ATI Mental Health Exam
Total Questions : 86
Showing 25 questions, Sign in for moreA nurse in an acute mental health unit is caring for a group of clients. For which of the following clients is seclusion contraindicated?
Explanation
A. An adolescent client who throws objects at other clients:
Explanation: Seclusion is contraindicated for this client due to safety concerns. The behavior of throwing objects at others indicates a potential danger to both the client and others in a confined space. Placing the client in seclusion could escalate the situation and potentially lead to further harm.
B. An older adult client who is manic and crying due to overstimulation:
Explanation: Seclusion might be contraindicated for this client as well. Older adults experiencing manic behavior and emotional distress could be further traumatized by seclusion. Alternatives like providing a calm and soothing environment, along with appropriate medications, might be more beneficial for this client.
C. A school-age client who attempts to repeatedly bite staff:
Explanation: Seclusion is a potential option for this client. The repeated attempts to bite staff pose a risk of physical harm to both the client and staff members. Seclusion might be used as a last resort to ensure the safety of everyone involved.
D. An adult client following a suicide attempt:
Explanation: Seclusion is generally contraindicated for clients who have attempted suicide. Placing them in isolation can worsen feelings of despair and isolation, potentially increasing the risk of self-harm or suicide. These clients require close monitoring, support, and therapeutic interventions to address the underlying issues.
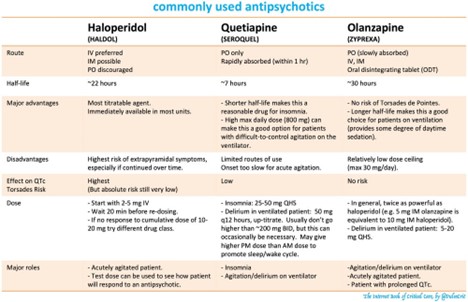
A nurse is caring for a client who has severe manifestations of schizophrenia and is medicated PRN for agitation with haloperidol. The nurse should assess the client for which of the following adverse effects?
Explanation
A. Bleeding:
Explanation: Bleeding is not a common adverse effect of haloperidol, which is an antipsychotic medication used to treat conditions like schizophrenia. Haloperidol primarily works on the central nervous system and is not known to directly cause bleeding issues.
B. Cataracts:
Explanation: Cataracts are not a common adverse effect of haloperidol either. While long-term use of some antipsychotic medications can lead to metabolic and endocrine disturbances, which might indirectly impact eye health, cataracts are not a direct and immediate concern with haloperidol use.
C. Dysrhythmias:
Explanation: Correct Answer. Haloperidol has the potential to cause cardiac-related adverse effects, including dysrhythmias (irregular heart rhythms). This is a particular concern in individuals who are predisposed to heart conditions or have other risk factors. The medication can prolong the QT interval, which is a measure of the time it takes for the heart's electrical system to recharge between beats. Prolonged QT interval can lead to serious and potentially life-threatening arrhythmias.
D. Pancreatitis:
Explanation: Pancreatitis is not a common adverse effect of haloperidol. Pancreatitis typically involves inflammation of the pancreas and can be caused by various factors such as gallstones, alcohol consumption, and certain medications. Haloperidol is not known to directly cause inflammation of the pancreas.
A nurse is preparing to minister amoxicillin 350 mg PO. Available is amoxicillin 250 mg/5 mL. How many mL should the nurse administer? (Round to the nearest whole number.)
Explanation
To calculate the volume (mL) of amoxicillin needed, you can use the following formula:
Volume (mL) = Dose (mg) / Concentration (mg/mL)
Given that the dose is 350 mg and the concentration is 250 mg/5 mL:
Volume (mL) = 350 mg / 250 mg/5 mL
First, calculate the concentration of amoxicillin in mg/mL:
250 mg / 5 mL = 50 mg/mL
Now, use the calculated concentration to find the volume:
Volume (mL) = 350 mg / 50 mg/mL = 7 mL
So, the nurse should administer 7 mL of amoxicillin.
A nurse is providing discharge teaching to a client who has bipolar disorder and will be discharged with a prescription for lithium. The nurse could teach the client which of the following factors puts her at risk for lithium toxicity?
Explanation
A. A client runs 4 miles outdoors every afternoon:
Explanation: Physical activity or exercise, such as running, does not inherently put the client at risk for lithium toxicity. However, excessive sweating due to vigorous exercise can lead to dehydration, which could affect lithium levels. Dehydration may lead to reduced kidney function, which could slow the excretion of lithium, potentially increasing the risk of toxicity.
B. The client eats 2 to 3 gm of sodium-containing foods daily:
Explanation: Correct Answer. High sodium intake can affect the balance of sodium and lithium in the body. When sodium levels are low, the kidneys might reabsorb more lithium, potentially leading to elevated lithium levels and toxicity. It's important to note that consistent sodium intake is crucial, as sudden increases or decreases can impact lithium levels.
C. The client drinks 2 liters of liquids daily:
Explanation: Adequate fluid intake is generally important, but it is not a direct risk factor for lithium toxicity. In fact, staying hydrated can be beneficial for overall health and proper kidney function, which plays a role in lithium excretion.
D. The client eats foods high in tyramine:
Explanation: Foods high in tyramine are a concern when taking certain classes of antidepressants called monoamine oxidase inhibitors (MAOIs). Lithium does not interact with tyramine-containing foods in the same way. Tyramine-rich foods are associated with a "cheese effect" when combined with MAOIs, but this is not relevant to lithium toxicity.
A nurse is making a home visit to a client who has Alzheimer's disease and the client's partner. Which of the following observations indicates to the nurse that the partner is experiencing caregiver role strain?
Explanation
A. The partner has placed locks at the top of the doors leading to the outside:
Explanation: Placing locks at the top of doors leading outside is a safety measure to prevent the person with Alzheimer's disease from wandering or getting lost. While this does show that the partner is taking proactive steps to ensure the client's safety, it is not necessarily indicative of caregiver role strain.
B. The partner has hired a house cleaner:
Explanation: Hiring a house cleaner can be a sign of caregiver role strain. Caregivers often become overwhelmed with the responsibilities of caring for a person with Alzheimer's disease, and hiring help for household tasks can be an indication that they are finding it challenging to manage everything on their own.
C. The partner has lost 20 lb in the past 2 months:
Explanation: Rapid weight loss can be a sign of caregiver stress or burnout. The emotional and physical demands of caring for a loved one with Alzheimer's disease can lead to neglect of one's own well-being, including proper nutrition and self-care.
D. The partner redirects the client when the client is frustrated:
Explanation: While redirecting the client when they're frustrated shows that the partner is using appropriate strategies to manage challenging behaviors associated with Alzheimer's disease, this observation doesn't necessarily indicate caregiver role strain.
A nurse is preparing to administer haloperidol 75 mg IM per week. Available is haloperidol decanoate 100mg/ml for injection. How many ml should the nurse administer per dose? (Round the answer to the nearest hundredth. Use a leading zero if it applies.
Explanation
To calculate the volume (ml) of haloperidol decanoate needed for a dose of 75 mg, you can use the following formula:
Volume (ml) = Dose (mg) / Concentration (mg/ml)
Given:
Dose = 75 mg
Concentration = 100 mg/ml
Plugging in the values:
Volume (ml) = 75 mg / 100 mg/ml
Volume (ml) = 0.75 ml
Rounding to the nearest hundredth:
Volume (ml) = 0.75 ml
So, the nurse should administer 0.75 ml of haloperidol decanoate for the dose of 75 mg.

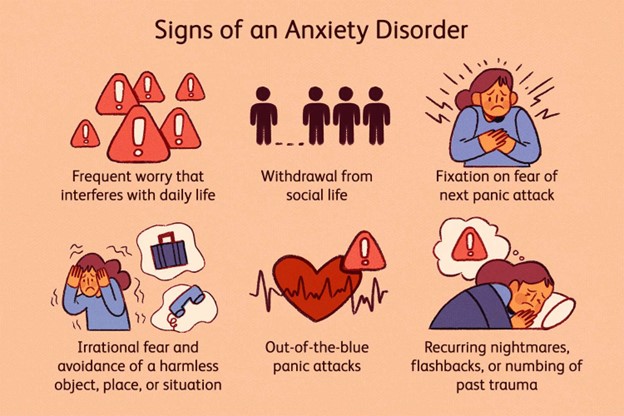
A nurse is caring for a young adult client who says he is experiencing increased anxiety and an inability to concentrate. Which of the following responses should the nurse make?
Explanation
A. "How long has this been going on?":
Explanation: Correct Answer. This response is appropriate because it seeks to gather more information about the duration of the client's symptoms. Understanding the timeline can help the nurse assess the severity and potential causes of the anxiety and concentration issues.
B. "Why do you think you are so anxious?":
Explanation: While it's important to understand the client's perspective, this response might come across as confrontational or judgmental. It's better to create an open and non-judgmental environment for the client to share their feelings.
C. "Have you talked to your parents about this yet?":
Explanation: This response assumes that the client has parents to talk to and may not be relevant for all clients. It's also important to establish trust and rapport with the client before asking about their support network.
D. "It sounds like you're having a difficult time.":
Explanation: This response validates the client's feelings and provides empathy. While it's empathetic, it might not prompt further discussion to gather more information about the situation, which is important for a comprehensive assessment.
A nurse is admitting a client who has multiple injuries following a motor vehicle crash. Shortly after admission, the client's partner arrives. He is distraught and blames himself for the accident. Which of the following responses should the nurse make?
Explanation
A. "I think you should calm down a little before you see your partner.":
Explanation: This response might come across as dismissive or insensitive to the partner's feelings. It's important to acknowledge the partner's emotions and offer support rather than suggesting they should calm down.
B. "Do not worry about that. Your wife will be fine.":
Explanation: While it's reassuring to say that the patient will be fine, dismissing the partner's feelings and concerns is not supportive. The partner needs a chance to express their emotions and concerns.
C. "Tell me more about your feelings about what happened to your partner.":
Explanation: Correct Answer. This response is empathetic and encourages the partner to express their emotions. It shows that the nurse is actively listening and is willing to provide a safe space for the partner to share their feelings.
D. "Why do you think the crash is your fault?":
Explanation: This response might come across as accusatory or confrontational, which could exacerbate the partner's feelings of guilt. Instead, the nurse should focus on providing support and understanding.
A nurse is teaching a client who has a new prescription for chlorpromazine. Which of the following client statements indicates an understanding of the teaching?
Explanation
A. "I may have a dry mouth while taking this medication.":
Explanation: Correct Answer. Dry mouth is a common side effect of chlorpromazine, which is a typical antipsychotic medication. This statement indicates that the client understands the potential side effects of the medication.
B. "This medication will help me stop smoking.":
Explanation: This statement is incorrect. Chlorpromazine is not used as a medication to aid in smoking cessation. It is primarily used to treat conditions such as schizophrenia and other psychotic disorders.
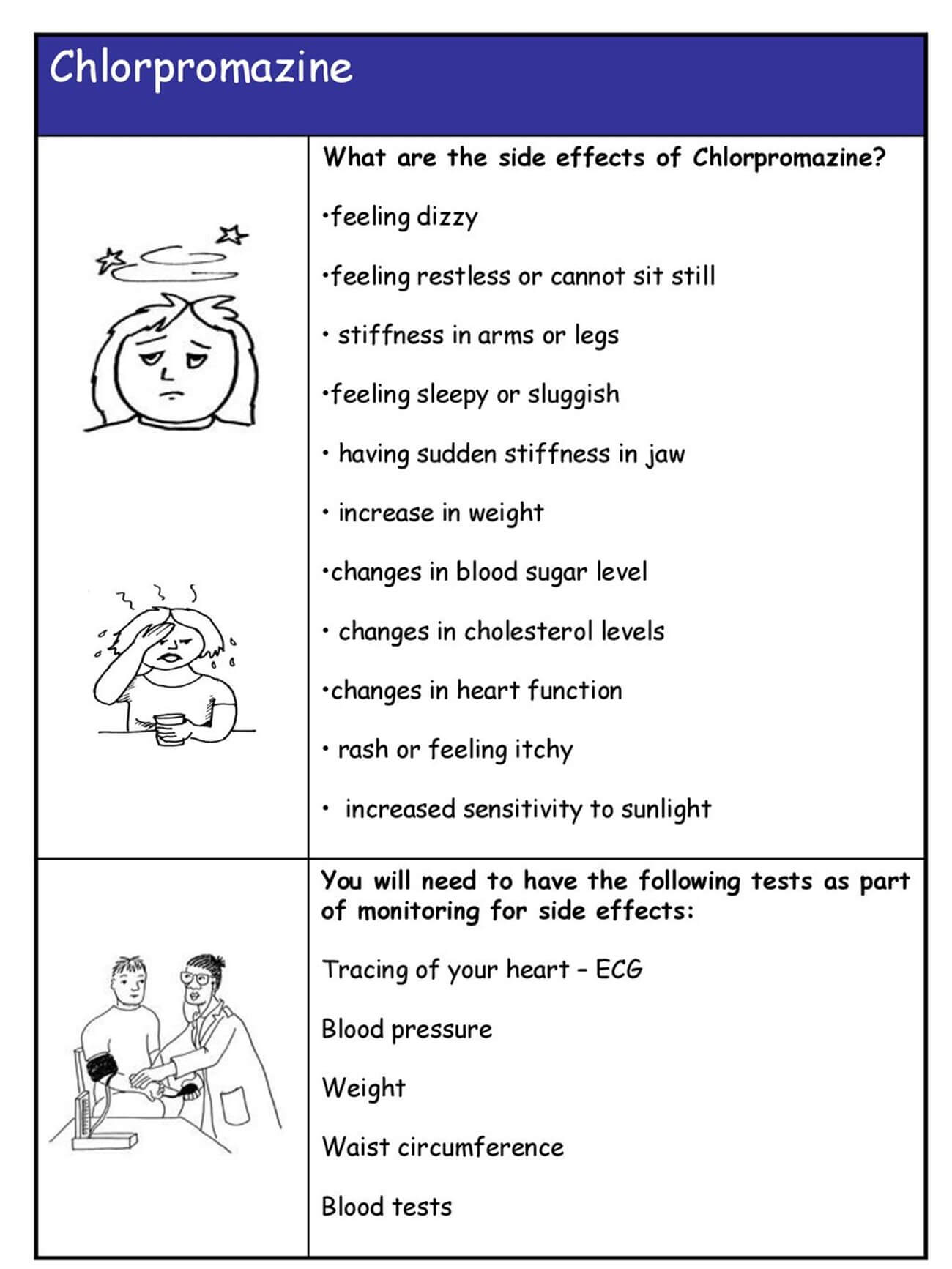
C. "I should expect flu-like symptoms while taking this medication.":
Explanation: This statement is incorrect. Flu-like symptoms are not a common side effect of chlorpromazine. Side effects more commonly associated with chlorpromazine include drowsiness, dizziness, and movement-related issues.
D. "This medication may cause me to urinate frequently.":
Explanation: This statement is incorrect. While chlorpromazine can cause various side effects, increased frequency of urination is not one of the typical side effects associated with this medication.
A nurse is caring for a client who is having difficulty sleeping and is pacing the floor. The client's head down, and he is wringing his hands. Which of the following actions should the nurse take?
Explanation
Remaining with the client provides support and ensures their safety. The client's behavior indicates distress, and having a nurse nearby can help the client feel more comfortable and secure.
B. Give the client a PRN sleeping medication:
Explanation: Administering a sleeping medication should not be the first response, especially if the client is agitated. It's important to address the underlying cause of the agitation and consider other interventions before resorting to medication.
C. Encourage the client to go back to bed:
Explanation: Encouraging the client to go back to bed might not be effective if they are experiencing significant distress or anxiety. It's better to address their emotional state first before suggesting any changes in activity.
D. Explore alternatives to pacing the floor with the client:
Explanation: This is a reasonable course of action. Exploring alternatives to the client's current behavior can help address their distress and find ways to manage their emotions more effectively.
A nurse is caring for a client who is having difficulty sleeping and is pacing the floor. The client's head down, and he is wringing his hands. Which of the following actions should the nurse take?
Explanation
Remaining with the client provides support and ensures their safety. The client's behavior indicates distress, and having a nurse nearby can help the client feel more comfortable and secure.
B. Give the client a PRN sleeping medication:
Explanation: Administering a sleeping medication should not be the first response, especially if the client is agitated. It's important to address the underlying cause of the agitation and consider other interventions before resorting to medication.
C. Encourage the client to go back to bed:
Explanation: Encouraging the client to go back to bed might not be effective if they are experiencing significant distress or anxiety. It's better to address their emotional state first before suggesting any changes in activity.
D. Explore alternatives to pacing the floor with the client:
Explanation: This is a reasonable course of action. Exploring alternatives to the client's current behavior can help address their distress and find ways to manage their emotions more effectively.
A nurse is caring for a client who has major depressive disorder and attempted suicide. The client tells the nurse, "I should have died because I am totally worthless." Which of the following responses should the nurse make?
Explanation
This response reflects active listening and acknowledges the client's emotions. It's a reflective statement that shows empathy without making judgments.
B. "You have a great deal to live for."
Explanation: While this response attempts to be positive and uplifting, it might not fully validate the client's feelings of worthlessness. It's important to acknowledge the client's emotions before trying to provide a more positive perspective.
C. "It's not unusual for depressed people to feel that way."
Explanation: This response normalizes the client's feelings, letting them know that their experience is understood and not uncommon. However, it might come across as somewhat dismissive if not followed by further validation and support.
D. "Why do you feel you are worthless?"
Explanation: Correct Answer. This response seeks to understand the client's feelings in a non-judgmental and open manner. It encourages the client to express their emotions and can help facilitate a therapeutic conversation.
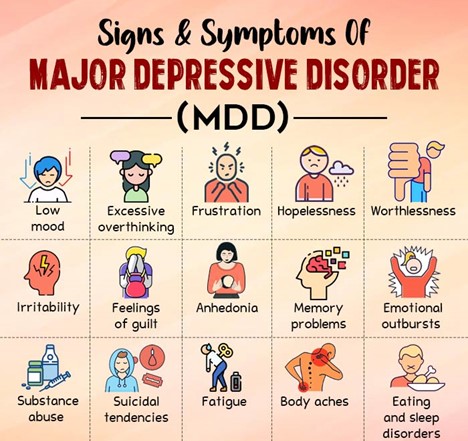
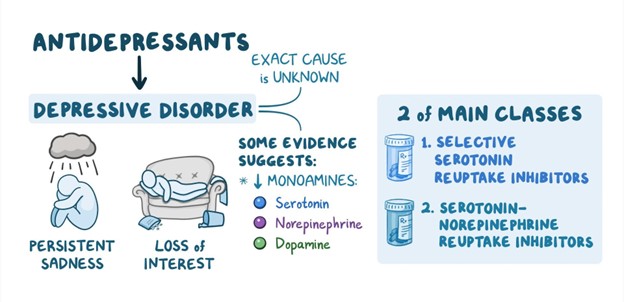
A nurse is caring for a client who has major depressive disorder and was prescribed citalopram 2 weeks ago with a planned dosage increase 1 week ago. The client reports having an improved appetite, but still feels very depressed and is still having trouble sleeping. Which of the following actions should the nurse take?
Explanation
This action might be premature. MAOIs (Monoamine Oxidase Inhibitors) are a class of antidepressants with specific dietary and medication interactions. They are typically considered when other classes of antidepressants have not been effective. It's important to exhaust other options before considering a switch to MAOIs.
B. Explain that antidepressants often take several weeks to be fully effective:
Explanation: Correct Answer. This is an appropriate response. Antidepressants, including citalopram, can take several weeks to show their full therapeutic effects. It's common for some symptoms to improve before others. Educating the client about the delayed onset of action is important to manage their expectations.
C. Tell the client that the provider will need to change citalopram to a different medication:
Explanation: It might be too early to consider changing the medication after just two weeks, especially since the client reports an improved appetite. Changes in dosage or medication should ideally be discussed with the provider after an adequate trial period.
D. Recommend a sleep study be done on the client:
Explanation: While sleep problems can be associated with depression, it might not be the most appropriate next step based solely on the information provided. It's more important to address the ongoing depressive symptoms before focusing solely on sleep.
A nurse is teaching a newly licensed nurse about appropriate actions to take when a client threatens to harm a specific individual. Which of the following statements by the newly licensed nurse indicates understanding?
Explanation
A. "I need to make sure that the potential victim is warned."
Explanation: Correct Answer. When a client threatens to harm a specific individual, it's important to take steps to ensure the safety of both the client and the potential victim. Warning the potential victim or taking appropriate measures to protect them is an important action to take.
B. "I need to keep the information confidential due to the client's right to privacy."
Explanation: While respecting a client's right to privacy is important, when there's a threat of harm to an individual, it becomes a matter of safety that takes precedence over confidentiality.
C. "I can only discuss the client's threats with a court order."
Explanation: This statement is incorrect. When there's a credible threat to harm an individual, waiting for a court order is not an appropriate or timely response. Immediate actions should be taken to ensure safety.
D. "I should verbally report this information to the psychiatrist."
Explanation: While involving the psychiatrist is important for the client's overall care, it's essential to take more immediate steps to ensure the safety of the potential victim, such as notifying the appropriate authorities or taking appropriate precautions.
A client becomes very dejected and states, "No one really cares what happens to me. Life isn't worth living anymore." Which of the following responses should the nurse make?
Explanation
A. "Tell me who you think doesn't care about you."
Explanation: This response might come across as confrontational or defensive, which could discourage the client from opening up further. It's important to offer support and understanding rather than putting the client on the spot.
B. "Of course people care. Your family comes to visit every day."
Explanation: While it's true that the client's family visits, depression often distorts perception and emotions. Telling the client that people care might not be fully effective in addressing their feelings of worthlessness.
C. "Why do you feel that way?"
Explanation: This response opens the door for the client to express their emotions and thoughts. It encourages further conversation and helps the nurse understand the underlying causes of the client's feelings.
D. "I care about you, and I am concerned that you feel so sad."
Explanation: Correct Answer. This response shows empathy and genuine concern for the client's well-being. It acknowledges the client's emotions, offers support, and validates their feelings.
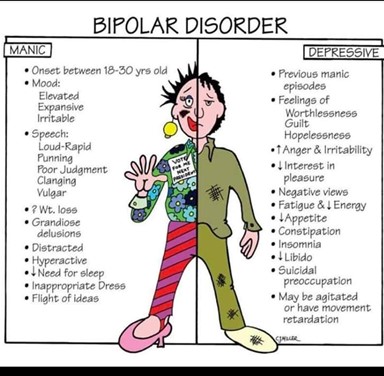
An acute mental health whit is admitting a client who has bipolar disorder. Which of the following findings supports the admitting diagnosis of acute mania?
Explanation
A. The client responds to questions with disorganized speech:
Explanation: Disorganized speech is a symptom often associated with various mental health conditions, including schizophrenia, but it is not specific to acute mania. It might indicate cognitive impairment or thought disorder, but it's not a hallmark of acute mania.
B. The client reports that voices are telling him to write a novel:
Explanation: Correct Answer. This finding supports the diagnosis of acute mania. Hearing voices (auditory hallucinations) that instruct or command the person to do something is a symptom commonly associated with manic episodes. This symptom can be indicative of the elevated mood and altered perception often seen in mania.
C. The client's spouse reports that the client has recently gained weight:
Explanation: Weight gain is not a typical hallmark of acute mania. In fact, during manic episodes, individuals might experience decreased appetite and sleep, leading to potential weight loss.
D. The client is dressed in all black:
Explanation: Dressing in all black is not a specific sign of acute mania. While changes in clothing choices or appearance can sometimes be associated with mood changes, this finding alone is not indicative of acute mania.
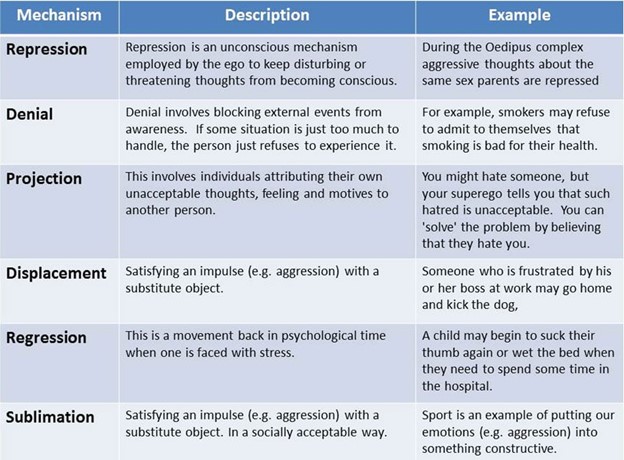
A nurse at a college campus mental health counseling center is caring for a student who just failed an examination. The student spends the session berating the teacher and the course. The nurse should recognize this behavior as which of the following defense mechanisms?
Explanation
A. Regression: Incorrect
Regression is a defense mechanism in which a person reverts to an earlier stage of development in response to stress or anxiety. For example, an adult might start behaving like a child when faced with a difficult situation. In this case, the student berating the teacher doesn't demonstrate a return to an earlier developmental stage, so regression is not the correct choice.
B. Conversion: Incorrect
Conversion refers to the conversion of emotional distress into physical symptoms, such as experiencing physical pain without any apparent physical cause. This mechanism is often seen in conditions like conversion disorder. The student berating the teacher is not exhibiting physical symptoms as a response to emotional distress, so conversion is not the correct choice.
C. Projection: Correct
Projection is the act of attributing one's own unacceptable feelings or thoughts to another person. In this scenario, the student is projecting their own failure onto the teacher and the course by blaming them for the failure. They are unable to accept their own role in the failure and are instead placing the blame on external factors. This aligns with the behavior described in the scenario.
D. Undoing: Incorrect
Undoing involves trying to compensate for or negate an unacceptable action or thought with a contrary action. For instance, someone who had angry thoughts might engage in excessive acts of kindness to "undo" those thoughts. The student berating the teacher is not engaging in actions to negate their negative feelings or thoughts; they are expressing their frustration directly.
A client who has major depressive disorder states to the nurse that he and his family would be better off if he were gone. Which of the following is the nurse's priority response?
Explanation
A. "Are you thinking of harming yourself?": Correct
This is the priority response because it directly addresses the client's statement about being better off gone, which raises concerns about potential suicidal thoughts. Asking this question allows the nurse to assess the client's risk of self-harm or suicide and take appropriate actions to ensure their safety.
B. "Do you really think your family would be better off without you?": Incorrect
While this response attempts to engage the client in a conversation, it doesn't directly address the immediate concern of suicidal thoughts. It's important to prioritize assessing the client's safety before exploring their feelings about their family's perspective.
C. "When did you first start feeling this way?": Incorrect
While understanding the client's history and the onset of their feelings is important, it's not the priority response in this situation. Assessing the client's risk of harm takes precedence over gathering historical information.
D. "Tell me what is happening right now.": Incorrect
This response doesn't directly address the client's statement about being better off gone and doesn't assess the immediate risk of self-harm or suicide. While understanding the client's current situation is valuable, safety concerns should be addressed first.
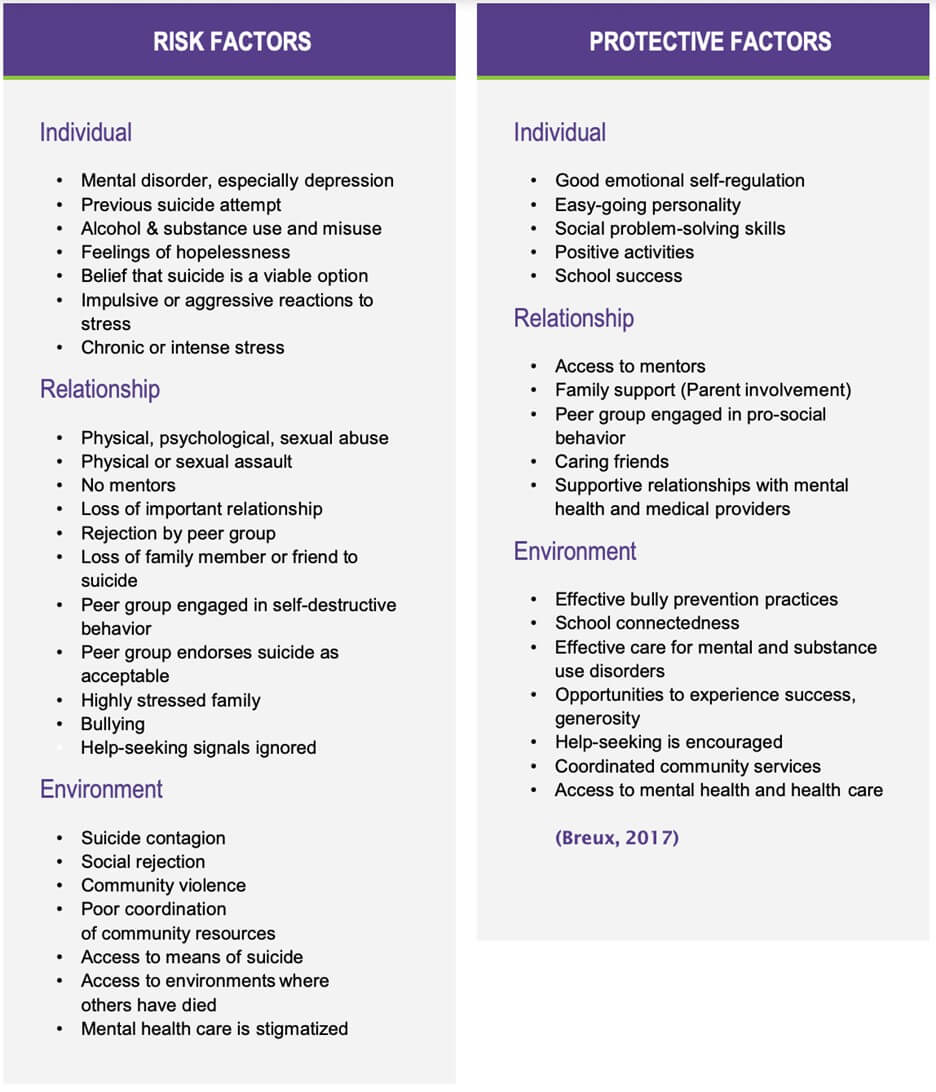
A nurse is providing a community health education class about suicide prevention. Which of the following should the nurse identify as risk factors for suicide? (Select all that apply).
Explanation
A. Female gender: Incorrect
While the risk of attempted suicide is generally higher in females, completed suicide rates are higher in males. Therefore, being female is not typically considered a primary risk factor for suicide.
B. Currently married: Incorrect
Being currently married is not typically considered a primary risk factor for suicide. In some cases, marital or relationship issues might contribute to suicide risk, but it's not a universally applicable risk factor.
C. Age greater than 45 years old: Incorrect
While suicide rates do tend to increase with age, particularly in individuals over 65, age greater than 45 is not a strict cutoff for suicide risk. People of all ages can be at risk, and age alone is not a definitive risk factor.
D. Substance use disorder: Correct
Substance use disorder is a significant risk factor for suicide. Substance abuse can contribute to feelings of hopelessness and despair, impair judgment, and lower inhibitions, increasing the likelihood of suicidal behavior.
E. Schizophrenia: Correct
Schizophrenia is a mental disorder associated with an increased risk of suicide. The symptoms of schizophrenia, such as hallucinations, delusions, and feelings of isolation, can contribute to severe distress and increase the risk of suicidal ideation and behaviors.
A nurse is caring for a client who is prescribed tetracycline 2 grams daily PO in four divided doses every 6 hr. Available is tetracycline 250 mg capsules. How many capsules should the nurse administer per dose? (Round the answer to the nearest tenth. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
To calculate the number of capsules that the nurse should administer per dose, the nurse should first divide the total daily dose of tetracycline by the number of doses per day. This gives the dose per administration:
2 grams / 4 doses = 0.5 grams per dose
Next, the nurse should convert the dose from grams to milligrams, since the available capsules are in milligrams. There are 1000 milligrams in one gram, so the nurse should multiply the dose by 1000:
0.5 grams x 1000 mg/g = 500 mg per dose
Finally, the nurse should divide the dose in milligrams by the strength of each capsule, which is 250 mg. This gives the number of capsules that the nurse should administer per dose:
500 mg / 250 mg/capsule = 2 capsules per dose
Therefore, the nurse should administer 2 capsules of tetracycline every 6 hours to the client.

A nurse is caring for a client who has schizophrenia and is experiencing a variety of hallucinations. Which of the following hallucinations is the priority for the nurse to address?
Explanation
A. Tactile hallucination: Incorrect
Tactile hallucinations involve false sensations of touch, such as feeling something on the skin that isn't there. While these hallucinations can be distressing, they are not typically considered a priority over other types of hallucinations, especially those that might pose more immediate risks.
B. Command hallucination: Correct
Command hallucinations involve hearing voices that command the individual to take specific actions, often harmful ones. These types of hallucinations are considered a significant priority because they can lead to dangerous behaviors, self-harm, or harm to others. Addressing and managing command hallucinations promptly is crucial to ensure the safety of the individual and those around them.
C. Visual hallucination: Incorrect
Visual hallucinations involve seeing things that aren't actually present. While these can be distressing, they are generally considered less urgent compared to command hallucinations, which can directly lead to risky actions.
D. Gustatory hallucination: Incorrect
Gustatory hallucinations involve false perceptions of taste. While these can be unsettling, they are not typically considered a priority over command hallucinations, which have a more immediate potential for harm.
A nurse in an emergency department is caring for an adolescent client who reports being sexually assaulted just prior to admission. Which of the following actions should the nurse take?
Explanation
A. Discuss self-defense techniques with the client: Incorrect
While self-defense techniques can be useful information, discussing them immediately after a traumatic event like sexual assault may not be appropriate. The client's immediate needs for emotional support, medical evaluation, and safety are more pressing.
B. Give the client a bed bath prior to physical examination: Incorrect
In cases of sexual assault, preserving evidence is important for legal purposes and for the client's well-being. Providing a bed bath could potentially compromise evidence and hinder a thorough examination by healthcare professionals.
C. Inform the client photographs of injuries are required for a police report: Correct
Preserving evidence is crucial in cases of sexual assault, especially if the client intends to involve law enforcement. Informing the client about the importance of photographs for a police report is appropriate and can contribute to a potential legal investigation.
D. Ask the client to describe the situation: Correct
It's important to encourage the client to share their experience, but it should be done in a sensitive and supportive manner. Gathering information about the situation can help the healthcare team understand the scope of the assault, provide appropriate medical care, and offer necessary emotional support.
A nurse on a long-term care unit is creating a plan of care for a client who has Alzheimer's disease. Which of the following interventions should the nurse include in the plan?
Explanation
A. Providing an activity schedule that changes from day to day might be overwhelming and confusing for a client with Alzheimer's disease, as routine and predictability are often more beneficial.
B. Constantly rotating caregivers can lead to increased confusion for the client, as familiarity and consistency are important in their care.
C. Limiting time for the client to perform activities can add unnecessary stress and may not be conducive to a comfortable and supportive environment for someone with Alzheimer's disease.
D. Talk the client through tasks one step at a time.
For a client with Alzheimer's disease, providing clear and simple instructions is crucial. Breaking tasks down into manageable steps helps the client follow and complete activities more effectively. This approach reduces confusion and frustration and promotes the client's ability to engage in activities of daily living.
A nurse is preparing to administer benztropine 2 mg IM every 12 hr to a client who is experiencing an extrapyramidal reaction. Available is benztropine 1 mg/mL for injection. How many ml should the nurse administer per dose? (Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
The nurse is preparing to administer benztropine 2 mg IM every 12 hours. The concentration of the available benztropine is 1 mg/mL.
To calculate the volume (mL) of the medication needed for the prescribed dose, you can use the formula:
Volume (mL) = Dose (mg) / Concentration (mg/mL)
Plugging in the values:
Volume (mL) = 2 mg / 1 mg/mL = 2 mL
So, the nurse should administer 2 mL of benztropine 1 mg/mL for each dose. Since we're looking for a whole number, we round to the nearest whole number, which is 2 mL.

A nurse is providing discharge teaching to a client who is taking risperidone. Which of the following instructions should the nurse include in the teaching?
Explanation
A. "This medication may increase your blood pressure."
This statement is incorrect. Risperidone is not typically associated with significant increases in blood pressure. One of the potential side effects of risperidone is orthostatic hypotension, which is a drop in blood pressure when changing positions (e.g., standing up quickly). Therefore, this choice is not the best instruction to include in the teaching.
B. "Flu-like symptoms are an expected adverse effect of this medication."
This statement is incorrect. While risperidone can have side effects, flu-like symptoms are not commonly associated with it. Common side effects of risperidone may include dizziness, drowsiness, weight gain, and movement disorders. Flu-like symptoms are not a typical adverse effect of this medication.
C. "Avoid becoming overheated while taking this medication."
This statement is correct. Risperidone, like many other antipsychotic medications, can interfere with the body's ability to regulate temperature. This can lead to an increased risk of overheating, especially in hot weather or during vigorous physical activity. Therefore, it's important for patients taking risperidone to be cautious and avoid becoming overheated, as this could potentially lead to heat-related complications.
D. "Muscle twitches can occur the first few weeks while taking this medication."
This statement is incorrect. Muscle twitches are not a common side effect of risperidone. While it's true that some movement disorders can occur with antipsychotic medications, the statement is too specific to muscle twitches and does not accurately reflect the typical side effect profile of risperidone.
Sign Up or Login to view all the 86 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

