ATI Paediatric Final Exam 2
Total Questions : 48
Showing 25 questions, Sign in for moreA nurse is reviewing data for four children. Which of the following children should the nurse assess first?
Explanation
A. Elevated temperature in a toddler with roseola is generally self-limiting and not immediately life-threatening.
B. A urine specific gravity of 1.016 in a 7-year-old with diabetes insipidus indicates a dilute urine concentration and is not an acute priority.
C. Sickle cell anemia can lead to vaso-occlusive crises, and severe chest pain could suggest a potential life-threatening complication such as acute chest syndrome. This requires immediate attention.
D. A PCO2 level of 37 mm Hg in a 4-year-old with asthma, while indicating respiratory distress, may not be as urgently life-threatening as severe chest pain in a child with sickle cell anemia.
A nurse is caring for a newborn whose mother voices concerns about sudden infant death syndrome (SIDS). The nurse should include which of the following statements in a discussion with the mother?
Explanation
A. Sleep apnea is different from SIDS; SIDS is a sudden, unexplained death during sleep in otherwise healthy infants.
B. SIDS rates have actually been decreasing due to public health campaigns promoting safe sleep practices.
C. There is no direct correlation between SIDS and diphtheria, tetanus, and pertussis vaccines.
SIDS is a multifactorial event, and vaccines have not been shown to cause it.
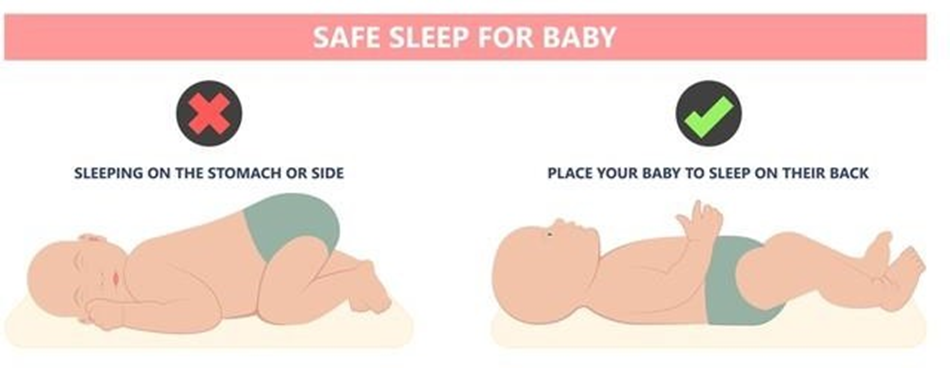
D. Placing infants on their back to sleep is a key recommendation for reducing the risk of SIDS, as per safe sleep guidelines endorsed by healthcare organizations.
A nurse is caring for an 8-month-old infant who screams when the parent leaves the room. The parent begins to cry and says, “I don’t understand why my child is so upset. I’ve never seen my child act this way around others before.” Which of the following statements should the nurse make?
Explanation
A. Separation anxiety is a normal developmental milestone that typically peaks around 8 months of age. It is a sign of healthy attachment and is expected during this stage of infancy.
B. While overstimulation can cause distress in some children, the scenario presented is more indicative of separation anxiety.
C. Overexposure to caregivers is not a recognized cause of the described behavior. Instead, it is a manifestation of the child's attachment to the primary caregiver.
D. The behavior described is more consistent with separation anxiety than illness. Illness-related distress would likely involve other signs and symptoms.
A nurse is assessing a child who is postoperative following a tonsillectomy. Which of the following findings is a manifestation of hemorrhage?
Explanation
A. Poor fluid intake may be a concern postoperatively, but it is not a specific manifestation of hemorrhage.
B. Increased pain is expected after a tonsillectomy, especially in the immediate postoperative period, but it is not a specific sign of hemorrhage.
C. Drooling is a key sign of hemorrhage after a tonsillectomy. Blood accumulating in the mouth can cause increased saliva production, leading to drooling.
D. Frequent swallowing may be seen with postoperative discomfort but is not as specific a sign of hemorrhage as drooling. Drooling indicates that blood is pooling in the oral cavity.
A nurse is planning care for a child who has mumps. Which of the following instructions should the nurse include in the plan?
Explanation
A. Standard precautions are used for all patients and are not specific to the transmission of mumps.
B. Contact precautions are typically used for conditions with skin-to-skin transmission or if the child has draining lesions. Mumps primarily spreads through respiratory droplets.
C. Mumps is transmitted via respiratory droplets, so droplet precautions, including wearing a mask, are appropriate.
D. Airborne precautions are not necessary for mumps. Airborne precautions are reserved for conditions with smaller particle transmission (e.g., tuberculosis).
A nurse in a pediatric clinic is caring for a child who has iron deficiency anemia and a new prescription for ferrous sulfate tablets. Which of the following instructions should the nurse provide the parents regarding administration of this medication?
Explanation
A. Iron absorption is enhanced when taken on an empty stomach, but it may cause gastrointestinal upset. It is generally recommended to take iron with food to reduce these side effects.
B. Administering iron at bedtime may increase the risk of gastrointestinal upset and disrupt sleep.
C. Calcium in milk can inhibit the absorption of iron. It is not recommended to give iron with milk or other calcium-containing products.
D. Vitamin C enhances iron absorption. Giving ferrous sulfate with orange juice, which is high in vitamin C, is a suitable recommendation to improve iron absorption.

A nurse is caring for a 4-year-old child who is resistant to taking medication. Which of the following strategies should the nurse use to elicit the child's cooperation?
Explanation
A. Threatening the child with a shot may create anxiety and fear, making cooperation even more challenging.
B. Hiding medication in food without the child's knowledge can lead to mistrust and may not be safe, as the child may not consume the entire dose.
C. Telling the child that the medication is candy is a strategy that may increase the likelihood of the child taking the medication willingly. However, it is important to ensure that the child understands the importance of taking the medication and that it is not actually candy.
D. Offering a choice of taking the medication with juice or water provides some control to the child, but it may not address the resistance to taking the medication itself. The child may still refuse regardless of the choice.
A nurse in an emergency department is caring for an infant who has a 2-day history of vomiting and an elevated temperature. Which of the following should the nurse recognize as the most reliable indicator of fluid loss?
Explanation
A. Body weight is the most reliable indicator of fluid loss in an infant. Changes in weight can reflect changes in fluid balance more accurately than other parameters.
B. Blood pressure may be affected by severe dehydration, but it is not as sensitive or specific as changes in body weight.
C. Skin integrity can be affected by dehydration, but it is not as direct a measure of fluid loss as changes in body weight.
D. Respiratory rate can be influenced by various factors, including respiratory distress, and is not as specific to fluid loss as changes in body weight.
A nurse is caring for an 18-month-old toddler who has been hospitalized for 10 days. After the toddler's mother leaves the room, the nurse observes the toddler sitting quietly in the corner of the crib, sucking her thumb. When the nurse approaches the crib, the toddler turns away from the nurse.
The nurse should understand that these behaviors indicate which of the following developmental reactions?
Explanation
A. The described behaviors, such as sitting quietly and turning away, may suggest the toddler is seeking comfort and self-soothing, which can be indicative of developing autonomy rather than anxiety.
B. Resentment toward the mother is a less likely interpretation of these behaviors, especially considering the age of the toddler.
C. Developing autonomy is a common developmental stage around this age. Toddlers begin to explore their independence and may engage in self-soothing behaviors.
D. Regression is a return to an earlier developmental stage. The behaviors described are more consistent with the development of autonomy rather than regression.
A nurse is caring for a child who has been physically abused by a family member. Which of the following statements should the nurse say to the child?
Explanation
A. Blaming the family may increase the child's sense of guilt or shame. It's important to focus on supporting the child rather than blaming the family outright.
B. Promising not to tell anyone may compromise the child's safety. Reporting abuse is essential to protect the child.
C. Affirming that it is not the child's fault helps to alleviate potential feelings of guilt or responsibility. This statement supports the child emotionally.
D. Discussing the incident with the family directly may not be safe for the child. Reporting suspicions of abuse to the appropriate authorities is necessary.
A nurse in a PACU is admitting a client who is postoperative following a tonsillectomy.
Which of the following actions should the nurse plan to take to prevent aspiration?
Explanation
A. Suctioning the nasopharynx as needed can help maintain airway patency but does not directly prevent aspiration during the recovery period.
B. Withholding fluids until the client demonstrates a gag reflex is a standard precaution to prevent aspiration, particularly in the immediate postoperative period.
C. Chest physiotherapy is not specifically indicated for preventing aspiration in the post- tonsillectomy period.
D. Placing a bedside humidifier at the head of the client's bed is not a specific intervention for preventing aspiration after tonsillectomy. Monitoring the client's ability to swallow and the return of the gag reflex is more relevant.
A nurse is speaking with the mother of a 6-year-old child. Which of the following statements by the mother should concern the nurse?
Explanation
A. Children may display cheating behavior in board games as part of normal development and competitive play.
B. Acting bossy with friends is a common behavior in some children and is not necessarily a cause for concern.
C. Squinting to see the board may indicate a vision problem, and it is important for the child to have an eye examination to address potential visual impairments.
D. Losing front top teeth is a normal part of the developmental process as primary teeth are replaced by permanent teeth.
A nurse is caring for an 18-month-old toddler who has been hospitalized for 10 days. After the toddler's mother leaves the room, the nurse observes the toddler sitting quietly in the corner of the crib, sucking her thumb. When the nurse approaches the crib, the toddler turns away from the nurse.
The nurse should understand that these behaviors indicate which of the following developmental reactions?
Explanation
A. The described behaviors, such as sitting quietly and turning away, may suggest the toddler is seeking comfort and self-soothing, which can be indicative of developing autonomy rather than anxiety.
B. Resentment toward the mother is a less likely interpretation of these behaviors, especially considering the age of the toddler.
C. Developing autonomy is a common developmental stage around this age. Toddlers begin to explore their independence and may engage in self-soothing behaviors.
D. Regression is a return to an earlier developmental stage. The behaviors described are more consistent with the development of autonomy rather than regression.
The parent of a 4-year-old child tells a nurse that the child believes there are monsters hiding in the closet at bedtime. Which one of the following statements should the nurse make?
Explanation
A. Staying with the child until asleep may temporarily address the fear but may not help the child develop coping skills for the future.
B. Allowing the child to sleep in the parent's bed may provide comfort but may not address the fear of monsters in the long term.
C. Keeping a night light on in the child's room can provide a sense of security and help alleviate fear by making the environment less intimidating.
D. Telling the child that monsters are not real may not be effective at this age, as young children often have difficulty distinguishing between fantasy and reality. Offering reassurance and
practical solutions like a night light may be more helpful.
A nurse is assessing an adolescent who experienced blunt trauma to the abdomen. Which of the following findings is the nurse's priority?
Explanation
A. A respiratory rate of 20/min is within the normal range, and while it should be monitored, it is not the priority in this case.
B. Blood pressure is a critical indicator of perfusion and can be affected by internal bleeding or other serious injuries. A low blood pressure may suggest significant blood loss and is the priority in assessing for shock.
C. A heart rate of 72/min is within the normal range for an adolescent. While it should be monitored, it is not the immediate priority.
D. Abdominal pain is a subjective measure and, while important, may not accurately reflect the severity of internal injuries. The priority is to assess the hemodynamic stability, as indicated by blood pressure.
A nurse is reinforcing teaching about nutritional considerations with the parents of a toddler.
Which of the following statements by the parents indicates an understanding of the teaching?
Explanation
A. Giving a toddler adult vitamins may lead to excessive intake of certain nutrients and is not recommended without consulting a healthcare provider.
B. Quality of food is crucial for toddlers, as they have small stomachs. Providing nutrient-dense foods ensures that they receive essential vitamins and minerals.
C. The average daily caloric intake for a toddler is considerably less than 3,000 calories. This statement reflects a misunderstanding of a toddler's nutritional needs.
D. Toddlers typically have unpredictable appetites. While they may go through phases of increased appetite, it is not a consistent expectation. The emphasis should be on providing a balanced and nutritious diet.
A nurse is caring for a toddler who is 24 hr postoperative following a cleft palate repair.
Which of the following actions should the nurse take?
Explanation
A. Applying bilateral wrist restraints is not a standard intervention after cleft palate repair.
Restraints should be used judiciously and with clear indications to prevent injury.
B. A soft diet is appropriate after cleft palate repair to minimize trauma to the surgical site and facilitate healing.
C. Opioids for pain management may be necessary, but the type and dosage should be determined based on the toddler's individual needs and response.
D. Offering fluids through a straw is contraindicated after cleft palate repair, as it can disrupt the healing process and increase the risk of complications. Sippy cups or other appropriate utensils should be used.
A nurse is planning care for a 6-year-old child who has bacterial meningitis. Which of the following nursing interventions is unnecessary in the client's plan of care?
Explanation
A. While monitoring for increased intracranial pressure is important, measuring head circumference every shift may not be necessary unless there is a specific indication or change in the child's condition.
B. Admitting the child to a private room is necessary to reduce the risk of spreading the infection to others.
C. Placing the child in a semi-Fowler's position can help reduce intracranial pressure and promote comfort.
D. Implementing seizure precautions is important, as children with bacterial meningitis are at risk for seizures.
A nurse is admitting a child who has suspected epiglottitis. Which of the following actions should the nurse take first?
Explanation
A. Placing the child on droplet precautions is the first priority to prevent the potential spread of infection, as epiglottitis is often caused by bacterial infection.
B. While obtaining an x-ray may be part of the diagnostic process, the immediate concern is to prevent the spread of infection.
C. Administering IV fluids may be necessary, but placing the child on droplet precautions takes precedence.
D. Initiating IV antibiotics is an essential treatment for epiglottitis, but placing the child on droplet precautions is the initial step to prevent transmission to healthcare providers and other patients.
A parent of a toddler asks a nurse at a well-child visit how the child's frequent temper tantrums can best be handled. Which of the following actions should the nurse suggest to the parent?
Explanation
A. Ignoring temper tantrums may not be effective in all situations. Some toddlers may escalate their behavior if they feel ignored.
B. Explicitly telling the child that temper tantrums are not acceptable may not be as effective in managing the behavior. Toddlers may not fully understand or respond well to verbal reasoning.
C. Distracting the child with a different activity, such as playing a game, can redirect their attention and help diffuse the situation.
D. Physical restraint is not an appropriate or effective method for managing temper tantrums. It can lead to increased resistance and may cause harm to the child.
A child is admitted with a suspected diagnosis of Wilms’ tumor. The nurse should place a sign with which of the following warnings over the child’s bed?
Explanation
A. Collecting all urine may be a part of the diagnostic process, but it is not the primary warning associated with Wilms' tumor.
B. Contact precautions are not typically required for Wilms' tumor.
C. The warning "Do not palpate abdomen" is crucial because palpation can potentially disrupt the tumor and cause hemorrhage.
D. No venipuncture or blood pressure in the left arm is not a typical precaution associated with Wilms' tumor. The emphasis is on avoiding abdominal palpation to prevent trauma to the tumor.
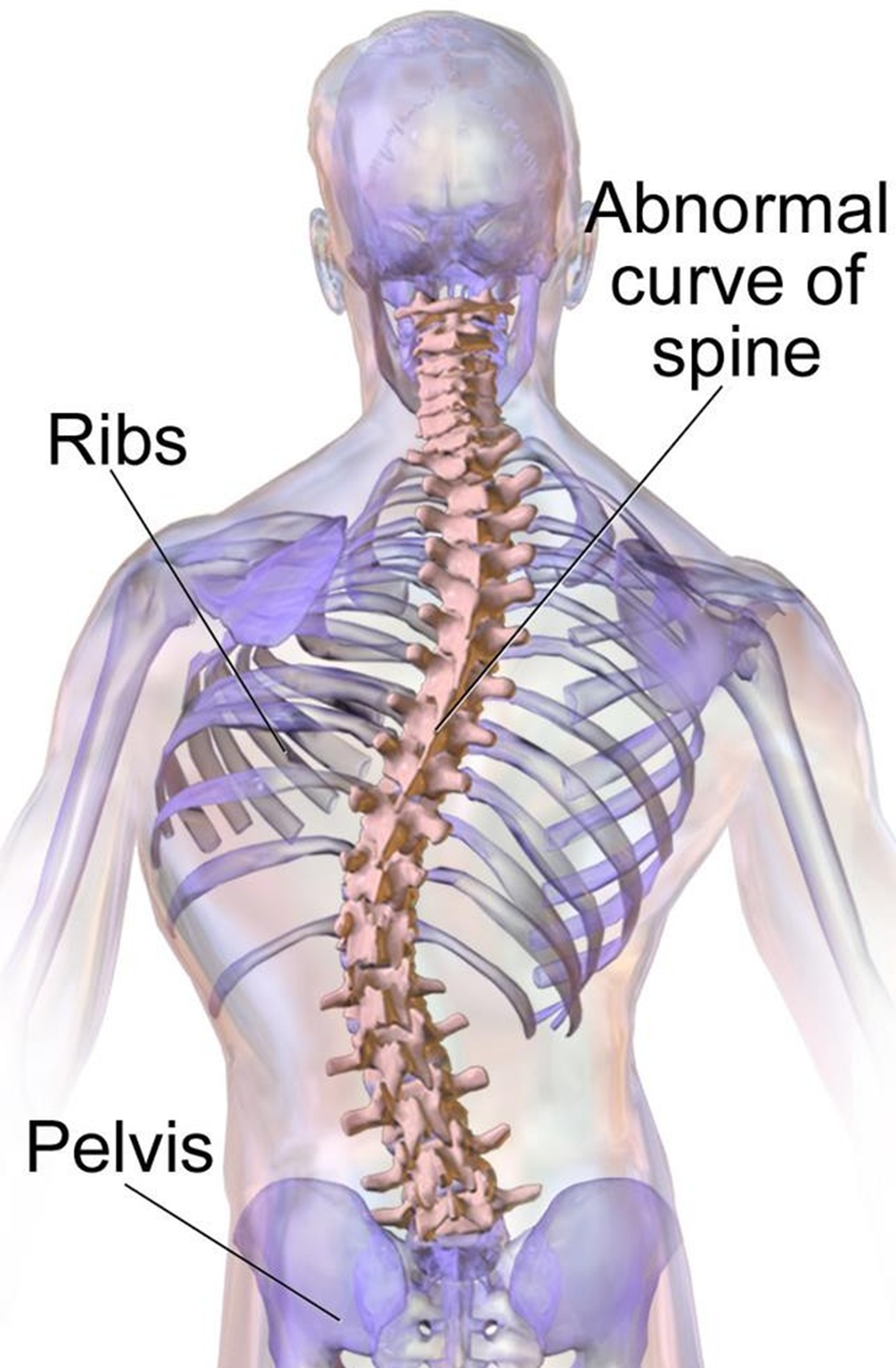
A nurse is assisting with a routine physical examination of an adolescent. The provider observes a lateral curvature of the spine. The nurse should expect the provider to document which of the following disorders?
Explanation
A. Scoliosis is a lateral curvature of the spine. It is commonly assessed during routine physical examinations, especially in adolescents.
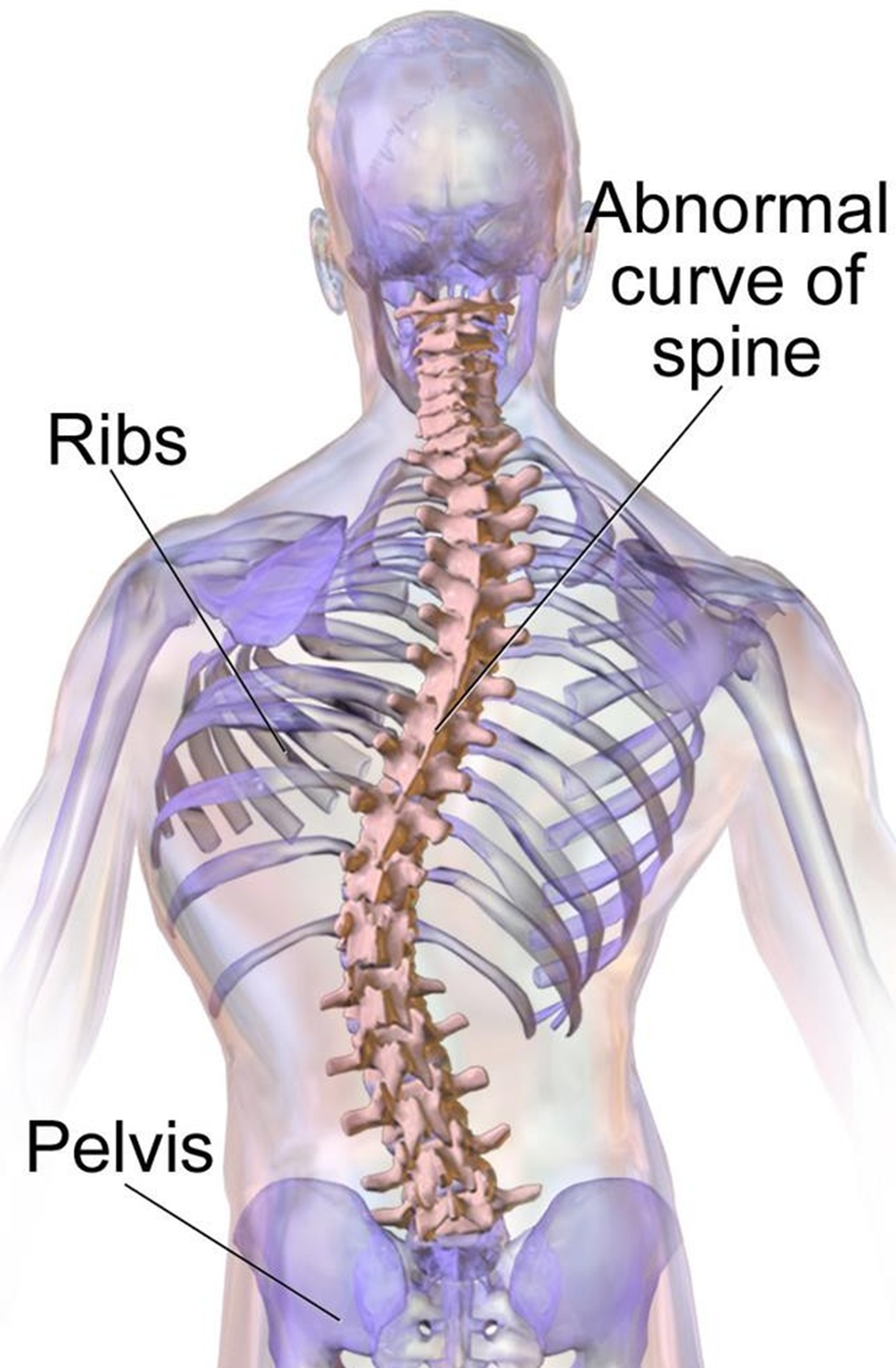
B. Lordosis refers to an exaggerated inward curvature of the spine, typically in the lumbar region.
C. Torticollis is a condition characterized by a tilt of the head to one side due to the shortening of muscles on one side of the neck.
D. Kyphosis is an exaggerated outward curvature of the thoracic spine, leading to a rounded upper back.
A nurse is caring for a 4-year-old child who has a new diagnosis of diabetes mellitus and is distressed after an insulin injection. Which of the following play activities should the nurse recognize is therapeutic in helping the child deal with the injection?
Explanation
A. While play in the playroom is generally beneficial, providing a specific activity related to the child's distress from the insulin injection is more targeted.
B. Offering a needleless syringe and a doll allows the child to engage in play that mimics the experience of receiving an injection. This can help the child gain a sense of control and understanding of the procedure.
C. A video game may serve as a distraction, but it may not specifically address the child's distress related to the insulin injection.
D. A storybook about a child who has diabetes may provide education and reassurance, but it may not actively engage the child in a therapeutic play activity related to the injection experience.
A nurse is caring for a child who has acute gastroenteritis but is able to tolerate oral fluids.
The nurse should anticipate providing which of the following types of fluid?
Explanation
A. Water alone may not provide the necessary electrolytes and sugars to help rehydrate the child effectively.
B. Oral rehydration solution is specifically designed to replace fluids and electrolytes lost during episodes of diarrhea or vomiting. It is the recommended choice for managing dehydration due to acute gastroenteritis.
C. Broth may provide some fluid but lacks the optimal balance of electrolytes and sugars found in oral rehydration solutions.
D. Diluted apple juice may not be as effective as an oral rehydration solution in replacing electrolytes and preventing dehydration.
A nurse is caring for a 2-year-old child who is hospitalized and throws a tantrum when his parent leaves. Which of the following toys should the nurse provide to alleviate the child’s stress?
Explanation
A. A toy hammer and pounding board may not be appropriate in a hospital setting and might not effectively address the child's emotional distress.
B. A stuffed animal can provide comfort and a sense of security for a young child experiencing separation anxiety. It serves as a transitional object, helping the child cope with the absence of the parent.
C. A picture book about hospitals may be informative, but it might not provide the immediate comfort and distraction needed during the tantrum.
D. A set of building blocks may be more suitable for creative play but may not offer the same level of emotional comfort as a stuffed animal in the given situation.
Sign Up or Login to view all the 48 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

