ATI Med Surg Exam 1
Total Questions : 41
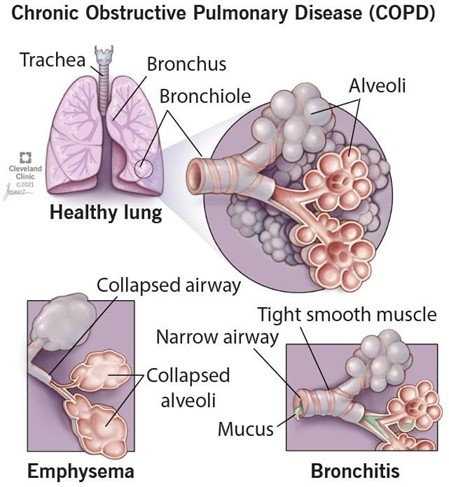
Showing 25 questions, Sign in for moreA nurse is developing a plan of care for a client who has COPD. The nurse should include which of the
following interventions in the plan?
Explanation
Pursed-lip breathing is a technique that helps clients with COPD to exhale more effectively and prevent air trapping in the lungs. It also reduces dyspnea and improves oxygenation.
a) A low protein diet is not recommended for clients with COPD, as they need adequate protein intake to maintain muscle mass and prevent malnutrition.
c) Fluid restriction is not necessary for clients with COPD, unless they have signs of fluid overload or heart failure. Adequate hydration helps to thin secretions and facilitate expectoration.
d) Early-morning hours are not the best time for exercise and activity for clients with COPD, as they may experience more shortness of breath and fatigue due to diurnal variations in lung function. A better time would be mid-morning or afternoon, after taking bronchodilators and clearing secretions.
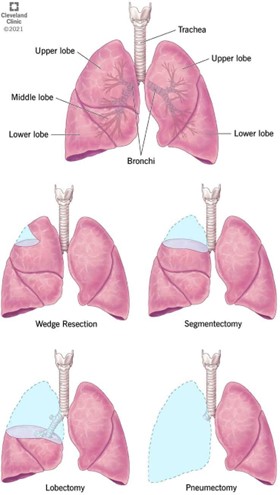
A nurse is assessing a client who is to undergo a left lobectomy to treat lung cancer. The client tells the nurse that she is scared and wishes she had never smoked. Which of the following responses should the nurse make?
Explanation
This response is empathetic and therapeutic, as it acknowledges the client's feelings and invites her to express her concerns. It also shows respect and interest in the client's perspective.
a) This response is false reassurance and nontherapeutic, as it dismisses the client's feelings and implies
that the surgery will solve everything.
b) This response is self-disclosure and nontherapeutic, as it shifts the focus from the client to the nurse and
does not address the client's fears.
d) This response is minimizing and nontherapeutic, as it tells the client how to feel and does not acknowledge the client's regret or anxiety.
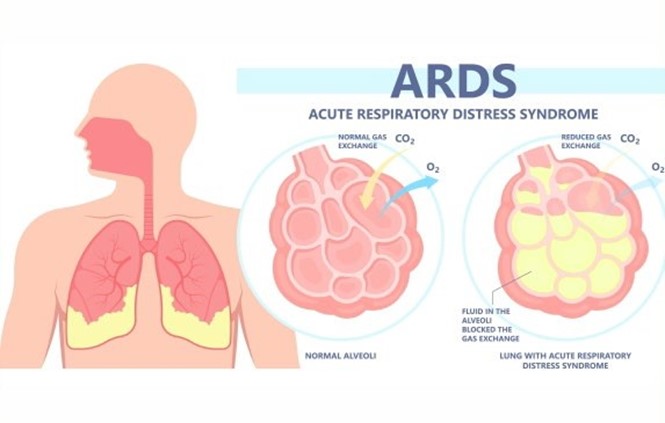
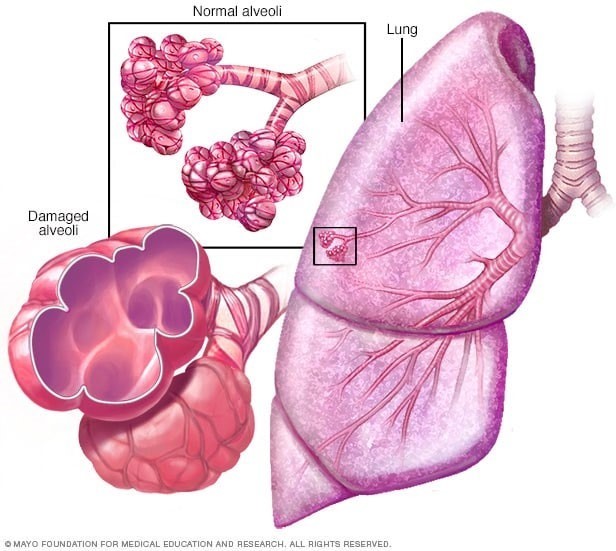
A nurse is planning care for a client who has acute respiratory distress syndrome (ARDS). Which of the following interventions should the nurse include in the plan?
Explanation
Placing the client in a prone position improves oxygenation and ventilation by reducing lung compression, increasing lung expansion, and redistributing blood flow to better match ventilation.
a) Administering low-flow oxygen via nasal cannula is not sufficient for a client with ARDS, who requires
high levels of oxygenation and positive pressure ventilation to prevent alveolar collapse and hypoxemia.
b) Offering high-protein and high-carbohydrate foods frequently is beneficial for a client with ARDS, as it provides adequate nutrition and energy to support lung healing and prevent muscle wasting. However, it is not the priority intervention for improving respiratory function.
d) Encouraging oral intake of at least 3,000 mL of fluids per day is contraindicated for a client with ARDS, who is at risk of fluid overload and pulmonary edema. Fluid intake should be restricted and diuretics should be administered as prescribed to reduce fluid accumulation in the lungs.
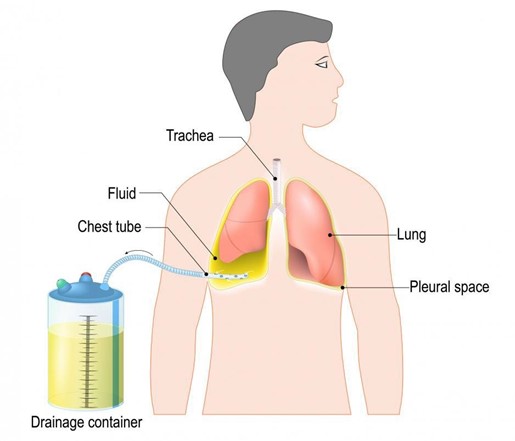
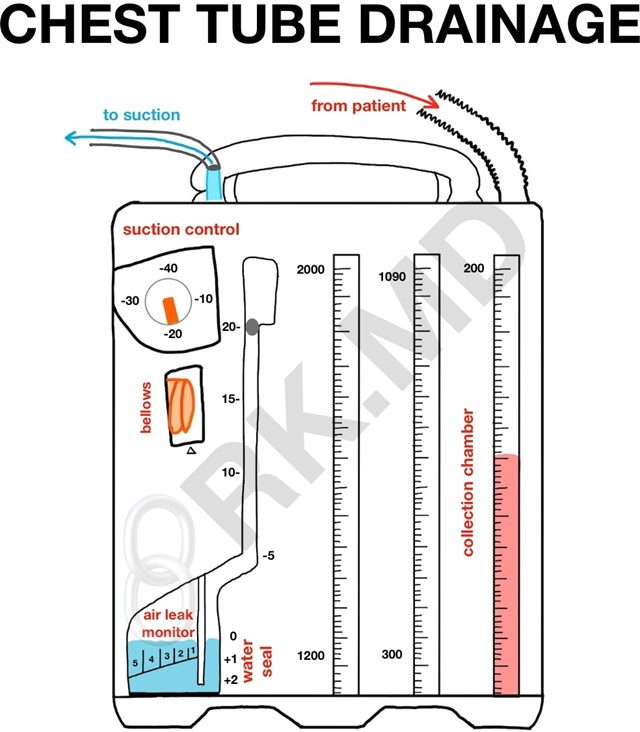
A nurse is caring for a client who has a chest tube connected to a closed drainage system and needs to be transported to the x-ray department. Which of the following actions should the nurse take?
Explanation
Keeping the drainage system below the level of the client's chest prevents backflow of fluid or air into the
pleural space and maintains negative pressure in the system.
a) Disconnecting the chest tube from the drainage system during transport is dangerous and can cause pneumothorax, infection, or bleeding. The chest tube should remain connected to the drainage system at all times unless ordered by the provider.
b) Emptying the collection chamber prior to transport is unnecessary and can interfere with accurate measurement of drainage. The collection chamber should be emptied only when it is full or at the end of each shift.
c) Clamping the chest tube prior to transferring the client to a wheelchair is contraindicated and can cause tension pneumothorax, as it prevents air from escaping the pleural space. The chest tube should only be clamped for a brief period when changing the drainage system or checking for air leaks, and only with a provider's order.
A nurse is providing dietary teaching for a client who has chronic obstructive pulmonary disease. Which of the following instructions should the nurse include?
Explanation
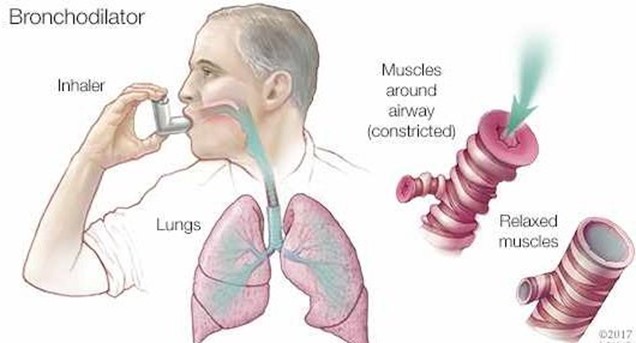
Using a bronchodilator 1 hour before eating can help reduce dyspnea and improve appetite for a client who has COPD. It can also facilitate oxygen delivery to the tissues and prevent hypoxia.
b) Eating 3 large meals each day is not recommended for a client who has COPD, as it can cause abdominal distension and increase pressure on the diaphragm, leading to dyspnea and fatigue. A better option is to eat 5 to 6 small meals throughout the day.
c) Limiting water intake with meals is not advisable for a client who has COPD, as it can cause dehydration and increase the viscosity of secretions, making them harder to expectorate. A better option is to drink at least 2 L of fluids per day, preferably between meals.
d) Reducing protein intake is not beneficial for a client who has COPD, as protein is essential for maintaining muscle mass and strength, especially of the respiratory muscles. A better option is to increase protein intake to at least 1.2 g/kg of body weight per day.
A nurse is caring for a client who has a chest tube connected to a closed drainage system and needs to be transported to the x-ray department. Which of the following actions should the nurse take?
Explanation
Keeping the drainage system below the level of the client's chest prevents backflow of fluid or air into the pleural space and maintains negative pressure in the system.
a) Disconnecting the chest tube from the drainage system during transport is dangerous and can cause pneumothorax, infection, or bleeding. The chest tube should remain connected to the drainage system at all times unless ordered by the provider.
b) Emptying the collection chamber prior to transport is unnecessary and can interfere with accurate measurement of drainage. The collection chamber should be emptied only when it is full or at the end of each shift.
c) Clamping the chest tube prior to transferring the client to a wheelchair is contraindicated and can cause tension pneumothorax, as it prevents air from escaping the pleural space. The chest tube should only be clamped for a brief period when changing the drainage system or checking for air leaks, and only with a provider's order.
A nurse on a medical-surgical unit is performing an admission assessment of a client who has COPD with emphysema. The client reports that he has a frequent productive cough and is short of breath. The nurse should anticipate which of the following assessment findings for this client?
Explanation
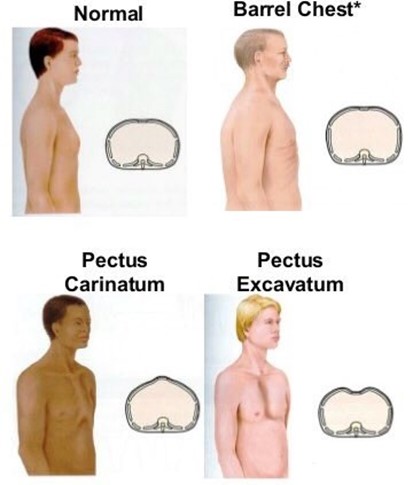
Increased anteroposterior diameter of the chest, also known as barrel chest, is a common finding in clients who have COPD with emphysema. It is caused by chronic air trapping and hyperinflation of the lungs, which results in fattening of the diaphragm and widening of the rib cage.
a) Oxygen saturation level 96% is within the normal range of 95% to 100% and does not indicate hypoxemia or impaired gas exchange. Clients who have COPD with emphysema typically have lower oxygen saturation levels, ranging from 88% to 92%.
b) Respiratory alkalosis is a condition in which the blood pH is elevated due to decreased carbon dioxide levels. It is caused by hyperventilation, which can occur in response to hypoxia, anxiety, or pain. Clients who have COPD with emphysema usually have respiratory acidosis, which is a condition in which the blood pH is lowered due to increased carbon dioxide levels. It is caused by hypoventilation, which results from impaired lung function and airway obstruction.
d) Petechiae on chest are small red or purple spots on the skin caused by bleeding from capillaries. They are not a typical finding in clients who have COPD with emphysema, unless they have severe coughing episodes or coagulation disorders. They can indicate infection, inflammation, trauma, or vascular disease.
A nurse is caring for a client who has asthma and is taking fluticasone. The nurse should monitor the client
for which of the following adverse effects?
Explanation
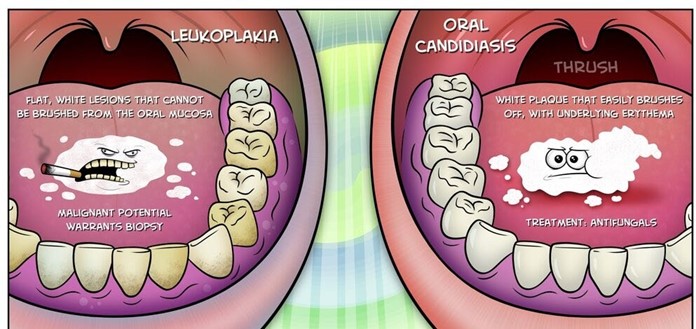
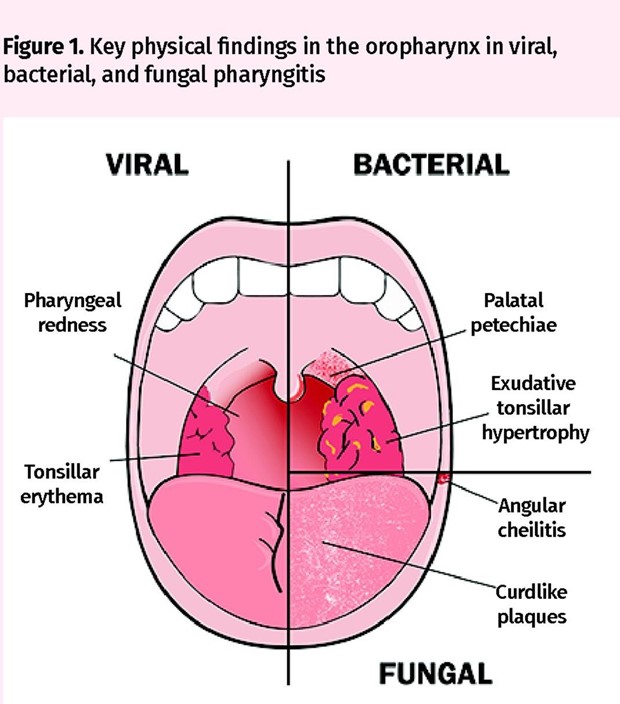
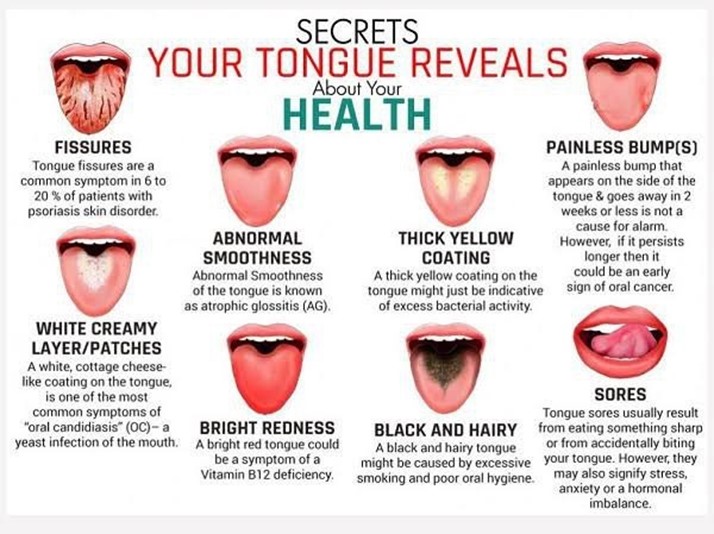
Oral candidiasis, also known as thrush, is a fungal infection of the mouth caused by Candida albicans. It is a common adverse effect of inhaled corticosteroids, such as fluticasone, which can suppress the normal flora of the oral cavity and create a favorable environment for fungal growth. It manifests as white patches or plaques on the tongue, palate, or cheeks that can be scraped off.
a) Polyuria, or excessive urination, is not an adverse effect of fluticasone. It can be caused by diabetes mellitus, diabetes insipidus, diuretics, or kidney disease.
b) Hypoglycemia, or low blood glucose level, is not an adverse effect of fluticasone. It can be caused by
insulin overdose, oral hypoglycemic agents, alcohol intake, or prolonged fasting.
c) Hypertension, or high blood pressure, is not an adverse effect of fluticasone. It can be caused by stress, obesity, smoking, salt intake, or kidney disease.
A nurse is caring for a client who has just developed a pulmonary embolism. Which of the following medications should the nurse anticipate administering?
Explanation
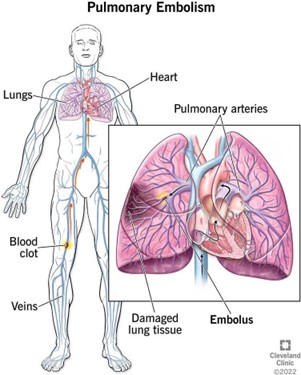
Heparin is an anticoagulant that prevents the formation of new clots and the extension of existing clots. It is the drug of choice for treating acute pulmonary embolism, which is a life-threatening condition caused by a blood clot that travels to the lungs and blocks a pulmonary artery.
a) Dexamethasone is a corticosteroid that reduces inflammation and suppresses immune response. It is not indicated for treating pulmonary embolism, but it may be used for other pulmonary conditions, such as asthma or COPD.
b) Atropine is an anticholinergic that blocks the action of acetylcholine and increases heart rate and cardiac output. It is not indicated for treating pulmonary embolism, but it may be used for bradycardia or asystole.
d) Furosemide is a loop diuretic that increases urine output and reduces fluid volume and blood pressure. It is not indicated for treating pulmonary embolism, but it may be used for heart failure or edema.
A nurse is providing teaching to the parents of a child who has streptococcal pharyngitis about ways to prevent disease transmission. Which of the following responses by the parents indicates an understanding of the teaching?
Explanation
Discarding the toothbrush and buying another is a way to prevent disease transmission, as the toothbrush can harbor bacteria and reinfect the child or spread the infection to others. The toothbrush should be discarded after 24 hours of antibiotic therapy.
a) Encouraging the child to drink lots of fluids is a way to promote hydration and soothe the throat, but it does not prevent disease transmission. The child should avoid sharing cups or utensils with others and use disposable tissues or paper towels.
b) Taking the child's temperature every 4 hours is a way to monitor fever, but it does not prevent disease transmission. The thermometer should be cleaned and disinfected after each use and not shared with others.
d) Giving the child Tylenol for the pain is a way to relieve discomfort, but it does not prevent disease transmission. The medication should be administered according to the label instructions and not shared with others.
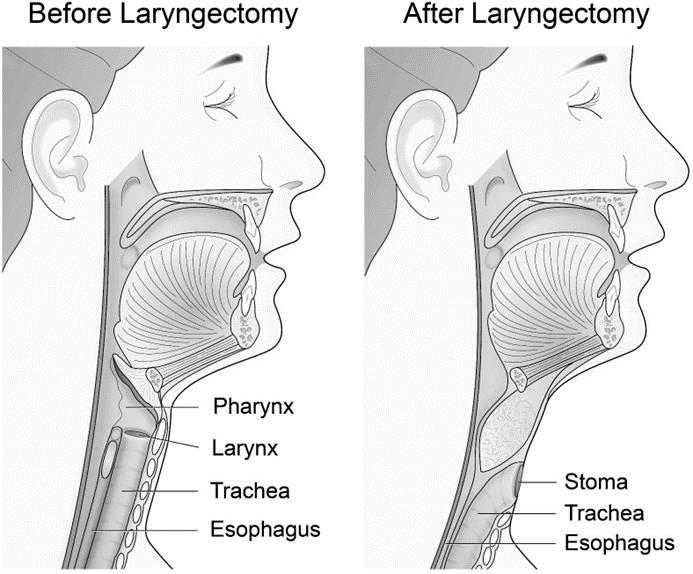
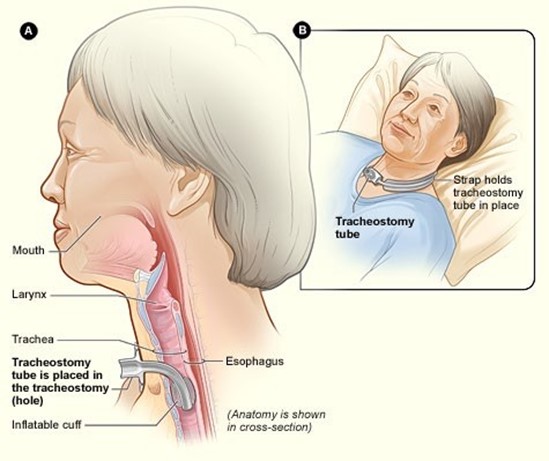
A nurse is caring for a client following a total laryngectomy. Which of the following is the priority observation in the client's care?
Explanation
Suctioning is the priority observation in the client's care, as it prevents airway obstruction and respiratory distress caused by blood, mucus, or secretions. The client has a permanent tracheostomy and cannot cough or clear the airway effectively. The nurse should assess the need for suctioning frequently and perform it as needed, using sterile technique and maintaining oxygenation.
a) Patency of the intravenous line is important, but not the priority observation in the client's care. The intravenous line provides fluids, electrolytes, and medications to the client, but it does not affect the airway patency or oxygenation.
c) Integrity of the dressing is important, but not the priority observation in the client's care. The dressing protects the surgical site from infection and bleeding, but it does not affect the airway patency or oxygenation.
d) Level of pain is important, but not the priority observation in the client's care. The pain can be managed with analgesics and nonpharmacological measures, but it does not affect the airway patency or oxygenation.
A nurse is preparing to administer hydrocortisone 100 mg IM daily to a client. Available is hydrocortisone 250 mg/2 mL. How many mL should the nurse administer per dose?
(Round the answer to the nearest tenth number. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
To calculate the amount of mL to administer, the nurse should use the following formula:
(mg ordered / mg available) x mL available = mL to administer
Substituting the values from the question, the nurse should do the following:
(100 mg / 250 mg) x 2 mL = 0.8 mL

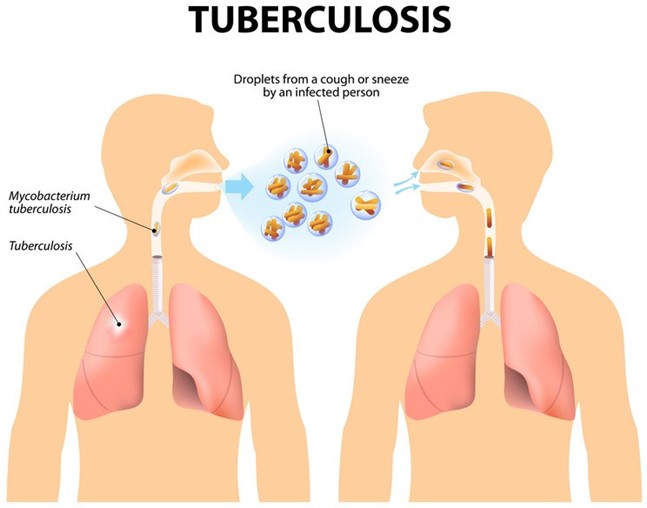
A nurse is teaching a client who has tuberculosis and is to start medication therapy with isoniazid, rifampin, and pyrazinamide. Which of the following instructions should the nurse include?
Explanation
Providing a sputum specimen every 2 weeks to the clinic for testing is an important instruction for the client who has tuberculosis and is on medication therapy. The sputum specimen is used to monitor the effectiveness of the treatment and the presence of drug-resistant strains. The client should continue to provide sputum specimens until they are negative for three consecutive tests.
a) Expecting the sputum cultures to be negative after 6 months of therapy is not a realistic or accurate instruction. The duration of therapy for tuberculosis varies depending on the type and extent of the disease, the drug regimen, and the client's response. It can range from 6 to 12 months or longer. The client should not stop taking the medications until instructed by the provider, even if the symptoms improve or the sputum cultures are negative.
b) Drinking at least 8 ounces of water when taking the pyrazinamide tablet is not a specific or necessary instruction. Pyrazinamide can cause hepatotoxicity and hyperuricemia, so the client should drink adequate fluids throughout the day to prevent these adverse effects. However, there is no evidence that drinking water with the tablet has any additional benefit. The client should also avoid alcohol and report any signs of liver damage or gout.
d) Taking isoniazid with an antacid is not a correct or advisable instruction. Antacids can decrease the absorption and effectiveness of isoniazid, which can lead to treatment failure or drug resistance. The client should take isoniazid on an empty stomach, at least 1 hour before or 2 hours after meals, and avoid antacids within 1 hour of taking it.
A nurse is providing discharge teaching to a client who has asthma and a new prescription for fluticasone/salmeterol. For which of the following adverse effects should the nurse instruct the client to report to the provider?
Explanation
White coating in the mouth, also known as oral candidiasis or thrush, is a serious adverse effect of fluticasone/salmeterol, which is a combination of an inhaled corticosteroid and a long-acting beta2 agonist. It is caused by fungal infection of the oral cavity due to suppression of the normal flora by the corticosteroid component. The client should report this symptom to the provider, as it may require antifungal treatment and discontinuation of the medication.
a) Dry oral mucous membranes is a common and mild adverse effect of fluticasone/salmeterol, which can be relieved by drinking water, chewing sugarless gum, or using artificial saliva. It does not require reporting to the provider or stopping the medication.
c) Sedation is not an adverse effect of fluticasone/salmeterol, but it may be caused by other medications, such as antihistamines, opioids, or benzodiazepines. The client should avoid driving or operating machinery if sedated and consult with the provider about possible drug interactions.
d) Increased appetite is not an adverse effect of fluticasone/salmeterol, but it may be caused by other factors, such as stress, boredom, or hormonal changes. The client should maintain a balanced diet and exercise regularly to prevent weight gain and promote health.
A nurse is caring for a client following a total laryngectomy. Which of the following is the priority observation in the client's care?
Explanation
Suctioning is the priority observation in the client's care, as it prevents airway obstruction and respiratory distress caused by blood, mucus, or secretions. The client has a permanent tracheostomy and cannot cough
or clear the airway effectively. The nurse should assess the need for suctioning frequently and perform it as needed, using sterile technique and maintaining oxygenation.
a) Patency of the intravenous line is important, but not the priority observation in the client's care. The intravenous line provides fluids, electrolytes, and medications to the client, but it does not affect the airway patency or oxygenation.
c) Integrity of the dressing is important, but not the priority observation in the client's care. The dressing protects the surgical site from infection and bleeding, but it does not affect the airway patency or oxygenation.
d) Level of pain is important, but not the priority observation in the client's care. The pain can be managed with analgesics and nonpharmacological measures, but it does not affect the airway patency or oxygenation.
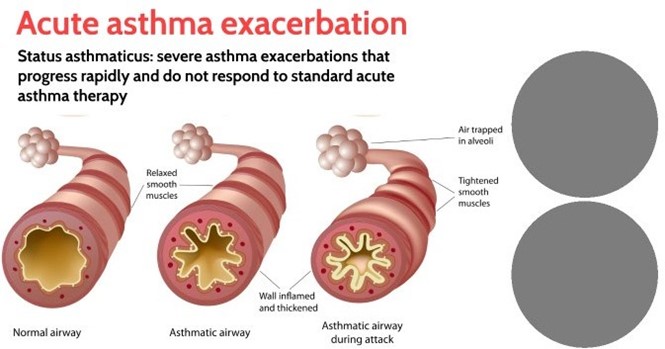
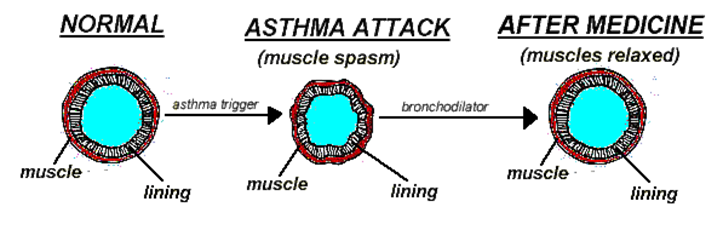
A nurse is caring for a child who is experiencing status asthmaticus. Which of the following interventions is the priority for the nurse to take?
Explanation
Administering a short-acting beta2-agonist (SABA), such as albuterol, is the priority intervention for the nurse to take, as it provides rapid bronchodilation and relieves bronchospasm, which are the main features of status asthmaticus. Status asthmaticus is a severe and life-threatening asthma attack that does not respond to usual treatment and requires immediate medical attention.
a) Determining the cause of the acute exacerbation is important, but not the priority intervention for the nurse to take. The cause may be an allergen, infection, stress, or exercise, but it does not affect the immediate management of status asthmaticus. The nurse should focus on restoring airway patency and oxygenation first, and then identify and avoid triggers later.
b) Obtaining a peak flow reading is important, but not the priority intervention for the nurse to take. The peak flow reading measures the maximum expiratory flow rate and indicates the degree of airway obstruction. However, it may not be feasible or accurate in a child who is experiencing status asthmaticus, as they may be too dyspneic or agitated to perform the test. The nurse should rely on other signs of respiratory distress, such as wheezes, retractions, cyanosis, or pulse oximetry.
c) Administering an inhaled glucocorticoid is important, but not the priority intervention for the nurse to take. Glucocorticoids, such as fluticasone or budesonide, reduce inflammation and mucus production in the airways, but they have a delayed onset of action and are not effective for acute asthma attacks. They are used for long-term control and prevention of asthma symptoms.
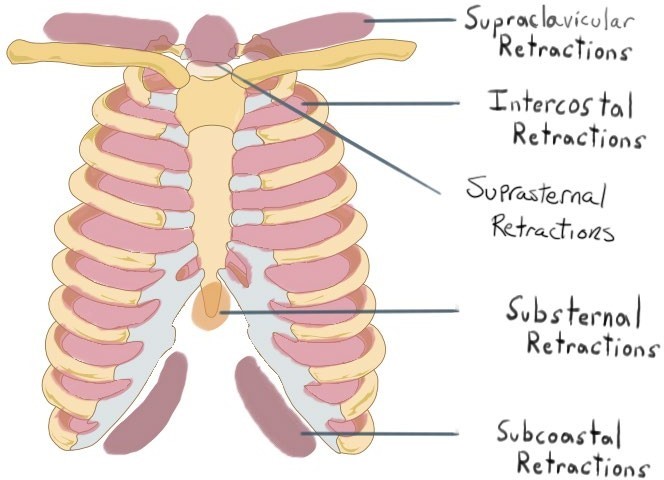
A nurse is assessing a client who has postoperative atelectasis and is hypoxic. Which of the following manifestations should the nurse expect?
Explanation
Intercostal retractions, or the inward movement of the chest wall between the ribs, are a sign of respiratory distress and hypoxia. They indicate increased work of breathing and reduced lung expansion, which are common in clients who have postoperative atelectasis. Atelectasis is a collapse of alveoli in a part of the lung, which impairs gas exchange and oxygenation.
a) Lethargy, or a state of reduced mental alertness and energy, is not a typical manifestation of hypoxia. It can be caused by other factors, such as pain, medication, infection, or electrolyte imbalance. Hypoxia usually causes restlessness, anxiety, or confusion.
b) Bradycardia, or a slow heart rate, is not a typical manifestation of hypoxia. It can be caused by other factors, such as medication, vagal stimulation, or heart block. Hypoxia usually causes tachycardia, or a fast heart rate, as the body tries to compensate for the low oxygen level.
d) Bradypnea, or a slow respiratory rate, is not a typical manifestation of hypoxia. It can be caused by other factors, such as medication, brain injury, or metabolic alkalosis. Hypoxia usually causes tachypnea, or a fast respiratory rate, as the body tries to increase oxygen intake and carbon dioxide elimination.
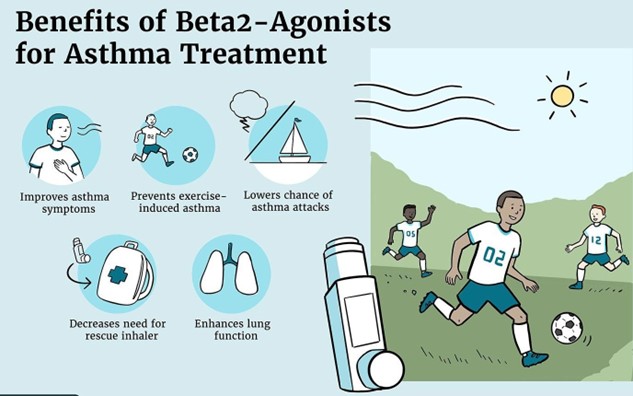
A nurse is caring for a client who asks how albuterol helps his breathing. Which of the following responses should the nurse make? (Select all that apply.)
Explanation
These responses are correct and explain how albuterol helps the client's breathing. Albuterol is a short- acting beta2-agonist that causes bronchodilation and relieves bronchospasm, which are the main causes of wheezing and dyspnea in clients who have asthma or COPD. By opening the airways, albuterol improves gas exchange and oxygenation.
b) The medication will decrease coughing episodes. This response is incorrect and does not explain how albuterol helps the client's breathing. Albuterol does not have a direct effect on coughing, which is a reflex response to irritation or obstruction of the airways. Coughing may be beneficial for clearing secretions and mucus from the lungs, but it may also cause bronchoconstriction and inflammation. The nurse should advise the client to use other measures to decrease coughing, such as drinking fluids, using a humidifier, or taking an expectorant.
c) The medication will reduce inflammation. This response is incorrect and does not explain how albuterol helps the client's breathing. Albuterol does not have an anti-inflammatory effect on the airways, which are often inflamed and swollen in clients who have asthma or COPD. Inflammation can contribute to airway obstruction and mucus production, which impair gas exchange and oxygenation. The nurse should inform the client that albuterol is used for quick relief of acute symptoms, but not for long-term control or prevention of inflammation. The client may need to use another medication, such as an inhaled corticosteroid, to reduce inflammation.
e) The medication will stimulate flow of mucus. This response is incorrect and does not explain how albuterol helps the client's breathing. Albuterol does not have a direct effect on mucus production or clearance, which are often increased in clients who have asthma or COPD. Mucus can cause airway obstruction and infection, which impair gas exchange and oxygenation. The nurse should advise the client to use other measures to stimulate flow of mucus, such as drinking fluids, using a humidifier, or taking an expectorant.
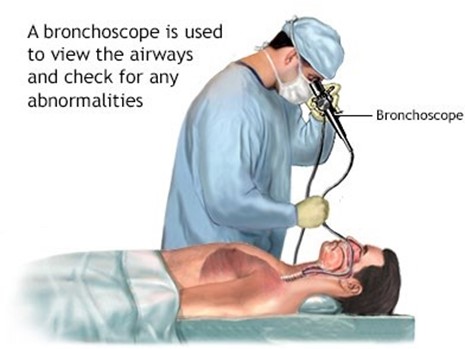
A nurse is teaching a client who will undergo a bronchoscopy procedure. The provider will use a rigid scope and general anesthesia. The nurse should explain that the client's neck will be in which of the following positions?
Explanation
Hyperextended position, or backward bending of the neck, is the correct position for the client's neck during a bronchoscopy procedure with a rigid scope and general anesthesia. This position allows the provider to insert the scope through the mouth and into the trachea and bronchi, while avoiding injury to the teeth, tongue, or larynx. It also facilitates visualization of the airways and removal of foreign bodies or secretions.
b) Neutral position, or alignment of the head and neck with the spine, is not the correct position for the client's neck during a bronchoscopy procedure with a rigid scope and general anesthesia. This position may interfere with the insertion of the scope and cause damage to the oral structures or airways.
c) Extended position, or forward bending of the neck, is not the correct position for the client's neck during a bronchoscopy procedure with a rigid scope and general anesthesia. This position may obstruct the airway and make it difficult for the provider to insert the scope and access the bronchi.
d) Flexed position, or downward bending of the neck, is not the correct position for the client's neck during a bronchoscopy procedure with a rigid scope and general anesthesia. This position may compress the airway and prevent adequate ventilation and oxygenation of the client.
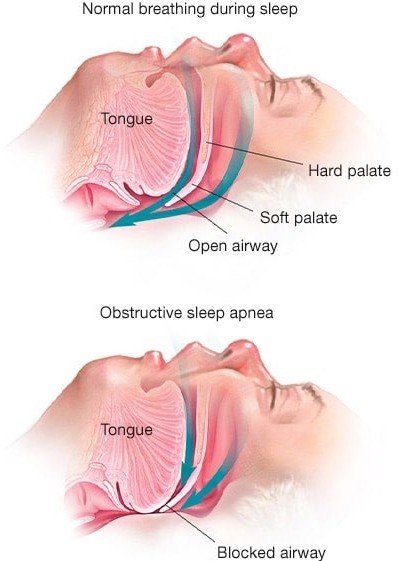
A nurse is teaching a client who is obese and has obstructive sleep apnea how to decrease the number of nightly apneic episodes. Which of the following client statements indicates an understanding of the teaching?
Explanation
This statement indicates an understanding of the teaching, as weight loss is one of the most effective ways to decrease the number of nightly apneic episodes in clients who are obese and have obstructive sleep apnea. Obstructive sleep apnea is a condition in which the upper airway collapses or becomes blocked during sleep, causing pauses in breathing and hypoxia. Obesity is a major risk factor for obstructive sleep apnea, as excess fat tissue around the neck and throat can narrow the airway and increase its collapsibility. Losing weight can reduce the pressure on the airway and improve its patency.
b) "I sleep better if I take a sleeping pill at night." This statement indicates a lack of understanding of the teaching, as sleeping pills are not recommended for clients who have obstructive sleep apnea. Sleeping pills can worsen the condition by relaxing the muscles of the throat and tongue, which can further obstruct the airway and decrease the arousal response to hypoxia. The nurse should advise the client to avoid sleeping pills and other sedatives or alcohol before bedtime.
c) "It might help if I tried sleeping only on my back." This statement indicates a lack of understanding of the teaching, as sleeping on the back is not helpful for clients who have obstructive sleep apnea. Sleeping on the back can increase the risk of airway obstruction by allowing gravity to pull the tongue and soft palate backward, which can block the airway and cause snoring and apnea. The nurse should suggest that the client try sleeping on the side or elevate the head of the bed to prevent this.
d) "I should get a humidifier to run at my bedside at night." This statement indicates a lack of understanding of the teaching, as a humidifier is not likely to decrease the number of nightly apneic episodes in clients who have obstructive sleep apnea. A humidifier can moisten the air and ease breathing for clients who have dry or irritated nasal passages, but it does not address the underlying cause of airway obstruction or hypoxia. The nurse should inform the client that a humidifier may not be effective for obstructive sleep apnea and may increase the risk of infection or mold growth if not cleaned properly.
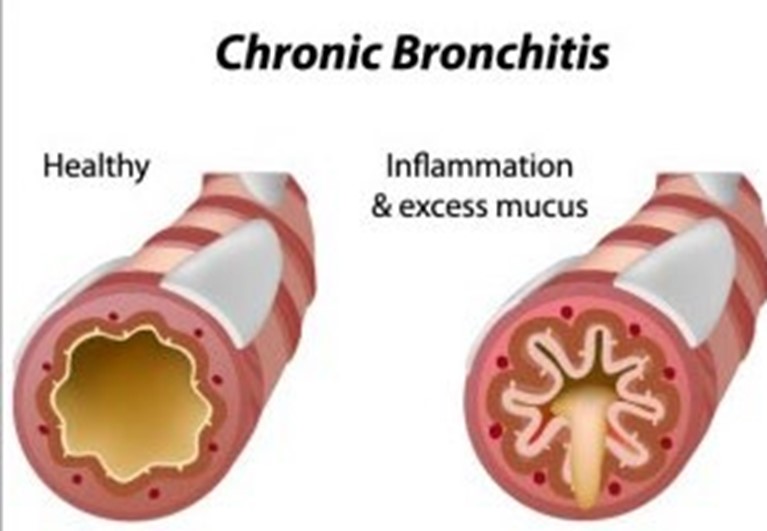
A nurse is giving a presentation at a community center about chronic bronchitis. Which of the following information should the nurse include as effective for preventing this disorder?
Explanation
Smoking cessation is the most effective way to prevent chronic bronchitis, which is a type of chronic obstructive pulmonary disease (COPD) characterized by inflammation and excess mucus production in the
bronchi. Smoking is the main cause of chronic bronchitis, as it damages the cilia and mucous membranes of the airways, leading to chronic cough, sputum, and infection. Quitting smoking can reduce the risk of developing or worsening chronic bronchitis and improve lung function and quality of life.
a) Regular moderate exercise is beneficial for preventing chronic bronchitis, but not as effective as smoking cessation. Exercise can improve cardiovascular and respiratory health, increase oxygen delivery to the tissues, and enhance immune function. However, exercise alone cannot reverse the damage caused by smoking or prevent further deterioration of the airways.
b) Maintenance of ideal weight is beneficial for preventing chronic bronchitis, but not as effective as smoking cessation. Maintaining a healthy weight can reduce the workload on the heart and lungs, prevent obesity-related complications, and improve self-esteem and well-being. However, weight management alone cannot restore the normal structure and function of the airways or prevent chronic inflammation and mucus production.
c) Annual influenza immunization is beneficial for preventing chronic bronchitis, but not as effective as smoking cessation. Influenza immunization can protect against viral infections that can trigger or exacerbate chronic bronchitis symptoms, such as fever, cough, wheezes, and dyspnea. However, influenza immunization cannot prevent other causes of chronic bronchitis, such as bacterial infections, environmental pollutants, or genetic factors.
A nurse is caring for a client with a tracheostomy. The client's partner has been taught to perform suctioning. Which of the following actions by the partner should indicate to the nurse a readiness for the client's discharge?
Explanation
Performing the procedure independently is the best indicator of the partner's readiness for the client's discharge, as it demonstrates competence and confidence in suctioning. Suctioning is a skill that requires practice and supervision until mastery is achieved. The nurse should observe and evaluate the partner's performance of suctioning and provide feedback and reinforcement as needed.
b) Attending a class given about tracheostomy care is a good action by the partner, but not the best indicator of readiness for the client's discharge. Attending a class can provide information and education about tracheostomy care, but it does not necessarily translate into skill acquisition or application. The nurse should assess the partner's understanding and retention of the information and provide additional teaching or clarification as needed.
c) Verbalizing all steps in the procedure is a good action by the partner, but not the best indicator of readiness for the client's discharge. Verbalizing all steps in the procedure can help the partner remember and follow the correct sequence and technique of suctioning, but it does not necessarily reflect actual performance or ability. The nurse should observe and verify that the partner is doing what they are saying and correct any errors or omissions as needed.
d) Asking appropriate questions about suctioning is a good action by the partner, but not the best indicator of readiness for the client's discharge. Asking appropriate questions about suctioning can show interest and involvement in learning and caring for the client, but it does not necessarily indicate competence or confidence in suctioning. The nurse should answer the partner's questions and provide additional resources or referrals as needed.
A nurse is caring for a client who asks how albuterol helps his breathing. Which of the following responses should the nurse make? (Select all that apply.)
Explanation
These responses are correct and explain how albuterol helps the client's breathing. Albuterol is a short- acting beta2-agonist that causes bronchodilation and relieves bronchospasm, which are the main causes of wheezing and dyspnea in clients who have asthma or COPD. By opening the airways, albuterol improves gas exchange and oxygenation.
b) The medication will decrease coughing episodes. This response is incorrect and does not explain how albuterol helps the client's breathing. Albuterol does not have a direct effect on coughing, which is a reflex response to irritation or obstruction of the airways. Coughing may be beneficial for clearing secretions and mucus from the lungs, but it may also cause bronchoconstriction and inflammation. The nurse should advise the client to use other measures to decrease coughing, such as drinking fluids, using a humidifier, or taking an expectorant.
c) The medication will reduce inflammation. This response is incorrect and does not explain how albuterol helps the client's breathing. Albuterol does not have an anti-inflammatory effect on the airways, which are often inflamed and swollen in clients who have asthma or COPD. Inflammation can contribute to airway obstruction and mucus production, which impair gas exchange and oxygenation. The nurse should inform the client that albuterol is used for quick relief of acute symptoms, but not for long-term control or prevention of inflammation. The client may need to use another medication, such as an inhaled corticosteroid, to reduce inflammation.
e) The medication will stimulate flow of mucus. This response is incorrect and does not explain how albuterol helps the client's breathing. Albuterol does not have a direct effect on mucus production or clearance, which are often increased in clients who have asthma or COPD. Mucus can cause airway obstruction and infection, which impair gas exchange and oxygenation. The nurse should advise the client to use other measures to stimulate flow of mucus, such as drinking fluids, using a humidifier, or taking an expectorant.
A nurse is caring for a client who has a three-chamber closed chest tube system. Which of the following actions should the nurse take after noticing a rise in the water seal chamber with client inspiration?
Explanation
Continuing to monitor the client is the appropriate action for the nurse to take, as a rise in the water seal chamber with client inspiration is a normal and expected finding. The water seal chamber acts as a one-way valve that allows air to exit from the pleural space and prevents air from entering. The water level in this chamber fluctuates with breathing, rising with inspiration and falling with expiration. This indicates that the chest tube system is functioning properly and that there is no air leak.
a) Immediately notifying the provider is not necessary, as a rise in the water seal chamber with client inspiration is not an abnormal or urgent finding. The nurse should only notify the provider if there are signs of complications, such as persistent bubbling in the water seal chamber, which indicates an air leak, or no fluctuation in the water level, which indicates an obstruction or resolution of pneumothorax.
b) Clamping the chest tube near the water seal is not advisable, as it can cause increased pressure in the pleural space and lead to tension pneumothorax. Clamping the chest tube should only be done for a brief period of time and under specific circumstances, such as changing the drainage system, assessing for an air leak, or preparing for chest tube removal.
d) Repositioning the client toward the left side is not helpful, as it does not affect the water level in the water seal chamber. The nurse should position the client according to their comfort and condition, and avoid placing them flat or on their affected side, as this can impair drainage and ventilation.
A nurse is caring for a client who has emphysema. Which of the following findings should the nurse expect to assess in this client? (Select all that apply.)
Explanation
These findings are expected to be assessed in a client who has emphysema, which is a type of chronic obstructive pulmonary disease (COPD) characterized by destruction and enlargement of alveoli, loss of elastic recoil, and air trapping. These changes impair gas exchange and oxygenation, leading to chronic hypoxia and hypercapnia.
a) Dyspnea, or difficulty breathing, is a common symptom of emphysema, as the client has reduced lung capacity and increased work of breathing. Dyspnea may be worse with exertion, stress, or infection, and may cause anxiety and fatigue. The nurse should monitor the client's respiratory rate, rhythm, depth, and effort, and provide oxygen therapy as prescribed.
b) Barrel chest, or increased anteroposterior diameter of the chest, is a physical sign of emphysema, as the client has chronic air trapping and hyperinflation of the lungs. Barrel chest may also cause kyphosis, or curvature of the spine, and reduced chest wall movement. The nurse should measure the client's chest circumference and observe for any deformities or asymmetry.
d) Clubbing of the fingers, or enlargement and rounding of the nail beds, is a late sign of emphysema, as the client has chronic hypoxia and tissue ischemia. Clubbing may also affect the toes and ears, and may indicate pulmonary or cardiac disease. The nurse should inspect the client's nails for shape, color, angle, and capillary refill.
c) Deep respirations are not expected to be assessed in a client who has emphysema, as the client has shallow and rapid breathing due to air trapping and reduced lung compliance. Deep respirations may indicate other conditions, such as metabolic acidosis or anxiety. The nurse should assess the client's arterial blood gas levels and provide reassurance and relaxation techniques as needed.
e) Bradycardia, or slow heart rate, is not expected to be assessed in a client who has emphysema, as the client has tachycardia or normal heart rate due to hypoxia and increased sympathetic stimulation. Bradycardia may indicate other conditions, such as medication side effects, vagal stimulation, or heart block. The nurse should monitor the client's pulse rate, rhythm, quality, and electrocardiogram as indicated.
Sign Up or Login to view all the 41 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

