Ati nurse 142 final
Total Questions : 45
Showing 25 questions, Sign in for moreThe nurse is caring for two clients who both are in pain due to sickle cell anemia. One of the clients rates the pain as a 7 out of 10 (0 is no pain and 10 is the worst pain possible). This client is moving around easily and is eating well, but has asked for pain medication. Which action by the nurse is most appropriate?
Explanation
Pain is a subjective experience, and the client's report of pain should be respected and addressed promptly. If the pain medication is ordered and it has been longer than the ordered interval, the nurse should administer the medication as prescribed. In general, withholding pain medication for a client in pain is not an appropriate action.
Administering half the ordered dose of pain medication without a healthcare provider's order is also not appropriate. The nurse should follow the healthcare provider's orders for pain medication administration and titration.
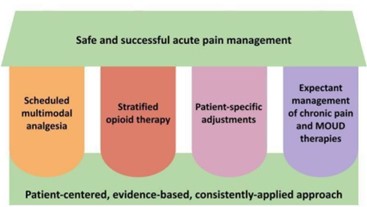
It's also not appropriate to assume that the client is faking pain without adequate assessment and evidence to support such a claim. The nurse should perform a thorough pain assessment, including the location, intensity, and quality of the pain, and consider non-pharmacological interventions to help manage the pain.
The nurse is assessing the patient's lips and notes a bluish tinge. This finding would indicate that the patient may be experiencing which problem?
Explanation
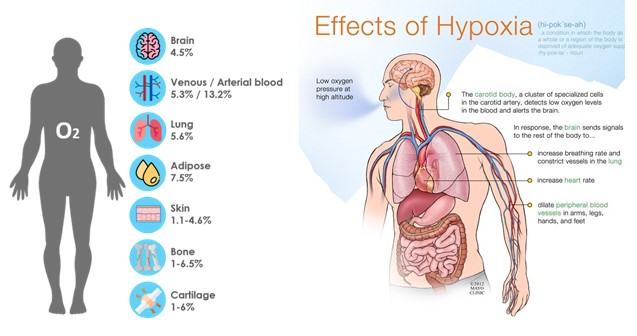
Hypoxia is a medical condition characterized by a lack of oxygen in the body's tissues, which can occur due to a variety of reasons, such as respiratory failure, cardiac arrest, or other serious medical conditions. Cyanosis occurs when the oxygen saturation level in the blood falls below 85%, which causes a bluish color to appear on the skin, especially on the lips and fingertips. Therefore, if a nurse observes cyanosis in a patient's lips, it is a significant sign of hypoxia, and the patient requires immediate medical attention.
When assessing the abdomen, the nurse would expect to auscultate which sounds?
Explanation
When assessing the abdomen, the nurse would expect to auscultate bowel sounds, which are the sounds made by the movement of gas and fluid through the intestines. The normal bowel sounds are characterized as high-pitched, gurgling, and occurring at a rate of 5-30 sounds per minute.
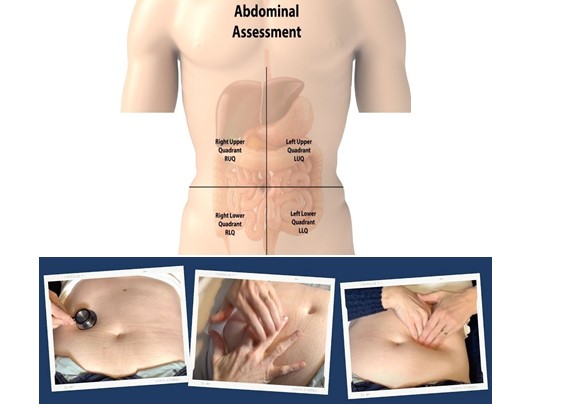
Bruits are abnormal sounds indicating turbulent blood flow and are usually assessed in other areas of the body, such as the epigastric and renal arteries, as well as in the aorta.
Friction rubs are also abnormal sounds, but they are typically heard during auscultation of the heart and lungs.
Low-pitched sonorous sounds are not typical sounds that are expected to be heard during an abdominal assessment
The nurse is performing a nutritional assessment. Which of the following would be considered objective data?
Explanation
Objective data are measurable and observable findings that can be obtained through physical examination, laboratory tests, or other diagnostic procedures.
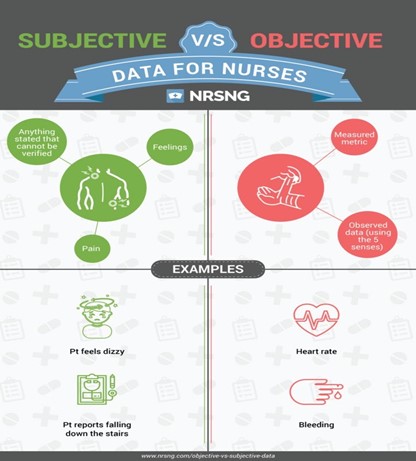
Option A is subjective data because it is information reported by the patient and may not be entirely accurate. Option Bis also subjective data because it is the patient's perception of their weight loss, which may not be an accurate reflection of actual weight loss.
Option Dis also subjective data because it relies on the patient's self-report of their alcohol intake, which may not be entirely accurate.
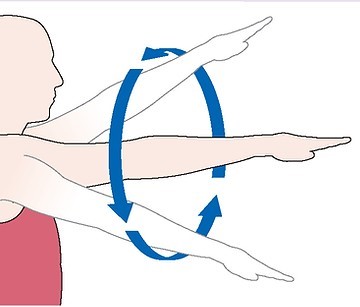
The nurse is assessing the patient's range of motion. The nurse asks the patient to circumduct his arms. When the patient asks what this means, the nurse explains:
Explanation
Circumduction is a movement that involves the circular rotation of a limb, such as an arm or leg, around a fixed point. When assessing the patient's range of motion, the nurse may ask the patient to perform circumduction of their arms to evaluate their ability to move their arms in a circular motion.
When assessing the anus, the nurse should inspect for: (Select all that apply)
Explanation
Prostate enlargement is not directly assessed through an anal examination.

The nurse is teaching the patient about different stages of sleep. The nurse knows that REM sleep includes which one of the following?
Explanation
REM (Rapid Eye Movement) sleep is a stage of sleep that is part of the sleep cycle, which also includes non-REM (NREM) sleep. Dreaming occurs during REM sleep, and it usually composes about 20-25% of total sleep time in adults. NREM sleep, on the other hand, makes up the largest amount of total sleep time, typically about 75-80%. Both REM and NREM sleep are important for restorative sleep, but each plays a different role in physiological and cognitive functioning.
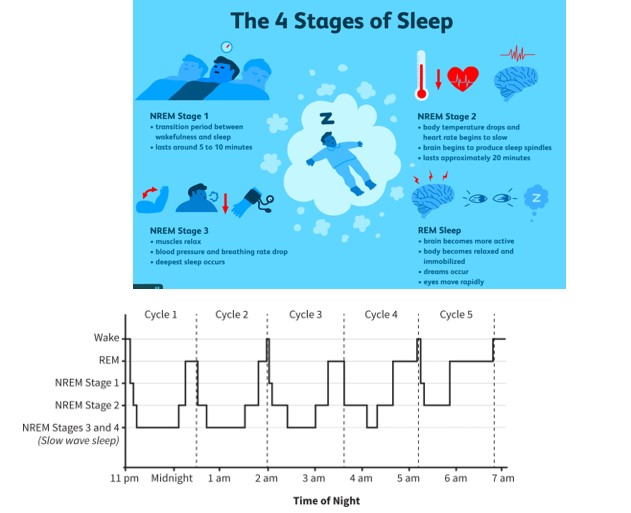
The nurse is assessing the patients sleep habits. Which of the patients responses indicate a need for the nurse to provide teaching?
Explanation
Napping during the day can interfere with a person's ability to sleep at night, especially if it is done for long periods or close to bedtime. The nurse can provide education on proper sleep hygiene and recommend ways to establish a consistent sleep schedule that promotes restful sleep, such as avoiding caffeine and alcohol, practicing relaxation techniques, and limiting exposure to electronic devices before bedtime.
In the SBAR reporting system, which of the following would be an example of a recommendation?
Explanation
The SBAR (Situation, Background, Assessment, Recommendation) system is a standardized way of communicating critical information between healthcare professionals, particularly during patient handoffs or when escalating a concern.
The recommendation component is where the healthcare professional providing the report suggests a course of action or plan for the patient based on the situation, background, and assessment. For example, a recommendation might be, "I recommend increasing Mr. Smith's pain medication to manage his discomfort," or "I recommend a consult with the nutritionist to address Mrs. Brown's malnutrition."

Of the options provided, (a) provides the situation, (c) provides the assessment, and (d) provides a specific finding from the assessment. Option (b) is a specific recommendation or plan.
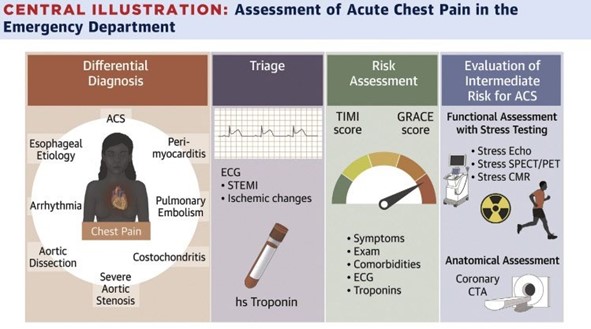
A patient is admitted to the floor with a diagnosis of chest pain. Which of the following would be a priority for the assessment?
Explanation
When a patient is admitted with a complaint of chest pain, the priority assessment would be to determine whether the patient is experiencing an acute cardiac event, such as a heart attack. This would involve a comprehensive assessment that includes obtaining the patient's medical history, vital signs (blood pressure, heart rate, respiratory rate, oxygen saturation), performing a physical exam, and obtaining an electrocardiogram (ECG).
Other important factors to assess include the location and nature of the pain, any associated symptoms (such as shortness of breath or diaphoresis), the patient's current medications and medical history (including any history of heart disease or risk factors), and any recent procedures or interventions that may have led to the current presentation.
Prompt assessment and intervention are crucial in managing a patient with chest pain, as timely treatment can help to minimize damage to the heart muscle and prevent further complications. Therefore, any signs of an acute cardiac event should be immediately reported to the healthcare provider in charge, and appropriate interventions should be initiated promptly.
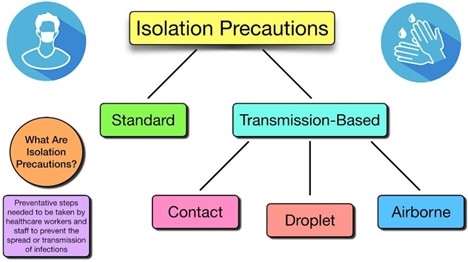
The nurse should utilize what type of precaution when palpating the lips in a healthy adult?
Explanation
Standard precautions refer to the basic infection prevention measures that should be taken with all patients, regardless of their known or suspected infection status. This includes hand hygiene, the use of personal protective equipment (such as gloves), and the proper handling and disposal of contaminated items.
If there is a concern for an infection, additional precautions may be necessary based on the suspected or confirmed pathogen. In such cases, the nurse should follow transmission-based precautions, which are specific measures designed to prevent the spread of certain types of infections. For example, if there is a concern for a respiratory infection such as influenza, the nurse may need to use droplet precautions, which would include wearing a mask in addition to standard precautions.
It's important for the nurse to assess the patient's medical history and current condition to determine what precautions are necessary. The nurse should also be aware of and follow the infection control policies and procedures of their healthcare facility.
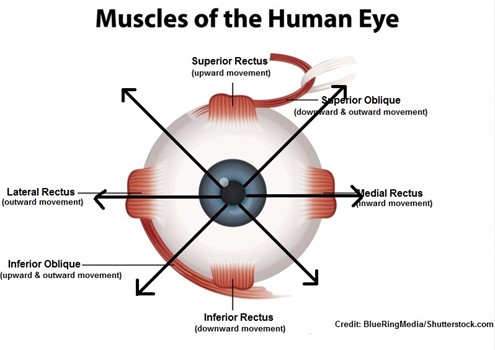
The nurse is assessing the 6 stages of cardinal gaze. This test assesses:
Explanation
The nurse is assessing the 6 stages of the cardinal gaze to evaluate the function of the cranial nerves III, IV, and VI for ocular motor movements, which control eye movement and positioning.
Cranial nerve III controls the superior rectus, inferior rectus, and medial rectus muscles, which move the eye up, down, and inward, respectively. Cranial nerve IV controls the superior oblique muscle, which moves the eye downward and laterally. Cranial nerve VI controls the lateral rectus muscle, which moves the eye outward.
Therefore, the nurse will observe the patient's ability to move their eyes smoothly in each of the six cardinal positions of gaze and note any abnormalities that may indicate dysfunction of these cranial nerves. This test is used to diagnose conditions such as strabismus, nystagmus, and palsy of the ocular motor nerves.
Cranial nerve II, on the other hand, is responsible for visual acuity, not eye movement, and is tested separately using a visual acuity chart or other vision tests.
The nurse is conducting a psychosocial assessment. Which of the following would be included in this assessment? (Select all that apply)
Explanation
The Mini-Mental Status Exam assesses cognitive function, which is often included in the psychosocial assessment, and the Activities of Daily Living Tool assesses the patient's ability to perform daily tasks, which is also important to understand the patient's level of functioning.
Some of the factors that negatively affect nutrition in the older adult include which of the following? (Select all that apply)
Explanation
A. Low economic status: This can limit their access to healthy and nutritious foods.
B. Self-care deficits that may hurt their ability to eat, prepare food, or secure food: This can include physical or cognitive impairments that make it difficult for them to shop, cook or feed themselves.
D. Dental problems: These can affect their ability to chew and digest food properly.
The patient reports an inability to taste. What is the most appropriate action for the nurse to take?
Explanation
The sense of taste is primarily mediated by the facial nerve (cranial nerve VII) and the glossopharyngeal nerve (cranial nerve IX). However, testing the function of specific cranial nerves such as the hypoglossal nerve (cranial nerve XII) or cranial nerve XI (11) is not directly related to evaluating the patient's ability to taste. Therefore, options a, b, and c would not be the most appropriate actions for the nurse to take in this scenario.

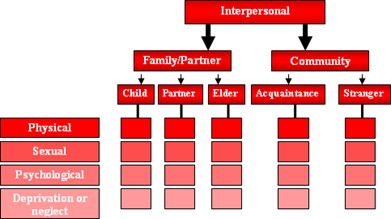
Child maltreatment, sibling violence, bullying, elder abuse, hate crimes and war/combat violence are types of?
Explanation
Human/interpersonal violence refers to violence that occurs between individuals, including physical, sexual, and psychological harm. It can occur in various forms and settings, including the examples you mentioned such as child maltreatment, sibling violence, bullying, elder abuse, hate crimes, and war/combat violence. These forms of violence can have serious and long-lasting consequences for the victims, their families, and society.
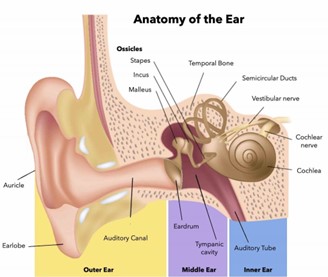
The nurse is assessing the patient's ear. The correct procedure for straightening the ear canal of an adult is to pull the pinna…
Explanation
The correct procedure for straightening the ear canal of an adult is to gently pull the auricle (the cartilage portion of the outer ear) upward and backward.
It's important to note that the technique of pulling the pinna down and back is typically used for children under the age of 3, as their ear anatomy is different from that of adults. However, for adults, pulling the pinna down and back can close off the ear canal and make it more difficult to see inside. Therefore, it's important to use the correct technique based on the patient's age and anatomy.
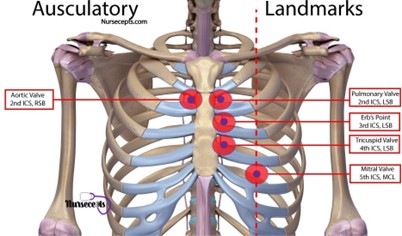
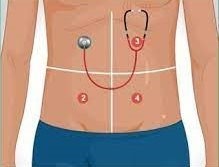
The nurse would use which of the following skills first when examining the cardiovascular system of a patient?
Explanation
The nurse would use the skill of "inspection" first when examining the cardiovascular system of a patient. The inspection involves observing the patient's physical appearance, skin color, and breathing pattern. After inspection, the nurse would move on to palpation, percussion, and auscultation.
Palpation involves feeling for pulses and areas of tenderness, while percussion involves tapping the chest to assess the density of underlying tissues. Auscultation involves listening to heart sounds using a stethoscope.
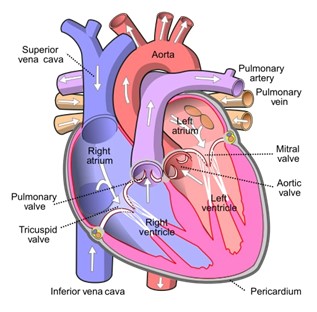
When assessing the heart, the nurse inspects and palpitates which of the following?
Explanation
When assessing the heart, the nurse will inspect and palpate the precordium, which is the area of the chest overlying the heart, and the PMI (point of maximal impulse), which is the point on the chest where the heartbeat is the strongest. These assessments allow the nurse to gather information about the size, shape, and location of the heart and to detect any abnormalities in the heartbeat or rhythm. The peritoneum is a membrane lining the abdominal cavity and has no relevance in the assessment of the heart. The tricuspid area and left sternal border are areas of the chest that may be auscultated to assess heart sounds but are not palpated during a heart assessment.
A 70-year-old male complains of ringing in the ears. The nurse describes this as:
Explanation
The nurse would describe this as tinnitus, which is a sensation of hearing sound when no external sound is present. Tinnitus is commonly described as ringing in the ears, but can also be perceived as buzzing, humming, hissing, or other sounds. Tinnitus can be caused by a variety of factors, including age-related hearing loss, exposure to loud noises, ear infections, certain medications, and underlying medical conditions such as high blood pressure, thyroid disorders, or head and neck injuries. It is important for the patient to see a healthcare provider to determine the underlying cause and appropriate treatment.
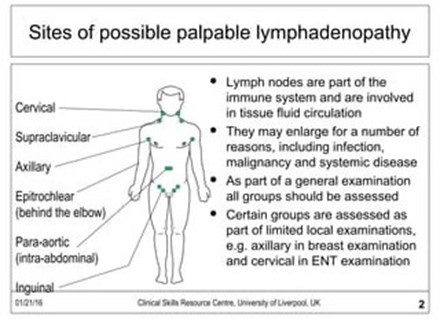
When assessing the lymph nodes, the nurse should: (select all that apply)
Explanation
Assessing unilaterally is not recommended as it may lead to missing important findings on one side.
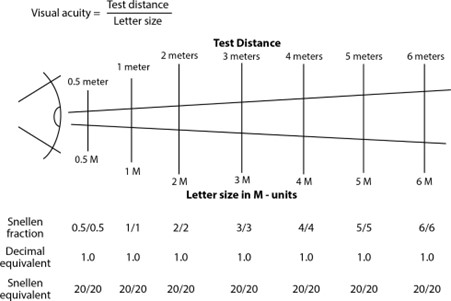
The nurse is performing a focused interview and eye assessment on a client. Which assessment findings indicate the client is experiencing a vision problem? (Select all that apply)
Explanation
A. Dilated pupils in response to dimmed lights are a normal response and not an indication of a
vision problem.
B. Pupils that remain dilated during an accommodation test indicate that the client may have an
issue with their autonomic nervous system and is not able to adjust their pupil size appropriately.
C. Far vision acuity of 20/20 bilaterally indicates normal vision.
D. A symmetrical pupillary light reflex response is a normal finding and not an indication of a vision
problem.
E. Frowning and squinting while reading the Snellen chart may indicate that the client is having difficulty seeing the letters clearly and may have a vision problem.
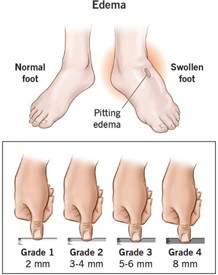
The nurse is checking for edema in the lower extremities of a patient with Congestive heart failure. The nurse will do which of the following when checking for edema. (Select all that apply)
Explanation
When checking for edema in the lower extremities of a patient with Congestive heart failure, the nurse will grade the edema on a scale of +1 to +4 and press the skin over the tibia. Plantar flexing the feet is not necessary for assessing edema in the lower extremities, and checking only one limb is not sufficient as edema may occur in both legs.
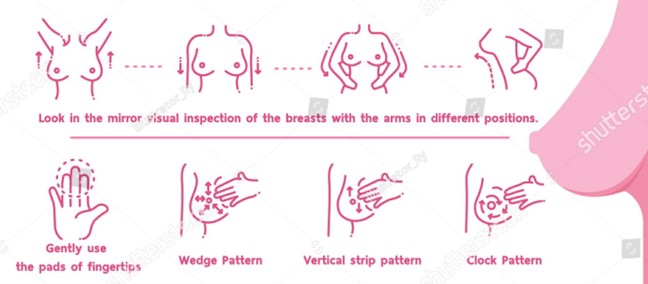
When assessing the breast, the nurse would teach the patient to palpate which of the following areas?
Explanation
The nurses would teach the patient to palpate all four quadrants of the breast, including the upper outer quadrant, lower inner quadrant, and upper inner quadrant, as well as the tail of Spence, which is the extension of breast tissue into the axilla (armpit). It's important for the patient to be familiar with their own breast tissue and report any changes or abnormalities to their healthcare provider.
The nurse auscultates the client’s abdomen for 1 minute and does not hear any bowel sounds. What should the nurse do next?
Explanation
The appropriate next step would be to auscultate for another 4 minutes. The absence of bowel sounds for one minute does not necessarily indicate a surgical emergency, as bowel sounds may be affected by various factors such as the client's diet, medications, and level of activity. Listening for another minute may not provide enough information to make an accurate assessment, so it is recommended to listen for a longer period. If after the additional 4 minutes, there are still no bowel sounds heard, the nurse should notify the physician to further evaluate the client. Listening posteriorly may also provide additional information, but it should be done after the nurse has completed listening to all four quadrants of the abdomen anteriorly.
Sign Up or Login to view all the 45 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

