ATI Med Surg Custom N235 Final Summer 2023
Total Questions : 70
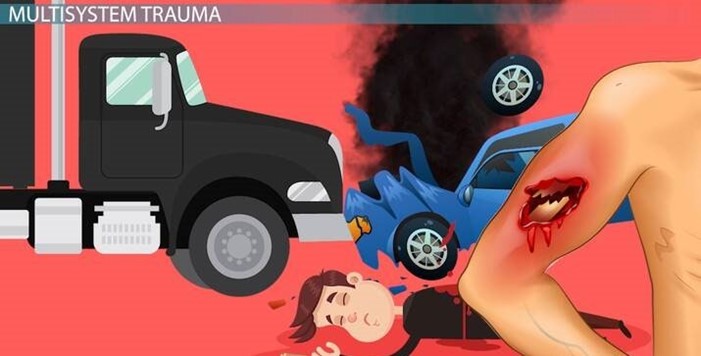
Showing 25 questions, Sign in for moreA nurse in an emergency department is preparing to care for a client who is being brought in with multiple system trauma following a motor vehicle crash. Which of the following should the nurse identify as the priority focus of care?
Explanation
Choice A Reason: Preventing musculoskeletal disability is important, but not the priority focus of care. The nurse should first assess and manage the client's life-threatening injuries, such as airway obstruction, bleeding, shock, or brain injury.
Choice B Reason: Airway protection is the priority focus of care for a client with multiple system trauma. The nurse should ensure that the client has a patent airway and adequate ventilation, as any compromise in these areas can quickly lead to hypoxia, respiratory failure, and death.
Choice C Reason: Stabilizing cardiac arrhythmias is also important, but not the priority focus of care. The nurse should monitor the client's cardiac rhythm and treat any arrhythmias that may occur, but only after securing the airway and breathing.
Choice D Reason: Decreasing intracranial pressure is another important goal, but not the priority focus of care. The nurse should assess the client's neurological status and intervene to prevent or reduce increased intracranial pressure, such as elevating the head of the bed, maintaining normothermia, and administering osmotic diuretics. However, these measures are secondary to ensuring adequate oxygenation and perfusion.
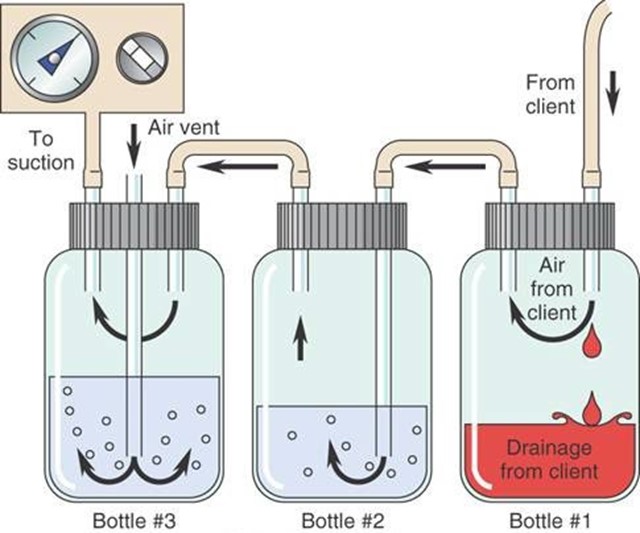
The nurse is caring for a postoperative client who has a chest tube connected to suction and a water seal drainage system. Which of the following indicates to the nurse that the chest tube is functioning properly?
Explanation
Choice A Reason: Equal amount of fluid drainage in each collection chamber is not a sign of proper chest tube function. The amount of fluid drainage depends on the type and extent of the client's injury or surgery, and may vary from one chamber to another.
Choice B Reason: Fluctuation of the fluid level within the water seal chamber is a sign of proper chest tube function. It indicates that the chest tube is patent and that there is no air leak in the system. The fluid level should rise and fall with the client's respiratory cycle.
Choice C Reason: Continuous bubbling within the water seal chamber is not a sign of proper chest tube function. It indicates that there is an air leak in the system, either from the client's pleural space or from a loose connection. The nurse should locate and correct the source of the leak.
Choice D Reason: Absence of fluid in the drainage tubing is not a sign of proper chest tube function. It may indicate that the chest tube is obstructed, kinked, or clamped, or that the suction is not working properly. The nurse should assess and troubleshoot the chest tube system.
A nurse in the emergency department is caring for a client who has extensive partial and full-thickness burns of the head, neck, and chest. While planning the client's care, the nurse should identify which of the following risks as the priority for assessment and intervention?
Explanation
Choice A Reason: Infection is a serious complication of burn injuries, but not the priority risk for assessment and intervention. The nurse should monitor the client's wound healing, temperature, white blood cell count, and signs of sepsis, and administer antibiotics as prescribed. However, these measures are secondary to ensuring adequate oxygenation and ventilation.
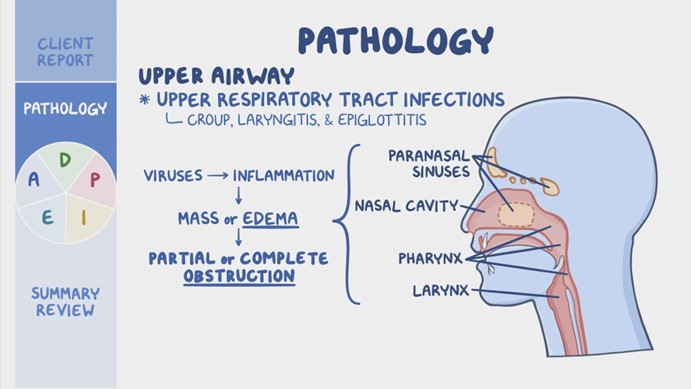
Choice B Reason: Airway obstruction is the priority risk for assessment and intervention for a client who has burns of the head, neck, and chest. The nurse should assess the client's airway patency, respiratory rate, oxygen saturation, breath sounds, and signs of respiratory distress, such as stridor, wheezes, or cyanosis. The nurse should also provide humidified oxygen, suction secretions, elevate the head of the bed, and prepare for endotracheal intubation if needed. Airway obstruction can occur due to edema, inflammation, or inhalation injury of the upper airway, and can quickly lead to hypoxia, respiratory failure, and death.
Choice C Reason: Paralytic ileus is a potential complication of burn injuries, but not the priority risk for assessment and intervention. The nurse should assess the client's bowel sounds, abdominal distension, nausea, vomiting, and stool output, and administer fluids, electrolytes, and nutritional support as prescribed. However, these measures are secondary to ensuring adequate oxygenation and ventilation.
Choice D Reason: Fluid imbalance is another potential complication of burn injuries, but not the priority risk for assessment and intervention. The nurse should assess the client's fluid status, urine output, vital signs, weight, and serum electrolytes, and administer intravenous fluids as prescribed. However, these measures are secondary to ensuring adequate oxygenation and ventilation.
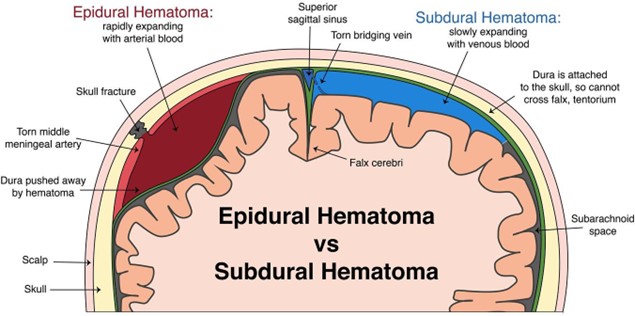
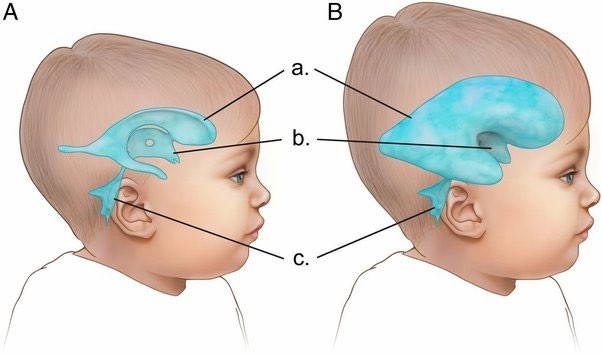
A nurse is caring for a client who had an evacuation of a subdural hematoma. Which of the following actions should the nurse take first?
Explanation
Choice A Reason: Observing for cerebrospinal fluid (CSF) leaks from the evacuation site is important, but not the first action that the nurse should take. CSF leaks can indicate a breach in the dura mater, which can increase the risk of infection and meningitis. The nurse should inspect the dressing and the nose and ears for any clear or bloody drainage, and report any findings to the provider. However, these measures are secondary to ensuring adequate oxygenation and perfusion.
Choice B Reason: Checking the oximeter is also important, but not the first action that the nurse should take. The oximeter measures the oxygen saturation of the blood, which reflects the adequacy of gas exchange in the lungs. The nurse should maintain the oxygen saturation above 90%, and administer supplemental oxygen as prescribed.
However, these measures are secondary to ensuring adequate oxygenation and perfusion.
Choice C Reason: Assessing for an increase in temperature is another important action, but not the first one that the nurse should take. An increase in temperature can indicate an infection, inflammation, or damage to the hypothalamus, which can affect the thermoregulation of the body. The nurse should monitor the temperature and administer antipyretics as prescribed. However, these measures are secondary to ensuring adequate oxygenation and perfusion.
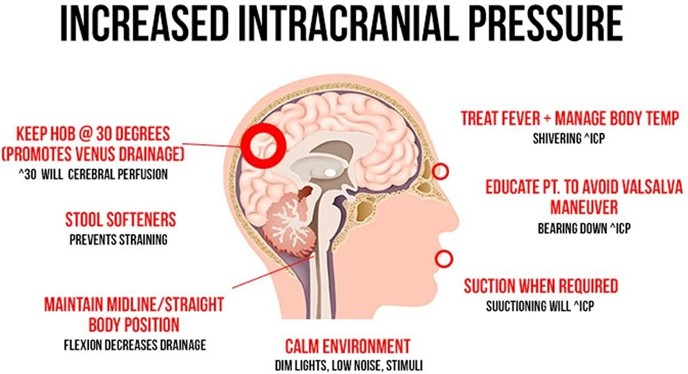
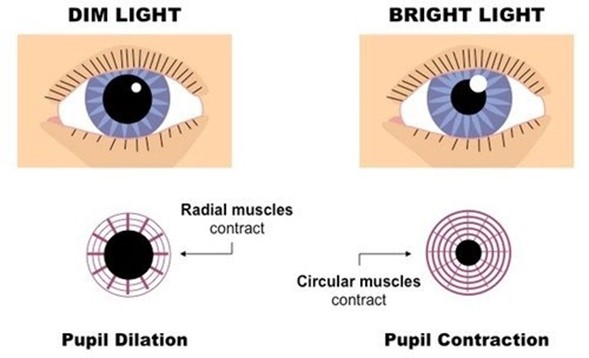
Choice D Reason: Monitoring for manifestations of increased intracranial pressure is the first action that the nurse should take. Increased intracranial pressure can result from bleeding, swelling, or fluid accumulation in the brain, which can compress and damage brain tissue and blood vessels. The nurse should assess for signs and symptoms of increased intracranial pressure, such as headache, nausea, vomiting, altered level of consciousness, pupillary changes, or Cushing's triad (bradycardia, hypertension, and irregular respirations). The nurse should also intervene to prevent or reduce increased intracranial pressure, such as elevating the head of the bed, maintaining normothermia, and administering osmotic diuretics. Monitoring for manifestations of increased intracranial pressure is essential to prevent further brain injury and preserve neurological function.
A nurse is caring for a client who had an evacuation of a subdural hematoma. Which of the following actions should the nurse take first?
Explanation
Choice A Reason: Observing for cerebrospinal fluid (CSF) leaks from the evacuation site is important, but not the first action that the nurse should take. CSF leaks can indicate a breach in the dura mater, which can increase the risk of infection and meningitis. The nurse should inspect the dressing and the nose and ears for any clear or bloody drainage, and report any findings to the provider. However, these measures are secondary to ensuring adequate oxygenation and perfusion.
Choice B Reason: Checking the oximeter is also important, but not the first action that the nurse should take. The oximeter measures the oxygen saturation of the blood, which reflects the adequacy of gas exchange in the lungs. The nurse should maintain the oxygen saturation above 90%, and administer supplemental oxygen as prescribed.
However, these measures are secondary to ensuring adequate oxygenation and perfusion.
Choice C Reason: Assessing for an increase in temperature is another important action, but not the first one that the nurse should take. An increase in temperature can indicate an infection, inflammation, or damage to the hypothalamus, which can affect the thermoregulation of the body. The nurse should monitor the temperature and administer antipyretics as prescribed. However, these measures are secondary to ensuring adequate oxygenation and perfusion.
Choice D Reason: Monitoring for manifestations of increased intracranial pressure is the first action that the nurse should take. Increased intracranial pressure can result from bleeding, swelling, or fluid accumulation in the brain, which can compress and damage brain tissue and blood vessels. The nurse should assess for signs and symptoms of increased intracranial pressure, such as headache, nausea, vomiting, altered level of consciousness, pupillary changes, or Cushing's triad (bradycardia, hypertension, and irregular respirations). The nurse should also intervene to prevent or reduce increased intracranial pressure, such as elevating the head of the bed, maintaining normothermia, and administering osmotic diuretics. Monitoring for manifestations of increased intracranial pressure is essential to prevent further brain injury and preserve neurological function.
A nurse is monitoring a client who was admited with a severe burn injury and is receiving IV fluid resuscitation therapy. The nurse should identify a decrease in which of the following findings as an indication of adequate fluid replacement?
Explanation
Choice A Reason: Urine output is not a finding that should decrease with adequate fluid replacement. On the contrary, urine output should increase as the fluid therapy restores the renal perfusion and function. The nurse should monitor the urine output and ensure that it is at least 0.5 mL/kg/hr for adults and 1 mL/kg/hr for children.
Choice B Reason: Heart rate is a finding that should decrease with adequate fluid replacement. A high heart rate is a sign of hypovolemia, which occurs when the burn injury causes fluid loss from the intravascular space. The nurse should monitor the heart rate and expect it to decrease as the fluid therapy replenishes the blood volume and improves the cardiac output.
Choice C Reason: Weight is not a finding that should decrease with adequate fluid replacement. On the contrary, weight may increase as the fluid therapy restores the hydration status and corrects the fluid deficit. The nurse should monitor the weight and compare it with the pre-burn weight to evaluate the fluid balance.
Choice D Reason: Blood pressure is not a finding that should decrease with adequate fluid replacement. On the contrary, blood pressure may increase as the fluid therapy restores the vascular tone and improves the tissue perfusion. The nurse should monitor the blood pressure and expect it to increase as the fluid therapy compensates for the fluid loss.
A nurse is caring for a client who has a traumatic head injury and is exhibiting signs of increasing intracranial pressure. Which of the following medications should the nurse plan to administer?
Explanation
Choice A Reason: Dextran 70 is not a medication that the nurse should plan to administer for a client who has a traumatic head injury and is exhibiting signs of increasing intracranial pressure. Dextran 70 is a plasma expander that increases the blood volume and viscosity, which can worsen the intracranial pressure by increasing the cerebral blood flow and edema.
Choice B Reason: Hydroxyethyl starch is not a medication that the nurse should plan to administer for a client who has a traumatic head injury and is exhibiting signs of increasing intracranial pressure. Hydroxyethyl starch is another plasma expander that has similar effects as dextran 70, and can also increase the risk of coagulopathy and renal failure.
Choice C Reason: Albumin 25% is not a medication that the nurse should plan to administer for a client who has a traumatic head injury and is exhibiting signs of increasing intracranial pressure. Albumin 25% is a colloid solution that increases the oncotic pressure and draws fluid from the interstitial space into the intravascular space, which can also worsen the intracranial pressure by increasing the cerebral blood flow and edema.
Choice D Reason: Mannitol 25% is a medication that the nurse should plan to administer for a client who has a traumatic head injury and is exhibiting signs of increasing intracranial pressure. Mannitol 25% is an osmotic diuretic that reduces the intracranial pressure by creating an osmotic gradient and drawing fluid from the brain tissue into the blood vessels, which can then be excreted by the kidneys. The nurse should monitor the urine output, serum osmolality, and electrolytes when administering mannitol 25%.
A nurse is caring for a client who has a deep vein thrombosis and is prescribed heparin by continuous IV infusion at 1,200 units/hr. Available is heparin 25,000 units in 500 mL D5W. The nurse should set the IV pump to deliver how many mL/hr? (Round the answer to the nearest tenth/whole number. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
- To find the concentration of heparin in the solution, divide the amount of heparin by the volume of D5W: 25,000 units / 500 mL = 50 units/mL
- To find the infusion rate, divide the prescribed dose by the concentration: 1,200 units/hr / 50 units/mL = 24 mL/hr
- Round the answer to the nearest tenth/whole number: 24 mL/hr
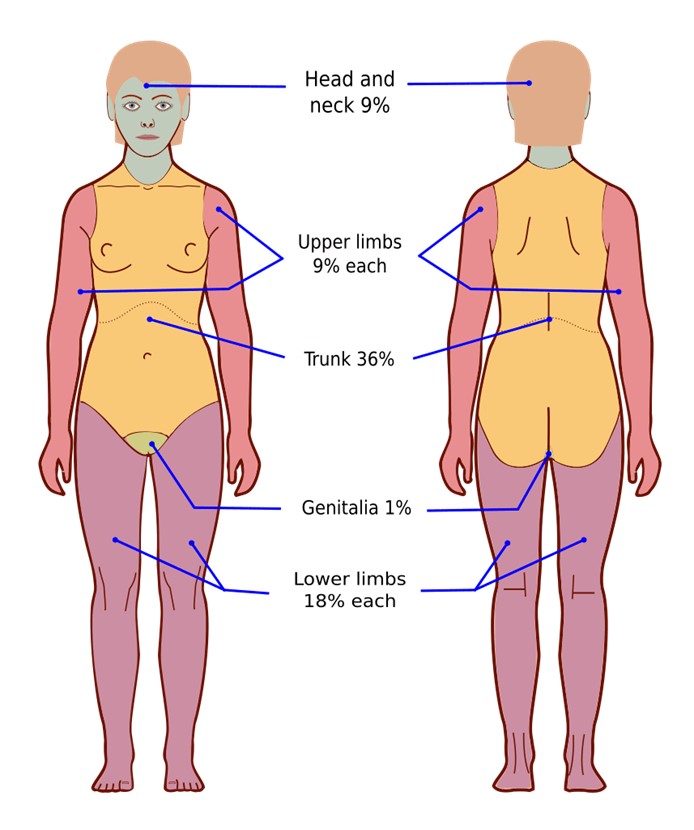
A nurse is assessing the depth and extent of injury on a client who has severe burns to the face, neck, and upper extremities. Which of the following factors is the nurse's priority when assessing the severity of the client's burns?
Explanation
Choice A Reason: Cause of the burn is not the nurse's priority when assessing the severity of the client's burns. The cause of the burn may indicate the type and duration of exposure, such as thermal, chemical, electrical, or radiation, which can affect the depth and extent of injury. However, these factors are secondary to ensuring adequate oxygenation and ventilation.
Choice B Reason: Age of the client is not the nurse's priority when assessing the severity of the client's burns. The age of the client may influence the response to burn injury, such as healing time, infection risk, and fluid requirements.
However, these factors are secondary to ensuring adequate oxygenation and ventilation.
Choice C Reason: Associated medical history is not the nurse's priority when assessing the severity of the client's burns. The associated medical history may affect the outcome and prognosis of burn injury, such as pre-existing conditions, medications, or allergies. However, these factors are secondary to ensuring adequate oxygenation and ventilation.
Choice D Reason: Location of the burn is the nurse's priority when assessing the severity of the client's burns. The location of the burn can indicate the potential for life-threatening complications, such as airway obstruction, inhalation injury, or impaired circulation. The nurse should assess for signs and symptoms of respiratory distress, such as stridor, wheezes, or cyanosis, and prepare for endotracheal intubation if needed. The nurse should also monitor for signs and symptoms of compartment syndrome, such as pain, pallor, paresthesia, pulselessness, or paralysis, and report any findings to the provider. The location of the burn can also affect the functional and cosmetic outcomes, such as vision loss, facial disfigurement, or joint contractures. The nurse should provide appropriate wound care, pain management, and rehabilitation as prescribed. Assessing for location of burn is essential to prevent further injury and preserve vital functions.
A nurse is caring for a client who is experiencing Cushing's triad following a subdural hematoma. Which of the following medications should the nurse plan to administer?
Explanation
Choice A Reason: Albumin 25% is not a medication that the nurse should plan to administer for a client who is experiencing Cushing's triad following a subdural hematoma. Albumin 25% is a colloid solution that increases the oncotic pressure and draws fluid from the interstitial space into the intravascular space, which can worsen the intracranial pressure by increasing the cerebral blood flow and edema.
Choice B Reason: Dextran 70 is not a medication that the nurse should plan to administer for a client who is experiencing Cushing's triad following a subdural hematoma. Dextran 70 is a plasma expander that increases the blood volume and viscosity, which can also worsen the intracranial pressure by increasing the cerebral blood flow and edema.
Choice C Reason: Mannitol 25% is a medication that the nurse should plan to administer for a client who is experiencing Cushing's triad following a subdural hematoma. Mannitol 25% is an osmotic diuretic that reduces the intracranial pressure by creating an osmotic gradient and drawing fluid from the brain tissue into the blood vessels, which can then be excreted by the kidneys. The nurse should monitor the urine output, serum osmolality, and electrolytes when administering mannitol 25%.
Choice D Reason: Hydroxyethyl starch is not a medication that the nurse should plan to administer for a client who is experiencing Cushing's triad following a subdural hematoma. Hydroxyethyl starch is another plasma expander that has similar effects as dextran 70, and can also increase the risk of coagulopathy and renal failure.
A nurse is caring for a client who has a deep vein thrombosis and is prescribed heparin by continuous IV infusion at 1,200 units/hr. Available is heparin 25,000 units in 500 mL D5W. The nurse should set the IV pump to deliver how many mL/hr? (Round the answer to the nearest tenth/whole number. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
- To find the concentration of heparin in the solution, divide the amount of heparin by the volume of D5W: 25,000 units / 500 mL = 50 units/mL
- To find the infusion rate, divide the prescribed dose by the concentration: 1,200 units/hr / 50 units/mL = 24 mL/hr
- Round the answer to the nearest tenth/whole number: 24 mL/hr
A nurse is caring for a client who is experiencing Cushing's triad following a subdural hematoma. Which of the following medications should the nurse plan to administer?
Explanation
Choice A Reason: Albumin 25% is not a medication that the nurse should plan to administer for a client who is experiencing Cushing's triad following a subdural hematoma. Albumin 25% is a colloid solution that increases the oncotic pressure and draws fluid from the interstitial space into the intravascular space, which can worsen the intracranial pressure by increasing the cerebral blood flow and edema.
Choice B Reason: Dextran 70 is not a medication that the nurse should plan to administer for a client who is experiencing Cushing's triad following a subdural hematoma. Dextran 70 is a plasma expander that increases the blood volume and viscosity, which can also worsen the intracranial pressure by increasing the cerebral blood flow and edema.
Choice C Reason: Mannitol 25% is a medication that the nurse should plan to administer for a client who is experiencing Cushing's triad following a subdural hematoma. Mannitol 25% is an osmotic diuretic that reduces the intracranial pressure by creating an osmotic gradient and drawing fluid from the brain tissue into the blood vessels, which can then be excreted by the kidneys. The nurse should monitor the urine output, serum osmolality, and electrolytes when administering mannitol 25%.
Choice D Reason: Hydroxyethyl starch is not a medication that the nurse should plan to administer for a client who is experiencing Cushing's triad following a subdural hematoma. Hydroxyethyl starch is another plasma expander that has similar effects as dextran 70, and can also increase the risk of coagulopathy and renal failure.
A nurse is assessing a client's cranial nerves as part of a neurological examination. Which of the following actions should the nurse take to assess cranial nerve III?
Explanation
Choice A: Eliciting the gag reflex is a way to assess cranial nerve IX (glossopharyngeal) and X (vagus), which are responsible for the sensation and motor function of the pharynx and larynx.
Choice B: Testing visual acuity is a way to assess cranial nerve II (optic), which is responsible for the sense of vision.
Choice C: Observing for facial symmetry is a way to assess cranial nerve VII (facial), which is responsible for the motor function of the facial muscles and the sensation of taste.
Choice D: Checking the pupillary response to light is a way to assess cranial nerve III (oculomotor), which is responsible for the motor function of most of the eye muscles, including those that control pupil size and lens shape.
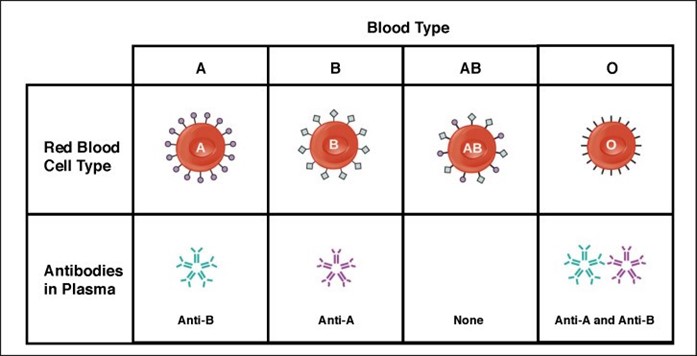
A nurse is preparing to administer blood to a client. The unit of blood on hand is type B, and the client has type AB blood. Which of the following actions should the nurse take?
Explanation
Choice A: Contacting the provider for further orders is not necessary, because the client has type AB blood, which is compatible with any other blood type. The client can receive type B blood without any adverse reactions.
Choice B: Notifying the blood bank of the discrepancy is not required, because there is no discrepancy. The blood bank sent the correct type of blood for the client, according to their blood type.
Choice C: Administering the blood as ordered is the correct action, because type B blood is compatible with type AB blood. The client will not have any transfusion reactions or complications from receiving this type of blood.
Choice D: Completing an incident report is not appropriate, because there is no incident. The nurse did not make any error or mistake in administering the blood to the client. There is no need to document or report anything unusual.
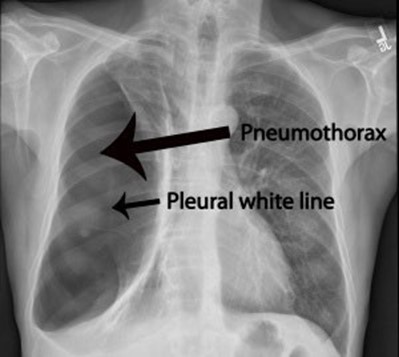
The nurse in a trauma unit has received a report on a client who has multiple injuries following a motor vehicle crash. Which of the following actions should the nurse plan to take first?
Explanation
Choice A: Evaluating chest expansion is the first action that the nurse should take, because it assesses the client's respiratory status and potential for pneumothorax, which is a life-threatening condition that can result from chest trauma. The nurse should compare the movement of both sides of the chest and listen for breath sounds.
Choice B: Checking pupillary response to light is an important action, but not the first one, because it assesses the client's neurological status and potential for brain injury. The nurse should observe the size, shape, and symmetry of the pupils and their reaction to light.
Choice C: Checking the client's response to questions about place and time is another important action, but not the first one, because it assesses the client's level of consciousness and orientation. The nurse should ask the client simple questions such as their name, date, and location.
Choice D: Assessing the capillary refill is a less important action, and not the first one, because it assesses the client's peripheral circulation and tissue perfusion. The nurse should press on the client's nail beds or fingertips and observe how quickly the color returns.
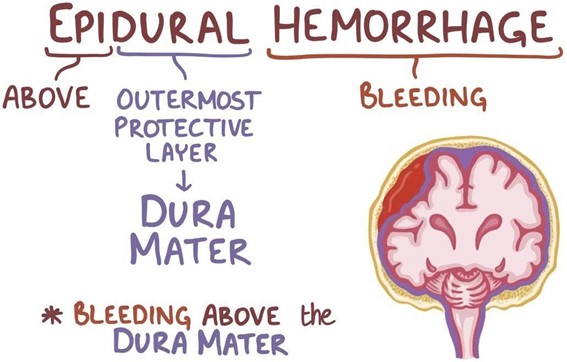
A nurse in the emergency department is caring for a client who has an epidural hematoma following a motor-vehicle crash. Which of the following is an expected finding for this client?
Explanation
Choice A: Drainage of clear fluid from the ears is not an expected finding for a client who has an epidural hematoma, but rather a sign of a basilar skull fracture, which is a different type of head injury. The clear fluid is cerebrospinal fluid (CSF), which leaks from the brain through the fractured skull.
Choice B: Alternating periods of alertness and unconsciousness is an expected finding for a client who has an epidural hematoma, because it indicates a rapid increase in intracranial pressure (ICP) due to bleeding between the dura mater and the skull. The client may have a brief loss of consciousness at the time of injury, followed by a lucid interval, and then a rapid deterioration of mental status.
Choice C: Narrowing pulse pressure is not an expected finding for a client who has an epidural hematoma, but rather a sign of increased ICP due to any cause. Pulse pressure is the difference between systolic and diastolic blood pressure. As ICP rises, it compresses the brainstem and causes bradycardia and hypertension, resulting in a decreased pulse pressure.
Choice D: Extensive bruising in the mastoid area is not an expected finding for a client who has an epidural hematoma, but rather a sign of a basilar skull fracture, which is a different type of head injury. The bruising is also known as Batle's sign, and it occurs due to blood pooling behind the ear.
A nurse is caring for a client who is experiencing hypovolemic shock. Which of the following blood products should the nurse anticipate administering to this client?
Explanation
Choice A Reason: Packed RBCs are indicated for clients who have hypovolemic shock due to blood loss, as they increase the oxygen-carrying capacity of the blood and restore the blood volume.
Choice B Reason: Cryoprecipitates are indicated for clients who have hemophilia or von Willebrand disease, as they contain clotting factors that help stop bleeding.
Choice C Reason: Albumin is indicated for clients who have hypovolemic shock due to fluid loss, such as from burns or ascites, as it increases the plasma oncotic pressure and draws fluid into the vascular space.
Choice D Reason: Platelets are indicated for clients who have thrombocytopenia or platelet dysfunction, as they help prevent or control bleeding.
A nurse is caring for a client who has a disposable three-chamber chest tube in place. Which of the following findings should indicate to the nurse that the client is experiencing a complication?
Explanation
Choice A Reason: Continuous bubbling in the water-seal chamber indicates an air leak in the chest tube system, which can compromise the drainage of air and fluid from the pleural space and impair lung expansion.
Choice B Reason: Occasional bubbling in the water-seal chamber is normal and expected, as it indicates that air is being removed from the pleural space.
Choice C Reason: Fluctuations in the fluid level in the water-seal chamber are normal and expected, as they reflect changes in intrathoracic pressure during inspiration and expiration.
Choice D Reason: Constant bubbling in the suction-control chamber is normal and expected, as it indicates that suction is being applied to the chest tube system.
A nurse is preparing to administer 40 mEq of potassium chloride in 45% sodium chloride (NaCl) 500 mL IV to infuse 10 mEq/hr. The nurse should set the IV pump to deliver how many mL/hr? (Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
To calculate the infusion rate, you can use the formula: (Desired dose / Concentration) * (Volume / Time).
In thiscase, the desired dose is 10 mEq/hr, the concentration is 40 mEq in 500 mL, and the volume is 500 mL.
So, it would be (10 mEq/hr / 40 mEq/500 mL) * (500 mL / 1 hour) = 25 mL/hr.
This ensures the patient receives the prescribed dose of potassium chloride at the correct rate.
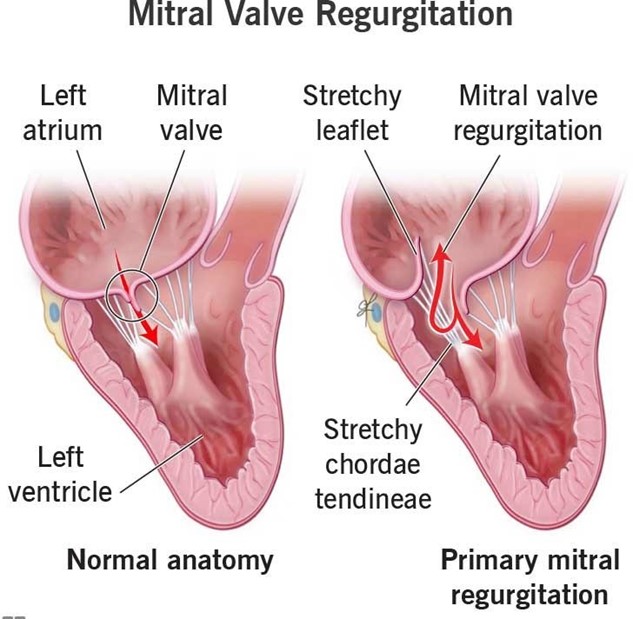
A nurse is monitoring the pulmonary artery wedge pressure (PAWP) for a client. The nurse should identify that a reading of 17 mm Hg is an indication of which of the following conditions?
Explanation
Choice A Reason: This is incorrect because right ventricular failure would cause an increase in right atrial pressure and right ventricular end-diastolic pressure, but not in PAWP, which reflects left atrial pressure and left ventricular end- diastolic pressure.
Choice B Reason: This is incorrect because fluid volume deficit would cause a decrease in PAWP, as there would be less blood volume in the pulmonary circulation.
Choice C Reason: This is correct because mitral regurgitation would cause an increase in PAWP, as the blood would back up into the left atrium and pulmonary veins due to the incompetent mitral valve.
Choice D Reason: This is incorrect because afterload reduction would cause a decrease in PAWP, as there would be less resistance to the left ventricular ejection and less blood volume in the pulmonary circulation.
A nurse is monitoring a client who has a chest tube in place connected to wall suction due to a right-sided pneumothorax. The client complains of chest burning. Which of the following actions should the nurse take?
Explanation
Choice A Reason: This is incorrect because clamping the client's chest tube can cause a tension pneumothorax, which is a life-threatening condition that requires immediate intervention.
Choice B Reason: This is incorrect because increasing the client's wall suction can cause excessive negative pressure in the pleural space, which can damage the lung tissue and impair ventilation.
Choice C Reason: This is correct because repositioning the client can help relieve chest burning, which may be caused by irritation of the intercostal nerves by the chest tube or by air trapping in the pleural space.
Choice D Reason: This is incorrect because stripping the client's chest tube can create high negative pressure in the pleural space, which can damage the lung tissue and impair ventilation.
A nurse is preparing to administer an osmotic diuretic IV to a client with increased intracranial pressure. Which of the following should the nurse identify as the purpose of the medication?
Explanation
Choice A Reason: This is correct because an osmotic diuretic, such as mannitol, works by creating an osmotic gradient that draws fluid from the brain tissue into the blood vessels, thereby reducing cerebral edema and intracranial pressure.
Choice B Reason: This is incorrect because an osmotic diuretic would decrease, not increase, the cell size in the brain by removing fluid from the intracellular space.
Choice C Reason: This is incorrect because an osmotic diuretic would decrease, not expand, the extracellular fluid volume by increasing the urine output and excreting excess fluid from the body.
Choice D Reason: This is incorrect because an osmotic diuretic would not provide fluid hydration, but rather cause fluid loss and dehydration.
A nurse is caring for a client who is unconscious following a cerebral hemorrhage. Which of the following nursing interventions is of highest priority?
Explanation
Choice A Reason: This is incorrect because monitoring the client's electrolyte levels is not the highest priority, as it does not address the immediate risk of airway obstruction or aspiration.
Choice B Reason: This is correct because suctioning saliva from the client's mouth is the highest priority, as it prevents airway obstruction and aspiration, which can lead to respiratory distress and infection.
Choice C Reason: This is incorrect because recording the client's intake and output is not the highest priority, as it does not address the immediate risk of airway obstruction or aspiration.
Choice D Reason: This is incorrect because performing passive range of motion on each extremity is not the highest priority, as it does not address the immediate risk of airway obstruction or aspiration.
A nurse is preparing to administer medications to four clients. The nurse should administer medications to which of the following clients first?
Explanation
Choice A Reason: This is incorrect because a client who is post-CABG and has high cholesterol is not in immediate danger, as atorvastatin is a long-term medication that lowers cholesterol and prevents cardiovascular complications.
Choice B Reason: This is incorrect because a client who has pneumonia and a slightly elevated WBC count is not in immediate danger, as piperacillin is an antibiotic that treats bacterial infections.
Choice C Reason: This is correct because a client who has renal failure and a high serum potassium level is in immediate danger, as sodium polystyrene sulfonate is an emergency medication that lowers potassium and prevents cardiac arrhythmias.
Choice D Reason: This is incorrect because a client who has anemia and a mild hemoglobin deficiency is not in immediate danger, as epoetin alfa is a long-term medication that stimulates red blood cell production and improves oxygen delivery.
A nurse is caring for a client who has a pulmonary embolism and has a new prescription for enoxaparin 1.5 mg/kg/dose subcutaneously every 12 hours. The client weighs 245 lbs. How many mg should the nurse administer per dose? (Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
To calculate the dose of enoxaparin, follow these steps:
1) Convert the client's weight from pounds to kilograms:
245 lbs / 2.2046 (kg/lb) = 111.13 kg (rounded to the nearest whole number, it's 111 kg).
2) Multiply the weight in kilograms by the prescribed dose per kilogram:
111 kg x 1.5 mg/kg = 166.5 mg.
Round the answer to the nearest whole number, so the nurse should administer 167 mg per dose of enoxaparin every 12 hours to the client with a pulmonary embolism.
Sign Up or Login to view all the 70 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

