ATI Medical Surgical integ/burns Exam
Total Questions : 40
Showing 25 questions, Sign in for moreA nurse is teaching a class about expected changes to the skin in older adults. Which of the following information should the nurse include?
Explanation
Choice A rationale: the epidermis becomes thinner and more fragile with age hence making the skin of elderly individuals more prone to injury, bruising, and infections.
Choice B rationale: this is incorrect because the skin in old age loses its elasticity and becomes more wrinkled due to the loss of collagen and elastin fibers responsible for maintaining the elasticity of the skin.
Choice C rationale: subcutaneous tissue comprising mainly of fat and connective tissue increases with age especially in regions such as the abdomen.
Choice D rationale: blood vessels within the skin become narrower and less efficient with increasing age thus resulting in decreased blood flow and oxygen delivery to the skin.
Choice E rationale: sebum production which is responsible for skin lubrication increases with age thus making this statement incorrect.
A nurse is obtaining an aerobic wound culture for a client. Which of the following actions should the nurse take first?
Explanation
Choice A rationale: this is the third step after donning sterile gloves and cleansing the area around the wound to minimize the risk of contamination of the specimen and the introduction of micro-organisms to the wound site.
Choice B rationale: this is the second step after donning sterile gloves to prevent contamination of the site and exposure of the nurse to pathogens from the wound.
Choice C rationale: this is the first action to take since the procedure is aseptic to prevent the contamination of the wound site and also serve as a protective measure preventing the nurse from getting pathogens.
Choice D rationale: this is the final step after obtaining the specimen and labelling it appropriately.
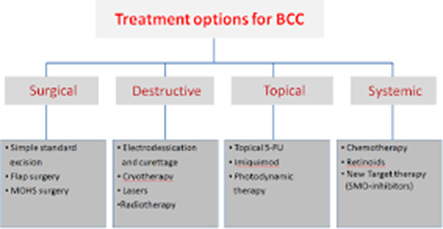
A nurse is caring for a client who has questions concerning the various treatment options for his new diagnosis of basal cell carcinoma. Which of the following treatments should the nurse include in the discussion? (Select all that apply)
Explanation
Choice A rationale: radiation therapy is one of the possible management options for basal cell carcinoma (BCC) that uses high-energy rays to kill the cancerous cells.
Choice B rationale: this is incorrect since topical corticosteroids are ineffective in BCC management and may worsen the patient’s condition by suppressing their immune system.
Choice C rationale: micrographic surgery can be used in BCC management and it involves the removal of thin layers of skin to a point where no cancer cells can be detected.
Choice D rationale: this is appropriate and involves the use of electric current to burn off the cancer cells.
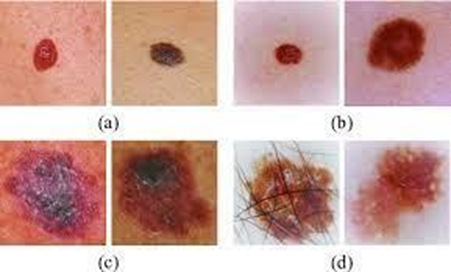
A nurse is caring for a client who has malignant melanoma. Which of the following findings should the nurse expect when assessing?
Explanation
Choice A rationale: pruritus is one of the symptoms of malignant melanoma, as well as changes in the shape, size, color, or texture of a mole or other skin lesion. However, pruritus is not specific to the disease and should always serve as a clue prompting further examination.
Choice B rationale: pain is a very rare symptom in malignant melanoma especially during the early stages of the disease. However, pain may occur in advanced stages of the disease when deeper tissues have been invaded and in cases of metastasis to distant sites.
Choice C rationale: purulent discharge is an indication of an underlying infection rather than malignant melanoma.
Choice D rationale: purplish skin discoloration is common in Kaposi’s sarcoma which manifests as purplish skin nodules rather than malignant melanoma. Furthermore, it may suggest bruising or bleeding under the skin. Malignant melanoma can have various colors, such as black, brown, red, blue, or white, depending on the type and amount of melanin produced by the tumor cells.
A nurse is caring for a male client who has a new diagnosis of genital herpes (HSV 2).
Which of the following findings should the nurse expect?
Explanation
Choice A rationale: white-or flesh-colored papillary growths in the genital region is a common finding in human papillomavirus (HPV) infection, not HSV 2 infection.
Choice B rationale: a patient with HSV 2 usually develop influenza-like symptoms such as headache, muscle aches, fever, and generalized body malaise. However, the above symptoms usually subside within a few days to weeks.
Choice C rationale: anuria refers to the absence of urine output indicating renal failure which is not associated with HSV 2 infection.
Choice D rationale: green penile discharge is associated with gonorrhea infection rather than HSV 2 infection.
A nurse is caring for a client who has burns to his face, ears, and eyelids. The nurse should identify which of the following is the priority report to the provider?
Explanation
Choice A rationale: tachycardia is an expected finding in burns patients due to the increase in metabolic rate and fluid loss.
Choice B rationale: a urine output of 25 ml/hr is too low for an individual with burns hence the need for adequate fluid resuscitation. However, this is not a priority sign compared with the difficulty in breathing.
Choice C rationale: difficulty in swallowing is an indicator of airway edema which may compromise the patients breathing and oxygenation which may result in death. Therefore, the healthcare provider should be notified to assess the need for intubation.
Choice D rationale: Pain of 6 on a scale of 0 to 10 is moderate and is expected due to burns and can be managed with analgesics and nonpharmacological interventions.
A nurse is teaching a class about the epidermis. Which of the following information should the nurse include?
Explanation
Choice A rationale: the epidermis which is the most superficial layer of the skin relies on the dermis for nutrition since it lacks its own blood supply.
Choice B rationale: adipose tissue is contained in the hypodermis which is part of the dermis layer of the skin and not the epidermis.
Choice C rationale: nerve fibers are contained in the dermis layer of the skin and not the epidermis.
Choice D rationale: blood vessels are contained in the dermis layer of the skin and not the epidermis.
A nurse is preparing to administer hydrocortisone 100 mg IM daily to a client. Available is hydrocortisone 250 mg/2 mL. How many ml should the nurse administer per dose? (Round the answer to the nearest tenth number. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
The amount to be administered = desired dose/ dose at hand X quantity of the solution
= 100/250 x 2
= 0.8 mL
A nurse in an emergency room is caring for a client who sustained partial-thickness burns to both lower legs, chest, face, and both forearms Which of the following is the priority action the nurse should take?
Explanation
Choice A rationale: this is important to assess the individual’s blood level and risk of infection but it is not a priority action compared to airway management.
Choice B rationale: The insertion of an indwelling urinary catheter is crucial for urine output monitoring but is not a priority action to take.
Choice C rationale: Inspection of the mouth for signs of inhalation injuries is a priority action for burns patients, especially those who have sustained facial burns since they can result in airway compromise and subsequent respiratory failure. The signs to look out for include; soot in the mouth and mouth, hoarseness, stridor, wheezes, or singed nasal hairs. In cases of suspected inhalation injuries, the nurse should inform the healthcare provider to assess for the need for intubation.
Choice D rationale: administration of analgesics is crucial for pain relief for all burn patients. However, this is not a priority action to take compared to airway management.
A nurse is preparing to start an IV infusion of lactated Ringer's for a client who sustained a burn injury. The client is prescribed 5,200 mL of fl over the first 24 hr. How many mL/hr should the nurse set the pump to infuse for the first 8 hr? Round the answer to the nearest whole nun Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
In burns, half the total fluids required within 24 hours should be given within 8 hours and the other half distributed over the remaining 16 hours to prevent hypovolemic shock and electrolyte imbalance.
Therefore, half the fluid that should be given within 8 hours is 5200/2= 2600
We will use the formula: drip rate= total volume of fluid to be administered/total duration
= 2600/8
=325 mL/hr
A nurse in an emergency department is reviewing the medical record of a client who has an extensive burn injury. Which of the following laboratory results should the nurse expect?
Explanation
Choice A rationale: individuals with extensive burn wounds are highly likely to develop metabolic acidosis and not metabolic alkalosis due to the increased risk of tissue hypoxia, increased lactic acid levels, and renal failure.
Choice B rationale: low hemoglobin is not an expected finding in individuals with extensive burn wounds but instead increased hemoglobin levels are expected due to hemoconcentration resulting from excessive fluid loss.
Choice C rationale: A patient with extensive burn wounds is expected to have hypovolemia and not hypervolemia due to increased fluid loss from the burned tissues and increased capillary permeability.
Choice D rationale: hyperkalemia is a common finding in individuals with extensive burn wounds due to massive cell destruction which releases potassium from the intracellular compartment to the extracellular compartment.
A nurse is planning care for a client who has an infected wound with significant exudate.
The nurse should plan to use which of the following dressings to cover the wound?
Explanation
Choice A rationale: this is a type of non-adherent dressing that can be used for wounds with minimal exudates hence this is not suitable for wounds with significant exudate since it causes maceration and leakage.
Choice B rationale: this is an absorbent dressing that can be used in wounds with moderate-significant exudate since it moistens the wound environment while facilitating autolytic debridement by forming a gel in contact with the exudate.
Choice C rationale: this is a type of hydrating dressing containing water or glycerin-based gel that is suitable for use in wounds with minimal exudate.
Choice D rationale: this is a type of occlusive dressing suitable for wounds with minimal-moderate exudates. It is unsuitable for wounds with significant exudate since it can result in maceration and leakage.
A nurse identifies a pressure ulcer after a client had a long, extensive recovery following a surgical procedure. When completing an incident about a pressure ulcer, the nurse should take which of the following actions?
Explanation
Choice A rationale: The nurse should not include any opinions, judgments, or blame in the incident report, as this could be used as evidence in a legal case. Therefore, the nurse should not question the charge nurse about care deficits.
Choice B rationale: The nurse should not include any opinions, judgments, or blame in the incident report, as this could be used as evidence in a legal case. Therefore, the nurse should not document what the nurse believes was the cause of ulcer development.
Choice C rationale: This is important because it provides factual information about the client's condition and perception of the event, which could help in identifying the factors that contributed to the ulcer development and preventing further complications.
Choice D rationale: Documenting in the client's medical record that the nurse completed an incident report is not the primary purpose of the incident report itself. Incident reports are internal documents used by the healthcare facility to track and investigate events. The documentation in the client's medical record should focus on the client's clinical condition, care provided, and response to treatment.
A nurse is caring for a preschooler who has a partial-thickness burn on her right forearm. Which of the following findings should the nurse expect? (Select all that apply.)
Explanation
Choice A rationale: partial-thickness burns are usually characterized by the formation of blisters as a result of increased capillary permeability resulting in edema formation separating the epidermis from the dermis.
Choice B rationale: wound blanching with pressure is expected in partial-thickness burns due to compromised blood circulation.
Choice C rationale: This is not a typical finding in a partial-thickness burn.
Choice D rationale: this is incorrect since partial-thickness burns involve damage to the epidermis.
Choice E rationale: nerve endings are damaged in partial-thickness burns thus making the area sensitive to touch.
A nurse is caring for an older adult client who is at risk for skin breakdown. Which of the following interventions should the nurse use to help maintain the integrity of the client's skin?
Explanation
Choice A rationale: older adults have thin skin hence massaging bony prominences increases the risk of skin breakdown and pressure ulcers formation.
Choice B rationale: frequent client repositioning every 2-3 hourly is one of the mitigations used to prevent skin breakdown especially in older adults who are bedridden. It aids in the distribution of pressure on bony prominences and also relieves the pressure on the areas at risk and maintains muscle mass and tissue integrity.
Choice C rationale: a high protein diet is important for healthy skin formation. However, in this case frequent repositioning is more crucial for maintaining skin integrity in older adults.
Choice D rationale: cornstarch application can be used to prevent skin damage from friction. However, this is not as important as frequent repositioning.
A nurse is caring for a client who has a stage I pressure ulcer. Which of the following dressings should the nurse plan to apply?
Explanation
Choice A rationale: Transparent dressings are commonly used for stage I pressure ulcers as they provide a protective barrier against external contaminants while allowing for visualization of the wound. This type of dressing helps maintain a moist environment to facilitate healing.
Choice B rationale: Hydrogel dressings are typically used for wounds with necrotic tissue or those that require a moist environment. They may not be the first choice for a stage I pressure ulcer with intact skin.
Choice C rationale: Wet-to-dry dressings are often used for wounds with debris or infection. They involve placing moist gauze into the wound and allowing it to dry, promoting debridement. This is not suitable for an intact stage I pressure ulcer.
Choice D rationale: Alginate dressings are absorbent and are more appropriate for wounds with moderate to heavy exudate. They may not be necessary for a stage I pressure ulcer with minimal or no exudate.
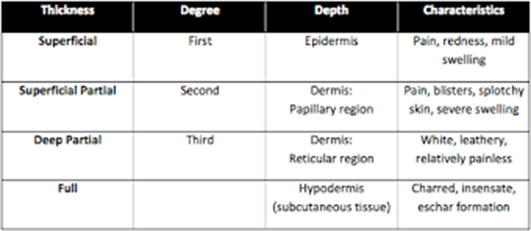
A nurse is assessing a client who is brought to the emergency room with burn injuries.
Which of the following findings should the nurse identify a deep partial-thickness burn?
Explanation
Choice A rationale: This describes a full-thickness burn with eschar formation, not a deep partial-thickness burn.
Choice B rationale: This may indicate a deeper burn involving the subcutaneous tissue, but the absence of blisters makes it less characteristic of a deep partial-thickness burn.
Choice C rationale: This suggests a full-thickness burn with damage to nerve endings, not a deep partial-thickness burn.
Choice D rationale: A deep partial-thickness burn is characterized by a pink or mottled appearance with the presence of blisters. This type of burn involves damage to the epidermis and portions of the dermis, causing pain and sensitivity to touch.
A nurse is providing teaching to a client who has widespread psoriasis and a prescription for phototherapy. The nurse should include the following information in the teaching?
Explanation
Choice A rationale: Phototherapy can sometimes cause sensitivity to light, and wearing dark glasses can help protect the eyes from excessive light exposure.
Choice B rationale: It is not typical to interrupt phototherapy due to redness and tenderness, as some skin reactions may occur during treatment but can be managed without interruption.
Choice C rationale: The schedule of phototherapy can vary, and the choice of days on and off may not necessarily be fixed in a three-day pattern.
Choice D rationale: The frequency and timing of phototherapy sessions depend on the specific treatment plan prescribed by the healthcare provider.
A nurse in a provider's office is assessing a client who has AIDS. The nurse notes that the client has multiple and widespread raised, purplish- brown skin lesions. The nurse should recognize that these findings indicate which of the following conditions
Explanation
Choice A rationale: Actinic keratosis presents as rough, scaly patches on sun-exposed skin and is not associated with the purplish-brown lesions seen in Kaposi's sarcoma.
Choice B rationale: Basal cell carcinoma typically presents as pearly or waxy bumps and is not characterized by widespread purplish-brown lesions.
Choice C rationale: Kaposi's sarcoma is characterized by the development of purplish-brown skin lesions, and it is commonly associated with advanced HIV/AIDS.
Choice D rationale: Toxic epidermal necrolysis is a severe skin reaction but is not typically associated with purplish-brown lesions.

A nurse is caring for a client who has shingles with multiple skin lesions. Which of the following actions by the nurse require intervention nurse's supervisor?
Explanation
Choice A rationale: Wearing gloves is appropriate when providing direct care to a client with shingles to prevent the spread of the virus.
Choice B rationale: Shingles is caused by the varicella-zoster virus, and it is highly contagious. Placing a client with shingles in a double room increases the risk of spreading the virus to other clients, especially those with compromised immune systems.
Choice C rationale: Wearing a gown is appropriate when there is a risk of contact with the client's lesions to prevent the spread of the virus.
Choice D rationale: While wearing a mask may be indicated for certain respiratory conditions, it is not typically required when caring for a client with shingles.
A nurse is caring for a client who has pruritus following treatment for scabies. Which of the following actions should the nurse take?
Explanation
Choice A rationale: Rubbing the affected area may exacerbate pruritus and potentially spread scabies.
Choice B rationale: Providing mittens can prevent the client from scratching the affected areas, promoting healing and preventing the spread of scabies.
Choice C rationale: Hot water can worsen itching and should be avoided in scabies management.
Choice D rationale: The application of scabicide should follow the prescribed treatment plan, and additional application without guidance may lead to overuse and potential adverse effects.
A nurse in a provider's office is caring for a client who has a new diagnosis of tinea pedis, which of the following findings should the nurse expect?
Explanation
Choice A rationale: Circular, erythematous patches on the scalp are more indicative of tinea capitis, a fungal infection affecting the scalp, and not tinea pedis.
Choice B rationale: Tinea pedis, commonly known as athlete's foot, typically presents with symptoms such as scaling, redness, and itching between the toes. It is a fungal infection affecting the feet.
Choice C rationale: Poison ivy exposure would result in contact dermatitis, characterized by a rash and blistering, rather than the typical presentation of tinea pedis.
Choice D rationale: Antiseizure medications are not typically associated with the development of tinea pedis; the symptoms described are more consistent with a fungal infection.

A nurse is admitting a client who sustained severe burn injuries. The nurse refers to the rule of nines to determine the total body surface area of Your injury What percentage of body surface area should the nurse estimate the client has burned?
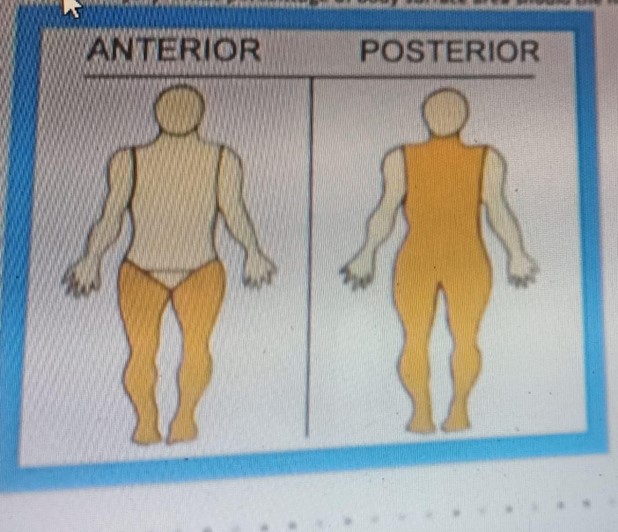
Explanation
Rationale: This is because according to the rule of nines, the lower limbs anteriorly and posteriorly will account for 18% each, and the back accounting for 18%
So, the TBSA will be, (18+18+18) =54%
A nurse is assessing the depth and extent of injury on a client who has severe burns to the face, neck, and upper extremities. Which of the following factors is the nurse's priority when assessing the severity of the client's burns?
Explanation
Choice A rationale: While age can influence the overall prognosis and response to treatment, the location of the burn is more critical in the immediate assessment of severity.
Choice B rationale: The priority when assessing the severity of burns is the location of the burn. Burns to certain areas, such as the face, neck, or major joints, can be more critical due to the potential for complications, including impairment of breathing, vision, or mobility. Burns to these areas may require prompt intervention and closer monitoring to ensure early mitigation of the above complications
Choice C rationale: While understanding the cause is important for prevention and future education, it is not the immediate priority in assessing the severity of the current burn.
Choice D rationale: While medical history may impact the overall treatment plan, it is not the primary factor in the initial assessment of burn severity.
A nurse has just finished a wound irrigation for a client who requires contact precautions. Which of the following pieces of personal protective equipment (PPE) should the nurse remove first?
Explanation
Choice A rationale: When removing personal protective equipment (PPE) after a procedure involving contact precautions, the nurse should remove the items in a specific order to minimize the risk of contamination. Gloves should be removed first because they are the most likely to be contaminated and can transfer microorganisms to other surfaces or PPE during removal.
Choice B rationale: The mask should be removed after gloves and gown. Removing the mask first could potentially contaminate the hands, leading to the risk of transferring microorganisms to the face during mask removal.
Choice C rationale: The gown should be removed after gloves and before the mask. Removing the gown too early could lead to potential contamination of the hands.
Choice D rationale: The face shield should be removed after gloves, mask, and gown. It provides additional protection for the face and should be retained until the end of the removal process to minimize the risk of contamination.
Sign Up or Login to view all the 40 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

