Ati med surg RN Helene fuld college nurs 221A exam
Total Questions : 40
Showing 25 questions, Sign in for morePhenytoin (Dilantin) suspension 200 mg is prescribed for a client with epilepsy.The suspension contains 125 mg/5 ml. How much solution should the nurse administer? Record your answer using a whole number.
Explanation
Step 1: Determine the desired dose in mL.
We need to convert the desired dose of 200 mg to mL based on the concentration of the suspension (125 mg/5 mL). We can achieve this using the following proportion:
Desired dose (mg) / Concentration (mg/mL) = Volume (mL) Step 2: Perform the calculation.
Substituting the known values:
200 mg / 125 mg/mL = Volume (mL) Solving for the volume:
Volume = 200 mg / 125 mg/mL
Volume ≈ 1.6 mL
Step 3: Round the answer to a whole number, considering clinical practice.
In medication administration, especially for liquid volumes, doses are typically rounded to a whole number for accuracy and to avoid medication waste. Rounding up to 2 mL would be inaccurate and potentially lead to an overdose. Therefore, we round down to the nearest whole number, which is 1 mL.
Step 4: Adjust the dose based on minimum volume recommendations (Optional).
Some medication suspensions have minimum recommended volumes for accurate dosing, regardless of the calculated dose. Consult the specific medication guidelines to determine if there is a minimum volume requirement. In this case, if the medication guidelines recommend not administering less than 5 mL, then the nurse would administer 5 mL as the minimum safe volume, even though the calculated dose is lower.
Therefore, based on the calculations and considering potential volume minimums, the nurse should administer 8 mL of the phenytoin suspension.
A nurse is discussing gout with a patient who is concerned about developing the disorder. Which of the following findings should the nurse identify as risk factors for this disease? Select all that applies.
Explanation
Cardiovascular disease (CVD) is a significant risk factor for gout. This is because CVD often coexists with other conditions that can elevate uric acid levels, such as hypertension, obesity, and chronic kidney disease. Additionally, some medications used to treat CVD, such as thiazide diuretics, can also increase uric acid levels.
Research has shown that people with CVD have a 2-3 times higher risk of developing gout compared to those without CVD.
The mechanisms linking CVD and gout are complex and not fully understood, but they likely involve shared pathways of inflammation and endothelial dysfunction.
Choice D rationale:
Diuretic use, particularly thiazide diuretics, is a well-established risk factor for gout. These medications work by increasing the excretion of fluids and electrolytes from the body, which can also lead to a decrease in the excretion of uric acid.
This can result in a buildup of uric acid in the blood, which can then crystallize in joints and cause gout attacks.
The risk of gout associated with diuretic use is dose-dependent, meaning that higher doses of diuretics are associated with a higher risk of gout.
Choice A rationale:
Depression has not been consistently shown to be an independent risk factor for gout. Some studies have suggested a possible link between depression and gout, but others have not found any association. More research is needed to clarify the relationship between these two conditions.
Choice B rationale:
Deep sleep deprivation has not been studied as a risk factor for gout. There is currently no evidence to suggest that it is directly associated with an increased risk of developing the disease.
What is the nurse's primary consideration when caring for a client with rheumatoid arthritis?
Explanation
Choice A rationale:
Pain management: Rheumatoid arthritis (RA) is a chronic inflammatory disease that causes pain, stiffness, swelling, and fatigue in the joints. Pain is often the most debilitating symptom of RA, and it can significantly impact a person's quality of life.
Therefore, the nurse's primary consideration is to ensure the client's comfort by effectively managing their pain. This may involve using a variety of interventions, such as:
Administering pain medications as prescribed Applying heat or cold therapy
Using assistive devices to reduce joint strain
Teaching the client about pain management techniques, such as relaxation exercises and pacing activities
Promoting rest and sleep: Rest and sleep are essential for healing and reducing inflammation. The nurse can encourage the client to rest during the day and to get enough sleep at night.
Creating a comfortable environment: The nurse can help to create a comfortable environment for the client by adjusting the room temperature, providing soft bedding and pillows, and reducing noise and distractions.
Providing emotional support: RA can be a challenging disease to live with, and it can take a toll on a person's emotional well- being. The nurse can provide emotional support by listening to the client's concerns, offering reassurance, and encouraging them to express their feelings.
Choice B rationale:
Motivation is important: While motivation is important for self-management of RA, it is not the primary consideration for the nurse. The nurse's focus is on providing comfort and addressing the client's immediate needs. Once the client's pain and other symptoms are managed, the nurse can then work with the client to develop a plan for managing their RA long-term. This may include providing education about the disease, teaching self-care strategies, and encouraging the client to participate in activities that promote physical and emotional well-being.
Choice C rationale:
Surgery may be an option: Surgery may be an option for some clients with RA, but it is not the primary consideration for the nurse. Surgery is typically considered only after other treatment options have failed to control the client's symptoms.
Choice D rationale:
Education is important: Education is an important part of managing RA, but it is not the primary consideration for the nurse. The nurse's focus is on providing comfort and addressing the client's immediate needs. Once the client's pain and other symptoms are managed, the nurse can then provide education about the disease and its management.
A nurse is completing discharge instructions with a client following an acute onset of gout. Which of the following client statements indicates an understanding of the treatment regimen?
Explanation
Choice A rationale:
A high-purine diet is not recommended for clients with gout. Purines are substances found in certain foods, such as red meat, organ meats, seafood, and beer. When the body breaks down purines, it produces uric acid. Uric acid is a waste product that can build up in the blood and cause gout attacks.
Choice B rationale:
Aspirin is not typically recommended for clients with gout. In fact, aspirin can sometimes worsen gout symptoms by increasing uric acid levels in the blood.
Choice C rationale:
Limiting alcohol intake is a key part of the treatment regimen for gout. Alcohol can increase uric acid levels in the blood and trigger gout attacks.
Choice D rationale:
Limiting fluid intake is not recommended for clients with gout. In fact, it is important for clients with gout to stay well- hydrated to help flush uric acid out of the body.
A nurse in a clinic is assessing a client who has AIDS and a significantly decreased CD4 T-cell count. The nurse should recognize that the client is at risk for developing which of the following infectious oral conditions?
Explanation
Choice A rationale:
Candidiasis, also known as thrush, is a fungal infection caused by Candida albicans. It commonly affects the mouth, causing white patches on the tongue, inner cheeks, gums, or tonsils.
Individuals with AIDS often have weakened immune systems due to a decreased CD4 T-cell count. This makes them more susceptible to opportunistic infections like candidiasis.
The fungal infection can spread to the esophagus, causing difficulty swallowing, or even to the bloodstream, leading to more serious complications.
Choice B rationale:
Xerostomia refers to dry mouth. It can be caused by various factors, including medications, salivary gland dysfunction, or radiation therapy. While it can occur in individuals with AIDS, it's not directly linked to a decreased CD4 T-cell count.
Choice C rationale:
Halitosis, or bad breath, can have multiple causes, including poor oral hygiene, gum disease, or digestive issues. It's not specifically associated with AIDS or a decreased CD4 T-cell count.
Choice D rationale:
Gingivitis is inflammation of the gums, often caused by plaque buildup. It's a common condition, but it's not directly linked to AIDS or a decreased CD4 T-cell count.
A nurse is completing discharge teaching to a patient who has seizures and received a vagal nerve stimulator to decrease seizure activity. Which of the following statements should the nurse include in the teaching?
Explanation
Choice A rationale:
Magnet activation: Placing a magnet over the implantable device activates an on-demand feature of the VNS, delivering extra stimulation to the vagus nerve. This can potentially disrupt or shorten a seizure, especially when used at the onset of an aura (a warning sign that a seizure may be imminent).
Patient empowerment: Teaching the patient how to use the magnet provides them with a sense of control and a way to actively manage their seizures. It can reduce anxiety and improve quality of life.
Choice B rationale:
Microwave safety: While there's no definitive evidence that microwaves directly interfere with VNS devices, manufacturers generally recommend avoiding close or prolonged exposure to microwaves as a precaution. Specific guidelines may vary, but they often suggest keeping a distance of at least 15-20 inches from microwaves. The statement in Choice B about 12,000 watts or less is inaccurate and misleading.
Choice C rationale:
CT scans with contrast: There's no contraindication for patients with VNS to undergo CT scans with contrast. The device is designed to withstand common imaging procedures.
Choice D rationale:
Pain management: Burst catheters are typically used for pain management after surgery or during childbirth. They have no direct relevance to VNS therapy or seizure management.
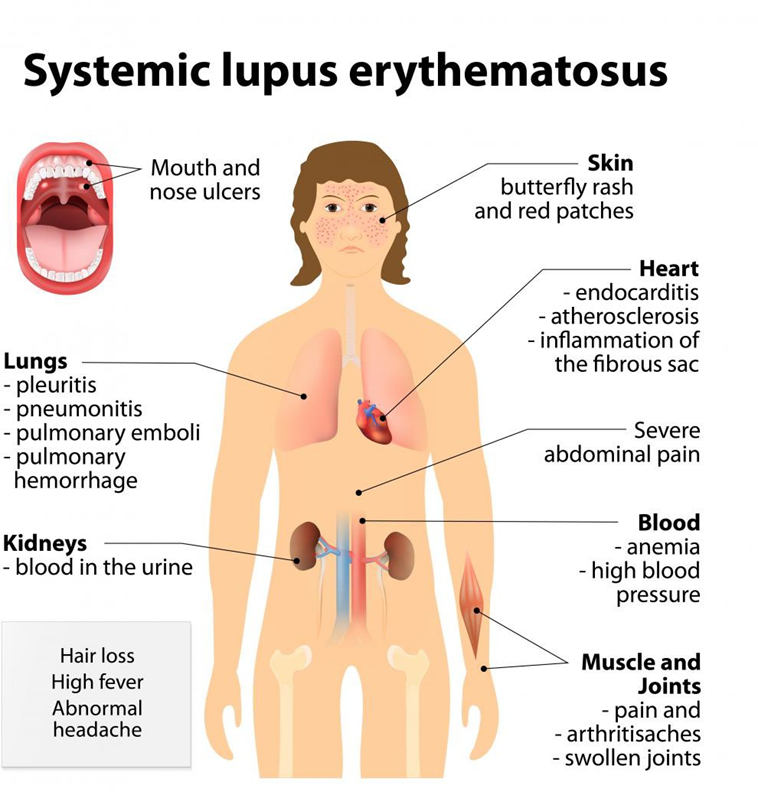
A nurse is teaching a female client who has a new diagnosis of systemic lupus erythematosus (SLE). The nurse should recognize the need for further teaching when the client identifies which of the following as a factor that can exacerbate SLE?
Explanation
Choice A: Exercise: Moderate exercise is actually beneficial for people with SLE by improving cardiovascular health, muscle strength, and flexibility, and reducing fatigue. It can also help to maintain a healthy weight, which is important for managing SLE symptoms.
Choice B: Diet: While maintaining a healthy diet is important for overall health, there is no specific diet that has been proven to help manage SLE symptoms. Certain dietary changes, such as reducing salt intake or avoiding processed foods, may be helpful for some individuals, but these would be individualized based on the client's specific needs and other health conditions.
Choice C: Sunlight: Sunlight exposure can trigger SLE flares in some individuals, but it is not a universal trigger. The nurse should educate the client about sun protection measures, such as wearing sunscreen, protective clothing, and seeking shade during peak sun hours, but this alone would not indicate a need for further teaching.
Infection: Infections are a major trigger for SLE flares. This is because the immune system is already overactive in SLE, and an infection can further exacerbate this activity, leading to inflammation and worsening symptoms. Therefore, the nurse should recognize the client's identification of infection as a trigger as a crucial piece of information and provide further education on recognizing signs and symptoms of infection, practicing good hygiene habits, and promptly seeking medical attention for any suspected infections.
The client tells the nurse, "I am about to have a seizure." Which of the actions should the nurse implement? (Select all that apply)
Explanation
Choice A rationale:
Loosening the patient's clothing around the neck and chest promotes easier breathing during the seizure. It also prevents potential injury from constrictive clothing that could restrict movement or circulation.
Choice B rationale:
Easing the patient to the floor if they are standing helps to prevent falls and injuries that could occur due to loss of consciousness and muscle control during the seizure. It's crucial to guide the patient gently to the floor to avoid abrupt movements that could trigger or worsen the seizure.
Choice C rationale:
Restraining the patient during a seizure is not recommended as it can cause harm. Attempting to restrain a patient's movements during a seizure can lead to muscle strains, joint injuries, or even fractures. It can also increase anxiety and agitation, potentially prolonging the seizure.
Choice D rationale:
Protecting the patient's mouth with a padded tongue blade is not necessary and can even be dangerous. It was once a common practice, but it's now discouraged as it can cause oral injuries, obstruct the airway, or induce vomiting.
Choice E rationale:
Providing privacy helps to protect the patient's dignity and reduce any potential embarrassment during the seizure. It also creates a calmer and less stimulating environment, which can be beneficial in managing the seizure.
What intervention should the nurse identify as a priority for a client with a nursing diagnosis of ineffective airway clearance related to HIV related pneumonia?
Explanation
Choice A rationale:
Coughing and deep breathing are essential for mobilizing and removing secretions from the airways, which is crucial for improving airway clearance in patients with pneumonia. These techniques help to loosen mucus and bring it up from the lungs, allowing it to be expelled through coughing.
Hydration maintenance is also critical because it helps to thin secretions, making them easier to cough up. Adequate hydration helps to keep mucus moist and less sticky, which promotes easier expectoration.
Choice B rationale:
Keeping the head of the bed elevated can help to improve oxygenation and reduce the work of breathing, but it does not directly address the issue of airway clearance. It may be a helpful adjunct intervention, but it's not the priority for this specific nursing diagnosis.
Choice C rationale:
Preparation for insertion of a tracheostomy tube is a more invasive intervention that may be necessary in severe cases of airway obstruction, but it is not the first-line intervention for ineffective airway clearance related to pneumonia. It would be considered if other measures fail to maintain adequate ventilation.
Choice D rationale:
Providing supplemental oxygen can help to improve oxygenation in patients with pneumonia, but it does not directly address the issue of airway clearance. It's important to support oxygenation, but it's not the primary intervention to clear secretions.
A nurse is reviewing laboratory values for a client who has systemic lupus erythematosus (SLE). Which of the following values should give the nurse the best indication of the client's renal function?
Explanation
Choice A rationale:
Serum creatinine is a waste product that is produced by muscle metabolism and is normally excreted by the kidneys.
When kidney function is impaired, creatinine levels in the blood increase, making it a sensitive and specific indicator of renal function.
It is considered one of the most reliable markers for assessing kidney function and is routinely used to screen for and monitor kidney disease.
Choice B rationale:
Serum sodium is an electrolyte that is regulated by the kidneys, but it is not a direct measure of renal function. Sodium levels can be affected by various factors, including fluid intake, medications, and hormonal imbalances.
While abnormal sodium levels can sometimes be a sign of kidney dysfunction, they can also occur due to other conditions, making it less specific as an indicator of renal function.
Choice C rationale:
Blood urea nitrogen (BUN) is another waste product that is produced by the breakdown of proteins and is normally excreted by the kidneys.
However, BUN levels can be influenced by factors other than kidney function, such as dietary protein intake, dehydration, and gastrointestinal bleeding.
This makes BUN less specific than serum creatinine as a marker of renal function.
Choice D rationale:
Urine-specific gravity measures the concentration of solutes in urine, which can provide some information about kidney function.
However, it is not as sensitive or specific as serum creatinine.
Urine-specific gravity can be affected by factors such as fluid intake and hydration status, which can make it less reliable as an indicator of renal function.
The nurse is caring for a group of patients on a medical surgical unit. Which of the following patients is at most risk for developing gout?
Explanation
Anorexia nervosa is a condition characterized by severe weight loss and malnutrition. People with anorexia nervosa are often deficient in nutrients, including purines. Purines are broken down in the body to produce uric acid. When there is an excess of purines in the body, uric acid levels can rise, leading to gout.
Choice B is incorrect. While consuming foods low in purines can help to prevent gout attacks, it is not a risk factor for developing gout.
Choice C is incorrect. Children are not at risk for developing gout. Gout is more common in adults, especially men.
Choice D is incorrect. Ulcerative colitis is an inflammatory bowel disease that is not associated with an increased risk of gout.
A nurse is caring for a client who requests prescription pain medication. Which of the following actions should the nurse perform first?
Explanation
Choice A rationale:
Administering the medication without first assessing the pain could lead to inappropriate medication administration and potentially mask underlying issues. It's crucial to gather more information about the pain before providing any medication.
Choice C rationale:
While repositioning might offer some relief in certain cases, it's not the first step in pain management. A thorough assessment to understand the nature, location, and severity of the pain is essential for determining the most appropriate intervention.
Choice D rationale:
Reviewing the effects of previous pain medication is important, but it doesn't take priority over assessing the current pain. Understanding the current pain experience is necessary to make informed decisions about medication administration and other interventions.
Choice B rationale:
Determining the location of the pain is the crucial first step in pain assessment. It helps to: Identify the potential source of the pain, which can guide treatment choices.
Understand the pain's characteristics, such as its quality, intensity, and duration.
Evaluate for any associated symptoms or patterns, which can provide further insights into the underlying cause. Assess for any aggravating or alleviating factors, which can help tailor treatment strategies.
Monitor the effectiveness of interventions by comparing changes in pain location and characteristics.
A nurse is in a client's room when the client begins having a tonic-clonic seizure. Which of the following actions should the nurse take first?
Explanation
Choice A rationale:
Protecting the airway is the highest priority during a tonic-clonic seizure. Tonic-clonic seizures involve intense muscle contractions, which can lead to biting the tongue, aspiration of secretions, or even respiratory arrest if the airway is obstructed. Turning the client's head to the side helps to maintain a clear airway and prevent these complications.
It is essential to act quickly to prevent injury and ensure adequate oxygenation. Delaying airway management could have serious consequences.
Choice B rationale:
Checking motor strength is not a priority during the active phase of a seizure. It is more important to focus on protecting the airway and preventing injury.
Motor strength can be assessed after the seizure has subsided.
Choice C rationale:
Loosening clothing around the waist may be helpful to promote comfort and breathing, but it is not the first priority. It is more important to address the airway and prevent aspiration.
Choice D rationale:
Documenting the time the seizure began is important for accurate record-keeping and assessment of seizure patterns, but it is not the first priority in the immediate management of the seizure. Documentation can be done after the client's airway and safety are ensured.

A nurse is completing discharge instructions with a client following an acute onset of gout. Which of the following client statements indicates an understanding of the treatment regimen?
Explanation
Choice A rationale:
A high-purine diet is actually contraindicated in gout because purines are metabolized into uric acid, which can accumulate in the joints and trigger gout attacks. Therefore, a low-purine diet is recommended.
Choice B rationale:
Aspirin is not typically recommended for gout because it can interfere with the excretion of uric acid and potentially worsen the condition. While low-dose aspirin might be used for specific cardiovascular benefits in some gout patients, it's not a general treatment for gout itself.
Choice C rationale:Alcohol intake is a common trigger for gout attacks because it can increase uric acid levels in the blood. Therefore, limiting alcohol intake is an important part of managing gout.
Choice D rationale:
Fluid intake should be increased, not limited, in gout patients. This is because adequate hydration helps to flush uric acid out of the body and reduce the risk of gout attacks.
The nurse is planning education for a patient diagnosed with fibromyalgia. Which risk factors should the nurse include in the teaching plan? (Select all that apply)
Explanation
Choice A rationale:
History of rheumatologic conditions: Research has demonstrated a link between fibromyalgia and other rheumatologic conditions, such as rheumatoid arthritis, lupus, and osteoarthritis. Individuals with these conditions may have a predisposition to developing fibromyalgia due to shared genetic factors, immune system dysregulation, and chronic inflammation.
Choice B rationale:
Nutritional deficiency: While nutritional deficiencies, particularly in vitamin D, magnesium, and iron, have been associated with fibromyalgia symptoms, there's not enough evidence to establish them as direct risk factors for its development.
Nutritional deficiencies can worsen pain and fatigue, but they aren't considered primary causes of fibromyalgia.
Choice C rationale:
Previous injury to the bone: Past bone injuries typically aren't considered a risk factor for fibromyalgia. Fibromyalgia is a chronic pain syndrome that affects muscles and soft tissues, not bones themselves. While pain from an injury might trigger fibromyalgia symptoms, it's not a direct cause.
Choice D rationale:
Deep sleep deprivation: Sleep disturbances, especially disruptions in deep sleep (also known as slow-wave sleep), are strongly linked to fibromyalgia. Deep sleep is crucial for restorative processes in the body, including pain regulation. Insufficient deep sleep can lead to heightened pain sensitivity and contribute to the development of fibromyalgia.
Choice E rationale:
Physical and emotional trauma: Physical and emotional trauma, such as experiencing accidents, abuse, or significant psychological stress, can significantly increase the risk of developing fibromyalgia. Trauma can trigger changes in the brain's pain processing pathways and stress hormone regulation, contributing to chronic pain and other fibromyalgia symptoms.
A nurse is caring for a client who is taking naproxen following an exacerbation of rheumatoid arthritis. Which of the following statements by the client requires further discussion by the nurse?
Explanation
Choice A rationale:
Losing 2 pounds in 2 weeks is not a significant weight loss and may not be a cause for concern in this context. It's important to monitor weight trends over time, but this isolated statement doesn't necessarily require immediate discussion.
Choice B rationale:
Engaging in physical activity like swimming is generally beneficial for individuals with rheumatoid arthritis. It can help improve joint mobility, reduce pain, and enhance overall well-being. The nurse might encourage the client to discuss any specific concerns or limitations with their healthcare provider, but the activity itself is not alarming.
Choice C rationale:
Taking an antibiotic concurrently with naproxen can potentially increase the risk of adverse effects. Some antibiotics, like those in the fluoroquinolone class (e.g., ciprofloxacin, levofloxacin), can interact with naproxen and increase the risk of tendonitis or tendon rupture. This interaction warrants further discussion to ensure the client is aware of potential risks and to explore alternative medications if necessary.
Choice D rationale:
Using applesauce to facilitate medication intake is a common and acceptable practice. It does not affect the absorption or efficacy of naproxen.
A nurse is performing discharge teaching for a client who has seizures and a new prescription for phenytoin. Which of the following statements by the client indicates a need for further teaching?
Explanation
Choice A rationale:
Phenytoin is an anticonvulsant medication that is typically used long-term to control seizures. It is not a medication that can be stopped abruptly, as this can lead to the recurrence of seizures or even status epilepticus, a life-threatening condition characterized by continuous seizure activity.
The client's statement, "I'll be glad when I can stop taking this medicine," indicates a lack of understanding about the long- term nature of phenytoin therapy and the potential risks associated with stopping the medication prematurely.
Further teaching is needed to emphasize the importance of medication adherence and the potential consequences of non- adherence.
Choice B rationale:
Phenytoin can cause gingival hyperplasia (overgrowth of gum tissue), so it is important for clients taking this medication to see a dentist regularly for checkups and cleanings.
The client's statement, "I have made an appointment to see my dentist next week," indicates an understanding of this potential side effect and the need for regular dental care.
Choice C rationale:
Phenytoin has a narrow therapeutic index, meaning that there is a small difference between the effective dose and the toxic dose.
Switching brands of phenytoin can lead to changes in blood levels of the medication, which could potentially result in therapeutic failure or toxicity.
The client's statement, "I know that I cannot switch brands of this medication," indicates an understanding of this important safety consideration.
Choice D rationale:
Phenytoin can interact with many other medications, including over-the-counter medications and herbal supplements.
It is important for clients taking phenytoin to notify their doctor before taking any other medications to avoid potential drug interactions.
The client's statement, "I will notify my doctor before taking any other medications," indicates an understanding of this potential risk.
A nurse is calculating the output of a client at the end of the shift.
The nurse notes the following: the client voided 400 mL at 1100 and 350 mL at 1430.
The closed chest drainage system was previously marked at 155 mL and is now at 175 mL. The NG tube has 575 mL in the drainage container, and 25 mL is emptied out of the Jackson-Pratt drainage tube.
How many mL should the nurse record in the medical record as the client's output?
Explanation
Step 1 is to add the amounts of urine:
400 mL + 350 mL = 750 mL
Step 2 is to calculate the amount of drainage from the chest tube:
175 mL - 155 mL = 20 mL
Step 3 is to add up all of the output sources:
750 mL (urine) + 20 mL (chest tube) + 575 mL (NG tube) + 25 mL (Jackson-Pratt) = 1400 mL The nurse should record 1400 mL as the client's output.
A nurse is providing teaching to a client who has a new diagnosis of fibromyalgia. Which of the following client statements indicates an understanding of the teaching?
Explanation
Choice A is incorrect: Caffeine can worsen sleep disturbances, a common symptom of fibromyalgia.
Choice B is incorrect: While duloxetine is a medication used to manage fibromyalgia symptoms, taking it at a specific time for increased energy is not directly related to understanding the disease itself.
Choice C is incorrect: Fibromyalgia is a chronic condition with no cure. Chemotherapy is not indicated for its treatment.
Choice D is correct: Low-impact aerobics like walking, swimming, or yoga are recommended non-pharmacological interventions for fibromyalgia. They can improve cardiovascular health, flexibility, and pain management.
Additional notes:
Other non-pharmacological management strategies for fibromyalgia include stress management techniques, cognitive behavioral therapy, and adequate sleep hygiene.
Early and comprehensive management of fibromyalgia can significantly improve quality of life.
A nurse is teaching a client who has a new prescription for colchicine to treat gout. Which of the following instructions should the nurse include?
Explanation
Choice A rationale:
While taking colchicine with food can help minimize gastrointestinal side effects like nausea, it's not the most crucial instruction for this medication. The primary concern with colchicine is its potential for muscle toxicity.
Choice B rationale:
Colchicine can cause muscle pain, tenderness, or weakness, which can be a sign of a serious condition called rhabdomyolysis. Rhabdomyolysis involves the breakdown of muscle tissue, potentially leading to kidney damage and other complications.
It's crucial for patients to monitor for muscle pain and report it to their healthcare provider promptly if it occurs. Early detection and intervention can help prevent serious complications.
Choice C rationale:
Increased bruising is not a common side effect of colchicine. It's more frequently associated with medications that affect blood clotting, such as warfarin or aspirin.
Choice D rationale:
Grapefruit juice can interact with many medications, including colchicine. It can increase the concentration of colchicine in the bloodstream, potentially leading to toxicity.
It's crucial for patients taking colchicine to avoid grapefruit juice and other grapefruit products.
What intervention should the nurse identify as a priority for a client with a nursing diagnosis of ineffective airway clearance related to HIV-related pneumonia?
Explanation
Choice A rationale:
Coughing and deep breathing: These techniques directly promote airway clearance by mobilizing and expelling secretions from the lungs. They are essential for clients with pneumonia, as the buildup of secretions can obstruct the airways and impair gas exchange.
Hydration maintenance: Adequate hydration helps to thin secretions, making them easier to cough up and clear from the lungs. It also helps to prevent dehydration, which can worsen respiratory symptoms.
Choice B rationale:
Keeping the head of the bed elevated: This can help to improve breathing by decreasing the work of breathing and promoting lung expansion. However, it is not the most effective intervention for directly clearing secretions from the lungs.
Choice C rationale:
Preparation for insertion of a tracheostomy tube: This is a more invasive intervention that may be necessary in severe cases of airway obstruction. However, it is not the priority intervention for a client with ineffective airway clearance related to pneumonia.
Choice D rationale:
Providing supplemental oxygen: This can help to improve oxygenation in clients with pneumonia. However, it does not directly address the problem of ineffective airway clearance.
The nurse is providing discharge instructions to a patient who has a prescription for phenytoin. Which of the following information should the nurse include?
Explanation
Choice A rationale:
Providing a urine sample to determine therapeutic levels of phenytoin is not typically a part of routine discharge instructions. While monitoring of phenytoin levels is important, it's usually done through blood tests, and the frequency of testing is determined by the healthcare provider based on individual patient factors.
Choice C rationale:
Bleeding gums are not a common side effect of phenytoin. While some individuals might experience gum tenderness or overgrowth, significant bleeding is not expected.
Choice D rationale:
Antacids can actually interfere with the absorption of phenytoin, potentially reducing its effectiveness. Therefore, it's generally not recommended to take antacids regularly while on phenytoin therapy. If a patient needs to take an antacid for occasional heartburn or indigestion, it's best to take it at least 2 hours before or after the phenytoin dose.
A client who abused intravenous drugs was diagnosed with the human Immunodeficiency virus (HIV) several years ago.
The nurse explains that the diagnostic criterion for acquired immunodeficiency syndrome (AIDS) has been met when the client:
Explanation
Choice A rationale:
Acute retroviral syndrome (ARS) is an early stage of HIV infection that often presents with flu-like symptoms. It does not determine AIDS diagnosis.
Choice B rationale:
A CD4+ T lymphocyte level of less than 200 cells/mm is a defining criterion for AIDS diagnosis. This low count indicates a severely weakened immune system, leading to susceptibility to opportunistic infections and other AIDS-defining illnesses.
Choice C rationale:
A person with HIV can transmit the virus to others regardless of their CD4+ T cell count. Transmission risk is not a diagnostic criterion for AIDS.
Choice D rationale:
HIV-specific antibodies are produced by the immune system in response to HIV infection but their presence does not signify AIDS progression.
A client has a prescription for seizure precaution. Which intervention should the nurse include in the plan of care?
Explanation
Choice A is incorrect. While keeping the bed in a high position can minimize fall risk, it is not a specific precaution for preventing seizures. In fact, some types of seizures can be triggered by sudden changes in position.
Choice C is incorrect. Bright lights can worsen seizure activity and should be avoided, especially during the night when the client is more likely to be photosensitive.
Choice D is incorrect. Locking the bed in the lowest position can increase fall risk and is not a specific precaution for preventing seizures.
Rationale for Choice B:
Having seizure medication readily available at the bedside allows for immediate administration in case of a seizure, which can minimize its duration and severity. This is a crucial intervention for seizure precaution.
Keeping the medication within easy reach also ensures prompt administration by healthcare personnel or caregivers, further improving the client's safety and outcome.
Additionally, easy access to the medication empowers the client or caregiver to participate actively in their own care and respond quickly to a potential seizure.
Therefore, based on the importance of immediate access to seizure medication in managing and preventing seizures, Choice B is the most appropriate intervention to include in the client's plan of care.
A nurse is caring for a patient with rheumatoid arthritis. The patient is prescribed hydroxychloroquine to slow the progression of the disease. Which of the following laboratory results should the nurse monitor for this patient?
Explanation
Choice A rationale:
Hydroxychloroquine can cause a rare but serious side effect called bone marrow suppression. This is a decrease in the production of blood cells in the bone marrow.
White blood cells (WBCs) are a key component of the immune system, and a decrease in WBCs can make a patient more susceptible to infections.
Therefore, it's crucial for nurses to monitor the patient's WBC count to detect any potential bone marrow suppression early and take necessary actions to prevent or manage infections.
Choice B rationale:
An increased blood cell count is not a typical side effect of hydroxychloroquine.
Some conditions, like polycythemia vera, can cause an increase in blood cell count, but they are not related to hydroxychloroquine use.
Choice C rationale:
While hydroxychloroquine can sometimes cause a decrease in platelet count, it's less common than bone marrow suppression affecting WBCs.
However, it's still essential for nurses to monitor platelet counts as well, as a significantly low platelet count can impair blood clotting and increase the risk of bleeding.
Choice D rationale:
Hydroxychloroquine does not typically affect red blood cell (RBC) counts.
Conditions that affect RBC counts, such as anemia, are not directly related to hydroxychloroquine use.
Sign Up or Login to view all the 40 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

