ATI Monroe college NY PN 23NS SP 126 exam 3
Total Questions : 25
Showing 25 questions, Sign in for moreA nurse is reviewing the medical record of a client who has hyperthyroidism (Graves disease). Which of the following serum laboratory findings should the nurse expect to be below the expected reference range?
Explanation
Choice A: Thyroxine (T4) level. This is incorrect because T4 is one of the thyroid hormones that is increased in hyperthyroidism. T4 is produced by the thyroid gland and converted to T3 in the tissues. A high level of T4 indicates overactivity of the thyroid gland.1
Choice B: Triiodothyronine (T3) level. This is incorrect because T3 is another thyroid hormone that is increased in hyperthyroidism. T3 is the more active form of thyroid hormone and regulates the metabolism of cells. A high level of T3 indicates overactivity of the thyroid gland.1
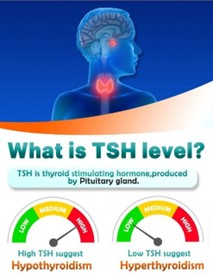
Choice C: Thyroid stimulating hormone (TSH) level. This is correct because TSH is a hormone that stimulates the thyroid gland to produce T4 and T3. TSH is produced by the pituitary gland and regulated by a feedback mechanism. When the levels of T4 and T3 are high, the pituitary gland reduces the secretion of TSH to inhibit further production of thyroid hormones. Therefore, a low level of TSH indicates hyperthyroidism.1
Choice D: Glucose level. This is incorrect because glucose level is not directly related to thyroid function. However, hyperthyroidism can affect glucose metabolism and cause increased blood sugar levels due to increased breakdown of glycogen and glucose uptake by cells. Therefore, glucose level may be elevated in some cases of hyperthyroidism, but it is not a specific indicator.
A nurse is reinforcing teaching with a client who has diabetes mellitus about the manifestations of hypoglycemia.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A: “I will feel shaky.” This is a correct statement, as shakiness is a common manifestation of hypoglycemia, which is a low blood glucose level. Hypoglycemia can cause the sympathetic nervous system to release adrenaline, which can cause tremors, nervousness, and anxiety.
Choice B: “My skin will be warm and moist.” This is an incorrect statement, as warm and moist skin is not a typical manifestation of hypoglycemia. Warm and moist skin can be a sign of hyperglycemia, which is a high blood glucose level. Hyperglycemia can cause dehydration, which can lead to sweating and flushing.
Choice C: “I will be more thirsty than usual.” This is an incorrect statement, as thirst is not a typical manifestation of hypoglycemia. Thirst can be a sign of hyperglycemia, which can cause dehydration, as the body tries to flush out excess glucose through urine.
Choice D: “My appetite will be decreased.” This is an incorrect statement, as decreased appetite is not a typical manifestation of hypoglycemia. Decreased appetite can be a sign of other conditions, such as nausea, infection, or depression. Hypoglycemia can cause increased hunger, as the body needs more glucose to function properly.

A nurse is collecting data from a client who has hypoparathyroidism. Which of the following findings should the nurse expect?
Explanation
Choice A: Negative Chvostek’s sign is the absence of facial twitching when the facial nerve is tapped. This is a normal finding and does not indicate hypoparathyroidism. A positive Chvostek’s sign is a sign of hypocalcemia, which can occur in hypoparathyroidism.
Choice B: Flaccid muscles are weak and limp muscles that lack tone and resistance. This is not a typical finding of hypoparathyroidism, as low levels of parathyroid hormone can cause muscle spasms, cramps, and tetany.
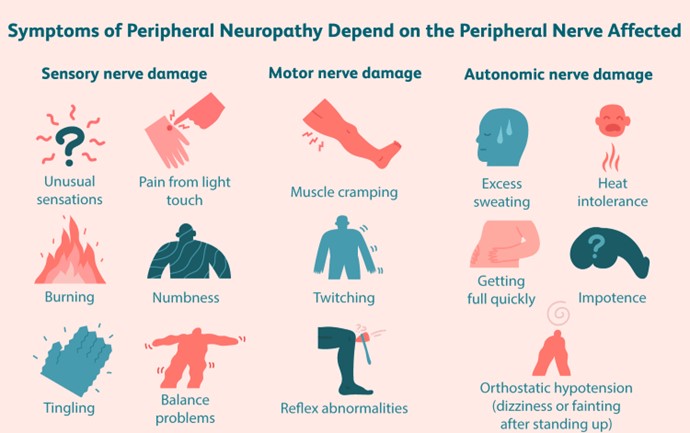
Choice C: Numbness of the hands is a common finding of hypoparathyroidism, as low levels of parathyroid hormone can cause hypocalcemia, which affects the nerve function and sensation. Numbness can also occur in the feet, lips, and tongue.
Choice D: Hypercalcemia is a high level of calcium in the blood. This is not a finding of hypoparathyroidism, as low levels of parathyroid hormone can cause hypocalcemia, which is a low level of calcium in the blood. Hypercalcemia can be a sign of hyperparathyroidism, which is the opposite condition of hypoparathyroidism.
A nurse in a provider’s office is collecting data from a client who has hypothyroidism. Which of the following findings should the nurse expect?
Explanation
Choice A: Blurred vision is not a typical finding of hypothyroidism. It can be caused by other conditions, such as diabetes, glaucoma, or eye strain.
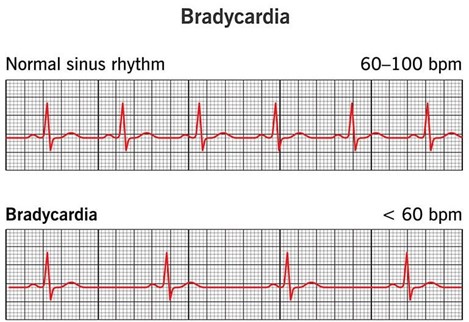
Choice B: Bradycardia is a slow heart rate, usually below 60 beats per minute. This is a common finding of hypothyroidism, as the thyroid hormone regulates the metabolic rate and affects the cardiovascular system. Low levels of thyroid hormone can cause the heart to beat slower and weaker.
Choice C: Insomnia is difficulty falling or staying asleep. This is not a common finding of hypothyroidism, as low thyroid hormone levels can cause fatigue, lethargy, and excessive sleepiness.
Choice D: Moist skin is not a common finding of hypothyroidism, as low thyroid hormone levels can cause dry skin, hair loss, and britle nails. Moist skin can be a sign of hyperthyroidism, which is the opposite condition of hypothyroidism.
A nurse is reinforcing teaching with a client who has diabetes mellitus and a new prescription for lispro and Lantus insulins. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A reason: Insulin injected into the thigh is not the most rapidly absorbed. The abdomen is the preferred site for insulin injection, as it has the fastest and most consistent absorption rate. The thigh, arm, and butock have slower and more variable absorption rates12.
Choice B reason: The botle of insulin should not be shaken before withdrawing the medication. Shaking can damage the insulin molecules and affect their potency and effectiveness. Instead, the botle should be gently rolled between the palms to mix the insulin evenly13.
Choice C reason: Lantus insulin should not be used immediately before each meal. Lantus is a long-acting insulin that provides a steady basal level of insulin for 24 hours. It should be taken once a day at the same time every day, regardless of meals. Humalog is a rapid-acting insulin that can be used immediately before each meal to cover the postprandial glucose spikes14.
Choice D reason: Unopened vials of insulin should be kept in the refrigerator until needed. This can help preserve their quality and potency until their expiration date. Opened vials of insulin can be kept at room temperature for up to 28 days, depending on the type and brand
A nurse is assisting with menu selections for a client who has recovered from the acute phase of diverticulitis. Which of the following foods should the nurse recommend?
Explanation
Choice A reason: Roast chicken with white rice is a low-fiber, easy-to-digest meal that is suitable for a client who has recovered from the acute phase of diverticulitis. A low-fiber diet can help reduce the stress on the colon and allow it to heal. White rice is a refined grain that has less fiber than whole grains, such as brown rice or quinoa12.
Choice B reason: A poached egg with sliced tomatoes is not a good choice for a client who has recovered from the acute phase of diverticulitis. Although eggs are a good source of protein and do not contain fiber, tomatoes are high in fiber and may irritate the colon. Tomatoes also have seeds, which were previously thought to cause problems for people with diverticular disease, but there is no evidence to support this. However, some people may still find them uncomfortable to eat13.
Choice C reason: Bean soup with steamed broccoli is not a good choice for a client who has recovered from the acute phase of diverticulitis. Beans and broccoli are both high in fiber and may cause gas, bloating, and cramping in the colon. A high-fiber diet is recommended for people with diverticulosis (the presence of pouches without inflammation) to prevent constipation and diverticulitis, but it should be avoided during or shortly after an episode of diverticulitis12.
Choice D reason: Ham sandwich on white bread is not a good choice for a client who has recovered from the acute phase of diverticulitis. Although white bread is low in fiber, ham is a processed meat that may increase the risk of developing diverticular disease. Research suggests that a diet high in red meat and processed meat may contribute to inflammation and infection of the pouches in the colon.

A nurse is reinforcing teaching about the manifestations of hyperglycemia with a client who has diabetes mellitus. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
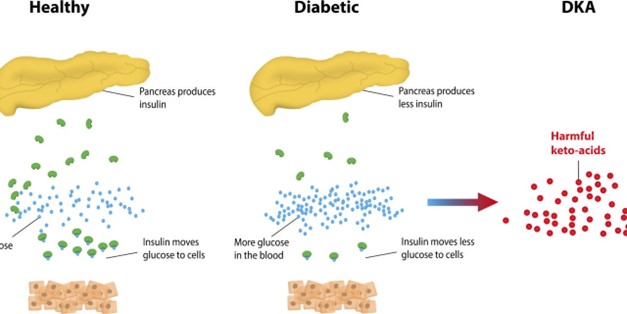
Choice A reason: A fruity odor in the breath is a symptom of hyperglycemia, especially when it is severe and causes ketoacidosis. Ketoacidosis is a condition where the body produces ketones, which are acidic substances that result from the breakdown of fat for energy when there is not enough insulin or glucose available. Ketones can make the breath smell fruity or like nail polish remover.
Choice B reason: A decreased appetite is not a symptom of hyperglycemia. On the contrary, an increased appetite or hunger is a symptom of hyperglycemia, as the body tries to compensate for the lack of glucose in the cells by stimulating the hunger center in the brain.
Choice C reason: An increased thirst is a symptom of hyperglycemia, as the body tries to flush out the excess glucose and ketones in the blood through urine. This leads to dehydration and thirst signals in the brain.
Choice D reason: A blurry vision at times is a symptom of hyperglycemia, as high blood glucose levels can cause swelling and damage to the lens of the eye, affecting its ability to focus light properly. This can lead to temporary or permanent vision problems.
A nurse is reinforcing teaching about preventing long-term complications of retinopathy and neuropathy with an older adult client who has diabetes mellitus. Which of the following actions is the most important for the nurse to include in the teaching?
Explanation
Choice A reason: Wearing closed-toed shoes daily is a good practice for people with diabetes, as it can protect the feet from injuries and infections. However, it is not the most important action for preventing long-term complications of retinopathy and neuropathy. These complications are mainly caused by high blood glucose levels that damage the blood vessels and nerves in the eyes and feet.
Choice B reason: Maintaining stable blood glucose levels is the most important action for preventing long-term complications of retinopathy and neuropathy. High blood glucose levels can cause oxidative stress, inflammation, and endothelial dysfunction, which impair the blood flow and oxygen delivery to the eyes and feet. This can lead to nerve damage (neuropathy) and vision loss (retinopathy) over time. Keeping blood glucose levels within the target range can reduce the risk of these complications and slow down their progression if they already exist.
Choice C reason: Planning to have an eye examination once per year is a recommended action for people with diabetes, as it can help detect and treat retinopathy before it causes irreversible damage to the retina. However, it is not the most important action for preventing long-term complications of retinopathy and neuropathy. Eye examinations cannot prevent retinopathy from occurring or worsening; they can only monitor its status and provide appropriate interventions.
Choice D reason: Examining your feet carefully every day is another recommended action for people with diabetes, as it can help identify and treat any signs of neuropathy, such as numbness, tingling, pain, or ulcers. However, it is not the most important action for preventing long-term complications of retinopathy and neuropathy. Foot examinations cannot prevent neuropathy from occurring or worsening; they can only monitor its status and provide appropriate care.
A nurse is reinforcing teaching with a client who is scheduled for a blood test to measure her thyroid stimulating hormone (TSH) level. Which of the following statements should the nurse give?
Explanation
Choice A reason: This test does not detect antithyroid antibodies in your blood. Antithyroid antibodies are proteins that atack the thyroid gland and can cause autoimmune thyroid diseases, such as Hashimoto’s thyroiditis or Graves’ disease. To detect antithyroid antibodies, you need a different blood test called the thyroid peroxidase (TPO) antibody test.
Choice B reason: This test does not measure the amount of thyroid hormone that ataches to a protein in your blood. Thyroid hormone can exist in two forms in the blood: free or bound. Free thyroid hormone is not atached to any protein and can enter the cells and tissues where it is needed. Bound thyroid hormone is atached to a protein called thyroxine-binding globulin (TBG) and cannot enter the cells and tissues. To measure the amount of thyroid hormone that ataches to TBG, you need a different blood test called the total thyroxine (T4) test.
Choice C reason: This test determines whether your thyroid gland is overactive, appropriately active, or underactive. TSH is a hormone produced by the pituitary gland that stimulates the thyroid gland to make and release thyroid hormones, such as thyroxine (T4) and triiodothyronine (T3). These hormones regulate many body functions, such as metabolism, growth, and development. The TSH test measures the amount of TSH in the blood and reflects how well the thyroid gland is working. If the TSH level is high, it means that the thyroid gland is underactive (hypothyroidism) and not making enough thyroid hormones. If the TSH level is low, it means that the thyroid gland is overactive (hyperthyroidism) and making too much thyroid hormones.
Choice D reason: This test does not measure the absorption of iodine and how it relates to the thyroid gland. Iodine is a mineral that is essential for the production of thyroid hormones. The thyroid gland absorbs iodine from the food and water we consume and uses it to make T4 and T3. To measure the absorption of iodine by the thyroid gland, you need a different test called the radioactive iodine uptake (RAIU) test.

A nurse is reinforcing teaching about exercise with a client who has type 1 diabetes mellitus. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A reason: Injecting insulin into a muscle that is going to be exercised can increase the absorption of insulin and lower the blood glucose level, leading to hypoglycemia. Therefore, it is advisable to avoid injecting insulin into the same body part that will be involved in the exercise.
Choice B reason: Carrying a complex carbohydrate snack with you when you exercise is not a good idea. Complex carbohydrates take longer to digest and raise the blood glucose level slowly. They are not suitable for treating or preventing hypoglycemia during or after exercise. A simple carbohydrate snack, such as glucose tablets, juice or candy, is more appropriate for this purpose.
Choice C reason: Exercising first thing in the morning before eating breakfast is not recommended for people with type 1 diabetes. This can cause a drop in blood glucose level and increase the risk of hypoglycemia. It is beter to have a balanced breakfast that includes some carbohydrates and adjust the insulin dose accordingly before exercising.
Choice D reason: Increasing the intensity of your exercise routine if your urine is positive for ketones is a dangerous practice. Ketones are produced when the body breaks down fat for energy due to lack of insulin or glucose. High levels of ketones can lead to diabetic ketoacidosis, a life-threatening condition that requires urgent medical atention. Intense exercise can raise the blood glucose level further and worsen the situation. If your urine is positive for ketones, you should avoid vigorous activity and check your blood glucose and ketone levels frequently.
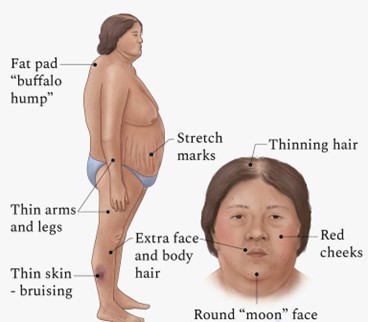
A nurse is collecting data from a client who has Cushing’s syndrome. Which of the following findings should the nurse expect?
Explanation
Choice A reason: Weight loss is not a symptom of Cushing’s syndrome. On the contrary, weight gain and obesity are common signs of this condition, especially in the trunk, face and upper back1.
Choice B reason: Diaphoresis, or excessive sweating, is not a symptom of Cushing’s syndrome. It can be caused by other conditions, such as hyperthyroidism, menopause or anxiety.
Choice C reason: Hyperpigmentation, or darkening of the skin, is a symptom of Cushing’s syndrome. It occurs due to increased production of melanin, the pigment that gives color to the skin. Hyperpigmentation can affect any part of the body, but it is more noticeable in areas exposed to friction or pressure, such as the elbows, knees, knuckles and armpits.
Choice D reason: Hypotension, or low blood pressure, is not a symptom of Cushing’s syndrome. In fact, high blood pressure (hypertension) is one of the common symptoms of this condition, due to the effects of cortisol on the cardiovascular system.
A nurse is preparing a client who has advanced cirrhosis for an abdominal paracentesis. Which of the following actions should the nurse take?
Explanation
Choice A: Place the client on his back. This is incorrect because the client should be placed in a sitting position with the head of the bed elevated to 30 to 45 degrees. This allows the fluid to accumulate in the lower abdomen and reduces the risk of puncturing the diaphragm.
Choice B: Have the client increase fluid intake after the procedure. This is also incorrect because the client should restrict fluid intake after the procedure to prevent fluid overload and electrolyte imbalance. The nurse should monitor the client’s intake and output, weight, and vital signs.
Choice C: Assure the client that the procedure is painless. This is not true because the client may experience some discomfort or pressure during the insertion of the needle or catheter. The nurse should administer analgesics as prescribed and provide emotional support.
Choice D: Instruct the client to empty his bladder. This is correct because this reduces the risk of bladder injury during the procedure. The nurse should also measure and record the amount of urine voided.
A nurse is reinforcing teaching for a client who has type 1 diabetes mellitus about foot care. Which of the following client statements should indicate to the nurse an understanding of the instructions?
Explanation
Choice A: “I put lotion between my toes.” This is incorrect because putting lotion between the toes can create a moist environment that promotes fungal growth and infection. The client should apply lotion to the tops and botoms of the feet, but avoid the areas between the toes.
Choice B: “I check my feet every day for sores and bruises.” This is correct because checking the feet every day for any signs of injury, infection, or ulceration is an important part of foot care for a client who has diabetes mellitus. The client should also report any problems to the provider and seek prompt treatment.
Choice C: “I wear sandals in warm weather.” This is incorrect because wearing sandals can expose the feet to injury, sunburn, or insect bites. The client should wear closed-toe shoes that fit well and protect the feet from trauma and environmental hazards.
Choice D: “I soak my feet in warm, soapy water every night before I go to bed.” This is incorrect because soaking the feet can cause maceration of the skin and increase the risk of infection. The client should wash the feet with mild soap and warm water, but not soak them. The client should also dry the feet thoroughly, especially between the toes.
A nurse is contributing to the plan of care for a client who has an intestinal obstruction and is receiving continuous gastrointestinal decompression using a nasogastric tube. Which of the following interventions should the nurse include in the plan of care?
Explanation
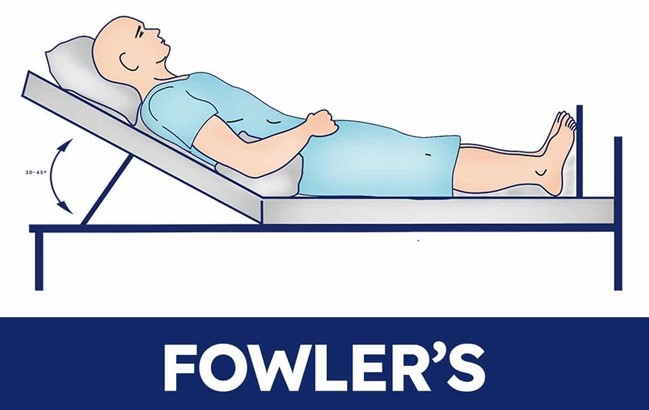
Choice A: Maintain the client in Fowler’s position. This is correct because Fowler’s position, which is a semi-sitting position with the head of the bed elevated 45 to 60 degrees, can facilitate the drainage of gastric contents and reduce the risk of aspiration.
Choice B: Use sterile water to irrigate the nasogastric tube. This is incorrect because sterile water is not necessary to irrigate the nasogastric tube, unless the client is immunocompromised or has a high risk of infection. Tap water or normal saline can be used to irrigate the nasogastric tube, following the provider’s orders or the facility’s protocol.
Choice C: Moisten the client’s lips with lemon-glycerin swabs. This is incorrect because lemon-glycerin swabs can dry out and irritate the client’s lips and oral mucosa, especially if used frequently. The nurse should use water-soluble lubricant or lip balm to moisturize the client’s lips and mouth.
Choice D: Measure abdominal girth daily. This is incorrect because measuring abdominal girth daily is not enough to monitor the progression of the intestinal obstruction and the effectiveness of the gastrointestinal decompression. The nurse should measure abdominal girth more frequently, such as every 4 hr or every shift, and report any changes or abnormalities.
A nurse finds a client who has type 1 diabetes mellitus lying in bed, sweating, tachycardic, and reporting feeling lightheaded and shaky. Which of the following complications should the nurse suspect?
Explanation
Choice A: Ketoacidosis. This is incorrect because ketoacidosis is a complication of hyperglycemia, not hypoglycemia. Ketoacidosis occurs when the body breaks down fat for energy due to insufficient insulin, resulting in the accumulation of ketones and acids in the blood. Ketoacidosis can cause symptoms such as nausea, vomiting, abdominal pain, fruity breath odor, deep and rapid breathing, and altered mental status.
Choice B: Hyperglycemia. This is incorrect because hyperglycemia is a condition of high blood glucose, not low blood glucose. Hyperglycemia can occur due to insufficient insulin, excessive carbohydrate intake, infection, stress, or illness. Hyperglycemia can cause symptoms such as polyuria, polydipsia, polyphagia, blurred vision, fatigue, and headache.
Choice C: Hypoglycemia. This is correct because hypoglycemia is a condition of low blood glucose, which can occur due to excessive insulin, inadequate carbohydrate intake, exercise, alcohol consumption, or medication interactions. Hypoglycemia can cause symptoms such as sweating, tachycardia, palpitations, tremors, hunger, anxiety, confusion, dizziness, weakness, and seizures.
Choice D: Nephropathy. This is incorrect because nephropathy is a complication of chronic hyperglycemia, not acute hypoglycemia. Nephropathy is a kidney disease that results from damage to the small blood vessels and glomeruli in the kidneys due to high blood glucose levels. Nephropathy can cause symptoms such as proteinuria, edema, hypertension, and renal failure.
A nurse is assisting with teaching a newly licensed nurse about parenteral nutrition (PN). Which of the following information should the nurse include in the teaching?
Explanation
Choice A: Weigh the client weekly. This is incorrect because the client receiving PN should be weighed daily, not weekly, to monitor fluid balance and nutritional status. The nurse should also measure the client’s intake and output, blood glucose, electrolytes, and other laboratory values daily.
Choice B: Reduce the rate of the solution gradually to discontinue. This is correct because the nurse should taper off the PN solution slowly to prevent rebound hypoglycemia, which can occur when the high concentration of glucose in the PN solution is abruptly stopped. The nurse should follow the provider’s orders or the facility’s protocol for reducing and discontinuing PN.
Choice C: Remove solution from refrigerator 2 hr before infusion. This is incorrect because the nurse should remove the PN solution from the refrigerator 30 to 60 minutes before infusion, not 2 hr, to allow it to reach room temperature. Infusing a cold solution can cause discomfort, vasoconstriction, and impaired absorption of nutrients.
Choice D: Shake the solution before hanging if there is a layer of fat present on the top. This is incorrect because the nurse should not shake the PN solution at all, as this can cause fat emulsion droplets to coalesce and form large particles that can clog the filter or cause embolism. The nurse should gently invert or roll the PN solution container to mix it if there is any separation of components.
A charge nurse is reinforcing teaching with a newly licensed nurse about the common link between ulcerative colitis and Crohn’s disease. Which of the following statements by the newly licensed nurse indicates an understanding of the teaching?
Explanation
Choice A: Both illnesses result in malabsorption of nutrients. This is incorrect because malabsorption of nutrients is more common in Crohn’s disease than in ulcerative colitis. Crohn’s disease can affect any part of the gastrointestinal tract, including the small intestine, where most of the nutrient absorption occurs. Ulcerative colitis mainly affects the colon and rectum, which are responsible for water and electrolyte absorption.
Choice B: Both illnesses begin in the rectum. This is incorrect because ulcerative colitis usually begins in the rectum and spreads proximally to the colon, while Crohn’s disease can begin anywhere in the gastrointestinal tract, from the mouth to the anus.
Choice C: Both illnesses manifest fistula formation. This is incorrect because fistula formation is more common in Crohn’s disease than in ulcerative colitis. Fistulas are abnormal connections between different parts of the gastrointestinal tract or other organs, such as the bladder, vagina, or skin. They are caused by inflammation, ulceration, and infection that penetrate through the bowel wall.
Choice D: Both illnesses are inflammatory in nature. This is correct because both ulcerative colitis and Crohn’s disease are types of inflammatory bowel disease (IBD), which are chronic conditions that cause inflammation and damage to the gastrointestinal tract. The exact cause of IBD is unknown, but it may involve genetic, immune, environmental, and microbial factors.

A nurse is collecting data on a client who has hyperthyroidism. Which of the following manifestations should the nurse expect the client to report?
Explanation
Choice A: Sensitivity to cold. This is incorrect because sensitivity to cold is a manifestation of hypothyroidism, not hyperthyroidism. Clients with hyperthyroidism have increased metabolism and heat production, which makes them more sensitive to heat.
Choice B: Frequent mood changes. This is correct because frequent mood changes are a manifestation of hyperthyroidism. Clients with hyperthyroidism have increased levels of thyroid hormones, which can affect their nervous system and cause irritability, anxiety, nervousness, or emotional instability.
Choice C: Weight gain. This is incorrect because weight gain is a manifestation of hypothyroidism, not hyperthyroidism. Clients with hyperthyroidism have increased metabolism and appetite, which makes them lose weight or have difficulty gaining weight.
Choice D: Constipation. This is incorrect because constipation is a manifestation of hypothyroidism, not hyperthyroidism. Clients with hyperthyroidism have increased bowel motility and peristalsis, which makes them more prone to diarrhea or frequent stools.
A nurse is contributing to the plan of care of a client who has a small bowel obstruction. Which of the following interventions should the nurse include?
Explanation
Choice A: Provide bulk-forming agent. This is incorrect because bulk-forming agents are used to treat constipation, not bowel obstruction. They can worsen the obstruction by increasing the stool volume and pressure in the bowel.
Choice B: Elevate the head of the bed. This is incorrect because elevating the head of the bed does not directly affect the bowel obstruction. It may help with respiratory comfort, but it is not a priority intervention.
Choice D: Monitor intake and output every 8 hr. This is incorrect because monitoring intake and output is not enough to assess the fluid and electrolyte balance of a client with a bowel obstruction. The nurse should monitor intake and output more frequently, such as every 4 hr or every shift, and report any signs of dehydration or imbalance.
Choice C: Measure abdominal girth daily. This is correct because measuring abdominal girth daily can help monitor the progression of the bowel obstruction and the effectiveness of the treatment. An increase in abdominal girth may indicate worsening obstruction, distension, or perforation, while a decrease may indicate resolution or relief of the obstruction.
A nurse is reviewing the laboratory report of a client who has hypoparathyroidism. The nurse should expect which of the following values?
Explanation
Choice A reason: Phosphate 5.7 mg/dL is an elevated value, as the normal range is 2.5 to 4.5 mg/dL. Hypoparathyroidism causes low levels of parathyroid hormone (PTH), which regulates calcium and phosphorus balance in the body. Low PTH leads to low calcium and high phosphorus levels in the blood.
Choice B reason: Vitamin D 25 ng/mL is a normal value, as the normal range is 20 to 50 ng/mL. Hypoparathyroidism does not directly affect vitamin D levels, but vitamin D supplements may be given to help increase calcium absorption and lower phosphorus levels in the blood.
Choice C reason: Calcium 9.8 mg/dL is a normal value, as the normal range is 8.6 to 10.2 mg/dL. Hypoparathyroidism causes low levels of parathyroid hormone (PTH), which regulates calcium and phosphorus balance in the body. Low PTH leads to low calcium and high phosphorus levels in the blood. However, calcium levels may be normal or near- normal in some cases of hypoparathyroidism, especially if the condition is mild or well-controlled with treatment.
Choice D reason: Magnesium 1.8 mEq/L is a normal value, as the normal range is 1.5 to 2.5 mEq/L. Hypoparathyroidism does not directly affect magnesium levels, but magnesium deficiency can cause or worsen hypoparathyroidism, as magnesium is needed for PTH secretion and action. Magnesium supplements may be given to correct magnesium deficiency and improve PTH function.
A nurse is caring for a client who is experiencing an acute exacerbation of ulcerative colitis. The nurse should recognize that which of the following actions is the priority?
Explanation
Choice A reason: Providing emotional support is important for a client who has ulcerative colitis, as the condition can affect their quality of life and mental health. However, this is not the priority action for a nurse who is caring for a client who is experiencing an acute exacerbation of ulcerative colitis, as it does not address the immediate physical needs of the client.
Choice B reason: Evaluating fluid and electrolyte levels is the priority action for a nurse who is caring for a client who is experiencing an acute exacerbation of ulcerative colitis, as the client is at risk of dehydration, hypovolemia, and electrolyte imbalances due to diarrhea, vomiting, and poor oral intake. The nurse should monitor the client’s vital signs, urine output, weight, skin turgor, mucous membranes, and laboratory values such as serum sodium, potassium, chloride, bicarbonate, blood urea nitrogen (BUN), and creatinine.
Choice C reason: Promoting physical mobility is beneficial for a client who has ulcerative colitis, as it can help prevent complications such as deep vein thrombosis (DVT), pulmonary embolism (PE), and pressure ulcers. However, this is not the priority action for a nurse who is caring for a client who is experiencing an acute exacerbation of ulcerative colitis, as the client may have abdominal pain, fatigue, and weakness that limit their mobility. The nurse should encourage rest and provide comfort measures such as positioning, heat therapy, and analgesics.
Choice D reason: Reviewing stress factors that can cause disease exacerbation is helpful for a client who has ulcerative colitis, as stress can trigger or worsen inflammation in the bowel. However, this is not the priority action for a nurse who is caring for a client who is experiencing an acute exacerbation of ulcerative colitis, as it does not address the immediate physical needs of the client. The nurse should teach the client about stress management techniques and refer them to appropriate resources such as counseling or support groups.
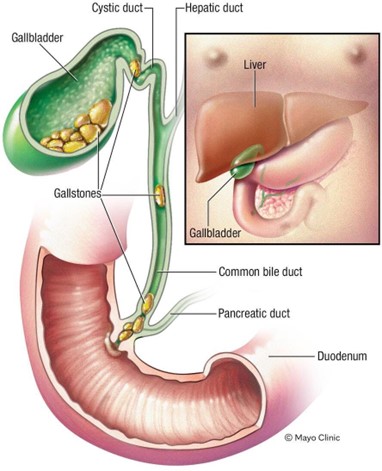
A nurse is collecting data on a client who has acute pancreatitis. Which of the following factors should the nurse anticipate in the client’s history?
Explanation
Choice A reason: Shock is not a cause of acute pancreatitis, but a possible complication of severe cases that can lead to organ failure and death.
Choice B reason: Gallstones are one of the major causes of acute pancreatitis, as they can block the pancreatic duct and prevent the flow of digestive enzymes, leading to inflammation and damage of the pancreas.
Choice C reason: Diabetes mellitus is not a cause of acute pancreatitis, but a possible complication of chronic pancreatitis, as the damage to the pancreas can impair its ability to produce insulin and regulate blood sugar levels.
Choice D reason: GERD (gastroesophageal reflux disease) is not a cause of acute pancreatitis, but a condition that affects the lower esophageal sphincter and allows stomach acid to reflux into the esophagus, causing heartburn and other symptoms.
A nurse is assisting in the plan of care for a client who had surgery for a bowel obstruction. The client has a nasogastric tube in place. Which of the following actions should the nurse include in the client’s plan of care? (Select all that apply).
Explanation
Choice A reason: Documenting the color, consistency, and amount of nasogastric drainage is an important action for the nurse to include in the client’s plan of care. This can help monitor the client’s GI function, fluid balance, and response to treatment. The normal color of nasogastric drainage is clear or yellow-green. Abnormal colors include red, brown, or black, which may indicate bleeding.
Choice B reason: Encouraging hourly use of an incentive spirometer while awake is an important action for the nurse to include in the client’s plan of care. This can help prevent respiratory complications, such as atelectasis and pneumonia, which are common after abdominal surgery. An incentive spirometer is a device that helps the client breathe deeply and expand the lungs.
Choice C reason: Irrigating the nasogastric tube every 4 to 8 hr is not an action that the nurse should include in the client’s plan of care. Routine irrigation of nasogastric tubes is not recommended, as it may increase the risk of infection, tube occlusion, or aspiration. Irrigation should only be done when indicated by specific orders or protocols, or when there is evidence of tube blockage.
Choice D reason: Performing leg exercises every 2 hr is an important action for the nurse to include in the client’s plan of care. This can help prevent venous thromboembolism (VTE), which is a serious complication that can occur after surgery due to immobility and hypercoagulability. Leg exercises can improve blood circulation and reduce stasis in the lower extremities.
A nurse is reinforcing teaching with a client who has type 2 diabetes mellitus. The nurse determines that teaching has been effective when the client identifies which of the following manifestations of hypoglycemia? (Select all that apply.)
Explanation
Choice A reason: Tachycardia is a common symptom of hypoglycemia, as the body releases adrenaline and other hormones to raise the blood sugar level. This can cause the heart to beat faster and stronger.
Choice B reason: Blurry vision is a common symptom of hypoglycemia, as low blood sugar can affect the ability of the eyes to focus and see clearly. This can also cause headaches, dizziness, or double vision.
Choice C reason: Sweating is a common symptom of hypoglycemia, as the body tries to cool down and cope with the stress of low blood sugar. This can also cause shakiness, trembling, or tingling in the lips, tongue, or cheek.
Choice D reason: Polydipsia (excessive thirst) is not a symptom of hypoglycemia, but a symptom of hyperglycemia (high blood sugar). High blood sugar can cause dehydration and dry mouth, which make the person feel thirsty.
Choice E reason: Polyuria (excessive urination) is not a symptom of hypoglycemia, but a symptom of hyperglycemia (high blood sugar). High blood sugar can cause the kidneys to filter out excess glucose and water from the blood, which make the person urinate more often.
A nurse is assisting with the care of a client in the emergency department.
Nurses Notes 1030:
Client reports nausea and indigestion for the past few days and worsens after meals and belches a lot. Denies vomiting. Client is alert and oriented to person, place and time. Clients skin is pink and moist to touch. Bowel sounds are normoactive and in all quadrants. Abdomen is soft, nontender to touch and doesn’t appear to be distended. Lung sounds are clear. Last bowel movement was this morning. Peripheral pulses +2. No edema present.
The nurse is reviewing the client’s health information. For each potential provider’s prescription, tick to specify if the assessment findings is consistent with myocardial infraction or gastroesophageal reflux disease (Gerd), each finding may support more than one disease process.
No explanation
Sign Up or Login to view all the 25 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

