ATI NUR 200 maternity exam
Total Questions : 49
Showing 25 questions, Sign in for moreAfter teaching a group of adolescents about HIV, the nurse asks them to identify the primary means by which adolescents are exposed to the virus. The nurse determines that the teaching was successful when the group identifies which means of exposure?
Explanation
A. Blood transfusion:
Historically, blood transfusions were a significant mode of HIV transmission. However, with improved screening techniques and blood supply management, the risk of HIV transmission through blood transfusions has been greatly reduced. It's still a potential risk, but much less common than it used to be.
B. Sharing needles for IV drug use:
Sharing needles or other drug paraphernalia is a high-risk behavior for HIV transmission because it can directly introduce infected blood into the bloodstream. Injection drug use is a significant risk factor for acquiring HIV, especially among adolescents and adults who engage in this behavior.
C. Perinatal transmission:
Perinatal transmission occurs when a pregnant woman with HIV passes the virus to her child during pregnancy, childbirth, or breastfeeding. With proper medical care and interventions, the risk of perinatal transmission can be significantly reduced. However, without appropriate interventions, the risk of transmission from mother to child is significant.
D. Sexual intercourse:
Sexual intercourse, particularly unprotected vaginal, anal, or oral sex with an infected partner, is the most common mode of HIV transmission among adolescents and adults. It's important to educate individuals about safe sex practices, including the use of condoms and communication with sexual partners about HIV status, to prevent transmission.
A nurse suspects that a client is developing HELLP syndrome. The nurse notifies the health care provider based on which finding?
Explanation
A. Disseminated intravascular coagulation (DIC):
DIC is a serious condition characterized by abnormal clotting throughout the body's blood vessels, leading to both bleeding and clotting simultaneously. While it can occur in severe cases of HELLP syndrome, it is not a specific finding used to diagnose HELLP syndrome. Instead, it's a complication that can develop due to various underlying conditions, including HELLP syndrome.
B. Elevated platelet count:
In HELLP syndrome, platelet count is typically decreased, not elevated. HELLP syndrome stands for Hemolysis, Elevated Liver enzymes, and Low Platelets. The low platelet count is a key diagnostic feature of HELLP syndrome and contributes to the risk of bleeding complications.
C. Elevated liver enzymes:
Elevated liver enzymes, particularly elevated levels of AST (aspartate aminotransferase) and ALT (alanine aminotransferase), are hallmark features of HELLP syndrome. Liver involvement is a significant component of this syndrome, and elevated liver enzymes are part of the diagnostic criteria.
D. Hyperglycemia:
While hyperglycemia can occur in various conditions, it is not a characteristic finding of HELLP syndrome. HELLP syndrome primarily affects the liver, blood clotting factors, and platelets, leading to features such as elevated liver enzymes, low platelet count, and hemolysis (destruction of red blood cells).

Which approach would be most appropriate when counseling a client who is a suspected victim of intimate partner violence?
Explanation
A. Ask, "Have you ever been physically hurt by your partner?":
This approach involves directly asking the client about their experience with intimate partner violence. While it's crucial to address the issue openly and directly, some clients may feel uncomfortable or unsafe disclosing abuse, especially during an initial encounter. However, for many clients, this direct approach can be empowering and may facilitate disclosure.
B. Offer the client a pamphlet about the local shelter for victims of intimate partner violence:
Providing informational resources about local shelters and support services can be a supportive and non-confrontational way to offer assistance to a client who may be experiencing intimate partner violence. It allows the client to access resources privately and at their own pace. However, it may not lead to immediate disclosure or intervention.
C. Call the client at home to ask some questions about the marriage:
Calling the client at home to inquire about their relationship may inadvertently escalate the situation and put the client at risk if the abusive partner overhears the conversation. It can also violate the client's privacy and autonomy, as they may not be comfortable discussing sensitive issues over the phone, especially if the abusive partner is present.
D. Wait until the client comes in a few more times to make a better assessment:
Delaying assessment and intervention can potentially prolong the client's exposure to abuse and increase their risk of harm. Intimate partner violence often escalates over time, so it's essential to address suspected abuse as soon as possible to ensure the client's safety and well-being.
When performing a clinical breast examination, which would the nurse do first?
Explanation
A. Inspect the breasts:
Inspecting the breasts visually is usually the first step in a clinical breast examination. The nurse observes the size, shape, symmetry, and skin characteristics of the breasts, including any visible abnormalities such as dimpling, puckering, or changes in skin texture or color.
B. Palpate the axillary area:
Palpating the axillary (underarm) area is typically done after inspecting the breasts. This allows the nurse to assess for any enlarged lymph nodes or palpable masses in the axillary region, which could indicate pathology or breast cancer metastasis.
C. Compress the nipple for a discharge:
If there are concerns about nipple discharge, this step may follow breast palpation. By gently compressing the nipple, the nurse can assess for any abnormal discharge, such as bloody or spontaneous discharge, which may warrant further investigation.
D. Palpate the breasts:
Palpating the breasts is usually performed after visual inspection and axillary palpation. During breast palpation, the nurse systematically examines each breast using circular motions with varying pressure to detect any lumps, masses, or areas of tenderness. This thorough palpation helps identify any abnormalities within the breast tissue.
The nurse is presenting a class at a local community health center on violence during pregnancy. Which possible complication would the nurse include?
Explanation
A. Postterm labor:
Postterm labor refers to labor that occurs after 42 weeks of gestation. While stress and trauma can contribute to preterm labor, there isn't a direct association between violence during pregnancy and postterm labor.
B. Chorioamnionitis:
Chorioamnionitis is an infection of the fetal membranes (chorion and amnion) and amniotic fluid. While violence during pregnancy doesn't directly cause chorioamnionitis, infections can occur if there are injuries sustained during violent episodes or if there's poor prenatal care due to the effects of violence.
C. Gestational hypertension:
Gestational hypertension, also known as pregnancy-induced hypertension, is characterized by high blood pressure that develops during pregnancy. Chronic stress and anxiety resulting from violence during pregnancy can contribute to elevated blood pressure levels, potentially leading to gestational hypertension.
D. Placenta previa:
Placenta previa occurs when the placenta partially or completely covers the cervix, increasing the risk of bleeding during pregnancy and delivery. While violence during pregnancy doesn't directly cause placenta previa, it can indirectly impact placental health and function due to stress-induced physiological changes.
Assessment of a female client reveals a thick, white vaginal discharge. The client also reports intense itching and dyspareunia. Based on these findings, the nurse would suspect that the client has:
Explanation
A. Candidiasis:
Candidiasis is caused by an overgrowth of the fungus Candida albicans in the vagina. It typically presents with symptoms such as thick, white vaginal discharge (resembling cottage cheese), itching, and discomfort during sexual intercourse (dyspareunia). This option is the most likely diagnosis based on the client's symptoms.
B. Genital herpes simplex:
Genital herpes simplex is caused by the herpes simplex virus (HSV). It presents with symptoms such as painful, fluid-filled blisters or sores in the genital area. While genital herpes can cause vaginal discharge, the discharge is typically clear or cloudy, not thick and white as described in the scenario.
C. Trichomoniasis:
Trichomoniasis is a sexually transmitted infection caused by the parasite Trichomonas vaginalis. It commonly presents with symptoms such as a frothy, yellow-green vaginal discharge, itching, and discomfort during urination or sexual intercourse. The discharge is typically not described as thick and white.
D. Bacterial vaginosis:
Bacterial vaginosis results from an imbalance of bacteria in the vagina, with a decrease in beneficial bacteria and an overgrowth of harmful bacteria. It presents with symptoms such as a thin, grayish-white vaginal discharge with a fishy odor. While bacterial vaginosis can cause vaginal discomfort, the discharge is not typically described as thick and white.

The nurse is developing the discharge plan for a woman who has had a left-sided radical mastectomy. The nurse is including instructions for ways to minimize lymphedema. Which statement by the client indicates the need for additional instruction?
Explanation
A. "I need to avoid driving to and from work every day."
This statement indicates a misunderstanding of how to minimize lymphedema. Driving itself does not directly contribute to lymphedema. However, activities that involve prolonged or repetitive use of the affected arm, such as gripping the steering wheel while driving for long periods, may increase the risk of developing lymphedema. The nurse should clarify that while driving is generally acceptable, the client should take breaks and perform arm exercises during long drives to promote circulation.
B. "Any blood pressures need to be taken in my right arm."
This statement demonstrates correct understanding. Taking blood pressure measurements, administering injections, or obtaining blood samples from the unaffected arm helps prevent trauma or injury to the arm at risk for lymphedema. This practice helps avoid disrupting lymphatic flow and reduces the risk of developing lymphedema in the affected arm.
C. "I need to wear gloves when doing any gardening."
Wearing gloves during gardening is a recommended precaution to minimize the risk of injury and infection, especially if the client has undergone lymph node removal. This statement reflects appropriate understanding and adherence to preventive measures to protect the affected arm from cuts, scratches, and potential infection that could exacerbate lymphedema.
D. "I should wear clothing with elasticized sleeves."
This statement indicates a misunderstanding of how to minimize lymphedema. While elasticized sleeves or compression garments can help manage lymphedema by providing gentle compression and support to the affected arm, wearing tight or constrictive clothing, including elasticized sleeves, can potentially restrict lymphatic flow and exacerbate lymphedema. The nurse should clarify that loose-fitting clothing is preferable to allow unrestricted movement and circulation in the affected arm.
A nurse is conducting a review class for a group of perinatal nurses working at the local clinic. The clinic sees a high population of women who are HIV positive. After discussing the recommendations for antiretroviral therapy with the group, the nurse determines that the teaching was successful when the group identifies which rationale as the underlying principle for the therapy?
Explanation
A. adjunct therapy to radiation and chemotherapy:
This option is not applicable to HIV/AIDS treatment. Antiretroviral therapy (ART) is specifically used to treat HIV infection by targeting the replication of the virus. It is not used as adjunct therapy to radiation or chemotherapy, which are treatments typically used for cancer.
B. treatment of opportunistic infections:
While antiretroviral therapy (ART) can help prevent opportunistic infections by boosting the immune system, its primary purpose is not the treatment of these infections. Rather, ART focuses on suppressing the replication of the HIV virus itself.
C. reduction in viral loads in the blood:
This is the correct rationale for antiretroviral therapy. The main goal of ART is to reduce the viral load in the blood to undetectable levels. By doing so, ART helps to slow the progression of HIV infection, improve immune function, and reduce the risk of transmitting the virus to others.
D. can cure acute HIV/AIDS infections:
This statement is incorrect. While antiretroviral therapy (ART) is highly effective in controlling HIV infection and preventing progression to AIDS, it does not cure acute HIV/AIDS infections. HIV remains a chronic condition that requires lifelong management with ART.
During a routine health check-up, a young adult woman asks the nurse about ways to prevent endometrial cancer. Which actions would the nurse most likely include? Select all that apply.
Explanation
A. Engaging in daily exercise:
Regular physical activity has been associated with a reduced risk of endometrial cancer. Exercise helps maintain a healthy weight and may help regulate hormone levels, which can contribute to a lower risk of developing endometrial cancer.
B. Eating a high-fat diet:
Consuming a high-fat diet may increase the risk of endometrial cancer. High-fat diets have been linked to obesity, which in turn is a risk factor for endometrial cancer. Additionally, high-fat diets may alter hormone levels in the body, potentially affecting the development of endometrial cancer.
C. Becoming pregnant:
Pregnancy and childbirth can have a protective effect against endometrial cancer. During pregnancy, hormonal changes and the cessation of menstrual cycles may reduce the exposure of the endometrium to estrogen, potentially decreasing the risk of developing endometrial cancer.
D. Using estrogen contraceptives:
Estrogen-containing contraceptives, such as birth control pills, patches, or hormonal intrauterine devices (IUDs), have been associated with a higher risk of endometrial cancer, especially if used for extended periods. Estrogen alone, without the balancing effect of progesterone, can stimulate the growth of the endometrium and increase the risk of cancer.
E. Having regular pelvic exams:
Regular pelvic exams, which may include a Pap smear and/or endometrial biopsy, can help detect abnormalities in the endometrium at an early stage. Early detection can lead to timely intervention and treatment, potentially reducing the risk of advanced endometrial cancer.
A client who is HIV-positive is in her second trimester and remains asymptomatic. She voices concern about her newborn's risk for the infection. Which statement by the nurse would be most appropriate?
Explanation
A. "You'll probably have a cesarean birth to prevent exposing your newborn."
This statement suggests a specific intervention without addressing the broader context of HIV management during pregnancy. While a cesarean birth may be recommended in certain cases to reduce the risk of vertical transmission of HIV, it is not the only or primary measure taken. Antiretroviral therapy (ART) is typically the mainstay of treatment during pregnancy to suppress viral load and reduce transmission risk.
B. "Antiretroviral medications are available to help reduce the risk of transmission."
This response provides accurate information about the use of antiretroviral medications during pregnancy to reduce the risk of mother-to-child transmission of HIV. ART is a critical component of HIV management in pregnant women and has been shown to significantly decrease the risk of vertical transmission when used appropriately.
C. "Wait until after the infant is born, and then something can be done."
This statement is not appropriate because it suggests delaying action until after the infant is born, which may increase the risk of HIV transmission during childbirth. Prompt initiation of antiretroviral therapy during pregnancy is essential to maximize the chances of preventing vertical transmission.
D. "Antibodies cross the placenta and provide immunity to the newborn."
While it is true that antibodies can cross the placenta and provide passive immunity to the newborn for certain infections, including some viral illnesses, this statement is not directly relevant to preventing HIV transmission from an HIV-positive mother to her newborn. Unlike some infections where maternal antibodies can confer protection to the infant, HIV transmission is not prevented solely by passive immunity. Instead, active measures such as antiretroviral therapy are necessary to reduce transmission risk.
During a clinical breast examination, the nurse palpates a well-defined, firm, mobile lump in a 60-year-old woman's left breast. The nurse notifies the primary care provider. What would the nurse anticipate the care provider to prescribe next?
Explanation
A. Mammogram
A mammogram is typically the next step in the diagnostic process when a breast lump is detected during a clinical breast examination. Mammography allows for further evaluation of the lump and surrounding breast tissue to determine its characteristics, such as size, shape, and density. It is an important tool for detecting breast abnormalities, including masses and calcifications, which can help in diagnosing breast cancer.
B. Hormone receptor status
While hormone receptor status testing may be part of the diagnostic workup for breast cancer, it is usually not the immediate next step after discovering a breast lump during a clinical examination. Hormone receptor status testing is typically performed after a confirmed diagnosis of breast cancer to guide treatment decisions, such as the use of hormone therapy.
C. Fine-needle aspiration
Fine-needle aspiration (FNA) may be used in conjunction with other diagnostic tests, such as mammography or ultrasound, to further evaluate a breast lump. However, it is not typically the first step in the diagnostic process, especially if a lump is found during a clinical breast examination. FNA involves using a thin needle to extract cells or fluid from the lump for examination under a microscope to determine if it is benign or malignant.
D. Genetic testing for BRCA
Genetic testing for BRCA mutations is typically not the immediate next step after finding a breast lump during a clinical examination. Genetic testing for BRCA mutations is usually recommended for individuals with a strong family history of breast or ovarian cancer or those who meet specific criteria based on personal or family history. It is not typically the initial diagnostic step in evaluating a breast lump.
A nurse is assessing a female client and suspects that the client may have endometrial polyps based on which clinical manifestation?
Explanation
A. Bleeding after intercourse
Endometrial polyps can cause bleeding after intercourse (postcoital bleeding) due to irritation or trauma to the polyps during sexual activity. This symptom occurs because the polyps protrude into the uterine cavity and are easily disturbed by movement or contact.
B. Vaginal discharge
While vaginal discharge can be a symptom of various gynecological conditions, it is not typically associated specifically with endometrial polyps. Instead, other conditions like bacterial vaginosis or vaginal infections are more commonly linked to vaginal discharge.
C. Irregular, acyclic bleeding
Endometrial polyps can cause irregular, acyclic bleeding, but this symptom is less specific compared to bleeding after intercourse. Irregular bleeding can occur due to hormonal changes, uterine fibroids, or other gynecological conditions as well.
D. Bleeding between menses
Bleeding between menstrual periods (intermenstrual bleeding) can occur with endometrial polyps, but it is not as specific a manifestation as bleeding after intercourse. Intermenstrual bleeding can also be caused by hormonal imbalances, cervical or uterine infections, or other underlying conditions.
A client is scheduled for cryosurgery to remove some abnormal tissue on the cervix. The nurse teaches the client about this treatment, explaining that the tissue will be removed by which method?
Explanation
A. Burning - This method involves using heat or a cautery device to burn away abnormal tissue. It is typically referred to as electrocautery or thermal ablation. While burning is a method used in some procedures, such as electrocautery for removing warts or lesions, it is not the technique used in cryosurgery.
B. Irradiating - This term refers to the use of radiation therapy to treat cancer or abnormal tissue growth. In irradiation, high-energy radiation beams are directed at the target area to destroy abnormal cells. It is not the method used in cryosurgery.
C. Freezing - Cryosurgery involves freezing the abnormal tissue using extremely cold temperatures, typically with the application of liquid nitrogen or another cryogen. The freezing process causes cellular destruction, leading to the removal of the abnormal tissue. Cryosurgery is commonly used in dermatology, gynecology, and other medical specialties for various conditions.
D. Cutting - Cutting involves physically removing tissue using surgical instruments such as scalpels or scissors. While cutting may be involved in some procedures to remove abnormal tissue, such as excisional biopsies, cryosurgery specifically does not involve cutting. Instead, it relies on freezing to destroy and remove the targeted tissue.
After teaching a woman who has had an evacuation for gestational trophoblastic disease (hydatidiform mole or molar pregnancy) about her condition, which statement indicates that the nurse's teaching was successful?
Explanation
A. "I won't use my birth control pills for at least a year or two." - This statement does not accurately reflect the teaching provided. After treatment for gestational trophoblastic disease, it is important for the woman to avoid pregnancy for a specified period of time to allow for monitoring and to reduce the risk of complications. However, the use of birth control pills is typically recommended to prevent pregnancy during this period.
B. "I will be sure to avoid getting pregnant for at least 1 year." - This statement demonstrates understanding of the teaching. After treatment for gestational trophoblastic disease, healthcare providers typically recommend avoiding pregnancy for at least one year. This allows for monitoring of hCG levels to ensure they return to normal and to reduce the risk of recurrence.
C. "My blood pressure will continue to be increased for about 6 more months." - This statement is not related to the teaching about gestational trophoblastic disease. Blood pressure may be affected during pregnancy, but it is not a specific concern related to treatment for gestational trophoblastic disease.
D. "My intake of iron will have to be closely monitored for 6 months." - This statement is not directly related to the teaching about gestational trophoblastic disease. While monitoring of iron levels may be important for overall health, it is not a specific recommendation related to treatment for this condition.
A woman with breast cancer is undergoing chemotherapy. Which side effect would the nurse interpret as being most serious?
Explanation
A. Fatigue - Fatigue is a common side effect of chemotherapy and can significantly impact a patient's quality of life. While it can be debilitating and affect daily activities, it is not typically considered as serious as myelosuppression. Fatigue usually improves over time after completion of chemotherapy treatment.
B. Hair loss - Hair loss, or alopecia, is another common side effect of chemotherapy. It can be distressing for many patients, but it is generally not considered medically serious. Hair typically grows back after the completion of chemotherapy treatment.
C. Vomiting - Nausea and vomiting are common side effects of chemotherapy, known as chemotherapy-induced nausea and vomiting (CINV). While they can cause discomfort and affect a patient's well-being, they are usually manageable with antiemetic medications. In severe cases, dehydration and electrolyte imbalances may occur, but they are generally reversible and not as serious as myelosuppression.
D. Myelosuppression - Myelosuppression, also known as bone marrow suppression, is a serious side effect of chemotherapy. It can lead to a decrease in the production of blood cells (white blood cells, red blood cells, and platelets) by the bone marrow. This can increase the risk of infections, anemia, and bleeding, which can be life-threatening if not managed promptly. Myelosuppression requires close monitoring and may necessitate treatment adjustments or supportive care measures to prevent complications.
A nurse is listening to a client who is a victim of intimate partner violence. The client is describing how events would unfold with the partner. The nurse interprets the client's statements and identifies which action as characteristic of the second phase of the cycle of violence?
Explanation
A. The batterer is contrite and attempts to apologize for the behavior. - This action is more characteristic of the "honeymoon" phase, which follows the tension-building phase and involves the abuser expressing remorse or making promises to change.
B. The victim accepts the anger as legitimately directed at him or her. - This is not specifically characteristic of the second phase but could potentially occur as a coping mechanism or as a result of manipulation and gaslighting tactics employed by the abuser.
C. The physical battery is abrupt and unpredictable. - This description aligns more closely with the acute battering incident, which occurs in the final phase of the cycle of violence, following the tension-building phase.
D. Verbal assaults begin to escalate toward the victim. - This option reflects the tension-building phase, where verbal abuse and other forms of intimidation may escalate in frequency and intensity as the tension between the abuser and victim increases.
When developing the plan of care for a woman who has had an abdominal hysterectomy, the nurse would identify which action as contraindicated?
Explanation
A. Encouraging range-of-motion exercises: Range-of-motion exercises are generally encouraged post-hysterectomy to prevent complications such as blood clots and promote circulation. This action is appropriate and not contraindicated.
B. Ambulating the client: Ambulation is an essential aspect of postoperative care to prevent complications like atelectasis, pneumonia, and deep vein thrombosis (DVT). This action helps improve circulation and aids in the recovery process. It is appropriate and not contraindicated.
C. Applying elasticized stockings: Elasticized stockings, also known as compression stockings, are commonly used postoperatively to prevent deep vein thrombosis (DVT) by promoting blood flow in the legs. However, in the case of abdominal hysterectomy, if the incision site is below the level of the stockings, they may impede circulation to the surgical site and hinder wound healing. Therefore, this action may be contraindicated depending on the specific circumstances of the surgery and incision site.
D. Massaging the client's legs: Massaging the client's legs is generally not recommended post-hysterectomy, especially in the immediate postoperative period. Manipulating the legs could potentially disrupt healing tissues, increase the risk of bleeding, or cause discomfort to the client. Therefore, this action may be contraindicated.
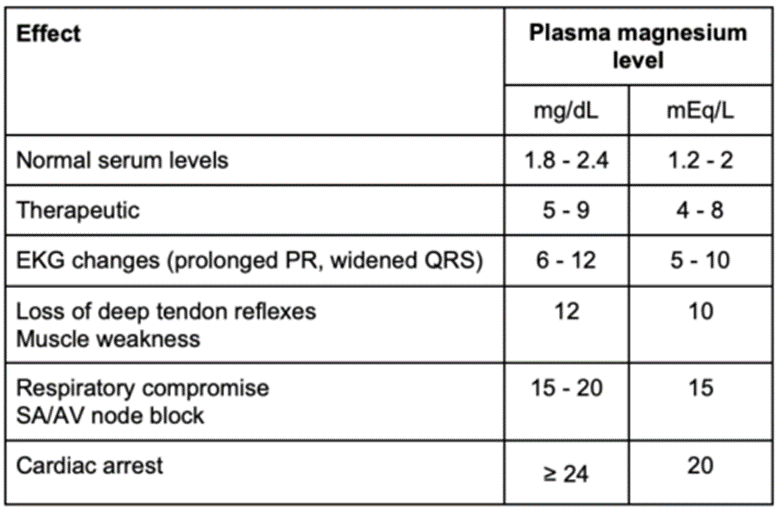
A client is diagnosed with gestational hypertension and is receiving magnesium sulfate. The nurse determines that the medication is at a therapeutic level based on which finding?
Explanation
A. Deep tendon reflexes 2+: Deep tendon reflexes are typically assessed to monitor for signs of magnesium sulfate toxicity. A normal finding of 2+ deep tendon reflexes suggests that the client is not experiencing magnesium sulfate toxicity. However, it does not specifically indicate whether the medication is at a therapeutic level.
B. Respiratory rate of 10 breaths/minute: A respiratory rate of 10 breaths/minute is below the normal range, and it could indicate respiratory depression, a potential side effect of magnesium sulfate toxicity. While this finding suggests a potential adverse reaction to the medication, it does not confirm whether the medication is at a therapeutic level.
C. Urinary output of 20 mL per hour: Adequate urinary output is essential for excreting magnesium sulfate and preventing toxicity. A urinary output of 20 mL per hour is within an acceptable range and suggests adequate renal function, which is important for maintaining therapeutic levels of the medication. However, it alone does not confirm whether the medication is at a therapeutic level.
D. Difficulty in arousing: Difficulty in arousing is a concerning sign of magnesium sulfate toxicity and suggests central nervous system depression. It indicates that the client may be experiencing an adverse reaction to the medication and that the dose may need adjustment. While this finding suggests a potential issue with medication dosing or toxicity, it does not confirm whether the medication is at a therapeutic level.
A laboratory technician arrives to draw blood for a complete blood count (CBC) for a client who had a left-sided mastectomy 8 hours ago. The client has an intravenous line with fluid infusing in her right antecubital space. The nurse enters the room and sees the technician beginning to place a tourniquet on the client's right arm. Which response by the nurse would be most appropriate?
Explanation
A. Have the technician come back later on:
This option suggests delaying the blood draw until a later time when the IV line is removed or after the infusion is completed. While this may seem like a reasonable approach to avoid interfering with the IV line, it could lead to unnecessary delays in obtaining essential laboratory test results.
B. Notify the surgeon to obtain the specimen via a cut-down procedure:
This option involves a more invasive procedure, called a cut-down, which is typically reserved for situations where peripheral venous access is challenging or impossible. It involves making an incision to expose a vein for direct cannulation. This approach is not warranted in this scenario, where obtaining blood from the opposite arm is a standard and less invasive practice.
C. Tell the technician to obtain the specimen from the client's left arm:
This option is the most appropriate response. It instructs the technician to draw blood from the client's left arm, which is free from the IV line. Drawing blood from the opposite arm minimizes the risk of complications associated with interfering with the IV infusion.
D. Stop the technician immediately:
While stopping the technician immediately may prevent them from proceeding with the incorrect approach, it lacks specific guidance on how to proceed correctly. It's essential to provide clear instructions to the technician to draw blood from the opposite arm rather than simply halting the procedure without further direction.
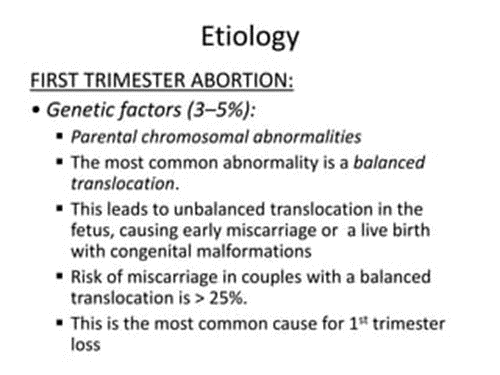
A nurse is conducting an in-service program for a group of nurses working at the women's health facility about the causes of spontaneous abortion. The nurse determines that the teaching was successful when the group identifies which condition as the most common cause of first trimester abortions?
Explanation
A. Cervical insufficiency:
Cervical insufficiency, also known as incompetent cervix, is a condition where the cervix begins to dilate and efface prematurely without contractions during the second trimester. While it can lead to second-trimester pregnancy loss, it's not typically the most common cause of first-trimester abortions.
B. Maternal disease:
While certain maternal conditions or diseases can contribute to pregnancy complications, such as pre-eclampsia or diabetes, they are not typically the most common cause of first-trimester abortions.
C. Uterine fibroids:
Uterine fibroids are noncancerous growths of the uterus that can lead to various pregnancy complications, including miscarriage. However, they are not typically the most common cause of first-trimester abortions.
D. Fetal genetic abnormalities:
This option is correct. Fetal genetic abnormalities, such as chromosomal abnormalities, are the most common cause of first-trimester spontaneous abortions, also known as miscarriages. These abnormalities can lead to developmental issues incompatible with life, resulting in spontaneous abortion.
A woman with a history of asthma comes to the clinic for evaluation for pregnancy. The woman's pregnancy test is positive. When reviewing the woman's medication therapy regimen for asthma, which medication would the nurse identify as problematic for the woman now that she is pregnant?
Explanation
A. Ipratropium:
Ipratropium is an anticholinergic bronchodilator used to relieve bronchospasm associated with asthma and chronic obstructive pulmonary disease (COPD). It works by relaxing the muscles around the airways to improve breathing. In pregnant women with asthma, ipratropium is generally considered safe for use when the benefits of controlling asthma symptoms outweigh the potential risks to the fetus. It is minimally absorbed systemically, reducing the risk of systemic side effects for both the mother and the fetus.
B. Albuterol:
Albuterol is a short-acting beta agonist (SABA) commonly used as a rescue inhaler for acute asthma symptoms. It works by relaxing the muscles in the airways, making it easier to breathe. Albuterol is considered safe for use during pregnancy, and it is often recommended as needed to relieve bronchospasm in pregnant women with asthma. Controlling asthma symptoms with albuterol can help improve maternal oxygenation and prevent complications associated with poorly controlled asthma during pregnancy.
C. Salmeterol:
Salmeterol is a long-acting beta agonist (LABA) used for the long-term control of asthma symptoms. It works similarly to albuterol but has a longer duration of action. Salmeterol is generally not recommended as the sole therapy for asthma during pregnancy due to limited safety data. While animal studies have shown adverse effects on fetal development, there are no adequate and well-controlled studies in pregnant women. Therefore, the risks versus benefits of using salmeterol during pregnancy should be carefully considered, and alternative treatments may be preferred.
D. Prednisone:
Prednisone is a corticosteroid medication used to reduce inflammation and suppress immune responses in conditions such as asthma. It is often prescribed to manage asthma exacerbations during pregnancy. While corticosteroids are generally considered safe for short-term use during pregnancy to control asthma symptoms, they may have risks associated with long-term or high-dose use, especially if used during the first trimester. Potential risks include fetal growth restriction and cleft palate. However, the benefits of controlling asthma symptoms and preventing exacerbations often outweigh the potential risks of corticosteroid use during pregnancy. Therefore, prednisone may be prescribed judiciously during pregnancy, and the dose should be tailored to the individual's needs while considering potential risks to the fetus.
When describing an episode of intimate partner violence, the victim reports attempting to calm the partner down to keep things from escalating. The nurse interprets this behavior as reflecting which phase of the cycle of violence?
Explanation
A. Battering: This phase involves the actual violent and abusive behavior, where the perpetrator inflicts harm or abuse upon the victim. It is characterized by physical, emotional, or psychological abuse.
B. Honeymoon: The honeymoon phase follows the period of violence or abuse. During this phase, the perpetrator may apologize, show remorse, and express love and affection toward the victim. The perpetrator may also promise to change their behavior and make efforts to reconcile with the victim.
C. Tension-building: The tension-building phase is characterized by increasing tension, anger, and hostility in the relationship. Minor conflicts and stressors escalate, leading to a buildup of tension between the partners. This phase often precedes the occurrence of the violent or abusive episode.
D. Reconciliation: The reconciliation phase occurs after the violent or abusive episode, during which the perpetrator attempts to reconcile with the victim. This phase may involve apologies, promises to change, and expressions of regret. However, it is important to note that the reconciliation phase may be temporary and may cycle back into the tension-building phase, leading to another episode of violence.
A pregnant woman is diagnosed with chlamydia and asks the nurse, "How will this infection affect my baby and pregnancy?" Which responses by the nurse are accurate? (Select All that Apply.)
Explanation
A. "Your membranes may rupture earlier than normal." - This statement is not directly associated with chlamydia infection during pregnancy. Premature rupture of membranes (PROM) can occur due to various factors, but chlamydia infection is not a direct cause.
B. "It will not have any effect on your pregnancy." - This statement is incorrect. Chlamydia infection during pregnancy can have implications for both the mother and the baby, so it is not accurate to say it will not have any effect.
C. "Your newborn can be infected during birth." - This is an accurate statement. Chlamydia can be transmitted from the mother to the newborn during vaginal childbirth, leading to neonatal chlamydial infection.
D. "Your newborn may have eye infections from this infection." - This is also correct. Neonatal chlamydial infection can cause conjunctivitis (eye infection) in newborns if they are exposed to the bacteria during delivery.
E. "Your newborn is protected from this infection." - This statement is incorrect. Newborns are not inherently protected from chlamydial infection if the mother is infected. Without appropriate treatment and preventive measures, the newborn can contract the infection during birth.
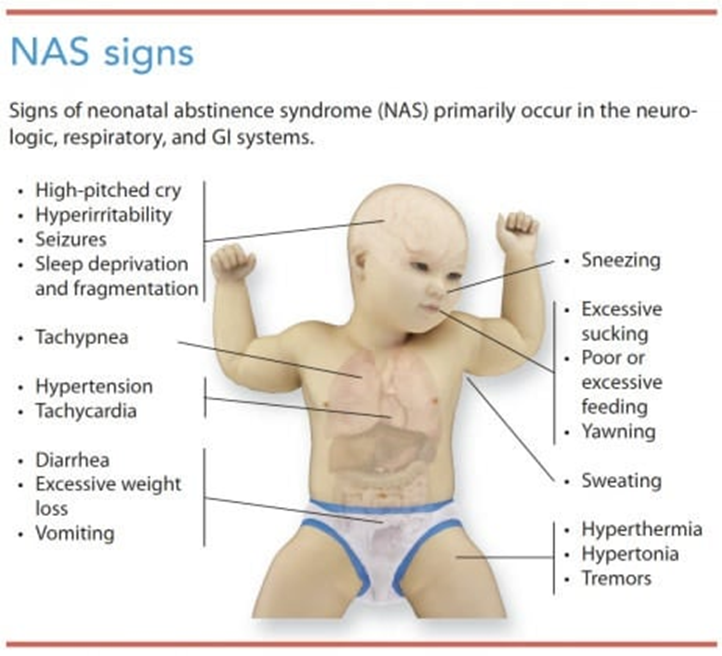
A neonate born to a mother who was abusing heroin is exhibiting signs and symptoms of withdrawal. Which signs would the nurse assess? (Select All that Apply.)
Explanation
A. Hypertonicity: Neonates experiencing withdrawal from heroin may exhibit increased muscle tone, leading to stiffness or rigidity. This is often observed as hypertonicity in their limbs or overall body.
B. Excessive sneezing: Nasal congestion and sneezing are common symptoms in neonates undergoing withdrawal. These symptoms can occur due to the irritant effects of withdrawal on the respiratory system.
C. Low whimpering cry: Infants with neonatal abstinence syndrome (NAS) may have a weak or high-pitched cry, which may sound like whimpering. This cry can be indicative of the discomfort and distress they are experiencing.
D. Overly vigorous sucking: Neonates with NAS may display exaggerated sucking behaviors, often characterized by frantic or overly vigorous sucking during feeding or when provided with a pacifier. This behavior is a manifestation of their heightened agitation and irritability.
E. Lethargy: Some neonates experiencing NAS may appear excessively drowsy, fatigued, or have decreased responsiveness. Lethargy is a common symptom associated with withdrawal from heroin or other opioids.
F. Tremors: Tremors or shaking movements, especially when the neonate is disturbed or agitated, are hallmark signs of NAS. These tremors can be mild to severe and may affect various parts of the body, such as the arms, legs, or jaw.
A pregnant woman is diagnosed with iron-deficiency anemia and is prescribed an iron supplement. After teaching her about her prescribed iron supplement, which statement indicates successful teaching?
Explanation
A. "I should avoid drinking orange juice."
- This statement is incorrect. Vitamin C, found in orange juice and other citrus fruits, can actually enhance the absorption of iron from iron supplements. Therefore, it is recommended to take iron supplements with vitamin C-rich foods or beverages to improve iron absorption. Advising the pregnant woman to avoid orange juice would be counterproductive to optimizing iron absorption.
B. "I should take my iron with milk."
- This statement is incorrect. Calcium, found in milk and dairy products, can inhibit the absorption of iron from iron supplements. Therefore, it is generally advised to avoid taking iron supplements with milk or other calcium-rich foods or beverages. Instead, iron supplements should be taken with water or vitamin C-rich foods or beverages to enhance iron absorption.
C. "I need to eat foods high in fiber."
- While it's important to maintain a balanced diet with adequate fiber intake for overall health, this statement does not directly relate to the appropriate use of iron supplements. While dietary fiber can affect digestion and bowel movements, it does not significantly impact the absorption of iron from iron supplements. Therefore, while it's beneficial to consume a diet high in fiber for various health reasons, it is not specifically necessary in relation to iron supplementation.
D. "I'll call the primary care provider if my stool is black and tarry."
- This statement is correct and indicates successful teaching. Black, tarry stools can indicate the presence of gastrointestinal bleeding, which can occur as a side effect of iron supplementation. By instructing the pregnant woman to contact her primary care provider if she experiences black, tarry stools, she demonstrates understanding of a potential adverse effect of iron supplementation and knows to seek appropriate medical attention if necessary.
Sign Up or Login to view all the 49 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

