ATI Paediatrics Exam 1
Total Questions : 53
Showing 25 questions, Sign in for moreWhich of the following manifestations can the nurse expect in a client with upper motor neuron deficit related to a spinal cord injury?
Explanation
Choice A Rationale: Leakage is not typically associated with upper motor neuron deficits related to a spinal cord injury.
Choice B Rationale: Anuria (absence of urine production) is not a common manifestation of upper motor neuron deficits in this context.
Choice C Rationale: A flaccid bladder and an inability to voluntarily void are more characteristic of lower motor neuron deficits. Upper motor neuron deficits often lead to spasticity and involuntary voiding.
Choice D Rationale: Spasticity and involuntary voiding are common manifestations of upper motor neuron deficits related to spinal cord injury. This is due to the loss of inhibitory control over reflexes, including the micturition reflex.
A client arrives reporting redness, warmth, and swelling after stepping on a nail one week ago. What is the nurse's priority action?
Explanation
Choice A Rationale: Cleansing the wound may be necessary, but the priority in this case is to assess for any retained foreign bodies, such as the nail, and potential structural damage, which can be done through an X-ray.
Choice B Rationale: The client's immunization history is not the priority when assessing and managing a wound like this.
Choice C Rationale: Dressing the wound may be necessary but should come after assessing for retained foreign bodies and potential structural damage.
Choice D Rationale: Requesting an X-ray is the priority action because it helps determine if the nail is still present and if there is any damage to deeper structures, such as bones or foreign body remnants.
After receiving change-of-shift report for clients on the memory unit, which patient will the nurse see first?
Explanation
Choice A Rationale: The patient who developed a new cough after eating breakfast should be seen first. This sudden change in respiratory status during or after eating suggests a potential risk of aspiration, which requires immediate assessment and intervention to prevent respiratory distress or pneumonia.
Choice B Rationale: Medication refusal, while important, is not an immediate life threatening issue compared to a new cough with the potential for aspiration.
Choice C Rationale: Although constipation can be uncomfortable, it is not an acute priority compared to a new cough that may indicate a respiratory problem.
Choice D Rationale: A stage II pressure ulcer on the coccyx, while concerning, is not an immediate priority over a potential respiratory issue that requires urgent attention.
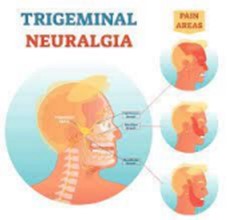
A client with a diagnosis of trigeminal neuralgia reports which of the following manifestations as significantly affecting her quality of life?
Explanation
Choice A Rationale: Lethargy is not a typical manifestation of trigeminal neuralgia.
Choice B Rationale: Pain is the hallmark symptom of trigeminal neuralgia and is known to significantly affect a person's quality of life. The pain is often severe, sudden, and recurrent.
Choice C Rationale: Social withdrawal can result from the pain and discomfort associated with trigeminal neuralgia, but it is a consequence rather than a primary manifestation.
Choice D Rationale: Poor hygiene may occur as a result of the pain and discomfort associated with trigeminal neuralgia, but it is not a primary symptom of the condition.
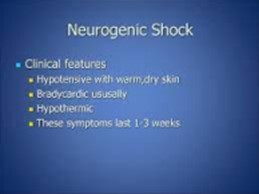
A client has sustained a T4-T5 injury and the nurse suspects he is in neurogenic shock. Which of the following manifestations are consistent with neurogenic shock? Select All that Apply
Explanation
Choice A Rationale: Hypertension is not a sign of neurogenic shock, but rather of autonomic dysreflexia, a life-threatening condition that can occur in patients with spinal cord injury above T6.
Choice B Rationale: Rapidly elevating temperature is also a sign of autonomic dysreflexia, not neurogenic shock. Neurogenic shock can cause hypothermia due to impaired thermoregulation.
Choice C Rationale: Bradycardia is a sign of neurogenic shock due to the loss of sympathetic stimulation to the heart, which normally increases the heart rate and contractility.
Choice D Rationale: Fixed and dilated pupils are a sign of brain death, not neurogenic shock. Neurogenic shock can cause miosis (constriction of the pupils) due to unopposed parasympathetic stimulation.
Choice E Rationale: Hypotension is a sign of neurogenic shock due to the vasodilation and decreased venous return caused by the loss of sympathetic tone.
A nurse is teaching the family of a client who is receiving treatment for a spinal cord injury with a halo fixation device. Which of the following statements should the nurse make?
Explanation
Choice A Rationale: The purpose of a halo fixation device is to immobilize the cervical spine and prevent movement, which is crucial for healing and preventing further spinal cord injury.
Choice B Rationale: A halo fixation device does not allow for neck movement during the healing process.
Choice C Rationale: Applying talcum powder under the vest may increase the risk of skin irritation or infection.
Choice D Rationale: Turning the screws on the device should only be done by qualified healthcare professionals, not by the family.
A 45 year old client with a history of drug and alcohol abuse is admitted to the hospital. On day 2 the client has rapidly fluctuating moods and believes the King of England is in his room. How will the nurse document these findings?
Explanation
Choice A Rationale: Documenting an overdose is premature without further assessment and evidence.
Choice B Rationale: Acute dementia is not typically diagnosed based on rapidly fluctuating moods alone, and it may not be appropriate for this situation.
Choice C Rationale: While substance abuse comorbidity may be present, it does not fully capture the client's current presentation.
Choice D Rationale: Documenting acute delirium is appropriate in this case. The client's symptoms, including rapidly fluctuating moods and delusions, are indicative of acute delirium, which can be related to substance withdrawal or other medical issues.
A nurse prepares to bathe a client with a spinal cord injury. Which of the following is the best first action?
Explanation
Choice A Rationale: Unscrewing the pins from the cervical tongs is not the best first action for bathing a client with a spinal cord injury.
Choice B Rationale: Asking the client to sit on the edge of the bed may not be appropriate or safe without proper assistance and equipment.
Choice C Rationale: The best first action is to gather supplies and at least 3 other people. Bathing a client with a spinal cord injury can be complex and may require additional assistance for safety and comfort.
Choice D Rationale: Removing the straps from the halo vest is not the first step in the bathing process and may not be necessary.
The day shift nurse at the long-term care facility learns that a patient with dementia experienced sundowning late in the afternoon on the previous two days. Which is the best action by the nurse?
Explanation
Choice A Rationale: Keeping window blinds open during the day is a non pharmacological approach to help regulate the patient's circadian rhythm and may reduce the severity of sundowning, a common phenomenon in dementia.
Choice B Rationale: Having the patient take a mid-morning nap may disrupt the patient's sleep-wake cycle and worsen sundowning.
Choice C Rationale: Providing hourly orientation to time and place may be overwhelming for the patient and not necessarily effective in addressing sundowning.
Choice D Rationale: Moving the patient to a quiet room in the afternoon may not address the underlying issue of sundowning and may not be practical in a long-term care setting.
A client who suffered partial paralysis is repositioned by the nurse every 2 hours. After placing the client in a side-lying position, what action will nurse take to prevent complications?
Explanation
Choice A Rationale: Measuring the calves for symmetry is not directly related to preventing complications after repositioning.
Choice B Rationale: Palpating the bladder is important for assessing urinary retention but is not the immediate action to prevent complications after repositioning.
Choice C Rationale: Placing a pillow between the knees and ankles is the correct action to prevent complications such as pressure ulcers and skin breakdown when a client is in a side-lying position.
Choice D Rationale: Checking the gag reflex is unrelated to repositioning and preventing complications.
After assessing a client with deficits from a spinal cord injury, the nurse identifies the client's 02 saturation is 92%. Which of the following is the best first action by the nurse?
Explanation
Choice A Rationale: Anticipating intubation is not warranted solely based on an O2 saturation of 92% and without further assessment.
Choice B Rationale: Asking the client to cough, then inhale and exhale deeply is an appropriate initial action to improve oxygenation and assess the client's respiratory status.
Choice C Rationale: Inserting an intravenous catheter is unrelated to the client's O2 saturation and would not address the immediate concern.
Choice D Rationale: Administering antihypertensives is not indicated based on the O2 saturation level, and it may not be safe without further assessment.
I client with a spinal cord injury reports hot, burning, tingling, pain that shoots down his extremities. When the client asks why this occurs, what is the nurse's best response?
Explanation
Choice A Rationale: Repositioning may be important for preventing complications, but it does not explain the pain described by the client.
Choice B Rationale: A continual inflammatory process is not typically the cause of the pain described by the client with a spinal cord injury.
Choice C Rationale: Nerve damage in the spinal cord is a common cause of neuropathic pain with these characteristics.
Choice D Rationale: Telling the client that the pain will go away in 2 weeks without further assessment or explanation is not accurate and may raise unrealistic expectations.
The nurse is caring for a client diagnosed with trigeminal neuralgia. The client asks the nurse, "Why do I have so much pain?" Which of the following responses by the nurse is most appropriate?
Explanation
Choice A Rationale: Linking the pain to nasal stuffiness is not an accurate explanation of trigeminal neuralgia.
Choice B Rationale: Hypoglycemia is not typically related to trigeminal neuralgia.
Choice C Rationale: Releasing catecholamines with infection or stress is not the primary cause of trigeminal neuralgia.
Choice D Rationale: Pain is often due to stimulation of the affected nerve by pressure and temperature. This is a more accurate and relevant explanation for trigeminal neuralgia.
After performing an assessment on a client with a spinal cord injury, which intervention will the nurse employ to prevent cardiovascular complications?
Explanation
Choice A Rationale: Sitting the client at a 90-degree angle (upright position) helps prevent orthostatic hypotension and cardiovascular complications in clients with spinal cord injuries by improving venous return and cardiac output.
Choice B Rationale: Administering 2000 liters of fluid is an inappropriate intervention, and the volume mentioned is excessive.
Choice C Rationale: Applying compression socks may help prevent deep vein thrombosis (DVT) but does not address cardiovascular complications related to sitting position.
Choice D Rationale: Maintaining blood pressure exactly at 110/80 is not a feasible or appropriate intervention.
When planning care for a client hospitalized with Guillain-Barre Syndrome, which of the following will the nurse report to the physician?
Explanation
Choice A Rationale: Reporting difficulty sleeping may be important but is not typically a critical concern in Guillain-Barre Syndrome.
Choice B Rationale: Removing the sequential compression device once a shift may require clarification or education but is not a significant medical concern.
Choice C Rationale: Hypoactive bowel sounds can indicate a potential bowel obstruction or paralytic ileus, which is a significant medical concern in clients with Guillain-Barre Syndrome and should be reported to the physician.
Choice D Rationale: A Glasgow Coma Score of 15 is within the normal range and would not typically require reporting to the physician in the context of Guillain-Barre Syndrome.
When reviewing the health history of a client, which of the following finding is consistent with a diagnosis of Bell's Palsy?
Explanation
Choice A Rationale: Being currently pregnant is a risk factor for developing Bell's Palsy.
Choice B Rationale: Thyroid disease is not a direct risk factor or consistent finding in Bell's Palsy.
Choice C Rationale: Having a seizure disorder is not directly related to Bell's Palsy.
Choice D Rationale: Current smoking is not a risk factor associated with Bell's Palsy

A nurse is offering teaching to a caregiver about urinary system complications that occur as a result of spinal cord injury. Which of the following will the nurse include in teaching?
Explanation
Choice A Rationale: The nurse will include instructions on draining the bladder with a clean intermittent catheter at appropriate intervals to prevent urinary retention and complications. This should be done every 3 to 6 hours, depending on the amount of fluid intake and output.
Choice B Rationale: Decreasing fluid intake is not typically recommended for individuals with spinal cord injuries, as adequate hydration is important.
Choice C Rationale: Observing the urine for a foul odor is relevant to monitor for urinary tract infections, but it is not a preventive measure.
Choice D Rationale: Keeping an indwelling catheter in place at all times is not typically recommended due to the increased risk of urinary tract infections and other complications.
A home health nurse is reinforcing coping strategies with the family caregiver of a client who has Alzheimer's disease. Which of the following information should the nurse include in the teaching? (Select all that apply.)
Explanation
Choice A Rationale: Understanding the expected physiological changes of Alzheimer's disease can help the caregiver better cope with the client's behaviors and needs.
Choice B Rationale: Teaching actions to reduce stress is important for both the caregiver and the client, as stress can exacerbate behavioral symptoms in Alzheimer's disease.
Choice C Rationale: Referring to available community resources can provide valuable support and assistance to both the caregiver and the client.
Choice D Rationale: Identifying a social support system is essential for the caregiver to have emotional and practical support while caring for a client with Alzheimer's disease.
Choice E Rationale: While medication administration is important, it may not be the primary focus of coping strategies for the caregiver.
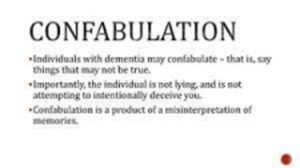
A nurse is caring for an older adult client who has dementia and handles anxiety by confabulating. The nurse should recognize which of the following as confabulation?
Explanation
Choice A Rationale: A person who makes up stories when he is unable to remember actual events is confabulating. This can be seen as a way of filling in the blanks in their memory with plausible details that may or may not have happened. For example, a person with dementia may confabulate that they had lunch with a friend yesterday, when in fact they did not see anyone.
Choice B Rationale: reminiscing about the past, which is a normal and healthy way of recalling one's life experiences and sharing them with others.
Choice C Rationale: displaying compulsive and ritualistic behaviors, which are repetitive actions that a person feels compelled to perform, often as a way of reducing anxiety or distress.
Choice D Rationale: refusing to leave home to see a provider, which is a sign of agoraphobia, a fear of being in situations where escape might be difficult or embarrassing.
A nurse is offering teaching to a caregiver about urinary system complications that occur as a result of spinal cord injury. Which of the following will the nurse include in teaching?
Explanation
Choice A Rationale: Draining the bladder with a clean intermittent catheter at appropriate intervals is an essential part of managing urinary system complications in clients with spinal cord injury to prevent urinary retention and complications.
Choice B Rationale: Decreasing fluid intake is not typically recommended for individuals with spinal cord injuries, as adequate hydration is important for overall health.
Choice C Rationale: Observing the urine for a foul odor is relevant to monitor for urinary tract infections, but it is not a preventive measure.
Choice D Rationale: Keeping an indwelling catheter in place at all times is not typically recommended due to the increased risk of urinary tract infections and other complications. Clean intermittent catheterization is often preferred.
When planning care for a client with a C3 spinal cord injury, which of the following will the nurse identify as the priority ongoing assessment?
Explanation
Choice A Rationale: Urinary output is also an important assessment in clients with a C3 spinal cord injury because it helps monitor for urinary retention and potential complications but it is not a priority compared to assessing the respiratory function of this client.
Choice B Rationale: Blood pressure is important to monitor but may not be the top priority assessment in this context.
Choice C Rationale: The nurse should prioritize counting respirations for a client with a C3 spinal cord injury, as this level of injury affects the phrenic nerve that innervates the diaphragm. The client may have difficulty breathing and require mechanical ventilation.
Choice D Rationale: Bowel sounds are important but may not be the priority assessment in this case.
A nurse is caring for an older adult client who has dementia. The client's family member asks why the provider will not prescribe a medication to calm the client down. Which of the following statements should the nurse make?
Explanation
Choice A Rationale: some medications that are used to calm down people with dementia can have serious side effects, especially for older adults. One of these side effects is an increased risk of experiencing a stroke, which can be life-threatening.
Choice B Rationale: Increased blood pressure can be a side effect of some medications used to calm patients with dementia, but it may not be the primary reason for not prescribing such medications. Furthermore, some medications can lower blood pressure, not increase it.
Choice C Rationale: Increased risk for infection is not typically a reason to avoid medications to calm dementia patients.
Choice D Rationale: is partially true because some medications can increase the risk for falls, but this is not the main reason why they are avoided.
The spouse of a 67-yr-old male patient with early stage Alzheimer's disease (AD) tells the nurse, "I am exhausted from worrying all the time. I don't know what to do." Which actions are best for the nurse to take at this time? Select All that Apply
Explanation
Choice A Rationale: Asking the spouse what she knows about dementia care options is a good starting point to assess her knowledge and provide information and resources, and empowering her to make informed decisions.
Choice B Rationale: Suggesting placement into a long-term care facility should not be the first option but can be explored if necessary, based on the client's condition and the caregiver's needs.
Choice C Rationale: Teaching the spouse about adult day care as a possible respite is a way of offering support and relief for the caregiver, who may experience stress and burnout from the constant demands of caring for a patient with AD.
Choice D Rationale: Suggesting that the spouse consult with the physician for antianxiety drugs is not helpful, as it may imply that the spouse's feelings are abnormal or that she needs medication to cope.
Choice E Rationale: Offering ideas for ways to distract or redirect the patient is not relevant to the spouse's needs, as it does not address her exhaustion and worry.
A nurse is teaching the family of an older adult client who has a new diagnosis of dementia. Which of the following statements should the nurse include in the teaching?
Explanation
Choice A Rationale: Dementia is not characterized by a sudden onset of confusion. It is a gradual and progressive condition.
Choice B Rationale: Dementia can be triggered or worsened by factors like infections, but it is not primarily characterized by a high fever or dehydration.
Choice C Rationale: An altered level of consciousness is not typically associated with dementia but may occur in acute delirium.
Choice D Rationale: The nurse should explain to the family that dementia is a chronic condition that affects the brain and causes cognitive impairment, memory loss, andbehavioral changes. The nurse should also inform the family that dementia is not caused by a single factor, but by a combination of genetic, environmental, and lifestyle factors. The nurse should emphasize that dementia is not a normal part of aging, and that it has different stages and types.
A family member arrives with a client indicating that they are concerned that the client is developing Alzheimer's disease. Which of the following items described by the family member are signs of Alzheimer's Disease? Select All that Apply
Explanation
Choice A Rationale: Forgetting names and faces, especially when previously introduced, can be a sign of memory impairment, which is common in Alzheimer's disease. Choice B Rationale: Neglecting bills and financial responsibilities is a sign of impaired executive function, which can occur in Alzheimer's disease.
Choice C Rationale: Mentioning excitement about starting a new job after retirement is a typical sign of Alzheimer's disease.
Choice D Rationale: Repeatedly forgetting that one has already read the newspaper and reading it again can be a sign of short-term memory loss, a characteristic of Alzheimer's disease.
Choice E Rationale: Placing car keys in unusual places and misplacing items like shoes in unexpected locations can be signs of disorientation and memory problems, which are common in Alzheimer's disease.
Sign Up or Login to view all the 53 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

