ATI Med Surg 2
Total Questions : 50
Showing 25 questions, Sign in for moreThe nurse is evaluating a client who had a cardiac catheterization with a left antecubital insertion site. Which of the following pulses should the nurse palpate?
Explanation
Choice A Reason: This is incorrect because the radial pulse in the right arm is not related to the left antecubital insertion site.
Choice B reason: This is correct because the radial pulse in the left arm is the closest pulse to the insertion site and would reflect any changes in blood flow or pressure. The nurse should palpate the radial pulse in the same arm as the insertion site to assess for any vascular complications, such as bleeding, hematoma, or thrombosis. The other choices are not relevant to the insertion site and would not provide accurate information about the client's condition.
Choice C Reason: This is incorrect because the brachial pulse in the left arm is not as close to the insertion site as the radial pulse and would not be as sensitive to detect any vascular complications.
Choice D Reason: This is incorrect because the brachial pulse in the right arm is not related to the left antecubital insertion site.

A nurse is receiving a transfer report for a client who has a head injury. The client has a Glasgow Coma Scale (GCS) score of 3 for eye opening, 5 for best verbal response, and 5 for best motor response. Which of the following is an appropriate conclusion based on this data?
Explanation
Choice A Reason: This is incorrect because the client's best motor response is 5, which means he can localize pain, not follow commands.
Choice B Reason: This is incorrect because the client's eye opening response is 3, which means he opens his eyes to pain, not to speech.
Choice C Reason: This is correct because the client's GCS score is 13, which indicates a severe impairment of consciousness. The GCS is a tool used to assess the level of consciousness of a person who has a head injury. The GCS score ranges from 3 to 15, with lower scores indicating lower levels of consciousness. A GCS score of 8 or less indicates coma. The client's GCS score is 3 + 5 + 5 = 13, which is above the coma threshold, but still indicates a severe impairment of consciousness. The other choices are not consistent with the client's GCS score.
Choice D Reason: This is incorrect because the client's best verbal response is 5, which means he can orient himself to person, place, and time, not that he is unable to make vocal sounds.
A nurse is helping to triage a group of clients at a mass casualty incident who were involved in an explosion at a local factory. Which of the following clients should the nurse tag to be the priority for care?
Explanation
Choice A Reason: This is incorrect because this client has signs of brain death, such as severe head injuries, low respiratory rate, and unresponsiveness. The nurse should tag this client as black, which means deceased or expectant.
Choice B Reason: This is incorrect because this client has non-life-threatening injuries, such as a simple fracture and scratches. The nurse should tag this client as green, which means minor or delayed care.
Choice C Reason: This is incorrect because this client has minor injuries and is able to walk around. The nurse should tag this client as green, which means minor or delayed care.
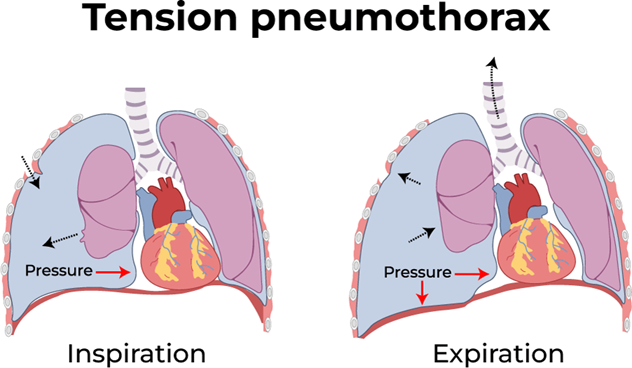
Choice D Reason: This is correct because this client has a life-threatening condition called tension pneumothorax, which requires immediate care. This client has a life-threatening condition called tension pneumothorax, which is caused by air leaking into the pleural space and compressing the lung and the heart. This can lead to respiratory failure, cardiac arrest, and death if not treated immediately. The hissing sound indicates that air is escaping from the lung through the wound. The nurse should tag this client as red, which means immediate care is needed.
A nurse is preparing to administer dabigatran to a client who has atrial fibrillation. The nurse should explain that the purpose of this medication is which of the following?
Explanation
Choice A Reason: This is incorrect because dabigatran does not affect the electrical activity of the heart or the conduction system. It does not slow down the ventricular response to the atrial impulses.
Choice B Reason: This is incorrect because dabigatran does not dissolve existing clots in the bloodstream. It only prevents new clots from forming.
Choice C Reason: This is correct because dabigatran reduces the risk of stroke in clients who have atrial fibrillation by preventing clot formation and reducing blood viscosity. Dabigatran is an anticoagulant medication that prevents the formation of blood clots in the heart and blood vessels. Atrial fibrillation is a condition where the atria beat irregularly and rapidly, which can cause blood to pool and clot in the heart chambers. These clots can travel to the brain and cause a stroke. Dabigatran reduces the risk of stroke by preventing clot formation and reducing blood viscosity.
Choice D Reason: This is incorrect because dabigatran does not restore normal sinus rhythm in clients who have atrial fibrillation. It does not affect the heart rate or rhythm.
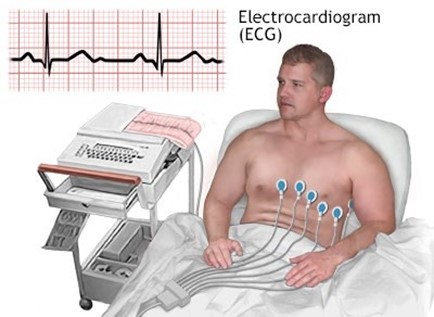
A nurse is caring for a client who has a serum potassium level of 5.5 mEq/L. The provider prescribes polystyrene sulfonate. If this medication is effective, the nurse should expect which of the following changes on the client’s ECG?
Explanation
Choice A Reason: This is incorrect because shortening of P-wave duration is not a sign of hyperkalemia or its reversal.
P-wave duration reflects the time it takes for the atria to depolarize and contract.
Choice B Reason: This is incorrect because restoration of QRS complex amplitude is not a sign of hyperkalemia or its reversal. QRS complex amplitude reflects the voltage or strength of the ventricular depolarization and contraction.
Choice C Reason: This is correct because the reduction of T-wave amplitude is a sign of hyperkalemia reversal. T-wave amplitude reflects the repolarization or recovery of the ventricles after contraction. Polystyrene sulfonate is a medication that lowers the serum potassium level by binding to it in the gastrointestinal tract and excreting it in the stool. High serum potassium level, or hyperkalemia, can cause cardiac arrhythmias and ECG changes, such as peaked T waves, prolonged PR interval, flatened P waves, widened QRS complex, and ventricular fibrillation. By lowering the serum potassium level, polystyrene sulfonate can reverse these ECG changes and normalize the cardiac rhythm.
Choice D Reason: This is incorrect because the widening of the QRS complex is a sign of hyperkalemia, not its reversal. Widening of the QRS complex reflects the delay or impairment of ventricular depolarization and contraction.

A nurse in an emergency department is caring for a client who is bleeding profusely from a deep laceration on his left lower forearm. After observing standard precautions, which of the following actions should the nurse perform first?
Explanation
Choice A Reason: This is incorrect because cleaning the wound is not a priority when the client is bleeding profusely. Cleaning the wound can also dislodge any clots that have formed and increase bleeding.
Choice B Reason: This is incorrect because applying a tourniquet is a last resort when direct pressure fails to stop bleeding. A tourniquet can cause tissue damage, nerve injury, and infection if applied incorrectly or for too long.
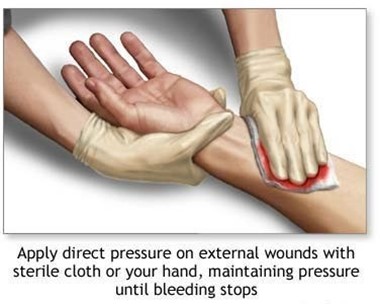
Choice C Reason: This is correct because applying direct pressure over the wound is the first and most effective action to stop bleeding from a wound. This is the first and most effective action to stop bleeding from a wound. Direct pressure compresses the blood vessels and prevents further blood loss. The nurse should use a clean cloth or dressing to cover the wound and apply firm pressure with both hands.
Choice D Reason: This is incorrect because elevating the limb and applying ice are not effective actions to stop bleeding from a wound. Elevating the limb can reduce blood flow to the injured area, but it does not compress the blood vessels or prevent blood loss. Applying ice can cause vasoconstriction, but it can also damage the skin and tissues if applied for too long.
A nurse is caring for a client who has hypertension and develops epistaxis. Which of the following actions should the nurse take? (Select all that apply.)
Explanation
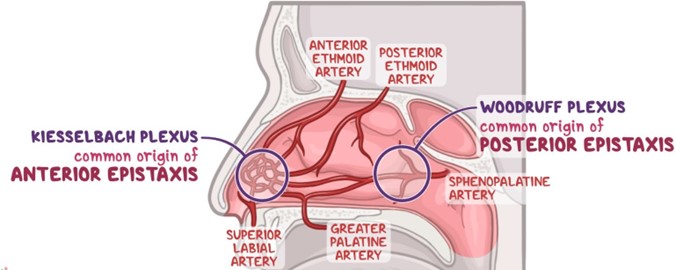
Choice A Reason: This is correct because placing ice to the bridge of the client’s nose can cause vasoconstriction and reduce blood flow to the nasal mucosa.
Choice B Reason: This is incorrect because tilting the client's head backward can cause blood to drain into the throat and increase the risk of aspiration, nausea, and vomiting.
Choice C Reason: This is correct because moving the client into high-Fowler position can lower the blood pressure in the head and neck and decrease bleeding.
Choice D reason Reason This is incorrect because instructing the client to blow his nose can dislodge any clots that have formed and worsen bleeding.
Choice E Reason: This is correct because applying pressure to the nares can compress the bleeding site and promote clotting.
A nurse is reviewing the arterial blood gas values of a client who has chronic kidney disease. Which of the following sets of values should the nurse expect?
Explanation
Choice A Reason: This is incorrect because these values indicate respiratory alkalosis, which is caused by hyperventilation or excess loss of carbon dioxide (PaCO2). Respiratory alkalosis increases the blood pH and decreases the HCO3- level.
Choice B Reason: This is incorrect because these values indicate metabolic alkalosis, which is caused by excess intake or retention of bases or loss of acids. Metabolic alkalosis increases the blood pH and the HCO3- level.
Choice C Reason: This is incorrect because these values indicate respiratory acidosis, which is caused by hypoventilation or excess retention of carbon dioxide (PaCO2). Respiratory acidosis decreases the blood pH and increases the HCO3- level.
Choice D Reason: This is correct because these values indicate metabolic acidosis, which is a common complication of chronic kidney disease. These values indicate metabolic acidosis, which is a common complication of chronic kidney disease. Metabolic acidosis occurs when the kidneys are unable to excrete excess acids or retain enough bicarbonate (HCO3-), which is a base that buffers the blood pH. As a result, the blood pH decreases and becomes more acidic. The normal range for blood pH is 7.35 to 7.45, for HCO3- is 22 to 26 mEq/L, and for PaCO2 is 35 to 45 mm Hg.
A nurse is planning a staff education session regarding biological weapons of mass destruction. Which of the following should he plan to include in the session? (Select all that apply.)
Explanation
Choice A Reason: This is correct because smallpox is a highly contagious and deadly viral disease that can be used as a biological weapon. Smallpox was eradicated in 1980, but some samples of the virus are still stored in laboratories. If released intentionally, smallpox could cause a global pandemic.
Choice B Reason: This is incorrect because hydrogen cyanide is a chemical weapon of mass destruction, not a biological one. Hydrogen cyanide is a colorless gas that interferes with cellular respiration and causes rapid death.
Choice C Reason: This is correct because botulism is a serious and potentially fatal illness caused by a toxin produced by the bacterium Clostridium botulinum. Botulism can be used as a biological weapon by contaminating food or water supplies or by aerosolizing the toxin.
Choice D Reason: This is correct because anthrax is an infection caused by the spore-forming bacterium Bacillus anthracis. Anthrax can be used as a biological weapon by releasing the spores into the air or by contaminating food or water sources.
Choice E Reason: This is incorrect because sarin is a chemical weapon of mass destruction, not a biological one. Sarin is a nerve agent that blocks the transmission of nerve impulses and causes respiratory failure and death.

A nurse is performing cardiopulmonary resuscitation (CPR) for an adult client who is unresponsive. The nurse should evaluate the client's circulation by palpating which of the following pulses?
Explanation
Choice A Reason: This is correct because the carotid pulse is the most accessible and reliable pulse to check during CPR for an adult client. The carotid pulse is the most accessible and reliable pulse to check during CPR for an adult client. The carotid pulse is located on the side of the neck, near the trachea. The nurse should use two fingers to palpate the carotid pulse for at least 5 seconds and no more than 10 seconds.
Choice B Reason: This is incorrect because the popliteal pulse is located behind the knee and is not easily palpable during CPR.
Choice C Reason: This is incorrect because the radial pulse is located on the wrist and may not be detectable during CPR due to low blood pressure or peripheral vasoconstriction.
Choice D Reason: This is incorrect because the apical pulse is located on the chest and requires a stethoscope to auscultate. The nurse should not interrupt chest compressions or ventilations to listen to the apical pulse during CPR.
A nurse is caring for a client who is in the compensatory stage of shock. Which of the following findings should the nurse expect?
Explanation
Choice A Reason: This is incorrect because a heart rate of 180/min is a sign of the progressive stage of shock, not the compensatory stage. In the progressive stage of shock, the compensatory mechanisms fail to maintain adequate perfusion and oxygenation, and the heart rate increases further to compensate for the low cardiac output.
Choice B Reason: Motled skin. Mottled skin is a sign of poor perfusion and tissue hypoxia, which are common in the compensatory stage of shock. Shock is a condition where the body's organs and tissues do not receive enough oxygen and nutrients due to low blood pressure, low cardiac output, or low blood volume. In the compensatory stage of shock, the body tries to maintain vital functions by activating various mechanisms, such as increasing heart rate, vasoconstriction, and hormonal stimulation. However, these mechanisms also cause reduced blood flow to the skin and extremities, resulting in motled skin.
Choice C Reason: This is incorrect because hypokalemia is not a sign of shock. Hypokalemia is a condition where the serum potassium level is lower than normal, which can be caused by various factors, such as diuretics, vomiting, diarrhea, or metabolic alkalosis.
Choice D Reason: This is incorrect because blood pressure 115/68 mm Hg is within the normal range and does not indicate shock. In the compensatory stage of shock, the blood pressure may be normal or slightly decreased due to the compensatory mechanisms.

A nurse is caring for a male client who reports nausea and vomiting and is receiving IV fluid therapy. His blood urea nitrogen (BUN) is 32 mg/dL, creatinine 1.1 mg/dL, and hematocrit 50%. Which of the following nursing interventions is appropriate?
Explanation
Choice A Reason: This is incorrect because the results are not within the expected reference range. The client's BUN, creatinine, and hematocrit are elevated, indicating dehydration or reduced renal perfusion.
Choice B Reason: This is correct because evaluating urine for amount and for specific gravity can help assess the client's hydration status and renal function. These actions can help assess the client's hydration status and renal function, which may be affected by nausea and vomiting. The client's BUN, creatinine, and hematocrit are elevated, indicating dehydration or reduced renal perfusion. The normal ranges for BUN are 7 to 20 mg/dL, for creatinine are
0.6 to 1.2 mg/dL, and for hematocrit are 38% to 50% for males. The nurse should monitor the urine output and specific gravity, which reflect the concentration and volume of urine. The normal range for urine output is 30 to 60 mL/hour, and for specific gravity is 1.005 to 1.030.
Choice C Reason: This is incorrect because collecting a urine specimen for culture and sensitivity is not indicated for this client. This action is used to diagnose urinary tract infections, which are not suggested by the client's symptoms or results.
Choice D Reason: This is incorrect because decreasing the IV fluid infusion rate and limiting oral fluid intake can worsen the client's dehydration and renal perfusion. The nurse should maintain adequate fluid intake and balance to prevent further complications.
A nurse is participating in a biological disaster simulation where citizens are exposed to pneumonic plague. Which of the following interventions should the nurse plan to use while caring for these clients?
Explanation
Choice A Reason: This is incorrect because droplet precautions are not sufficient to prevent the transmission of pneumonic plague. Droplet precautions are used to prevent the spread of infectious agents that are expelled through coughing, sneezing, or talking and travel only a short distance in the air. Droplet precautions include wearing a surgical mask, gown, and gloves, and placing the client in a private room or with a roommate who has the same infection.
Choice B Reason: This is incorrect because administering an antitoxin is not an intervention for pneumonic plague. An antitoxin is a substance that neutralizes the effects of a toxin produced by a microorganism. Pneumonic plague is not caused by a toxin, but by a bacterial infection.
Choice C Reason: This is correct because initiating airborne precautions is an intervention for pneumonic plague. Airborne precautions are used to prevent the spread of infectious agents that can remain suspended in the air and travel over long distances. Pneumonic plague is a severe and potentially fatal infection caused by the bacterium Yersinia pestis, which can be transmited through respiratory droplets or aerosols. Airborne precautions are used to prevent the spread of infectious agents that can remain suspended in the air and travel over long distances. Airborne precautions include wearing a respirator or N95 mask, placing the client in a negative-pressure room with an air filtration system, and limiting visitors and staff contact.
Choice D Reason: This is incorrect because destroying the linens after use is not an intervention for pneumonic plague. Linens that are contaminated with body fluids or secretions should be handled with gloves and placed in leak-proof bags for laundering or disposal, but they do not need to be destroyed.

A nurse is caring for a client who has a cardiopulmonary arrest. The nurse anticipates the emergency response team will administer which of the following medications if the client's restored rhythm is symptomatic bradycardia?
Explanation
Choice A Reason: This is incorrect because magnesium is not a medication for symptomatic bradycardia. Magnesium is a mineral that regulates muscle and nerve function, blood pressure, and blood sugar levels. Magnesium can be used to treat conditions such as torsades de pointes, eclampsia, or hypomagnesemia.
Choice B Reason: This is incorrect because sodium bicarbonate is not a medication for symptomatic bradycardia. Sodium bicarbonate is a substance that neutralizes acids and bases and regulates the pH of the blood. Sodium bicarbonate can be used to treat conditions such as metabolic acidosis, cardiac arrest, or overdose of certain drugs.
Choice C Reason: This is incorrect because epinephrine is not a medication for symptomatic bradycardia. Epinephrine is a hormone that activates the sympathetic nervous system and increases the heart rate, blood pressure, and blood flow to the muscles and brain. Epinephrine can be used to treat conditions such as anaphylaxis, cardiac arrest, or severe asthma.
Choice D Reason: This is correct because atropine is a medication for symptomatic bradycardia. Atropine blocks the action of the parasympathetic nervous system and increases the heart rate and conduction. Atropine is a medication that blocks the action of the parasympathetic nervous system and increases the heart rate and conduction.
Symptomatic bradycardia is a condition where the heart rate is slower than normal and causes symptoms such as dizziness, fatigue, chest pain, or fainting. Atropine can be used to treat symptomatic bradycardia by stimulating the sinoatrial node and the atrioventricular node, which are the natural pacemakers of the heart.

A nurse is triaging victims of a multiple motor-vehicle crash. The nurse assesses a client trapped under a car who is apneic and has a weak pulse at 120/min. After repositioning his upper airway, the client remains apneic. Which of the following actions should the nurse take?
Explanation
Choice A Reason: This is incorrect because placing a black tag on the client’s upper body indicates that he is deceased or expectant, which means he has no chance of survival. The nurse should not abandon the client without atempting to provide any care or assistance.
Choice B Reason: This is incorrect because starting CPR is not appropriate for this client at this time. CPR is indicated for clients who have no pulse and no breathing, which means they are in cardiac arrest. The client has a weak pulse, which means he has some cardiac activity, but no breathing. The nurse should focus on restoring his breathing and oxygenation first.
Choice C Reason: This is correct because placing a red tag on the client’s upper body and obtaining immediate help from other personnel indicates that he has an immediate or life-threatening condition that requires urgent intervention. This action indicates that the client has an immediate or life-threatening condition that requires urgent intervention. The client is apneic, which means he is not breathing and has no oxygen exchange. The nurse should place a red tag on the client to signal his priority status and seek help from other personnel to extricate him from under the car and provide advanced airway management.
Choice D Reason: This is incorrect because repositioning the client's upper airway a second time before assessing his respirations is not likely to improve his condition. The nurse has already repositioned his upper airway once and found no improvement in his breathing. The client may have other injuries or obstructions that prevent him from breathing normally.
A nurse is caring for a client who is at risk for shock. Which of the following findings is the earliest indicator that this complication is developing?
Explanation
Choice A Reason: This is incorrect because a decreased level of consciousness is a late sign of shock, not an early one. Decreased level of consciousness indicates that the brain is not receiving enough oxygen and blood flow, which can lead to irreversible damage and death.
Choice B Reason: This is correct because increased respiratory rate is an early sign of shock, indicating hypoxia. This finding indicates that the client is experiencing hypoxia, which is a lack of oxygen in the tissues and organs. Hypoxia is a common and early sign of shock, which is a condition where the body's vital organs do not receive enough blood
flow and oxygen due to low blood pressure, low cardiac output, or low blood volume. The client's respiratory rate increases as a compensatory mechanism to increase oxygen intake and delivery.
Choice C Reason: This is incorrect because hypotension is a late sign of shock, not an early one. Hypotension indicates that the blood pressure is too low to maintain adequate perfusion and oxygenation to the vital organs.
Choice D Reason: This is incorrect because anuria is a late sign of shock, not an early one. Anuria indicates that the kidneys are not receiving enough blood flow and oxygen, which can result in acute kidney injury or failure.
A nurse in a cardiac care unit is caring for a client with acute right-sided heart failure. Which of the following findings should the nurse expect?
Explanation
Choice A: Decreased specific gravity is not a finding of right-sided heart failure. Specific gravity is a measure of urine concentration, which can be affected by fluid intake, dehydration, kidney function, and diuretic use. Right-sided heart failure does not directly affect urine concentration, but it can cause fluid retention and edema in the body.
Choice B: Decreased brain natriuretic peptide (BNP) is not a finding of right-sided heart failure. BNP is a hormone that is released by the heart when it is stretched or overloaded. BNP helps to lower blood pressure and reduce fluid volume by increasing urine output and dilating blood vessels. BNP levels are elevated in both left-sided and right- sided heart failure, as the heart is under increased pressure and volume.
Choice C: Increased pulmonary artery wedge pressure (PAWP) is not a finding of right-sided heart failure. PAWP is a measure of the pressure in the left atrium, which reflects the pressure in the pulmonary capillaries. PAWP is elevated in left-sided heart failure, as the blood backs up in the lungs due to impaired left ventricular function. PAWP is normal or low in right-sided heart failure, as the blood backs up in the systemic circulation due to impaired right ventricular function.
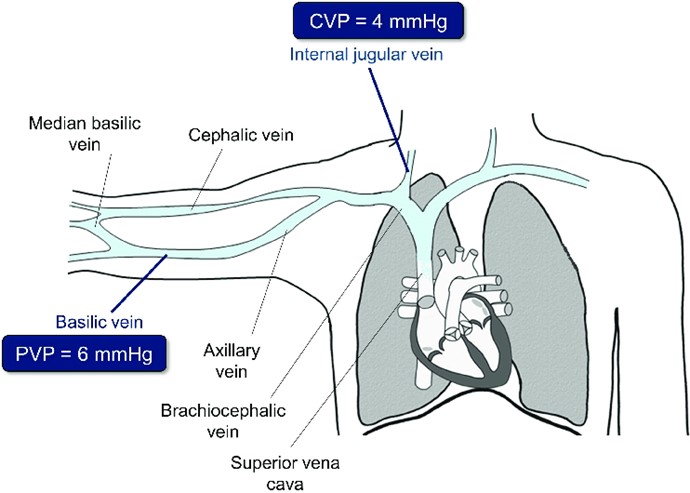
Choice D: Elevated central venous pressure (CVP) is a finding of right-sided heart failure. CVP is a measure of the pressure in the right atrium, which reflects the pressure in the systemic venous system. CVP is elevated in right-sided heart failure, as the blood backs up in the body due to impaired right ventricular function. CVP can cause jugular venous distension, hepatomegaly, splenomegaly, ascites, and peripheral edema.
A nurse is caring for a client who has valvular heart disease and is at risk for developing left-sided heart failure. Which of the following manifestations should alert the nurse that the client is developing this condition?
Explanation
Choice A: Weight gain is not a manifestation of left-sided heart failure. Weight gain is more likely to occur in right-sided heart failure, as the blood backs up in the systemic circulation and causes fluid retention and edema in the body.
Choice B: Anorexia is not a manifestation of left-sided heart failure. Anorexia is a loss of appetite, which can have many causes, such as psychological disorders, infections, medications, or cancer. Left-sided heart failure does not directly affect appetite, but it can cause nausea, fatigue, and weakness.
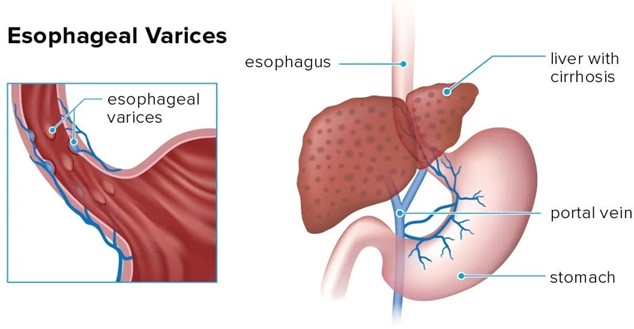
Choice C: A distended abdomen is not a manifestation of left-sided heart failure. A distended abdomen is more likely to occur in right-sided heart failure, as the blood backs up in the portal vein and causes increased pressure in the liver and spleen. This can lead to hepatomegaly, splenomegaly, ascites, and varices.
Choice D: Breathlessness is a manifestation of left-sided heart failure. Breathlessness, or dyspnea, is a sensation of difficulty breathing or shortness of breath. Breathlessness occurs in left-sided heart failure, as the blood backs up in the lungs and causes pulmonary congestion and edema. This impairs gas exchange and reduces oxygen delivery to the tissues.
A nurse is caring for a client who was admited with bleeding esophageal varices and has an esophagogastric balloon tamponade with a Sengstaken-Blakemore tube to control the bleeding. Which of the following actions should the nurse take?
Explanation
Choice A: Provide frequent oral and nares care is the correct action for the nurse to take. Oral and nares care can help prevent infection, dryness, and irritation of the mucous membranes, which can be damaged by the pressure and friction of the tube. The nurse should also monitor the tube position, secure it with tape, and keep scissors at the bedside in case of emergency deflation.
Choice B: Keep the client in a supine position is not the correct action for the nurse to take. The supine position can increase the risk of aspiration, regurgitation, and gastric distension, which can worsen the bleeding and compromise the airway. The nurse should elevate the head of the bed to at least 30 degrees and use a semi-Fowler's or high-Fowler's position.
Choice C: Ambulating the client four times per day is not the correct action for the nurse to take. Ambulation can increase abdominal pressure and dislodge the tube, which can cause bleeding and perforation. The nurse should keep the client on bed rest and use passive range-of-motion exercises to prevent complications such as thromboembolism and muscle atrophy.
Choice D: Encouraging the client to consume clear liquids is not the correct action for the nurse to take. Clear liquids can increase gastric volume and acidity, which can aggravate the bleeding and interfere with hemostasis. The nurse should maintain a nothing-by-mouth status and provide intravenous fluids and nutrition as prescribed.
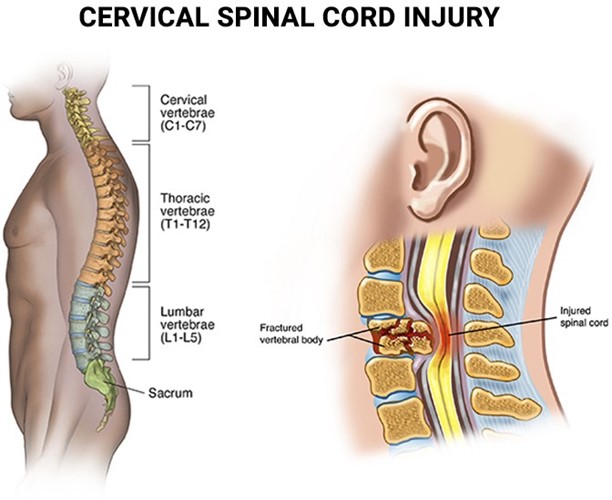
A nurse in the emergency department is monitoring a client who has a cervical spinal cord injury from a fall. The nurse should monitor the client for which of the following complications? (Select all that apply.)
Explanation
Choice A: Weakened gag reflex is a complication of cervical spinal cord injury. The gag reflex is a protective mechanism that prevents choking and aspiration. It is controlled by the cranial nerves IX and X, which originate from the brainstem. A cervical spinal cord injury can impair the transmission of nerve impulses from the brainstem to the pharynx and larynx, resulting in a reduced or absent gag reflex. This can increase the risk of aspiration pneumonia and respiratory failure.
Choice B: Hyperthermia is a complication of cervical spinal cord injury. Hyperthermia is an abnormally high body temperature, which can be caused by infection, inflammation, or environmental factors. A cervical spinal cord injury can disrupt the sympathetic nervous system, which regulates body temperature by controlling blood flow, sweating, and shivering. This can lead to impaired thermoregulation and hyperthermia, especially in hot and humid environments.
Choice C: Absence of bowel sounds is not a complication of cervical spinal cord injury. Bowel sounds are audible noises produced by the movement of gas and fluid through the intestines. They are influenced by factors such as diet, activity, medication, and bowel motility. A cervical spinal cord injury does not directly affect bowel sounds, but it
can cause neurogenic bowel dysfunction, which is a loss of voluntary control over bowel movements. This can lead to constipation, fecal impaction, or incontinence.
Choice D: Paralysis is a complication of cervical spinal cord injury. Paralysis is a loss of voluntary muscle movement and sensation in a part of the body. It is caused by damage to the motor and sensory neurons that carry signals from the brain to the muscles and skin. A cervical spinal cord injury can damage the neurons that innervate the arms, trunk, legs, and pelvic organs, resulting in quadriplegia or tetraplegia, which is paralysis of all four limbs and the trunk.
Choice E: Polyuria is not a complication of cervical spinal cord injury. Polyuria is an excessive production of urine, which can be caused by diabetes mellitus, diabetes insipidus, diuretics, or kidney disease. A cervical spinal cord injury does not directly affect urine production, but it can cause neurogenic bladder dysfunction, which is a loss of voluntary control over bladder function. This can lead to urinary retention, overflow incontinence, or reflex incontinence.
Choice F: Hypotension is a complication of cervical spinal cord injury. Hypotension is an abnormally low blood pressure, which can be caused by blood loss, dehydration, shock, or medication. A cervical spinal cord injury can impair the sympathetic nervous system, which regulates blood pressure by controlling heart rate, cardiac output, and vascular tone. This can lead to neurogenic shock, which is a type of distributive shock characterized by hypotension and bradycardia.
A nurse is caring for a client who has increased intracranial pressure. Which of the following interventions should the nurse take?
Explanation
Choice A: Provide a brightly lit environment is not an intervention that the nurse should take. A brightly lit environment can stimulate the brain and increase intracranial pressure. The nurse should provide a quiet and dimly lit environment to reduce sensory stimuli and promote rest.
Choice B: Elevate the head of the bed is an intervention that the nurse should take. Elevating the head of the bed to 30 degrees can help reduce intracranial pressure by facilitating venous drainage from the brain and decreasing cerebral blood volume. The nurse should avoid flexing or extending the neck, which can impede blood flow and increase intracranial pressure.
Choice C: Encourage a minimum intake of 2000 mL (67.6 oz) of clear fluids per day is not an intervention that the nurse should take. A high fluid intake can increase intracranial pressure by increasing blood volume and cerebral edema. The nurse should monitor fluid balance and restrict fluid intake as prescribed to maintain normal osmolality and prevent fluid overload.
Choice D: Teach controlled coughing and deep breathing is not an intervention that the nurse should take. Coughing and deep breathing can increase intrathoracic pressure, which can increase intracranial pressure by reducing venous return from the brain. The nurse should avoid activities that can increase intrathoracic pressure, such as straining, sneezing, or blowing the nose. The nurse should also administer oxygen as prescribed to maintain adequate oxygenation and perfusion of the brain.
A nurse is collecting a medication history from a client who is scheduled to have a cardiac catheterization. Which of the following medications taken by the client interacts with contrast material and places the client at risk for acute kidney injury?
Explanation
Choice A: Carvedilol is not a medication that interacts with contrast material and places the client at risk for acute kidney injury. Carvedilol is a beta-blocker that lowers blood pressure and heart rate by blocking the effects of adrenaline on the heart and blood vessels. Carvedilol does not affect kidney function or contrast excretion, but it can cause hypotension, bradycardia, or heart failure in some clients.
Choice B: Nitroglycerin is not a medication that interacts with contrast material and places the client at risk for acute kidney injury. Nitroglycerin is a vasodilator that relaxes the smooth muscles of the blood vessels and increases blood flow to the heart. Nitroglycerin does not affect kidney function or contrast excretion, but it can cause hypotension, headache, or flushing in some clients.
Choice C: Atorvastatin is not a medication that interacts with contrast material and places the client at risk for acute kidney injury. Atorvastatin is a statin that lowers cholesterol levels by inhibiting an enzyme that produces cholesterol in the liver. Atorvastatin does not affect kidney function or contrast excretion, but it can cause liver damage, muscle pain, or rhabdomyolysis in some clients.
Choice D: Metformin is a medication that interacts with contrast material and places the client at risk for acute kidney injury. Metformin is an oral antidiabetic drug that lowers blood glucose levels by decreasing hepatic glucose production and increasing insulin sensitivity. Metformin can accumulate in the kidneys and cause lactic acidosis, a life-threatening condition characterized by high levels of lactic acid in the blood. Contrast material can worsen kidney function and increase the risk of lactic acidosis in clients taking metformin. Therefore, metformin should be discontinued before and after the procedure as prescribed.

A nurse is reviewing a client's laboratory values. Which of the following values should the nurse report to the provider?
Explanation
Choice A: Hct 45% is not a value that the nurse should report to the provider. Hct, or hematocrit, is the percentage of red blood cells in the total blood volume. The normal range for Hct is 37% to 51% for men and 32% to 45% for women. Hct 45% is within the normal range and does not indicate any abnormality.
Choice B: Platelets 160,000/mm³ is not a value that the nurse should report to the provider. Platelets, or thrombocytes, are cell fragments that help with blood clotting and hemostasis. The normal range for platelets is 150,000 to 450,000/mm³. Platelets 160,000/mm³ is within the normal range and does not indicate any abnormality.
Choice C: WBC 1,700/mm³ is a value that the nurse should report to the provider. WBC, or white blood cells, are cells that fight infection and inflammation. The normal range for WBC is 4,500 to 11,000/mm³. WBC 1,700/mm³ is below the normal range and indicates leukopenia, which is a low number of white blood cells. Leukopenia can be caused by various conditions, such as viral infections, autoimmune disorders, bone marrow suppression, or chemotherapy. Leukopenia can increase the risk of infection and sepsis and requires prompt evaluation and treatment.
Choice D: Hgb 14.7 g/dL is not a value that the nurse should report to the provider. Hgb, or hemoglobin, is a protein in red blood cells that carries oxygen to the tissues. The normal range for Hgb is 13.5 to 17.5 g/dL for men and 12.0 to 15.5 g/dL for women. Hgb 14.7 g/dL is within the normal range and does not indicate any abnormality.
A nurse is providing discharge teaching to a client who has a new arteriovenous fistula in the right forearm. Which of the following manifestations should the nurse include in the teaching as a possible indication of venous insufficiency?
Explanation
Choice A: Cold and numb sensation distal to the fistula site is a possible indication of venous insufficiency. Venous insufficiency is a condition in which the veins have difficulty returning blood from the limbs to the heart, resulting in blood pooling and reduced perfusion. A new arteriovenous fistula can cause increased blood flow through the artery and decreased blood flow through the vein, leading to venous insufficiency. This can manifest as coldness, numbness, tingling, or cyanosis in the fingers or hand below the fistula site.
Choice B: A raised red rash around the fistula site is not a possible indication of venous insufficiency. A raised red rash around the fistula site can indicate an allergic reaction, an infection, or an inflammation of the skin or subcutaneous tissue. The nurse should assess the rash for size, shape, color, texture, temperature, and drainage, and report any signs of infection or inflammation, such as fever, pus, or swelling.
Choice C: Pain in the right arm proximal to the fistula site is not a possible indication of venous insufficiency. Pain in the right arm proximal to the fistula site can indicate arterial insufficiency, which is a condition in which the arteries have difficulty delivering oxygen-rich blood to the tissues, resulting in ischemia and necrosis. Arterial insufficiency can be caused by atherosclerosis, thrombosis, embolism, or vasospasm. The nurse should assess the pain for location, intensity, duration, frequency, and quality, and report any signs of ischemia or necrosis, such as pallor, coolness, weak pulses, or ulceration.
Choice D: Foul-smelling drainage from the fistula site is not a possible indication of venous insufficiency. Foul-smelling drainage from the fistula site can indicate an infection of the fistula or surrounding tissue. The nurse should assess the drainage for color, odor, amount, and consistency, and report any signs of infection or sepsis, such as fever, chills, malaise, or hypotension.
A nurse is assisting with obtaining an electrocardiogram (ECG) for a client who has atrial fibrillation. Which of the following actions should the nurse take? (Select all that apply.)
Explanation
Choice A: Inspecting the electrode pads is an action that the nurse should take. The electrode pads are adhesive patches that atach to the skin and connect to the ECG machine. The nurse should inspect the electrode pads for expiration date, cleanliness, and stickiness, and replace them if necessary. The nurse should also check for any signs of skin irritation or allergy from the electrode pads.
Choice B: Instructing the client not to talk during the test is an action that the nurse should take. Talking during the test can interfere with the ECG recording and cause artifacts or false readings. The nurse should instruct the client to remain still and quiet during the test, and avoid any movements or activities that can affect the heart rate or rhythm, such as coughing, deep breathing, or shivering.
Choice C: Administering an analgesic prior to the procedure is not an action that the nurse should take. An analgesic is a pain reliever that can be given orally, intravenously, or topically. An analgesic is not necessary for an ECG, as it is a noninvasive and painless procedure. An analgesic can also alter the heart rate or rhythm and affect the ECG results. The nurse should only administer an analgesic if prescribed by the provider for another reason.
Choice D: Washing the skin with plain water before placing the electrodes is an action that the nurse should take. Washing the skin with plain water can help remove any dirt, oil, or lotion that can interfere with the electrical conductivity and signal quality of the electrodes. The nurse should avoid using alcohol, soap, or antiseptic solutions, as they can irritate or dry out the skin and cause poor adhesion or contact of the electrodes.
Choice E: Keeping the client NPO after midnight is not an action that the nurse should take. NPO means nothing by mouth, which is a restriction of food and fluids before certain procedures or surgeries. NPO is not required for an ECG, as it does not involve any anesthesia or sedation. The nurse should allow the client to eat and drink normally before and after the test, unless instructed otherwise by the provider.
Sign Up or Login to view all the 50 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

