ATI Med Surg Exam 8
Total Questions : 46
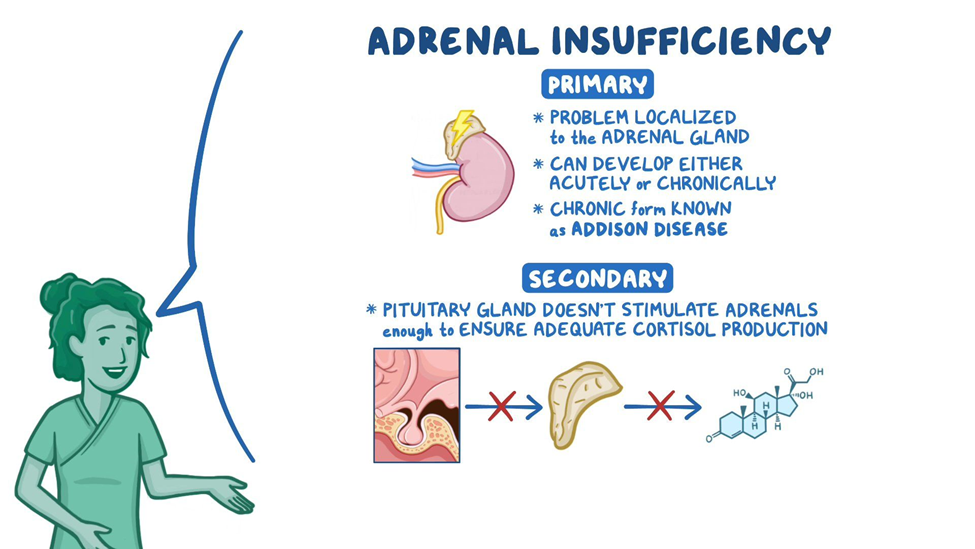
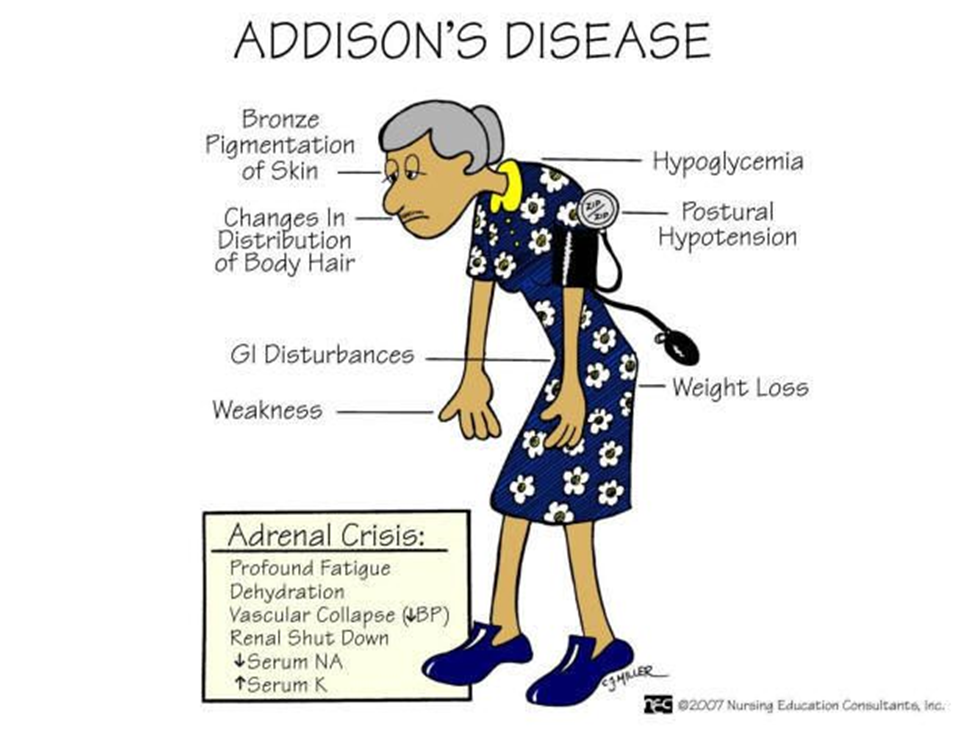
Showing 25 questions, Sign in for moreA client with a history of Addison's disease and flu-like symptoms accompanied by nausea and vomiting over the past week is brought to the facility. His wife reports that he acted confused and was extremely weak when he awoke that morning. The client's blood pressure is 90/58 mm Hg, his pulse is 116 beats/minute, and his temperature is 101° F (38.3° C). A diagnosis of acute adrenal insufficiency is made. What should the nurse expect to administer by I.V. infusion?
Explanation
A. Methylprednisolone (Solu-medrol):
Explanation: Acute adrenal insufficiency is a life-threatening condition characterized by a sudden deficiency of adrenal hormones. In this situation, intravenous glucocorticoids such as methylprednisolone are administered to replace the deficient hormones and stabilize the patient. This is the appropriate intervention to address the acute adrenal crisis.
B. Hypotonic saline:
Explanation: Hypotonic saline is not the first-line treatment for acute adrenal insufficiency. The priority is to replace glucocorticoids to address the adrenal hormone deficiency.
C. Potassium (K-dur):
Explanation: While electrolyte imbalances can occur in adrenal insufficiency, potassium replacement alone does not address the primary issue of glucocorticoid deficiency in acute adrenal insufficiency.
D. Regular Insulin:
Explanation: Regular insulin is not the primary treatment for acute adrenal insufficiency. Glucocorticoid replacement, such as methylprednisolone, is the key intervention.
The nurse is caring for a patient with Addison's disease who is scheduled for discharge. When teaching the patient about hormone replacement therapy, the nurse should address what topic?
Explanation
A. The need to match the daily steroid dose to immediate symptoms:
Explanation: Adjusting the steroid dose based on immediate symptoms is not a recommended approach. Patients should follow the prescribed regimen provided by their healthcare provider.
B. The importance of monitoring liver function:
Explanation: While monitoring liver function is important for some medications, it is not the primary focus when teaching about hormone replacement therapy in Addison's disease. The emphasis is on the need for life-long steroid replacement.
C. The need for life-long steroid replacement:
Explanation: Patients with Addison's disease require life-long steroid replacement therapy to compensate for the deficiency in adrenal hormones. It's important for the patient to understand that adherence to the prescribed steroid regimen is essential for maintaining health and preventing adrenal crisis.
D. The possibility extreme weight loss from the use of corticosteroids:
Explanation: While corticosteroids can have various side effects, extreme weight loss is not a typical or desired outcome of steroid therapy for Addison's disease. Weight changes and potential side effects should be discussed, but the emphasis should be on the importance of long-term steroid replacement.
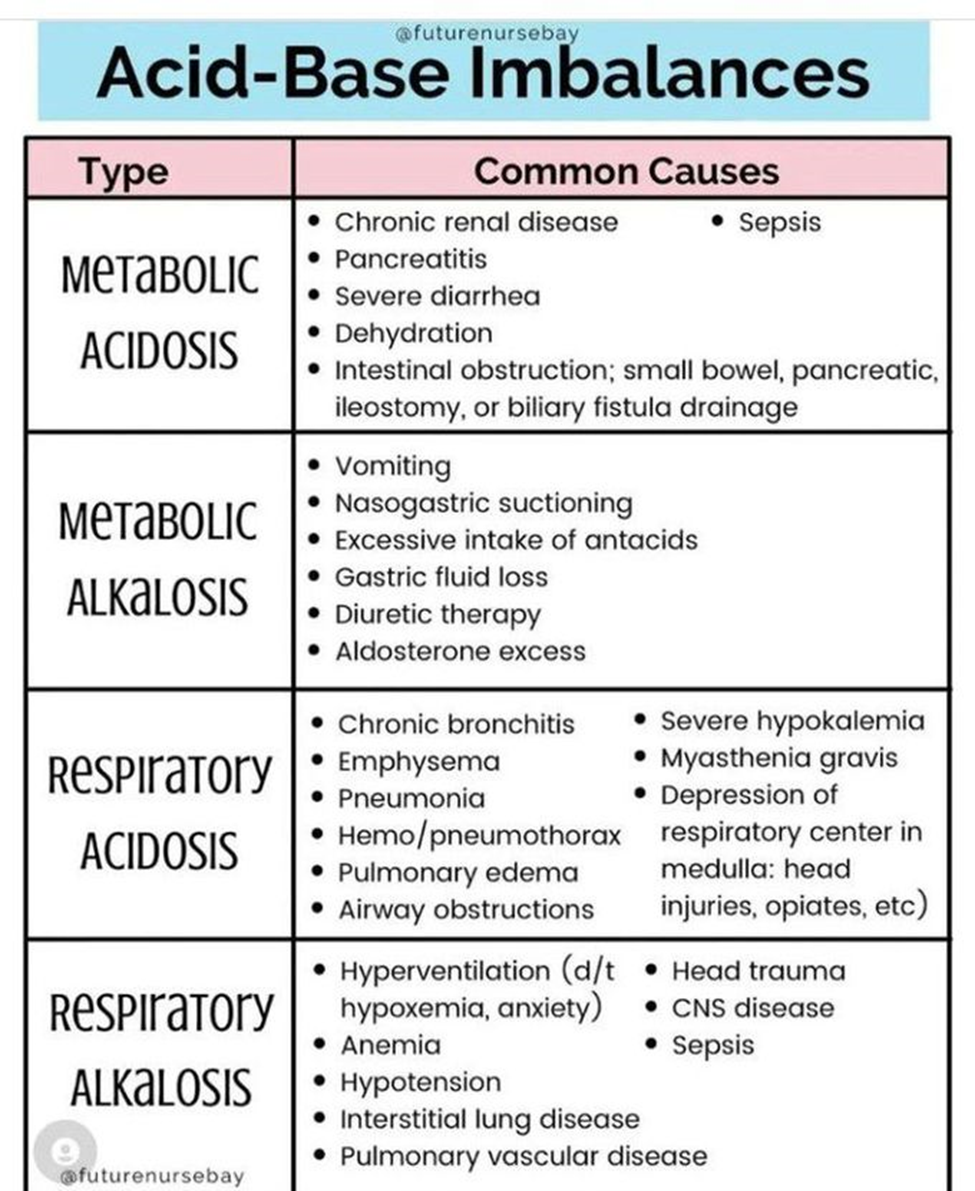
A patient with a longstanding diagnosis of generalized anxiety disorder presents to the emergency room. The triage nurse notes upon an assessment that the patient is hyperventilating. The triage nurse is aware that hyperventilation is the MOST common cause of which acid-base imbalance?
Explanation
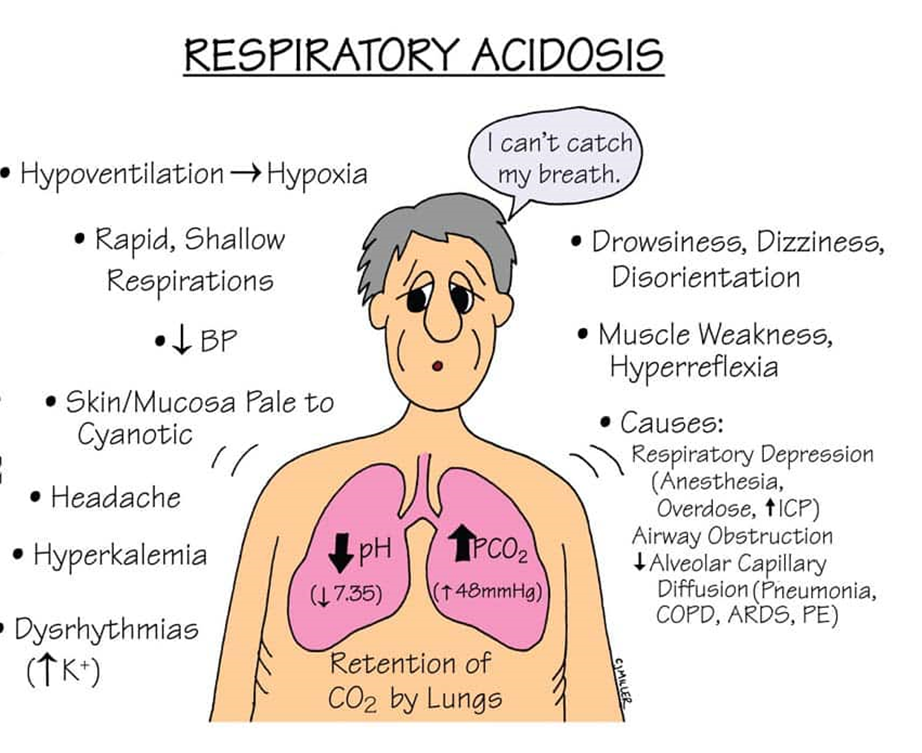
A. Respiratory Acidosis:
Explanation: Respiratory acidosis occurs when there is inadequate elimination of carbon dioxide, leading to an increase in PaCO2 and a decrease in blood pH. This is typically associated with conditions that impair ventilation.
B. Metabolic Alkalosis:
Explanation: Metabolic alkalosis is characterized by an elevated blood pH and bicarbonate (HCO3-) concentration. It is not directly caused by hyperventilation but is often associated with conditions such as excessive vomiting or excessive bicarbonate intake.
C. Metabolic Acidosis:
Explanation: Metabolic acidosis is characterized by a decrease in blood pH and bicarbonate concentration. It is not directly caused by hyperventilation but may result from conditions such as diabetic ketoacidosis or lactic acidosis.
D. Respiratory Alkalosis:
Explanation: Hyperventilation is the most common cause of respiratory alkalosis. During hyperventilation, there is an excessive loss of carbon dioxide (CO2) through rapid breathing, leading to a decrease in the partial pressure of carbon dioxide (PaCO2) in the blood. This results in an increase in blood pH, causing an alkalotic state.
A client is being treated on the medical unit for a sickle cell crisis. The nurse's most recent assessment reveals an oral temperature of 100.5°F and a new onset of fine crackles on lung auscultation. What is the nurse's most appropriate action?
Explanation
A. Inform the primary care provider that the patient may have an infection:
Explanation: The presence of an elevated oral temperature and new onset of fine crackles on lung auscultation suggests a potential respiratory infection, which is a significant concern in a patient with sickle cell disease. Notifying the primary care provider allows for further evaluation and appropriate management of the infection.
B. Liaise with the respiratory therapist and consider high-flow oxygen:
Explanation: While oxygenation may be necessary, especially if the patient is experiencing respiratory distress, addressing the potential infection is the priority. Consulting with the respiratory therapist and considering high-flow oxygen can be part of the overall plan based on the primary care provider's recommendations.
C. Apply supplementary oxygen by nasal cannula:
Explanation: Providing oxygen support may be necessary, but it should be done in consultation with the primary care provider, who can guide the appropriate level of oxygen therapy based on the patient's condition.
D. Administer bronchodilators by nebulizer:
Explanation: Bronchodilators are typically used for conditions like asthma or COPD, and their use might not be the primary intervention in the context of a sickle cell crisis with signs of a potential respiratory infection. Addressing the infection takes precedence, and the primary care provider's input is essential in determining the appropriate course of action.
A client with chronic kidney disease has chronic anemia. What pharmacologic alternative to blood transfusion may be used for this patient?
Explanation
A. Erythropoietin (Epogen):
Explanation: Erythropoietin is a hormone that stimulates the production of red blood cells. In chronic kidney disease, especially when associated with anemia, the production of erythropoietin by the kidneys may be reduced. Erythropoietin (Epogen) is commonly used to stimulate the production of red blood cells and manage anemia in patients with chronic kidney disease.
B. Eltrombopag (Promacta):
Explanation: Eltrombopag is a medication used to stimulate the production of platelets and is primarily indicated for conditions associated with thrombocytopenia (low platelet count). It is not used to treat anemia associated with chronic kidney disease.
C. GM-CSF (Leukine):
Explanation: Granulocyte-macrophage colony-stimulating factor (GM-CSF or Leukine) is a medication that stimulates the production of white blood cells and is used in certain conditions to address decreased white blood cell counts. It is not typically used for managing anemia.
D. Thrombopoietin (TPO):
Explanation: Thrombopoietin is a hormone that stimulates the production of platelets. Medications that mimic the action of thrombopoietin, such as romiplostim and eltrombopag, are used to treat thrombocytopenia. Thrombopoietin is not used for the treatment of anemia.
A client with Cushing's syndrome is receiving education about dietary changes from the nurse. Which statement by the patient demonstrates the need for further teaching?
Explanation
A. "I can eat a salad with oil and vinegar dressing":
Explanation: This statement is correct. A salad with oil and vinegar dressing is a healthy option, and the patient does not need to avoid this.
B. "I can cook soup using canned vegetables":
Explanation: This statement is generally acceptable. However, the patient should be aware of the sodium content in canned vegetables and choose low-sodium options to manage fluid retention, which can be a concern in Cushing's syndrome.
C. "I can eat dried fruit for breakfast with my oatmeal":
Explanation: This statement is questionable. Dried fruits may have higher sugar content and can contribute to an increase in calorie intake. In Cushing's syndrome, where there may be weight gain, it's advisable to choose fresh fruits over dried ones.
D. "I can eat baked chicken with green beans for dinner":
Explanation: This statement is correct. Baked chicken with green beans is a healthy and balanced option.
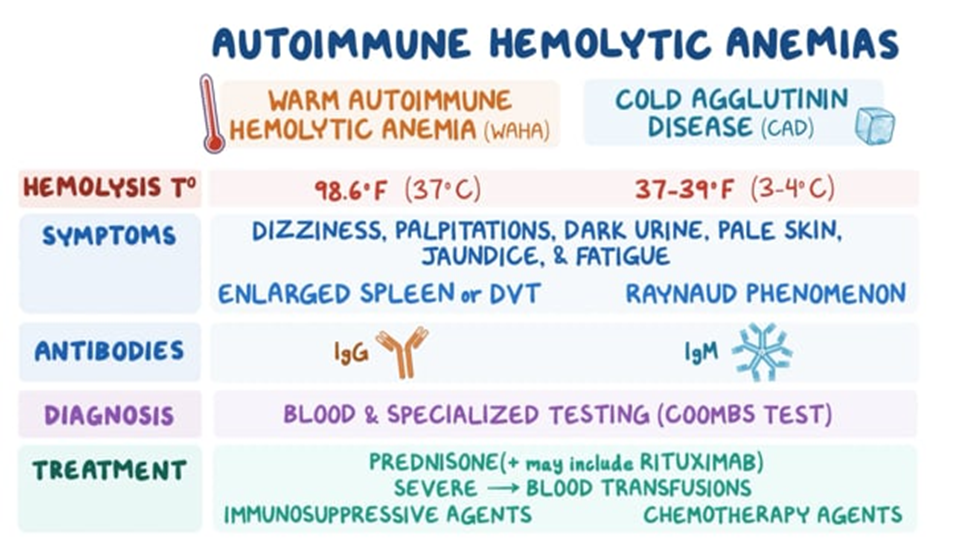
A client comes into the clinic complaining of fatigue. Blood work shows an increased bilirubin concentration and an increased reticulocyte count. What would the nurse suspect the patient has?
Explanation
A. Leukemia:
Explanation: Leukemia is a cancer of the blood-forming tissues, including the bone marrow and lymphatic system. It typically presents with an abnormal increase in white blood cells. While fatigue can be a symptom, increased bilirubin concentration and an increased reticulocyte count are not typical findings in leukemia.
B. Hemolytic Anemia:
Explanation: Hemolytic anemia is characterized by the premature destruction of red blood cells, leading to an increased release of bilirubin (from the breakdown of hemoglobin) and an increased reticulocyte count (as the body attempts to compensate by producing more red blood cells). This is a likely possibility given the presented symptoms.
C. Hypoproliferative Anemia:
Explanation: Hypoproliferative anemia is characterized by a decreased production of red blood cells. It is unlikely in this scenario, as an increased reticulocyte count suggests an attempt by the bone marrow to increase red blood cell production.
D. Thrombocytopenia:
Explanation: Thrombocytopenia is a condition characterized by a low platelet count. It does not typically present with an increased bilirubin concentration or an increased reticulocyte count.
A nurse is providing education to a client with iron deficiency anemia who has been prescribed iron supplements. What should the nurse include in health education?
Explanation
A. Increase the intake of vitamin E to enhance absorption:
Explanation: Iron absorption can be enhanced by taking vitamin C, not vitamin E. Therefore, this statement is not accurate.
B. Iron will cause the stools to darken in color:
Explanation: This statement is accurate. Iron supplements can cause stools to become darker in color. This is a common and harmless side effect.
C. Take the iron with dairy products to enhance absorption:
Explanation: Calcium-containing foods and supplements can inhibit the absorption of iron. Therefore, it is recommended to avoid taking iron supplements with dairy products.
D. Limit foods high in fiber due to the risk for diarrhea:
Explanation: Iron supplements can cause constipation, not diarrhea. Therefore, limiting foods high in fiber is not necessary.
The nurse is collecting data for a client who has been diagnosed with iron-deficiency anemia. What subjective findings does the nurse recognize as symptoms related to this type of anemia?
Explanation
A. "I have difficulty breathing when walking 30 feet":
Explanation: Difficulty breathing on exertion (dyspnea) is a common symptom of iron-deficiency anemia. This is because iron is a crucial component of hemoglobin, which carries oxygen to body tissues. In the absence of sufficient iron, the oxygen-carrying capacity of the blood is reduced, leading to symptoms such as shortness of breath.
B. "I feel hot all of the time":
Explanation: Feeling hot all the time is not a typical symptom of iron-deficiency anemia. Anemia is more likely to cause symptoms related to poor oxygen delivery, such as fatigue and shortness of breath.
C. "I have a difficult time falling asleep at night":
Explanation: Difficulty falling asleep is not a classic symptom of iron-deficiency anemia. Symptoms are more likely to be related to fatigue and weakness.
D. "I have an increase in my appetite":
Explanation: An increase in appetite is not a typical symptom of iron-deficiency anemia. In fact, individuals with anemia may experience a decrease in appetite.
A nurse is caring for a patient with Addison's Disease. Which of the following clinical manifestations should the nurse expect to observe? (SELECT ALL THAT APPLY)
Explanation
A. Buffalo hump:
Explanation: A buffalo hump is associated with excess cortisol, which is not a typical manifestation of Addison's disease. Instead, patients with Addison's disease may experience weight loss and muscle wasting.
B. Hyponatremia:
Explanation: Correct. Hyponatremia (low sodium levels) can occur in Addison's disease due to the loss of aldosterone, which plays a role in sodium and water balance.
C. Decreased glucose level:
Explanation: Correct. Addison's disease can lead to hypoglycemia (low blood glucose levels) because cortisol, which is important for maintaining blood glucose, is deficient.
D. Weight gain:
Explanation: Weight gain is not a typical manifestation of Addison's disease. Instead, weight loss and muscle wasting may occur.
E. Craving for salt:
Explanation: Correct. Addison's disease can lead to salt craving, as aldosterone deficiency results in increased sodium loss and potassium retention.
The nurse understands causes of respiratory acidosis include: (SELECT ALL THAT APPLY)
Explanation
A. Asthma:
Explanation: Asthma is associated with respiratory alkalosis, not respiratory acidosis. In asthma, there is often hyperventilation leading to a decrease in carbon dioxide levels.
B. Hyperventilation:
Explanation: Correct. Hyperventilation can cause respiratory alkalosis, not respiratory acidosis. It leads to a decrease in carbon dioxide levels.
C. Chronic obstructive pulmonary disease (COPD):
Explanation: Correct. Conditions like COPD can lead to respiratory acidosis. In COPD, there is impaired ventilation, leading to an accumulation of carbon dioxide.
D. Renal insufficiency:
Explanation: Renal insufficiency is not a direct cause of respiratory acidosis. Respiratory acidosis is primarily related to respiratory system dysfunction.
E. Pneumonia:
Explanation: Correct. Pneumonia can cause respiratory acidosis. In pneumonia, there may be difficulty in eliminating carbon dioxide due to impaired gas exchange.
The nurse is monitoring a client who was diagnosed with Type 1 Diabetes Mellitus and is being treated with NPH and regular insulin. Which manifestations alert the nurse to the presence of a possible hypoglycemic reaction? (SELECT ALL THAT APPLY)
Explanation
A. Nervousness:
Explanation: Correct. Nervousness is a common symptom of hypoglycemia.
B. Tremors:
Explanation: Correct. Tremors or shakiness can occur with hypoglycemia.
C. Irritability:
Explanation: Correct. Irritability is one of the signs of hypoglycemia.
D. Anorexia:
Explanation: Anorexia or loss of appetite is a possible symptom of hypoglycemia but not as commonly observed as other symptoms.
E. Hot, dry skin:
Explanation: Hot, dry skin is not typically associated with hypoglycemia. Diaphoresis or sweating is more common.
F. Muscle cramps:
Explanation: Muscle cramps are not typical symptoms of hypoglycemia.
A patient is post-op from knee surgery. The patient has been receiving Morphine 4 mg IV every 2 hours. The nurse notices the patient is exhibiting a respiratory rate of 8 and is extremely drowsy. Which of the following conditions is the patient at risk for?
Explanation
A. Respiratory acidosis:
This occurs when there is inadequate removal of carbon dioxide (CO2) by the respiratory system. In the case of the patient post-op from knee surgery receiving Morphine, the opioid can cause respiratory depression, leading to the retention of CO2 and the development of respiratory acidosis. Signs include a decreased respiratory rate and drowsiness.
B. Hypokalemia:
This is a condition characterized by low levels of potassium in the blood. While opioids can cause constipation, they are not directly associated with hypokalemia.
C. Metabolic acidosis:
This occurs when there is an increase in acid production or a loss of bicarbonate, leading to an imbalance in the body's acid-base status. The symptoms of metabolic acidosis are not typically associated with opioid use.
D. Respiratory alkalosis:
This occurs when there is excessive elimination of CO2, leading to decreased carbon dioxide levels in the blood. Opioids, especially in higher doses, are more likely to cause respiratory depression and acidosis rather than alkalosis. The patient's low respiratory rate and drowsiness are indicative of respiratory acidosis rather than alkalosis.
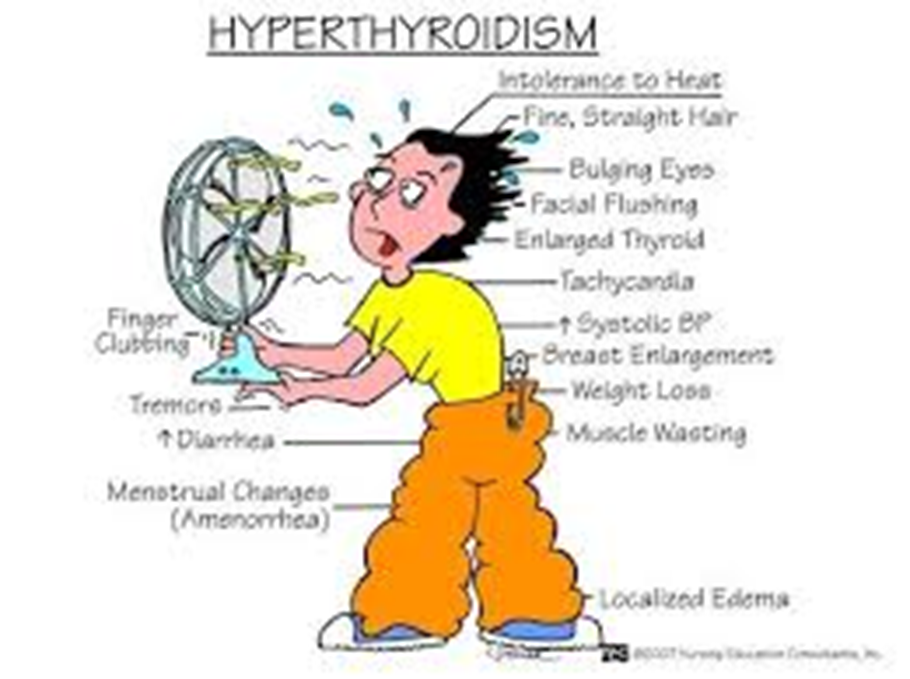
A nurse is performing a physical examination on an adolescent male suspected of having an endocrine disorder. Which of the following assessment findings might be indicative of a problem with the thyroid gland?
Explanation
A. Development of a buffalo hump and moon face:
This is associated with Cushing's syndrome, a disorder characterized by prolonged exposure to high levels of cortisol.
B. Central obesity and purple striations:
Also indicative of Cushing's syndrome, where excess cortisol can lead to the accumulation of fat in the abdominal area (central obesity) and the development of purple stretch marks (striae).
C. Sudden weight loss without dieting:
This is more characteristic of hyperthyroidism, where the thyroid gland is overactive, leading to increased metabolism and unintended weight loss.
D. Positive Trousseau's sign when checking the client's blood pressure:
Trousseau's sign is associated with hypocalcemia and is seen in conditions affecting the parathyroid gland rather than the thyroid. It involves carpal spasm induced by inflating a blood pressure cuff above the systolic pressure for a few minutes.
The nurse is caring for a client with a nasogastric tube that is attached to low suction. The nurse monitors the client for manifestations of which disorder that the client is at risk for?
Explanation
A. Respiratory acidosis:
This occurs when there is inadequate ventilation, leading to an accumulation of carbon dioxide (CO2) in the blood. In the context of a nasogastric tube attached to low suction, respiratory acidosis is not the primary concern. It is more associated with conditions like respiratory depression or lung diseases.
B. Metabolic acidosis:
Metabolic acidosis results from an excess of acid or a loss of bicarbonate. It is not the typical outcome of a nasogastric tube attached to low suction. Conditions like diarrhea or renal failure are more commonly associated with metabolic acidosis.
C. Respiratory alkalosis:
Respiratory alkalosis occurs when there is excessive loss of carbon dioxide from the body, often due to hyperventilation. This is not a typical consequence of a nasogastric tube attached to low suction.
D. Metabolic alkalosis:
Metabolic alkalosis is characterized by an excess of bicarbonate or a loss of acid. In the given context, with the nasogastric tube attached to low suction, there is a potential loss of gastric acid, contributing to metabolic alkalosis.
A client in the emergency department reports that he has been vomiting excessively for the last 2 days. His arterial blood gas (ABG) analysis shows a pH of 7.50, the partial pressure of arterial carbon dioxide (PaCO2) of 43 mm Hg, partial pressure of arterial oxygen (PaO2) of 75 mm Hg, and bicarbonate (HCO3) of 42 mEq/L. Based on these findings, the nurse documents that the client is experiencing which type of acid-base imbalance?
Explanation
A. Metabolic Alkalosis:
pH: Elevated (alkalotic).
PaCO2: Normal or slightly decreased (compensation may or may not be present).
HCO3: Elevated.
Explanation: Metabolic alkalosis is characterized by an excess of bicarbonate (HCO3) in the blood, leading to an elevated pH. In this case, the elevated pH and HCO3 levels suggest that the primary imbalance is metabolic alkalosis.
B. Respiratory Alkalosis:
pH: Elevated (alkalotic).
PaCO2: Decreased (due to hyperventilation, which blows off CO2).
HCO3: Normal or slightly decreased (compensation).
Explanation: Respiratory alkalosis is characterized by low levels of carbon dioxide (PaCO2) due to hyperventilation. However, in the provided ABG, the PaCO2 is not significantly decreased, suggesting that respiratory alkalosis is not the primary issue.
C. Respiratory Acidosis:
pH: Decreased (acidotic).
PaCO2: Increased (due to inadequate ventilation).
HCO3: Normal or slightly elevated (compensation).
Explanation: Respiratory acidosis is characterized by an increase in carbon dioxide (PaCO2) levels. In this case, the PaCO2 is within the normal range, indicating that respiratory acidosis is not the primary problem.
D. Metabolic Acidosis:
pH: Decreased (acidotic).
PaCO2: Normal or slightly decreased (compensation).
HCO3: Decreased.
Explanation: Metabolic acidosis is characterized by a decrease in bicarbonate (HCO3) levels. In this ABG, the HCO3 is elevated, ruling out metabolic acidosis as the primary issue.
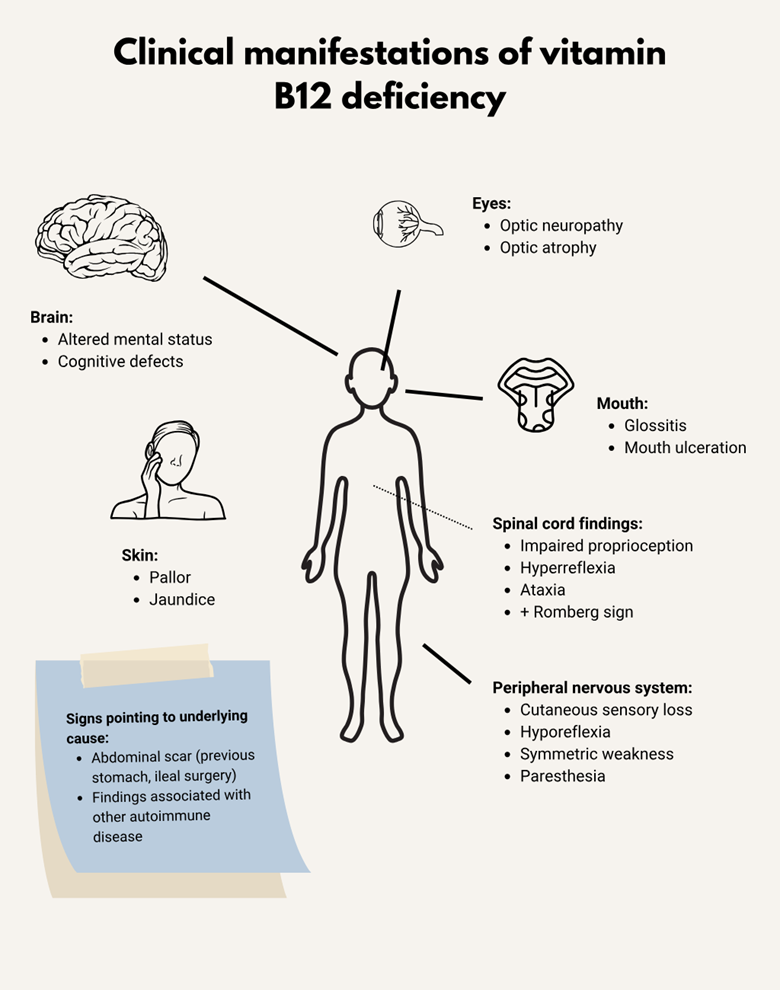
A client comes into the emergency room with complaints of an enlarged tongue. The tongue appears smooth and beefy red in color. The nurse also observes a 5-cm incision on the upper left quadrant of the abdomen. When questioned, the patient states, "I had a partial gastrostomy 2 years ago." Based on this information, the nurse attributes these symptoms to which of the following problems?
Explanation
A. Vitamin A Deficiency:
Symptoms: Enlarged tongue and smooth, beefy red appearance.
Relevance: Vitamin A deficiency is not typically associated with an enlarged tongue. It is more commonly linked to night blindness and skin issues.
B. Folic Acid Deficiency:
Symptoms: Enlarged tongue and smooth, beefy red appearance.
Relevance: Folic acid deficiency can lead to megaloblastic anemia and glossitis (inflammation of the tongue), which may present as an enlarged, smooth, and red tongue.
C. Vitamin B12 Deficiency:
Symptoms: Enlarged tongue and smooth, beefy red appearance.
Relevance: Vitamin B12 deficiency can cause pernicious anemia and glossitis, resulting in an enlarged, smooth, and red tongue.
D. Vitamin C Deficiency:
Symptoms: Not typically associated with an enlarged tongue.
Relevance: Vitamin C deficiency is more commonly associated with symptoms like scurvy, which includes bleeding gums, joint pain, and skin issues, but not specifically an enlarged tongue.
A patient has the following blood gases: PaCO2 33, pH 7.50, HCO3 23. Which of the following could NOT be the cause of this condition?
Explanation
A. Aspirin Toxicity:
Effect on Blood Gases: Aspirin toxicity can cause respiratory alkalosis due to increased respiratory rate (hyperventilation), leading to a decreased PaCO2 and increased pH.
Relation to Given Blood Gases: It could potentially cause the observed blood gas values (low PaCO2 and high pH), making it a possible cause.
B. Fever:
Effect on Blood Gases: Fever might cause hyperventilation, resulting in respiratory alkalosis with decreased PaCO2 and increased pH.
Relation to Given Blood Gases: It could potentially cause the observed blood gas values.
C. Anxiety Attack:
Effect on Blood Gases: Anxiety attacks can lead to hyperventilation and subsequent respiratory alkalosis with low PaCO2 and high pH.
Relation to Given Blood Gases: It could potentially cause the observed blood gas values.
D. Chronic Obstructive Pulmonary Disease (COPD):
Effect on Blood Gases: COPD typically causes respiratory acidosis due to impaired gas exchange, resulting in elevated PaCO2 and decreased pH.
Relation to Given Blood Gases: COPD wouldn't typically cause the observed blood gas values of low PaCO2 and high pH.
A nursing instructor is evaluating a student caring for a neutropenic client. The instructor concludes that the nursing student demonstrates accurate knowledge of neutropenia based on which of the following interventions?
Explanation
A. Monitoring the patient's breathing and reviewing the patient's arterial blood gases:
Rationale: While respiratory status is crucial in any patient assessment, arterial blood gases primarily evaluate respiratory function. Neutropenia directly affects the immune system, not respiratory function.
Appropriateness: Not directly related to assessing neutropenia.
B. Monitoring the patient's temperature and reviewing the patient's complete blood count with differential:
Rationale: Neutropenia can cause fever due to the increased risk of infection. Monitoring temperature and reviewing the complete blood count (CBC) with differential, specifically the neutrophil count, is essential in evaluating neutropenia and identifying potential infections.
Appropriateness: Correct. Monitoring temperature and reviewing CBC with differential are crucial in assessing neutropenia.
C. Monitoring the patient's blood pressure and reviewing the patient's hematocrit:
Rationale: Blood pressure assessment and hematocrit evaluation are essential aspects of general patient care but are not specific to neutropenia.
Appropriateness: Not directly related to assessing neutropenia.
D. Monitoring the patient's heart rate and reviewing the patient's hemoglobin:
Rationale: Heart rate monitoring and hemoglobin assessment are crucial in various clinical situations but are not specific indicators of neutropenia.
Appropriateness: Not directly related to assessing neutropenia.
A nurse is providing education to a client with iron deficiency anemia who has been prescribed iron supplements. What should the nurse include in health education?
Explanation
A. Increase the intake of vitamin E to enhance absorption:
While vitamin C can enhance iron absorption, vitamin E does not play a significant role in iron absorption. Vitamin C-rich foods can be advised to enhance iron absorption.
B. Iron will cause the stools to darken in color:
This statement is accurate. Iron supplements can cause stools to appear darker in color, often black or greenish-black. This change in stool color is normal and expected when taking iron supplements.
C. Take the iron with dairy products to enhance absorption:
Dairy products can inhibit iron absorption. It's better to take iron supplements with vitamin C-rich foods or orange juice to enhance absorption.
D. Limit foods high in fiber due to the risk for diarrhea:
Fiber-rich foods do not necessarily need to be limited when taking iron supplements. However, some individuals may experience constipation when taking iron supplements, in which case increasing fluid intake and dietary fiber can help alleviate constipation.
A medical nurse is caring for a patient with type 1 diabetes. The patient's medication administration record includes the administration of regular insulin three times daily. Knowing that the patient's dinner tray will arrive at 1645, when should the nurse administer the patient's insulin to ensure the onset of the insulin coincides with the start of the meal?
Explanation
A. 1645:
This would be the actual time the dinner tray arrives. Administering regular insulin at this time may not allow sufficient time for it to start working before the meal.
B. 1615:
This is 30 minutes before the dinner tray arrives. It's a reasonable choice, but the standard recommendation is to administer regular insulin about 30 minutes before the meal.
C. 1545:
This is the optimal choice. Administering regular insulin at 1545, 30 minutes before the meal at 1615, allows for its onset of action to coincide with the start of the meal.
D. 1600:
While close to the mealtime, it's slightly earlier than the recommended 30-minute window before the meal. It may still work, but 1545 is a more precise choice for the desired timing.
An occupational health nurse is screen a group of workers for diabetes. What statement should the nurse interpret as being suggestive of diabetes?
Explanation
A. "When I went to the restroom the last few days, my urine smelled odd."
Changes in the smell of urine can be associated with various conditions, including diabetes. However, it's not a specific symptom.
B. "I've always been a fan of sweet foods, but lately I'm turned off by them."
A change in taste preferences may not be directly related to diabetes. It's not a typical symptom.
C. "No matter how much sleep I get, it seems to take me hours to wake up."
Fatigue and difficulty waking up are general symptoms that can be caused by various factors, including diabetes. However, it's not specific to diabetes alone.
D. "Lately, I drink a lot, but I can't seem to quench my thirst."
Excessive thirst (polydipsia) and increased urination (polyuria) are classic symptoms of diabetes, suggesting elevated blood sugar levels.
The nurse is preparing to administer Insulin Lispro (Humalog) to a client with Type 2 Diabetes Mellitus for carbohydrate coverage. The nurse understands the injection should be administered:
Explanation
A. With the meal:
Insulin Lispro is a rapid-acting insulin that is designed to be taken just before or with meals.
It helps control the rise in blood sugar that occurs after eating.
B. Post-prandial:
"Post-prandial" refers to after a meal. Insulin Lispro is usually administered before or with a meal to cover the increase in blood glucose that happens after eating.
C. Pre-prandial:
"Pre-prandial" refers to before a meal. This is accurate for Insulin Lispro, as it is given shortly before or with meals.
D. AC/HS:
"AC" stands for "ante cibum," which means before meals, and "HS" stands for "hora somni," which means at bedtime. This terminology is more commonly associated with the timing of oral medications rather than insulin.
A nurse is conducting a class on how to self-manage insulin regimens. A client asks how long a vial of insulin can be stored at room temperature before it "goes bad." What would be the nurse's best answer?
Explanation
A. "If a vial of insulin will be used up within 21 days, it may be kept at room temperature."
This statement suggests a duration of up to 21 days for room temperature storage after the vial is in use. However, most insulins can typically be stored at room temperature for up to 28 days after initial use. This recommendation might be more conservative than necessary for many types of insulin.
B. "If a vial of insulin will be used up within 2 weeks, it may be kept at room temperature."
This choice suggests a timeframe of 14 days for room temperature storage after opening the vial. However, for many insulins, the recommended duration for room temperature storage after opening is up to 28 days.
C. "If you are going to use up the vial within 1 month, it can be kept at room temperature."
This option extends the timeframe to 1 month for room temperature storage after the vial is in use. However, the generally recommended duration for many insulins is up to 28 days after opening.
D. "If a vial of insulin will be used up within 1 week, it may be kept at room temperature."
This choice suggests a very short duration of 7 days for room temperature storage after opening the vial. Most insulins can typically be stored at room temperature for a longer duration after initial use.
A diabetes educator is teaching a patient about type 2 diabetes. The educator recognizes that the patient understands the primary treatment for type 2 diabetes when the patient states what?
Explanation
A. "I will make sure I call the diabetes educator each time I adjust my insulin dose."
This statement suggests a reliance on insulin adjustment and implies frequent contact with the diabetes educator. However, it doesn't address the primary treatment for type 2 diabetes.
B. "I read that a pancreas transplant will provide a cure for my diabetes."
This statement mentions a pancreas transplant, which is a significant and rare intervention typically reserved for severe cases of diabetes. However, it's not considered the primary treatment for type 2 diabetes.
C. "I will make sure to follow the weight loss plan designed by the dietitian."
This statement aligns with a key aspect of managing type 2 diabetes, as weight management, along with diet and exercise, is a primary approach. Lifestyle modifications, including weight loss, are often part of the primary treatment plan.
D. "I will take my oral anti-diabetic agents when my morning blood sugar is high."
This statement indicates an understanding of the importance of oral anti-diabetic agents, which are commonly used in the management of type 2 diabetes. Timing medication based on blood sugar levels is a key aspect of treatment.
Sign Up or Login to view all the 46 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

