lack of blood supply. While it is a potential complication of hip dislocation, it is not the immediate rationale for considering hip dislocation a medical emergency. The urgency primarily lies in the difficulty of reducing the dislocation and preventing further complications.
C. The client's pain will increase until the joint is realigned:
This statement is partially correct. While it is true that dislocated joints are extremely painful, the urgency in reducing the dislocation is not solely based on pain management. It is essential to prevent complications, restore joint function, and minimize long-term damage to the affected area.
D. Dislocation can become permanent if the process of bone remodeling begins:
This statement is accurate. If a dislocated joint is not promptly reduced, the surrounding tissues may undergo changes, and the process of bone remodeling can begin. This can lead to the dislocation becoming more difficult or even impossible to reduce, resulting in a permanent dislocation. Early intervention is essential to prevent this outcome.
A female client has been experiencing recurrent urinary tract infections. What health education should the nurse provide to this client?
Explanation
A. Void every 6 to 8 hours:
Regular voiding helps prevent urinary stasis, which can reduce the risk of UTIs. However, specific time intervals might vary from person to person based on individual needs and habits.
B. Avoid voiding immediately after sexual intercourse.
The nurse should educate the client to avoid voiding immediately after sexual intercourse. This practice helps to flush out any bacteria that might have entered the urethra during intercourse, reducing the risk of urinary tract infections (UTIs). It's an important preventive measure for individuals prone to recurrent UTIs.
C. Take a bubble bath daily and keep the perineal region clean:
While keeping the perineal region clean is important for general hygiene, taking bubble baths and using heavily scented products can irritate the urethra and potentially increase the risk of UTIs. The nurse should advise against frequent bubble baths and suggest using mild, unscented soaps for the perineal area.
D. Increase the daily amount of water consumed:
Adequate hydration is crucial for overall health, including urinary tract health. Drinking plenty of water can help flush out bacteria from the urinary system and reduce the risk of UTIs. This is generally good advice but does not specifically address the prevention of recurrent UTIs.
A nurse is teaching a client who is scheduled for dual-energy x-ray absorptiometry (DEXA) to screen for osteoporosis. Which of the following instructions should the nurse include in the teaching?
Explanation
A. There is no need for the client to lie flat for an extended period after a DEXA scan. The procedure is non-invasive and does not require immobilization.
B. Emptying the bladder before the test is essential to ensure a clear and accurate scan of the pelvis and lower spine. A full bladder might obstruct the view and affect the accuracy of the results.
C. DEXA scans do not typically require the use of IV dye. It is a simple X-ray procedure that measures bone density, and no contrast material is usually needed.
D. Fasting is not necessary for a DEXA scan. The procedure does not involve ingesting or injecting any substances that require fasting.
A nurse is teaching a client about preventing osteoporosis. Which of the following statements by the client indicates a need for further teaching?
Explanation
A. "I will reduce my intake of sodium." - This statement is correct. High sodium intake can lead to increased calcium excretion through the urine, which can weaken bones. Reducing sodium intake can help prevent osteoporosis.
B. "I will limit my intake of soft drinks." - This statement is correct. Soft drinks, especially cola beverages, contain phosphoric acid, which can leach calcium from bones, leading to decreased bone density. Limiting soft drink consumption is advisable for bone health.
C. "I will decrease my intake of caffeine." - This statement is correct. Excessive caffeine consumption can interfere with calcium absorption and increase calcium excretion. It is advisable to limit caffeine intake to prevent osteoporosis.
D. "I will reduce my intake of vitamin K-rich foods." - This statement is incorrect. Vitamin K is essential for bone health as it helps in bone mineralization and reduces the risk of fractures. Foods rich in vitamin K, such as leafy green vegetables, are beneficial for bone health and should not be reduced unless there are specific medical reasons to do so.
An 82-year-old diabetic client is being treated in the hospital for a sacral pressure ulcer. What age-related change is most likely to affect the client's course of treatment?
Explanation
A. Increased thickness of the subcutaneous skin layer - Aging typically results in thinning of the skin and subcutaneous tissue, making older adults more vulnerable to pressure ulcers rather than having increased thickness.
B. Changes in the character and quantity of bacterial skin flora - This is a common age-related change; however, it is not directly related to the course of treatment for a sacral pressure ulcer. Proper wound care can mitigate the impact of changes in skin flora.
C. Increased time required for wound healing - Aging often leads to a decline in the body's ability to repair and regenerate tissues, which can prolong the healing process of wounds, including pressure ulcers. Older adults may experience delayed wound healing compared to younger individuals.
D. Increased elasticity of the skin - Skin elasticity decreases with age, making older adults more susceptible to skin breakdown and pressure ulcers due to reduced skin resilience and ability to redistribute pressure. Increased elasticity would not affect the course of treatment positively but rather negatively in this context.
A nurse is talking with a young adult client who has a family history of osteoporosis, Which health promotion activity should the nurse recommend as a possible preventive measure?
Explanation
A. Increase sodium intake - This is not a preventive measure for osteoporosis. High sodium intake can lead to increased calcium excretion and weaken bones.
B. Drink a cup of coffee each morning - Caffeine consumption, especially in excess, can interfere with calcium absorption and increase calcium excretion. Limiting caffeine intake is recommended for bone health. Drinking coffee in moderation is acceptable but excessive consumption should be avoided.
C. Have a bone-density scan each year - While bone-density scans (DEXA scans) are useful for diagnosing osteoporosis or assessing bone health, they are not typically recommended for young adults with a family history of osteoporosis unless there are specific risk factors present. Yearly scans are unnecessary and not cost-effective for young adults without significant risk factors.
D. Engage in weight-bearing exercise regularly - Weight-bearing exercises, such as walking, jogging, dancing, and resistance training, help to increase bone density and strength. Regular physical activity, especially weight-bearing exercises, is a recommended preventive measure against osteoporosis.
Sign Up or Login to view all the 50 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

