ATI Med Surg Monroe College
Total Questions : 48
Showing 25 questions, Sign in for moreA nurse is caring for a client whose arterial blood gas results show a pH of 7.3 and a PaCO2 of 50 mm Hg. The nurse should identify that the client is experiencing which of the following acid-base imbalances?
Explanation
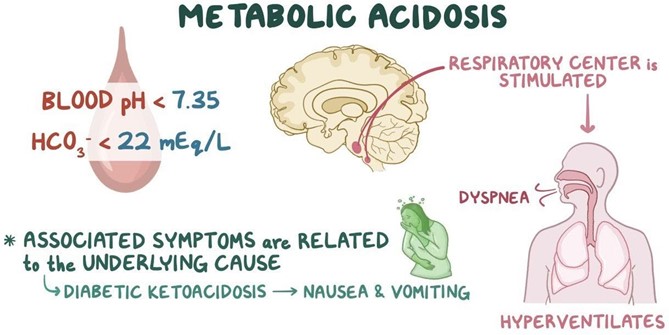
Choice A: Metabolic acidosis is incorrect because it is characterized by a low pH and a low HCO3, not a high PaCO2. Metabolic acidosis occurs when there is an excess of metabolic acids in the body, such as lactic acid, ketoacids, or salicylates.
Choice B: Respiratory alkalosis is incorrect because it is characterized by a high pH and a low PaCO2, not a low pH and a high PaCO2. Respiratory alkalosis occurs when there is excessive loss of carbon dioxide through hyperventilation, such as in anxiety, fever, or aspirin overdose.
Choice C: Respiratory acidosis is correct because it is characterized by a low pH and a high PaCO2. Respiratory acidosis occurs when there is impaired gas exchange or hypoventilation, resulting in accumulation of carbon dioxide in the blood. This can be caused by conditions such as chronic obstructive pulmonary disease (COPD), pneumonia, asthma, or chest trauma.
Choice D: Metabolic alkalosis is incorrect because it is characterized by a high pH and a high HCO3, not a low pH and a high PaCO2. Metabolic alkalosis occurs when there is a loss of metabolic acids or an excess of bicarbonate in the body, such as from vomiting, gastric suctioning, or diuretic therapy.
A nurse is reviewing the laboratory results of a client who is dehydrated. Which of the following BUN lab values should the nurse report to the provider?
Explanation
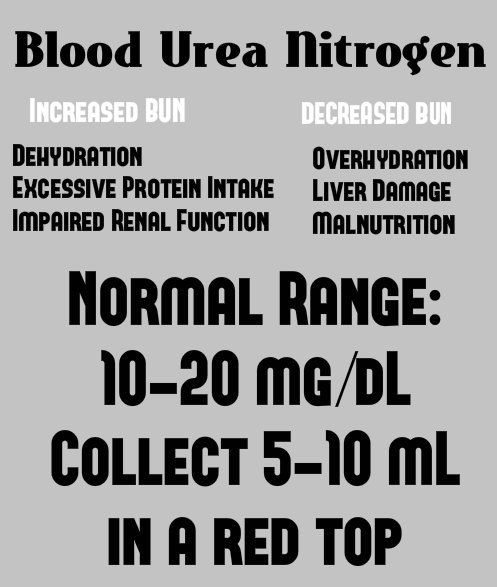
Choice A: 18 mg/dL is incorrect because it is within the normal range of BUN, which is 7 to 20 mg/dL. BUN stands for blood urea nitrogen, which is a measure of the amount of nitrogen in the blood that comes from urea, a waste product of protein metabolism. BUN can reflect the kidney function and hydration status of the client.
Choice B: 10 mg/dL is incorrect because it is also within the normal range of BUN. A low BUN level can indicate liver problems, malnutrition, or overhydration.
Choice C: 13 mg/dL is incorrect because it is also within the normal range of BUN. A normal BUN level does not necessarily rule out dehydration, as other factors such as diet, medications, and blood loss can affect the BUN level.
Choice D: 25 mg/dL is correct because it is above the normal range of BUN and indicates a high BUN level. A high BUN level can indicate dehydration, kidney failure, urinary tract obstruction, heart failure, or excessive protein intake. The nurse should report this value to the provider as it may require further evaluation and treatment.
The nurse is planning care for a patient with severe burns. What health problem should the nurse realize that this patient could develop?
Explanation
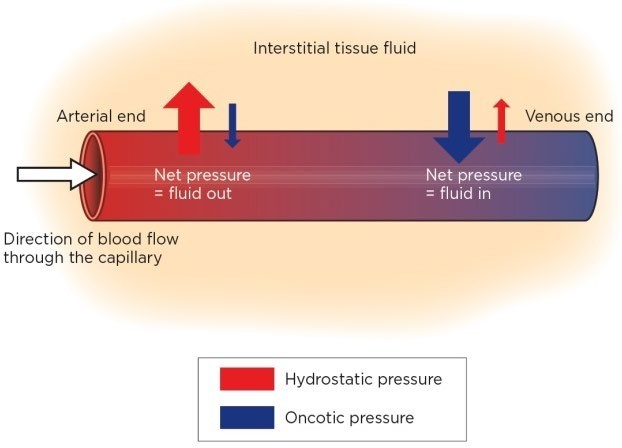
Choice A: Intracellular fluid overload is incorrect because it is a condition where the fluid inside the cells exceeds the normal range. This can cause cellular swelling and dysfunction. Intracellular fluid overload can be caused by conditions such as hyponatremia, water intoxication, or syndrome of inappropriate antidiuretic hormone secretion (SIADH).
Choice B: Intracellular fluid deficit is incorrect because it is a condition where the fluid inside the cells is below the normal range. This can cause cellular shrinkage and dysfunction. Intracellular fluid deficit can be caused by conditions such as hypernatremia, dehydration, or diabetes insipidus.
Choice C: Extracellular fluid deficit is correct because it is a condition where the fluid outside the cells is below the normal range. This can cause hypovolemia, hypotension, and impaired tissue perfusion. Extracellular fluid deficit can be caused by conditions such as burns, hemorrhage, vomiting, diarrhea, or excessive diuresis.
Choice D: Interstitial fluid deficit is incorrect because it is a condition where the fluid in the spaces between the cells is below the normal range. This can cause edema, impaired wound healing, and increased risk of infection. Interstitial fluid deficit can be caused by conditions such as inflammation, infection, or lymphatic obstruction.
A client is admited to the emergency room with a respiratory rate of 7/min. Arterial blood gases (ABG) reveal the following values. Which of the following is an appropriate analysis of the ABGs?
Explanation
Choice A: Metabolic alkalosis is incorrect because it is characterized by a high pH and a high HCO3, not a low pH and a normal HCO3. Metabolic alkalosis occurs when there is a loss of metabolic acids or an excess of bicarbonate in the body, such as from vomiting, gastric suctioning, or diuretic therapy.
Choice B: Respiratory acidosis is correct because it is characterized by a low pH and a high PaCO2. Respiratory acidosis occurs when there is impaired gas exchange or hypoventilation, resulting in accumulation of carbon dioxide in the blood. This can be caused by conditions such as chronic obstructive pulmonary disease (COPD), pneumonia, asthma, or chest trauma.
Choice C: Metabolic acidosis is incorrect because it is characterized by a low pH and a low HCO3, not a low pH and a normal HCO3. Metabolic acidosis occurs when there is an excess of metabolic acids in the body, such as lactic acid, ketoacids, or salicylates.
Choice D: Respiratory alkalosis is incorrect because it is characterized by a high pH and a low PaCO2, not a low pH and a high PaCO2. Respiratory alkalosis occurs when there is excessive loss of carbon dioxide through hyperventilation, such as in anxiety, fever, or aspirin overdose.
The nurse is caring for a patient diagnosed with hypocalcemia. What additional assessments should the nurse include when caring for this patient?
Explanation
Choice A: Hypertension is incorrect because it is not a common complication of hypocalcemia, which is a low level of calcium in the blood. Hypertension, or high blood pressure, can be caused by conditions such as kidney disease, diabetes, or preeclampsia.
Choice B: Drug toxicity is incorrect because it is not directly related to hypocalcemia, although some drugs can affect the calcium level in the blood. For example, loop diuretics can increase the urinary excretion of calcium, while bisphosphonates can inhibit the bone resorption of calcium.
Choice C: Other electrolyte disturbances is correct because hypocalcemia can be associated with other imbalances of electrolytes, such as magnesium, phosphorus, and potassium. For example, hypomagnesemia, or low magnesium level, can impair the secretion and action of parathyroid hormone, which regulates calcium balance.
Hyperphosphatemia, or high phosphorus level, can bind to calcium and lower its availability in the blood. Hypokalemia, or low potassium level, can increase the renal excretion of calcium.
Choice D: Visual disturbances is incorrect because it is not a typical manifestation of hypocalcemia, although severe hypocalcemia can affect the nervous system and cause confusion, hallucinations, or seizures. Visual disturbances can be caused by conditions such as glaucoma, macular degeneration, or diabetic retinopathy.

A nurse is reviewing the arterial blood gas results for a client in the ICU who has kidney failure and determines the client has respiratory acidosis. Which of the following findings should the nurse expect?
Explanation
Choice A: Widened QRS complexes is correct because it is a sign of cardiac dysrhythmias, which can occur in respiratory acidosis due to hyperkalemia, or high potassium level. Respiratory acidosis is a condition where the blood pH is low and the PaCO2 is high, indicating impaired gas exchange or hypoventilation. This can cause potassium to shift from the intracellular fluid to the extracellular fluid, thus raising the serum potassium level and affecting the cardiac conduction.
Choice B: Hyperactive deep tendon reflexes is incorrect because it is a sign of hypocalcemia, or low calcium level, which can occur in metabolic alkalosis, not respiratory acidosis. Metabolic alkalosis is a condition where the blood pH is high and the HCO3 is high, indicating a loss of metabolic acids or an excess of bicarbonate in the body. This can cause calcium to bind to albumin and lower its availability in the blood, thus increasing the neuromuscular excitability.
Choice C: Bounding peripheral pulses is incorrect because it is a sign of fluid overload, which can occur in heart failure, not respiratory acidosis. Fluid overload is a condition where the fluid volume in the body exceeds the normal range, causing edema, hypertension, and dyspnea. This can be caused by conditions such as kidney disease, liver disease, or excessive sodium intake.
Choice D: Warm, flushed skin is incorrect because it is a sign of vasodilation, which can occur in respiratory alkalosis, not respiratory acidosis. Respiratory alkalosis is a condition where the blood pH is high and the PaCO2 is low, indicating excessive loss of carbon dioxide through hyperventilation. This can cause the blood vessels to dilate and increase the blood flow to the skin, thus causing warmth and redness.
A patient is diagnosed with hypokalemia. After reviewing the patient's current medications, which drug should the nurse consider that might have contributed to the patient's health problem?
Explanation
Choice A: Corticosteroid is incorrect because it does not directly affect the potassium level in the blood, although it can cause sodium and water retention, which can dilute the potassium concentration. Corticosteroid is a type of anti- inflammatory medication that can be used to treat conditions such as asthma, arthritis, or allergic reactions.
Choice B: Narcotic is incorrect because it does not directly affect the potassium level in the blood, although it can cause respiratory depression, which can lead to respiratory acidosis and hyperkalemia, or high potassium level. Narcotic is a type of analgesic medication that can be used to treat moderate to severe pain.
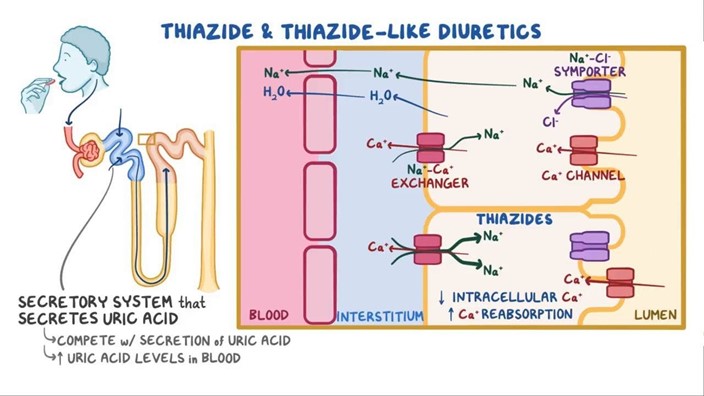
Choice C: Thiazide diuretic is correct because it is a type of medication that increases urine output and sodium excretion, but also causes potassium loss in the urine. Thiazide diuretic can be used to treat conditions such as hypertension, edema, or heart failure.
Choice D: Muscle relaxer is incorrect because it does not directly affect the potassium level in the blood, although it can cause muscle weakness, which can mimic the symptoms of hypokalemia. Muscle relaxer is a type of medication that can be used to treat conditions such as muscle spasms, back pain, or fibromyalgia.
A nurse is reviewing the medical record of a client who has a potassium level of 3.0 mEq/L. Which of the following findings should the nurse recognize as a potential causative factor?
Explanation
Choice A: Client is currently prescribed spironolactone is incorrect because spironolactone is a potassium-sparing diuretic that can cause hyperkalemia, or high potassium level, not hypokalemia, or low potassium level. Spironolactone works by blocking the action of aldosterone, which is a hormone that regulates sodium and potassium balance in the body.
Choice B: Client reports drinking 3.5 to 4 L of water each day is incorrect because drinking excessive water can cause hyponatremia, or low sodium level, not hypokalemia. Hyponatremia occurs when the water intake exceeds the water output, diluting the sodium concentration in the blood.
Choice C: Client has an NG tube to gastric suction is correct because gastric suction can cause hypokalemia by removing gastric fluids that contain potassium. Gastric suction can also cause metabolic alkalosis, which is a condition where the blood pH is high and the HCO3 is high, indicating a loss of metabolic acids or an excess of bicarbonate in the body. Metabolic alkalosis can cause potassium to shift from the extracellular fluid to the intracellular fluid, thus lowering the serum potassium level.
Choice D: Client has a history of alcohol abuse disorder is incorrect because alcohol abuse can cause hypomagnesemia, or low magnesium level, not hypokalemia. Hypomagnesemia occurs when there is inadequate intake or excessive loss of magnesium, which is an essential mineral for many enzymatic reactions in the body.
Hypomagnesemia can impair the secretion and action of parathyroid hormone, which regulates calcium and phosphorus balance in the body.
A patient is diagnosed with hypokalemia. After reviewing the patient's current medications, which drug should the nurse consider that might have contributed to the patient's health problem?
Explanation
Choice A: Corticosteroid is incorrect because it does not directly affect the potassium level in the blood, although it can cause sodium and water retention, which can dilute the potassium concentration. Corticosteroid is a type of anti- inflammatory medication that can be used to treat conditions such as asthma, arthritis, or allergic reactions.
Choice B: Narcotic is incorrect because it does not directly affect the potassium level in the blood, although it can cause respiratory depression, which can lead to respiratory acidosis and hyperkalemia, or high potassium level. Narcotic is a type of analgesic medication that can be used to treat moderate to severe pain.
Choice C: Thiazide diuretic is correct because it is a type of medication that increases urine output and sodium excretion, but also causes potassium loss in the urine. Thiazide diuretic can be used to treat conditions such as hypertension, edema, or heart failure.
Choice D: Muscle relaxer is incorrect because it does not directly affect the potassium level in the blood, although it can cause muscle weakness, which can mimic the symptoms of hypokalemia. Muscle relaxer is a type of medication that can be used to treat conditions such as muscle spasms, back pain, or fibromyalgia.
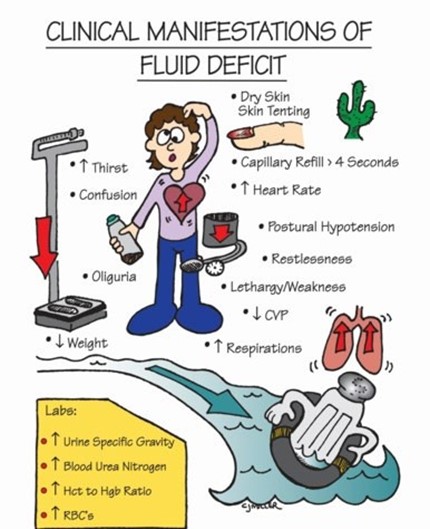
A nurse is reviewing the laboratory results of a client who has fluid volume deficit. The nurse would expect which of the following findings?
Explanation
Choice A: Sodium 155 mEq/L is correct because it indicates hypernatremia, or high sodium level, which can occur in fluid volume deficit due to dehydration, excessive sweating, or diuretic therapy. Sodium is an electrolyte that regulates fluid balance and osmotic pressure in the body. The normal range of sodium is 135 to 145 mEq/L.
Choice B: Hematocrit 44% is incorrect because it is within the normal range of hematocrit, which is the percentage of red blood cells in the blood. Hematocrit can reflect the oxygen-carrying capacity and viscosity of the blood. The normal range of hematocrit is 37% to 47% for females and 42% to 52% for males.
Choice C: Urine specific gravity 1.035 is correct because it indicates a high urine concentration, which can occur in fluid volume deficit due to decreased urine output and increased solute excretion. Urine specific gravity is a measure of the density of urine compared to water. The normal range of urine specific gravity is 1.005 to 1.030.
Choice D: BUN 19 mg/dL is incorrect because it is within the normal range of BUN, which stands for blood urea nitrogen, and is a measure of the amount of nitrogen in the blood that comes from urea, a waste product of protein metabolism. BUN can reflect the kidney function and hydration status of the client. The normal range of BUN is 7 to 20 mg/dL.
A patient is admited with hypernatremia caused by being stranded on a boat in the Atlantic Ocean for two days without water. What is the patient at risk for developing?
Explanation
Choice A: Cerebral bleeding is incorrect because it is not a common complication of hypernatremia, which is a high sodium level in the blood. Cerebral bleeding can be caused by conditions such as head trauma, stroke, or aneurysm.
Choice B: Pulmonary edema is incorrect because it is a condition where fluid accumulates in the lungs, causing shortness of breath, coughing, and wheezing. Pulmonary edema can be caused by conditions such as heart failure, kidney failure, or lung injury.
Choice C: Cardiac arrhythmias is correct because it is a condition where the heart beats irregularly, too fast, or too slow. Cardiac arrhythmias can be caused by hypernatremia, which can affect the electrical activity and contractility of the heart muscle. Hypernatremia can also cause dehydration, hypovolemia, and hypotension, which can impair the blood flow and oxygen delivery to the heart.
Choice D: Seizures is incorrect because it is a condition where abnormal electrical activity in the brain causes convulsions, loss of consciousness, or altered behavior. Seizures can be caused by conditions such as epilepsy, brain tumor, or infection.

A patient with atrial fibrillation and a serum potassium level of 3.0 mEq/L takes digoxin (Lanoxin), ASA (aspirin), KCL (potassium chloride) and warfarin (Coumadin) daily. The patient reports visual disturbances. The nurse suspects problems with which medication?
Explanation
Choice A: Digoxin is correct because it is a medication that can cause visual disturbances, such as blurred vision, yellow-green halos, or photophobia, as a sign of digoxin toxicity. Digoxin toxicity can occur when the serum digoxin level exceeds the therapeutic range of 0.5 to 2 ng/mL. Digoxin toxicity can also cause nausea, vomiting, anorexia, confusion, bradycardia, and cardiac arrhythmias. The risk of digoxin toxicity is increased by hypokalemia, which can lower the threshold for digoxin action and enhance its effects on the cardiac muscle.
Choice B: Aspirin is incorrect because it is a medication that can cause gastrointestinal bleeding, tinnitus, or allergic reactions, but not visual disturbances. Aspirin is an antiplatelet and anti-inflammatory medication that can be used to prevent thromboembolic events, such as stroke or myocardial infarction, in patients with atrial fibrillation.
Choice C: Potassium chloride is incorrect because it is a medication that can cause hyperkalemia, or high potassium level, if taken in excess or in combination with other potassium-sparing drugs, but not visual disturbances. Potassium chloride is a supplement that can be used to treat or prevent hypokalemia, or low potassium level, in patients who are taking diuretics or have other causes of potassium loss.
Choice D: Warfarin is incorrect because it is a medication that can cause bleeding, bruising, or hematoma formation, but not visual disturbances. Warfarin is an anticoagulant that can be used to prevent thromboembolic events, such as stroke or pulmonary embolism, in patients with atrial fibrillation.

A patient with atrial fibrillation and a serum potassium level of 3.0 mEq/L takes digoxin (Lanoxin), ASA (aspirin), KCL (potassium chloride) and warfarin (Coumadin) daily. The patient reports visual disturbances. The nurse suspects problems with which medication?
Explanation
Choice A: Digoxin is correct because it is a medication that can cause visual disturbances, such as blurred vision, yellow-green halos, or photophobia, as a sign of digoxin toxicity. Digoxin toxicity can occur when the serum digoxin level exceeds the therapeutic range of 0.5 to 2 ng/mL. Digoxin toxicity can also cause nausea, vomiting, anorexia, confusion, bradycardia, and cardiac arrhythmias. The risk of digoxin toxicity is increased by hypokalemia, which can lower the threshold for digoxin action and enhance its effects on the cardiac muscle.
Choice B: Aspirin is incorrect because it is a medication that can cause gastrointestinal bleeding, tinnitus, or allergic reactions, but not visual disturbances. Aspirin is an antiplatelet and anti-inflammatory medication that can be used to prevent thromboembolic events, such as stroke or myocardial infarction, in patients with atrial fibrillation.
Choice C: Potassium chloride is incorrect because it is a medication that can cause hyperkalemia, or high potassium level, if taken in excess or in combination with other potassium-sparing drugs, but not visual disturbances. Potassium chloride is a supplement that can be used to treat or prevent hypokalemia, or low potassium level, in patients who are taking diuretics or have other causes of potassium loss.
Choice D: Warfarin is incorrect because it is a medication that can cause bleeding, bruising, or hematoma formation, but not visual disturbances. Warfarin is an anticoagulant that can be used to prevent thromboembolic events, such as stroke or pulmonary embolism, in patients with atrial fibrillation.
A nurse is caring for a client who is receiving IV fluids to correct dehydration. Which of the following laboratory values should indicate to the nurse that the client is effectively responding to treatment?
Explanation
Choice A: Sodium 165 mEq/L is incorrect. This value indicates hypernatremia, which is a high level of sodium in the blood. Hypernatremia can be caused by dehydration, but it does not indicate that the client is responding to treatment. A normal sodium level is between 135 and 145 mEq/L.
Choice B: Potassium 5.2 mEq/L is incorrect. This value indicates hyperkalemia, which is a high level of potassium in the blood. Hyperkalemia can be caused by dehydration, but it does not indicate that the client is responding to treatment. A normal potassium level is between 3.5 and 5.0 mEq/L.
Choice C: Urine specific gravity 1.020 is correct. This value indicates that the urine is concentrated, but within the normal range. Urine specific gravity measures the amount of solutes in the urine compared to water. A high urine specific gravity indicates dehydration, while a low urine specific gravity indicates overhydration. A normal urine specific gravity is between 1.005 and 1.030.
Choice D: Hct 62% is incorrect. This value indicates polycythemia, which is a high level of red blood cells in the blood. Polycythemia can be caused by dehydration, but it does not indicate that the client is responding to treatment. A normal hematocrit (Hct) level is between 37% and 52% for men and between 32% and 47% for women.
A nurse is reviewing the laboratory values of a client who has respiratory acidosis. Which of the following findings should the nurse expect?
Explanation
The correct answer is a) PaCO2 50 mm Hg. This is because respiratory acidosis is a condition in which the lungs cannot remove enough carbon dioxide from the blood, resulting in a high level of PaCO2. The normal range of PaCO2 is 35 to 45 mm Hg.
Choice b) HCO3 30 mEq/L is incorrect because this is a normal value for bicarbonate, which is a buffer that helps maintain the acid-base balance in the blood. The normal range of HCO3 is 22 to 26 mEq/L.
Choice c) pH 7.45 is incorrect because this is a normal value for the acidity or alkalinity of the blood. The normal range of pH is 7.35 to 7.45. Respiratory acidosis causes a low pH, indicating acidemia.
Choice d) Potassium 3.3 mEq/L is incorrect because this is a low value for potassium, which is an electrolyte that helps regulate nerve and muscle function, fluid balance, and blood pressure. The normal range of potassium is 3.5 to 5.0 mEq/L. Respiratory acidosis can cause hyperkalemia, or high potassium levels, due to the shift of hydrogen ions into cells and potassium out of cells.
A patient's blood gases show a pH of 7.53 and bicarbonate level of 36 mEq/L. The nurse realizes that the patient is demonstrating which acid-base disorder?
Explanation
- Choice A: Respiratory acidosis is a condition that occurs when the lungs cannot remove enough carbon dioxide from the body, resulting in a low pH and a high bicarbonate level. This is not the case for the patient, who has a high pH and a high bicarbonate level.
- Choice B: Metabolic acidosis is a condition that occurs when the body produces too much acid or loses too much base, resulting in a low pH and a low bicarbonate level. This is not the case for the patient, who has a high pH and a high bicarbonate level.
- Choice C: Metabolic alkalosis is a condition that occurs when the body loses too much acid or gains too much base, resulting in a high pH and a high bicarbonate level. This is the case for the patient, who has a high pH and a high bicarbonate level.
- Choice D: Respiratory alkalosis is a condition that occurs when the lungs remove too much carbon dioxide from the body, resulting in a high pH and a low bicarbonate level. This is not the case for the patient, who has a high pH and a high bicarbonate level.
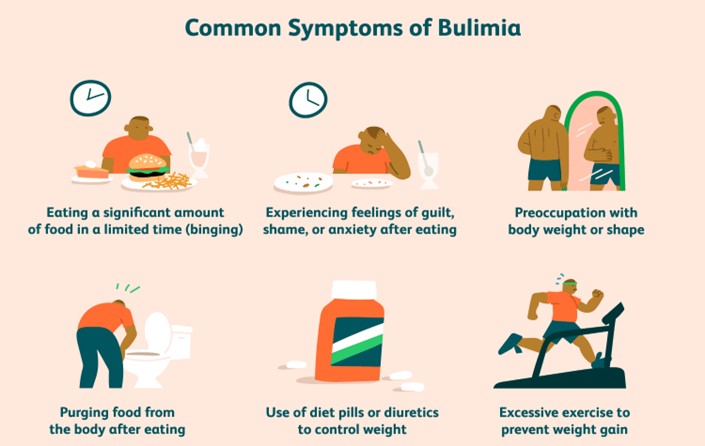
The nurse is reviewing the health problems for a group of assigned patients. Which patient does the nurse recognize as being at increased risk for developing metabolic alkalosis?
Explanation
Choice A: A patient with venous stasis ulcer is not at increased risk for metabolic alkalosis, because this condition does not affect the acid-base balance of the body. Venous stasis ulcer is a chronic wound that occurs due to impaired blood flow in the lower extremities.
Choice B: A patient on dialysis is not at increased risk for metabolic alkalosis, because dialysis helps to remove excess acids and bases from the blood. Dialysis is a treatment that filters and purifies the blood using a machine.
Choice C: A patient with bulimia is at increased risk for metabolic alkalosis, because this condition involves frequent vomiting that causes loss of gastric acid. Gastric acid is a source of hydrogen ions that lowers the pH of the blood. When gastric acid is lost, the blood becomes more alkaline.
Choice D: A patient with COPD is not at increased risk for metabolic alkalosis, but rather for respiratory acidosis. This is because COPD impairs the ability of the lungs to eliminate carbon dioxide, which is a source of carbonic acid that lowers the pH of the blood. When carbon dioxide accumulates, the blood becomes more acidic.
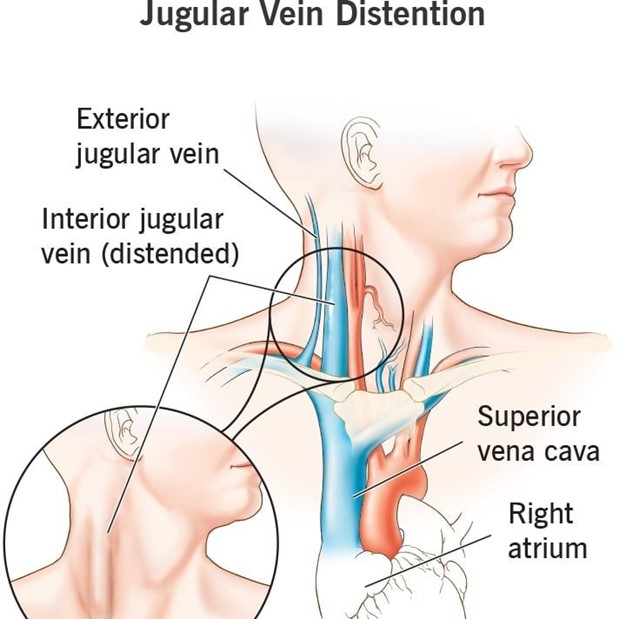
A postoperative patient is diagnosed with fluid volume overload. What should the nurse expect to assess in this patient?
Explanation
Choice A: Concentrated hemoglobin and hematocrit levels are not a sign of fluid volume overload, but rather of fluid volume deficit. This is a condition that occurs when the body loses more fluid than it gains. This can happen in patients who have excessive bleeding, vomiting, diarrhea, or diaphoresis. Concentrated hemoglobin and hematocrit levels indicate hemoconcentration, which is an increase in the ratio of blood cells to plasma.
Choice B: Distended neck veins are a sign of fluid volume overload, because this condition occurs when the body retains more fluid than it excretes. This can happen in patients who have heart failure, kidney failure, or excessive fluid intake. Distended neck veins indicate increased central venous pressure, which is a measure of the pressure in the right atrium of the heart.
Choice C: Decreased urine output is not a sign of fluid volume overload, but rather of oliguria or anuria. These are conditions that occur when the urine output is less than 400 mL or 50 mL per day, respectively. These can happen in patients who have acute or chronic kidney injury, urinary obstruction, or shock. Decreased urine output indicates impaired renal function and decreased glomerular filtration rate.
Choice D: Poor skin turgor is not a sign of fluid volume overload, but rather of dehydration. This is a condition that occurs when the body loses more water than it gains. This can happen in patients who have fever, diabetes insipidus, or hyperglycemia. Poor skin turgor indicates decreased skin elasticity and delayed return to normal shape after being pinched.
A nurse is reviewing the medical records of four clients who have an acid-base imbalance. The nurse should recognize that which of the following clients is at risk for metabolic acidosis?
Explanation
Choice A: A client who is taking a thiazide diuretic is not at risk for metabolic acidosis, but rather for metabolic alkalosis. This is a condition that occurs when the body has too much bicarbonate or loses too much acid. This can happen in patients who take thiazide diuretics, which increase the excretion of sodium, chloride, and water, but also cause the retention of bicarbonate.
Choice B: A client who has diarrhea is at risk for metabolic acidosis, because this condition occurs when the body produces too much acid or loses too much bicarbonate. This can happen in patients who have diarrhea, which causes the loss of intestinal fluids that contain bicarbonate and other bases.
Choice C: A client who is vomiting is not at risk for metabolic acidosis, but rather for metabolic alkalosis. This is a condition that occurs when the body has too much bicarbonate or loses too much acid. This can happen in patients who have vomiting, which causes the loss of gastric fluids that contain hydrochloric acid and other acids.
Choice D: A client who has salicylate intoxication is at risk for metabolic acidosis, because this condition occurs when the body produces too much acid or loses too much bicarbonate. This can happen in patients who have salicylate intoxication, which is a toxic reaction to aspirin or other salicylates. Salicylates increase the production of organic acids and interfere with the renal excretion of acids.
An older patient comes into the clinic complaining of watery diarrhea for several days with abdominal and muscle cramping. The nurse realizes that this patient is demonstrating which imbalance?
Explanation
Choice A: Hyperkalemia is not an imbalance that this patient is demonstrating, because this condition occurs when the blood potassium level is too high. This can happen in patients who have renal failure, acidosis, or excessive potassium intake. Hyperkalemia can cause muscle weakness, cardiac arrhythmias, and paralysis.
Choice B: Hyponatremia is an imbalance that this patient is demonstrating, because this condition occurs when the blood sodium level is too low. This can happen in patients who have watery diarrhea, which causes the loss of sodium and water from the body. Hyponatremia can cause abdominal and muscle cramping, nausea, confusion, and seizures.
Choice C: Fluid volume excess is not an imbalance that this patient is demonstrating, because this condition occurs when the body retains more fluid than it excretes. This can happen in patients who have heart failure, kidney failure, or excessive fluid intake. Fluid volume excess can cause edema, distended neck veins, and crackles in the lungs.
Choice D: Hypernatremia is not an imbalance that this patient is demonstrating, because this condition occurs when the blood sodium level is too high. This can happen in patients who have dehydration, diabetes insipidus, or excessive sodium intake. Hypernatremia can cause thirst, dry mucous membranes, agitation, and coma.
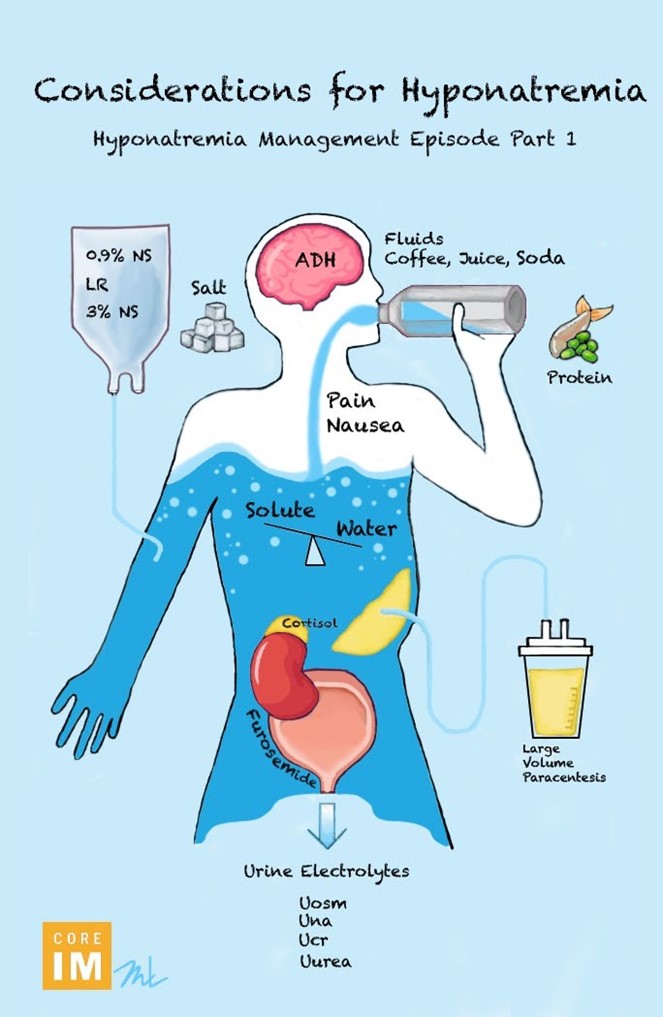
A nurse is caring for a patient whose sodium level is 118 mEq/L. Which nursing diagnosis is a priority for this patient?
Explanation
Choice A: Comfort, Impaired is not a priority nursing diagnosis for this patient, because this condition is not directly related to the low sodium level. Comfort, Impaired is a state of physical or psychological discomfort that can affect the patient's well-being and quality of life.
Choice B: Disturbed Sensory Perception is a priority nursing diagnosis for this patient, because this condition is a serious complication of the low sodium level. Disturbed Sensory Perception is a state of altered or impaired perception of reality that can affect the patient's cognitive and neurological functions. Low sodium level can cause cerebral edema, which is a swelling of the brain that can lead to confusion, seizures, coma, and death.
Choice C: Deficient Fluid Volume is not a priority nursing diagnosis for this patient, because this condition is not the cause of the low sodium level. Deficient Fluid Volume is a state of decreased intravascular, interstitial, or intracellular fluid that can affect the patient's fluid and electrolyte balance. Low sodium level can be caused by excess fluid intake, fluid retention, or loss of sodium from the body.
Choice D: Risk for Injury is not a priority nursing diagnosis for this patient, because this condition is not specific to the low sodium level. Risk for Injury is a state of vulnerability to physical or psychological harm that can affect the patient's safety and health. Low sodium level can increase the risk of injury from falls, accidents, or seizures.
A nurse is reviewing the laboratory results of a client who takes furosemide. Which of the following results should the nurse identify as the priority finding?
Explanation
- Choice A Reason: This is the correct answer because potassium 2.9 mEq/L indicates hypokalemia, which is a common and potentially lifethreatening adverse effect of furosemide. Hypokalemia can cause cardiac arrhythmias, muscle weakness, and paralysis. The nurse should report this finding to the provider and monitor the client's vital signs and electrocardiogram.
- Choice B Reason: This is incorrect because calcium 8.2 mg/dL is within the normal range of 8.5 to 10.5 mg/dL. Furosemide does not affect calcium levels significantly, and this result does not indicate an urgent problem for the client.
- Choice C Reason: This is incorrect because phosphorus 4.5 mEq/L is within the normal range of 2.5 to 4.5 mEq/L. Furosemide does not affect phosphorus levels significantly, and this result does not indicate an urgent problem for the client.
- Choice D Reason: This is incorrect because sodium 145 mEq/L is within the normal range of 135 to 145 mEq/L. Furosemide can cause hyponatremia, which is a low sodium level, but this result does not indicate that condition. The nurse should monitor the client's fluid balance and intake and output, but this result does not require immediate action.

A nurse is caring for four hospitalized clients. Which of the following clients should the nurse identify as being at risk for fluid volume deficit?
Explanation
- Choice A Reason: This is correct because the client who has gastroenteritis and is febrile is likely to lose fluid through vomiting, diarrhea, and sweating. These losses can lead to dehydration, hypotension, and electrolyte imbalances. The nurse should monitor the client's vital signs, fluid intake and output, and weight, and administer fluids and electrolytes as ordered.
- Choice B Reason: This is incorrect because the client who has leftsided heart failure and has a BNP level of 600 pg/ml is likely to have fluid volume excess, not deficit. BNP is a hormone that is released by the heart when it is stretched by increased blood volume. A high BNP level indicates that the heart is failing to pump effectively and that fluid is accumulating in the lungs and other tissues. The nurse should monitor the client's respiratory status, oxygen saturation, edema, and weight, and administer diuretics and other medications as ordered.
- Choice C Reason: This is incorrect because the client who has endstage renal failure and is scheduled for dialysis today is likely to have fluid volume excess, not deficit. Renal failure impairs the kidney's ability to excrete fluid and waste products, leading to fluid retention and azotemia. Dialysis is a procedure that removes excess fluid and toxins from the blood using an artificial membrane. The nurse should monitor the client's blood pressure, fluid intake and output, weight, and laboratory values, and prepare the client for dialysis as ordered.
- Choice D Reason: This is incorrect because the client who has been NPO since midnight for endoscopy is unlikely to have a significant fluid volume deficit, unless they have other risk factors or comorbidities. NPO means nothing by mouth, which is a common instruction before certain procedures or surgeries to prevent aspiration. Endoscopy is a procedure that uses a flexible tube with a camera to examine the digestive tract. The nurse should verify the client's NPO status, check their consent form, and administer preoperative medications as ordered.
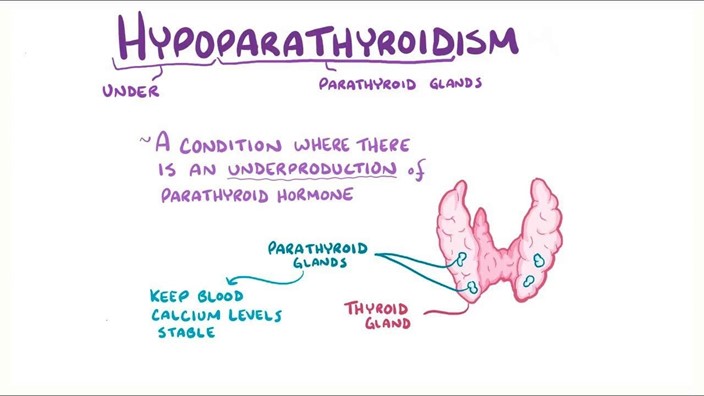
A nurse is reviewing the laboratory results for four clients. The nurse should recognize which of the following clients has a manifestation of hypoparathyroidism?
Explanation
Choice A Reason: This is correct because a phosphate of 5.7 mg/dL indicates hyperphosphatemia, which is a high level of phosphate in the blood. Hyperphosphatemia is a common manifestation of hypoparathyroidism, which is a condition that causes low levels of parathyroid hormone (PTH). PTH regulates calcium and phosphate balance in the body, and low PTH leads to decreased calcium and increased phosphate levels. The nurse should monitor the client's neuromuscular and cardiovascular status, and administer calcium and vitamin D supplements as ordered.
Choice B Reason: This is incorrect because a calcium of 9.8 mg/dL is within the normal range of 8.5 to 10.5 mg/dL. Hypoparathyroidism causes hypocalcemia, which is a low level of calcium in the blood. Calcium is essential for muscle contraction, nerve transmission, and blood clotting, and low calcium levels can cause tetany, seizures, and cardiac arrhythmias. The nurse should monitor the client's vital signs, electrocardiogram, and Chvostek's and Trousseau's signs, and administer calcium and vitamin D supplements as ordered.
Choice C Reason: This is incorrect because a magnesium of 1.8 mEq/L is within the normal range of 1.5 to 2.5 mEq/L. Hypoparathyroidism does not affect magnesium levels significantly, and this result does not indicate an urgent problem for the client.
Choice D Reason: This is incorrect because a vitamin D of 25 ng/mL is within the normal range of 20 to 50 ng/mL. Hypoparathyroidism causes low levels of vitamin D, which is needed for calcium absorption and bone health. Vitamin D deficiency can cause rickets, osteomalacia, and osteoporosis. The nurse should monitor the client's bone density and fractures, and administer vitamin D supplements as ordered.
The patient who has a serum magnesium level of 1.4 mg/dL is being treated with dietary modification. Which foods should the nurse suggest for this patient?
Explanation
Choice A Reason: This is correct because almonds are a rich source of magnesium, which is a mineral that is essential for nerve and muscle function, blood pressure regulation, and bone health. A serum magnesium level of 1.4 mg/dL indicates hypomagnesemia, which is a low level of magnesium in the blood. Hypomagnesemia can cause muscle weakness, cramps, tremors, seizures, and cardiac arrhythmias. The nurse should encourage the patient to eat foods high in magnesium, such as almonds, which contain about 80 mg of magnesium per ounce.
Choice B Reason: This is incorrect because white rice is a poor source of magnesium, as most of the magnesium is lost during the refining process. White rice contains only about 19 mg of magnesium per cup, which is not enough to meet the daily requirement of 310 to 420 mg for adults. The nurse should advise the patient to choose whole grains instead of refined grains, as they have more magnesium and other nutrients.
Choice C Reason: This is incorrect because seafood is a moderate source of magnesium, but not as high as almonds or other nuts and seeds. Seafood contains about 30 to 50 mg of magnesium per 3-ounce serving, depending on the
type and preparation method. The nurse should inform the patient that seafood can be part of a balanced diet, but it
is not the best choice for increasing magnesium intake.
Choice D Reason: This is incorrect because lean red meat is a low source of magnesium, as most of the magnesium is found in the bones and organs of animals. Lean red meat contains only about 20 mg of magnesium per 3-ounce serving, which is less than 10% of the daily requirement. The nurse should caution the patient that lean red meat can also be high in saturated fat and cholesterol, which can increase the risk of cardiovascular disease.
Choice E Reason: This is incorrect because romaine letuce is a very low source of magnesium, as most leafy greens have low mineral content due to their high water content. Romaine letuce contains only about 7 mg of magnesium per cup, which is negligible compared to the daily requirement. The nurse should suggest the patient to add other vegetables that are higher in magnesium, such as spinach, broccoli, or potatoes, to their salads.
Sign Up or Login to view all the 48 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

