ATI PAEDIATRICS EXAM SIMMONS U BSN
Total Questions : 50
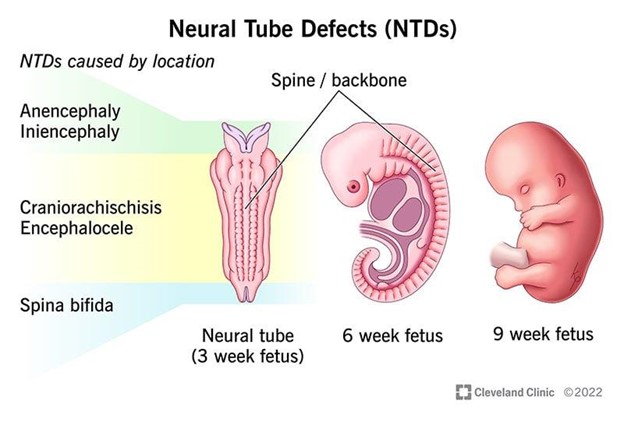
Showing 25 questions, Sign in for moreA nurse is teaching about neural tube defects to a group of females who are pregnant. Which of the following disease processes should the nurse include as an example of a neural tube defect?
Explanation
A. Spina bifida.
Explanation: Correct Choice. Spina bifida is a neural tube defect (NTD) that occurs during early fetal development when the neural tube doesn't close completely. It can result in various degrees of spinal cord and nerve damage. This is a suitable example to include when teaching about neural tube defects.
B. Hydrocephalus.
Explanation: Hydrocephalus is not a neural tube defect itself. It's a condition characterized by the accumulation of cerebrospinal fluid in the brain, leading to increased intracranial pressure. It can be caused by various factors, but it's not directly related to neural tube development.
C. Cerebral palsy.
Explanation: Cerebral palsy is a group of motor disorders caused by damage to the developing brain, usually before birth. It is not a neural tube defect. Instead, it's related to brain injury or abnormal development.
D. Muscular dystrophy.
Explanation: Muscular dystrophy is a group of genetic disorders characterized by progressive muscle weakness and degeneration. It's not related to neural tube defects. Muscular dystrophy affects muscle tissue, while neural tube defects involve improper development of the neural tube.
A nurse is providing discharge teaching to the parents of a child who has a new diagnosis of diabetes mellitus. Which of the following statements by the parents indicates an understanding of the teaching?
Explanation
A. "My son might complain of feeling shaky when he has a low blood glucose level."
Explanation: Correct Choice. Shaking or feeling shaky is a common symptom of low blood glucose levels, also known as hypoglycemia. When blood sugar drops too low, the body releases adrenaline, causing shaking or trembling. This response is indicative of an understanding of hypoglycemia symptoms.
B. "My son might have nausea and vomiting with hypoglycemia."
Explanation: Nausea and vomiting are not typical symptoms of hypoglycemia (low blood sugar). They are more commonly associated with hyperglycemia (high blood sugar) or other conditions. This statement is not accurate in the context of hypoglycemia.
C. "Sweating can occur with hyperglycemia."
Explanation: Sweating is more commonly associated with hypoglycemia (low blood sugar) rather than hyperglycemia (high blood sugar). When blood sugar levels drop too low, the body can respond with sweating as part of the adrenaline release. Sweating is not a typical symptom of hyperglycemia.
D. "The onset of low blood glucose usually occurs slowly."
Explanation: The onset of low blood glucose (hypoglycemia) can vary. It can occur suddenly, especially if the individual takes too much insulin or diabetes medication, leading to a rapid drop in blood sugar. The correct understanding is that the onset of low blood glucose can be rapid and not always slow.
A nurse is assessing an infant following a motor vehicle crash. Which of the following findings should the nurse monitor to identify increased Intracranial pressure?
Explanation
A. Brisk pupillary reaction to light.
Explanation: A brisk pupillary reaction to light is a normal response and doesn't necessarily indicate increased intracranial pressure (ICP). It's a sign that the visual pathway and cranial nerves are functioning appropriately.
B. Tachycardia.
Explanation: Tachycardia (increased heart rate) can occur for various reasons in response to trauma or distress, but it's not a direct indicator of increased intracranial pressure.
C. Increased sleeping.
Explanation: Increased sleeping alone is not a definitive sign of increased intracranial pressure. While changes in sleep patterns can occur due to brain injury, other factors need to be considered to confirm elevated ICP.
D. Depressed fontanelles.
Explanation: Correct Choice. Depressed fontanelles can be a sign of dehydration or decreased intravascular volume, which can contribute to increased intracranial pressure. A fontanelle that is sunken or depressed may indicate reduced cerebral perfusion and compensatory mechanisms to preserve fluid.
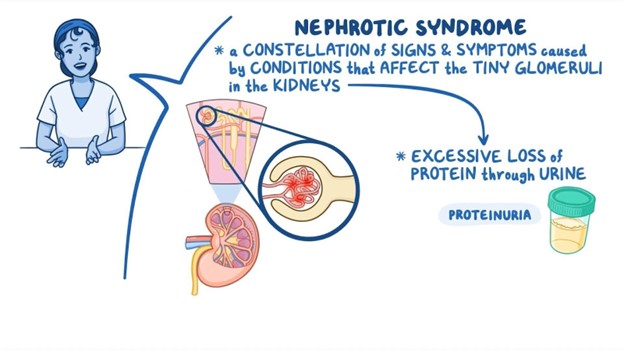
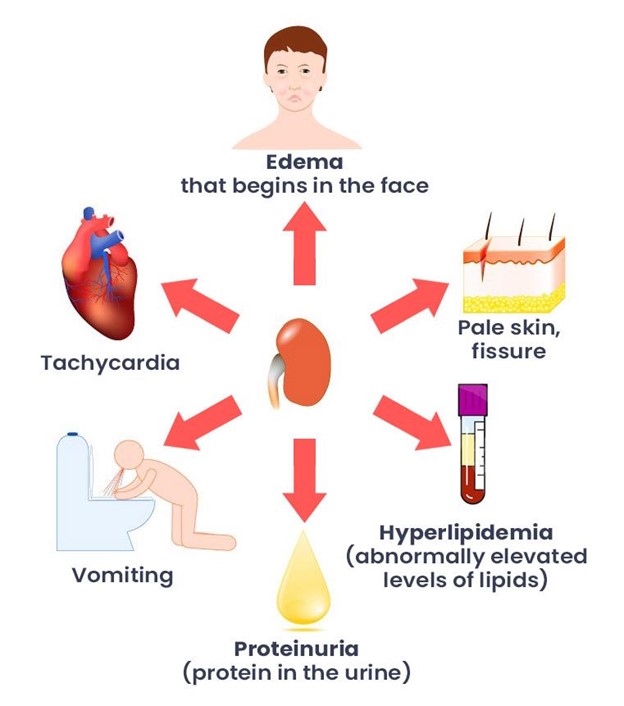
A 4-year-old with nephrotic syndrome is experiencing severe periorbital edema. The best measure the nurse could institute to help reduce the periorbital edema is:
Explanation
A. Apply cool sterile soaks to the child's head.
Explanation: Applying cool sterile soaks to the child's head would not directly address periorbital edema. Nephrotic syndrome is a kidney disorder that results in proteinuria (loss of protein in urine), leading to fluid accumulation and edema. Cooling the head would not have a significant impact on reducing periorbital edema caused by nephrotic syndrome.
B. Apply warm compresses.
Explanation: Correct Choice. Applying warm compresses can help increase blood circulation and promote the reabsorption of excess fluid causing periorbital edema. Warmth can dilate blood vessels and improve the movement of fluids, potentially alleviating the edema.
C. Encourage the child to eat low protein foods.
Explanation: While dietary modifications might be part of managing nephrotic syndrome, specifically encouraging low protein foods may not directly address periorbital edema. The primary treatment for nephrotic syndrome involves medications to control proteinuria and manage fluid balance.
D. Elevate the head of the bed.
Explanation: Elevating the head of the bed is more commonly used to manage conditions like heart failure or obstructive sleep apnea. It might have some impact on overall fluid distribution, but it's not the most effective measure for reducing periorbital edema caused by nephrotic syndrome.
A nurse is caring for a child who is having a tonic-clonic seizure and vomiting. Which of the following actions is the nurse's priority?
Explanation
A. Place a pillow under the child's head.
Explanation: While providing comfort is important, the priority in this scenario is to ensure the child's safety. Placing a pillow under the head can be considered after addressing immediate safety concerns.
B. Clear the area of hazards.
Explanation: Correct Choice. Ensuring the area is clear of hazards is the nurse's priority. During a seizure, the child can experience uncontrolled movements, and having hazards around can lead to injuries. Clearing the area helps prevent harm. But priority is to position the child side lying.
C. Position the child side-lying.
Explanation: Correct Choice. Placing the child in a side-lying position helps prevent choking and aspiration due to vomiting during the seizure. It also minimizes the risk of airway obstruction and helps manage secretions.
D. Loosen restrictive clothing.
Explanation: While loosening restrictive clothing can facilitate breathing, the priority in this situation is addressing safety concerns related to the seizure and vomiting. Ensuring a clear and safe environment takes precedence.
What do we include as part of our concussion/head injury prevention teaching to children and parents:
Explanation
A. Dizziness is always a sign of a concussion.
This statement is incorrect. While dizziness can be a symptom of a concussion, it is not always indicative of a concussion. There can be various causes of dizziness, and it is essential to consider other symptoms as well when assessing for a concussion.
B. Bike Helmet Safety
Explanation:
The correct answer to include as part of concussion/head injury prevention teaching to children and parents is "Bike helmet safety." This is because wearing a helmet while riding a bike or participating in other activities that involve head injury risks is crucial to prevent head injuries and concussions. Helmets provide protection to the head by absorbing impact energy and reducing the risk of skull fractures or traumatic brain injuries.
C. Normal fluid intake.
While staying hydrated is important for overall health, it is not directly related to concussion or head injury prevention teaching. This choice is unrelated to the topic.
D. Signs of autism.
Signs of autism are unrelated to concussion or head injury prevention teaching. This choice is not relevant to the topic at hand.
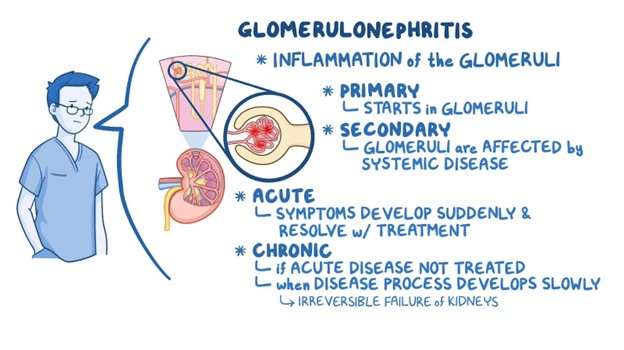
A nurse is caring for a child who has acute glomerulonephritis. Which of the following actions is the nurse's priority?
Explanation
A. Maintain a saline-lock:
This option involves keeping a saline-lock (also known as a saline flush or heparin lock) in place. A saline-lock is a device used to keep an IV line open without continuous fluids running through it. While this is important for various medical situations, it's not the priority in the case of a child with acute glomerulonephritis.
B. Check the child's daily weight:
This is the correct answer. The priority in a child with acute glomerulonephritis is to monitor their daily weight. Acute glomerulonephritis affects the kidneys' ability to filter waste and excess fluid from the blood. Weight gain can indicate fluid retention, a common complication of this condition. Rapid weight gain may indicate worsening fluid retention and potential complications like heart failure or hypertensive crisis.
C. Place the child on a no-salt-added diet:
While dietary modifications can be important for managing various health conditions, including kidney issues, this is not the top priority in this situation. Reducing salt intake can help manage fluid retention, but it is not the nurse's priority action at this moment.
D. Educate the parents about potential complications:
Patient education is crucial, especially in chronic conditions, but in this acute care scenario, the nurse's immediate priority is to address the child's needs. Educating parents about potential complications should be done, but it's not the most immediate action.
A nurse is reviewing the laboratory results of an adolescent who has chronic glomerulonephritis. Which of the following findings should the nurse expect?
Explanation
A) Absence of proteinuria:
Chronic glomerulonephritis often involves damage to the glomeruli in the kidneys, which can lead to the leakage of protein into the urine, resulting in proteinuria. The absence of proteinuria would be an unexpected finding in a patient with chronic glomerulonephritis. Therefore, this choice is incorrect.
B) Serum phosphorus 4.0 mg/dL (within expected reference range):
Serum phosphorus levels within the expected reference range are not directly related to chronic glomerulonephritis. While abnormalities in electrolyte levels might occur due to kidney dysfunction, serum phosphorus within the normal range is not a hallmark finding of glomerulonephritis. Therefore, this choice is incorrect.
C) Serum potassium 3.8 mEq/L (within the expected reference range):
Similar to serum phosphorus, serum potassium levels within the normal range are not specific to chronic glomerulonephritis. Kidney dysfunction can indeed affect electrolyte levels, but a serum potassium level within the normal range doesn't provide specific information about glomerulonephritis. Therefore, this choice is incorrect.
D) BUN 50 mg/dL (elevated):
Blood Urea Nitrogen (BUN) is a waste product that is filtered by the kidneys. Elevated BUN levels indicate impaired kidney function, as the kidneys are less efficient at filtering and excreting waste products. Chronic glomerulonephritis can lead to progressive kidney damage, which can result in elevated BUN levels due to decreased filtration and clearance. Therefore, an elevated BUN level is an expected finding in a patient with chronic glomerulonephritis.
A toddler diagnosed with nephrotic syndrome has a nursing diagnosis of excess fluid related to fluid accumulation (generalized edema). Which nursing intervention would be the priority to include in the nursing plan of care?
Explanation
A) Seizure Precautions:
While seizure precautions are important in certain clinical situations, they are not directly related to the excess fluid and generalized edema associated with nephrotic syndrome. Nephrotic syndrome is primarily characterized by proteinuria, hypoalbuminemia, and fluid retention, which can lead to edema. Seizure precautions would not directly address the fluid imbalance in this context.
B) Ambulation:
Ambulation involves walking or movement and is not a priority intervention for addressing excess fluid and generalized edema. The primary concern in nephrotic syndrome with fluid accumulation is to manage the fluid balance and prevent further complications related to edema, such as respiratory distress or compromised circulation.
C) Daily weight:
This is the correct priority intervention. Daily weight monitoring is crucial in managing fluid balance and assessing the effectiveness of treatment in a child with nephrotic syndrome and fluid accumulation. Sudden weight gain can indicate worsening edema, while weight loss might indicate a response to treatment. Daily weight monitoring provides essential information to adjust fluid and medication management accordingly.
D) Keep bed position flat:
While maintaining a flat bed position may help improve venous return and fluid distribution, it is not the priority intervention for managing excess fluid and generalized edema in a child with nephrotic syndrome. Monitoring daily weight and adjusting treatment based on weight changes are more directly related to addressing the fluid imbalance.
A child with epilepsy has been seizure free for 2 years. A father asks the nurse how much longer the child will need to take the anti-seizure medications. The nurse includes which of the following in the response?
Explanation
A) A step-wise approach will be used to reduce the dosage gradually.
Explanation:
After a certain period of seizure control, a healthcare provider may consider gradually tapering and discontinuing anti-seizure medications in consultation with the child's neurologist. This is often done in a step-wise manner to monitor the child's condition and minimize the risk of seizure recurrence. Stopping anti-seizure medications abruptly can increase the risk of seizures returning. Therefore, the response provided in option A is the most accurate and relevant to the situation.
The other options are incorrect:
B) Your child will always suffer seizures:
This statement is not accurate, as some children with epilepsy can achieve long-term seizure control with appropriate treatment. Epilepsy management varies from person to person, and many individuals can experience extended periods of seizure freedom.
C) This is always a hereditary disorder:
Epilepsy can have both genetic and non-genetic causes. While there are genetic forms of epilepsy, not all cases are hereditary. Epilepsy can be caused by a variety of factors, including brain injuries, infections, and other medical conditions.
D) Only her male offspring will experience seizures:
Epilepsy does not discriminate based on gender. Both males and females can be affected by epilepsy. This statement is not accurate and does not reflect the reality of epilepsy as a medical condition.
Which of the following statements by a mother of a toddler diagnosed with nephrotic syndrome indicates that the mother understands the teaching about the disease?
Explanation
A. "We worry about surgery. Do you think we should investigate direct donation of blood?"
Explanation: This statement doesn't show a clear understanding of nephrotic syndrome. Nephrotic syndrome is a kidney disorder that involves the kidneys' ability to filter blood, but it doesn't typically involve blood donation or surgery related to that. Direct donation of blood is not relevant to the treatment or management of nephrotic syndrome.
B. "We'll have to encourage lots of liquids. Did you say about Biters per day?"
Explanation: This statement suggests a misunderstanding of nephrotic syndrome and its management. Encouraging lots of liquids is generally not a primary concern in nephrotic syndrome. In fact, excess fluid intake might be counterproductive, as it could worsen edema (swelling) that often occurs with this condition. Additionally, the term "Biters per day" doesn't seem relevant to nephrotic syndrome or its management.
C. "My child really likes chips and bologna. I guess we will have to find something else."
Explanation: This statement indicates an understanding of dietary considerations related to nephrotic syndrome. Nephrotic syndrome involves protein loss through the urine, which can lead to low protein levels in the blood. To address this, dietary changes are often recommended to include foods rich in protein. Avoiding high-sodium foods like chips and bologna is also important, as excessive sodium intake can contribute to fluid retention and worsen edema.
D. "We understand the need for antibiotics, hope they can be given orally."
Explanation: This statement doesn't relate to nephrotic syndrome or its management. Nephrotic syndrome primarily involves issues with kidney function and protein loss, and antibiotics are not a standard treatment for this condition. Antibiotics are used to treat infections, which can sometimes be a complication of nephrotic syndrome due to the immune system's vulnerability, but the statement doesn't focus on the understanding of the disease itself.
Correct Answer: C. "My child really likes chips and bologna. I guess we will have to find something else."
Explanation: This statement shows an understanding of the dietary changes needed for a child with nephrotic syndrome. It acknowledges the importance of adjusting the child's diet to include protein-rich foods and avoid high-sodium options, which aligns with the nutritional considerations for managing nephrotic syndrome.
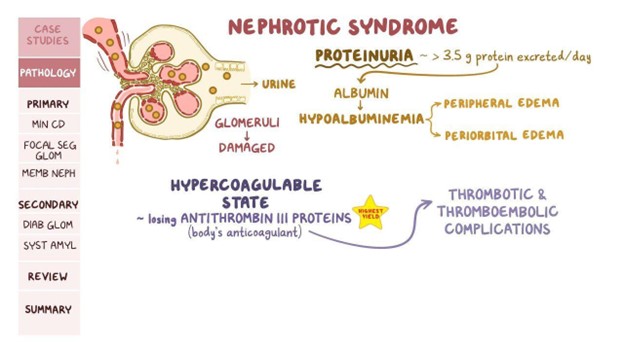
An eight-year-old with nephrotic syndrome is pale, lethargic, and has ascites. To determine if the ascites is increasing, the nurse should (chose one best answer):
Explanation
A. Assess the bowel sounds:
Bowel sounds are not directly related to the assessment of ascites. Bowel sounds are more relevant in assessing gastrointestinal function and peristalsis. While bowel changes could potentially be a sign of complications, monitoring abdominal girth is more specific to tracking ascites.
B. Frequently ambulate child:
While ambulation is important for overall health, it's not a direct assessment method for monitoring ascites. Ambulating a child might have benefits, but it won't provide specific information about the presence or progression of ascites.
C. Weigh child weekly:
Weekly weighing can provide some information about overall fluid balance, but it might not be as sensitive as measuring abdominal girth when it comes to detecting changes in ascites. Additionally, monitoring weight alone might not give insight into the distribution of fluid in the abdominal cavity.
D. Monitor and measure the abdominal girth.
Explanation: The presence of ascites (accumulation of fluid in the abdominal cavity) in a child with nephrotic syndrome could indicate worsening kidney function and fluid balance. Monitoring and measuring the abdominal girth is a reliable way to assess changes in the amount of fluid accumulation over time. An increase in abdominal girth could suggest a worsening condition.
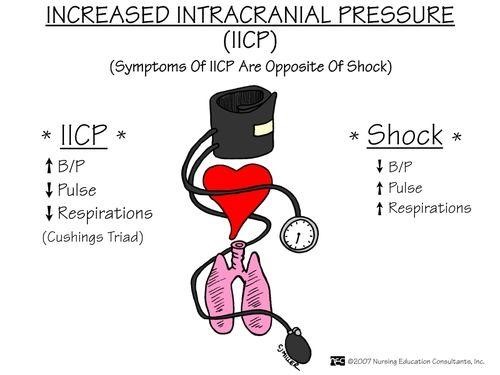
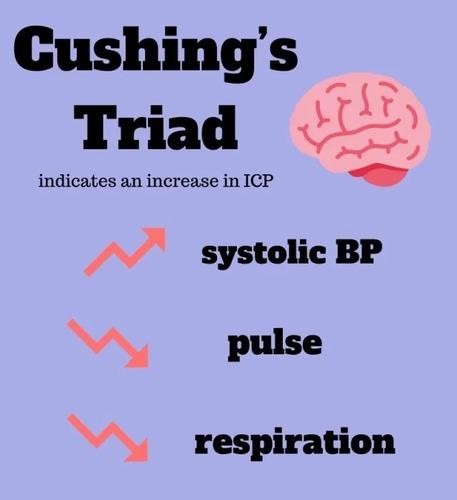
Cushings Triad is an ominous sign including the following:
Explanation
A. Elevated blood glucose is remarkable with Cushing's Triad:
Elevated blood glucose is not one of the components of Cushing's Triad. The triad focuses on cardiovascular and respiratory changes associated with increased intracranial pressure, not blood glucose levels.
B. Cushing's Triad includes a positive Macawen's sign:
Macawen's sign is not part of Cushing's Triad. Cushing's Triad is specifically related to the physiological responses seen in response to increased intracranial pressure and is not associated with Macawen's sign.
C. Cushing's Triad includes tachycardia, seizures and rapid respirations:
This option is not accurate. Cushing's Triad involves bradycardia (slow heart rate), irregular respirations, and a widening pulse pressure. Tachycardia (rapid heart rate) and seizures are not part of Cushing's Triad but might be indicative of other medical conditions or complications.
D. Bradycardia, irregular respirations and a widening pulse pressure.
Explanation: Cushing's Triad is a set of three clinical signs that are indicative of increased intracranial pressure (ICP) and are considered ominous as they suggest serious brain injury or pathology. The triad consists of:
Bradycardia: This refers to a slow heart rate. As intracranial pressure increases, it can lead to a decreased heart rate due to pressure on the brainstem, which is involved in regulating heart rate.
Irregular Respirations: Increased ICP can affect the brainstem's control over breathing, leading to irregular patterns of breathing, often known as Cheyne-Stokes respiration. This is characterized by periods of rapid breathing followed by apnea (temporary cessation of breathing).
Widening Pulse Pressure: Pulse pressure is the difference between systolic and diastolic blood pressure. An increase in ICP can cause an increase in systolic blood pressure and a decrease in diastolic blood pressure, leading to a widening pulse pressure.
A child with growth hormone deficiency (hypopituitarism) is being started on growth hormone therapy. Nursing considerations should be based on knowledge of which of the following:
Explanation
A. Replacement therapy may require daily subcutaneous injections.
Explanation: Growth hormone deficiency (hypopituitarism) often requires treatment with growth hormone therapy. One common method of administering growth hormone is through daily subcutaneous injections. Subcutaneous injections involve injecting the medication under the skin into the fatty tissue. This is a routine part of growth hormone therapy, and nursing considerations would include educating the child and their family about proper injection techniques, site rotation, and adherence to the treatment schedule.
Explanation for the other choices:
B. Lifelong replacement therapy will be required:
This statement is generally true. Growth hormone deficiency often requires long-term treatment, which may extend throughout childhood and adolescence. However, in some cases, the need for growth hormone therapy might change based on the individual's response to treatment and growth patterns.
C. Treatment is most successful if started during adolescence:
The optimal timing for starting growth hormone therapy can vary depending on the specific circumstances and the underlying cause of growth hormone deficiency. While treatment during adolescence can be effective, growth hormone therapy can also be successful if started earlier in childhood or later in adolescence. The key is identifying and treating the deficiency as soon as possible to promote healthy growth.
D. Treatment is considered successful if children attain full stature by adulthood:
While growth hormone therapy aims to support growth, achieving "full stature" might not always be possible. The goal of treatment is to help the child reach a more typical height based on their genetic potential and individual response to therapy. The success of treatment is determined by improvements in growth velocity and height, rather than necessarily achieving "full stature," which can vary greatly among individuals.
What is the daily fluid requirement (total in 24 hours) for a child who weighs 70.4lb? Do not use a label- it is ml. in the answer.(Answer in 24-hour clock system)
Explanation
Fluid Requirement (mL/24 hours) = Weight (kg) × Fluid Requirement (mL/kg)
Given that the child weighs 70.4 pounds, we first need to convert this weight to kilograms (1 lb = 0.453592 kg):
Weight in kg = 70.4 lb × 0.453592 kg/lb ≈ 31.89 kg
Now, let's calculate the fluid requirement using the given choices:
A) 1740:
Fluid Requirement = 31.89 kg × 55 mL/kg = 1753.95 mL
B) 134056:
This number is significantly larger than any reasonable fluid requirement and is likely an error.
C) 2:
This value is far too low to represent the fluid requirements of a child.
D) 12:
This value is also too low to represent the fluid requirements of a child.
So, the correct answer is A) 1740 mL. The child's estimated daily fluid requirement would be around 1740 mL in a 24-hour period, based on a weight of 70.4 pounds.
A nurse is providing teaching to an adolescent who has type 1 diabetes mellitus. Which of the following should the nurse include in the teaching?
Explanation
Type 1 diabetes mellitus is a condition where the body's immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. Individuals with type 1 diabetes require insulin therapy to manage their blood sugar levels. Since the question is about teaching an adolescent with type 1 diabetes, let's analyze each option:
A) Obtain an influenza vaccine annually:
This is a crucial recommendation. People with diabetes, including type 1 diabetes, have a higher risk of complications from infections, including influenza (the flu). The flu can lead to elevated blood sugar levels and potentially worsen diabetes control. Getting an annual influenza vaccine helps reduce the risk of getting the flu and its associated complications.
B) Take glyburide with breakfast:
Glyburide is a medication used to treat type 2 diabetes, not type 1 diabetes. It stimulates the pancreas to produce more insulin. Type 1 diabetes is characterized by a lack of insulin production, so taking glyburide would not be appropriate.
C) Administer glucagon for hyperglycemia:
Glucagon is a hormone used to raise blood sugar levels, typically in cases of severe hypoglycemia (low blood sugar). It is not used to treat hyperglycemia (high blood sugar) in type 1 diabetes. Instead, insulin administration is the primary method for managing high blood sugar levels.
D) Inject insulin in the deltoid muscle:
Insulin injections for individuals with type 1 diabetes are typically given in the subcutaneous fat, which is found just beneath the skin. The deltoid muscle is not a recommended site for insulin injections due to inconsistent absorption. The abdomen, thighs, and buttocks are commonly recommended injection sites.
A nurse is assessing a child who has nephrotic syndrome. Which of the following findings should the nurse expect?
Explanation
A) Smokey brown urine:
This finding is not typically associated with nephrotic syndrome. Smokey brown urine might indicate the presence of blood in the urine, which can be seen in conditions such as hematuria or certain kidney infections.
B) Polyuria:
Polyuria refers to excessive urination and is not a primary characteristic of nephrotic syndrome. However, children with nephrotic syndrome may have decreased urine output due to the loss of fluid and proteins through the damaged kidney filters.
C) Facial edema:
Facial edema (swelling of the face) is a hallmark of nephrotic syndrome. The loss of albumin in the urine results in a decrease in oncotic pressure (a force that helps keep fluid in the blood vessels), leading to fluid accumulation in the interstitial spaces, including the face, ankles, and abdomen.
D) Hypertension:
Hypertension (high blood pressure) is not a typical finding of nephrotic syndrome itself. However, it's possible for kidney damage to lead to secondary hypertension. In nephrotic syndrome, low levels of albumin can trigger the renin-angiotensin-aldosterone system, which can contribute to increased blood pressure.
A nurse is caring for a school-age child who has acute glomerulonephritis with peripheral edema and is producing 35 mL of urine per hour. The nurse should place the client on which of the following diets?
Explanation
A) Low-protein, low-potassium diet:
While low-protein and low-potassium diets can be appropriate for certain kidney conditions, such as chronic kidney disease, they are not typically the primary focus in the acute phase of glomerulonephritis. Protein restriction might be considered if there is significant kidney damage, and potassium levels are elevated.
B) Low-sodium fluid-restricted diet:
This is the most appropriate option. In acute glomerulonephritis, the kidneys' ability to regulate sodium and fluid balance may be impaired due to inflammation and decreased glomerular filtration. Fluid retention and peripheral edema are common. A low-sodium diet helps reduce fluid retention and manage edema.
C) Low carbohydrate, low-protein diet:
Low-carbohydrate and low-protein diets are not the main dietary considerations for acute glomerulonephritis. The primary focus is on managing sodium and fluid intake due to impaired kidney function.
D) Regular diet, no added salt:
A regular diet without added salt might exacerbate the fluid retention and edema associated with acute glomerulonephritis. Sodium intake needs to be controlled to prevent further fluid buildup.
The follow questions refer to the patient described below:
A 9 yr. old child with both hydrocephalus and a cardiac defect weighs 55 pounds. He requires digoxin by mouth once daily, the dose should be held if there are any symptoms of toxicity.
Pediatric maintenance dose is 5 mcg/kg daily given as a single dose. After listening to the apical rate for one full minute, you note it is only 50. Should you administer the digoxin as ordered?
Explanation
Digoxin is a medication commonly used to treat certain heart conditions, including some congenital heart defects. It's important to monitor the heart rate and other signs of toxicity when administering digoxin, especially in pediatric patients. Let's break down the information given:
The pediatric maintenance dose of digoxin is 5 mcg/kg daily.
The child weighs 55 pounds (approximately 25 kg).
Given these values, the total daily dose for this child would be:
Total daily dose = 5 mcg/kg × 25 kg = 125 mcg
This total daily dose is usually given as a single dose. However, the child's heart rate is noted to be only 50 beats per minute (bpm). A heart rate of 50 bpm in a child could potentially indicate bradycardia (slow heart rate), which can be a sign of digoxin toxicity. Bradycardia is a known adverse effect of digoxin, and it's important to assess for other signs of toxicity as well, such as nausea, vomiting, and changes in color vision.
In this case, it would be prudent to withhold the digoxin and assess the child further for signs of toxicity or bradycardia. The dose should not be administered until the healthcare provider is consulted and appropriate action is determined.
So, the correct answer is indeed NO. Administering the digoxin without considering the slow heart rate and the potential for toxicity could be unsafe for the child.
A nurse in a special education program is planning care for a child who has autism spectrum disorder. Which of the following interventions should the nurse include in the plan of care?
Explanation
A) Allow for adjustment of rules to correlate with the child's behavior:
Children with ASD often benefit from clear and consistent rules and expectations. Adjusting rules based on behavior might lead to confusion and unpredictability for the child. Instead, providing clear and predictable expectations can help them understand and navigate their environment.
B) Allow for imaginative play with peers without supervision:
Children with ASD might have challenges with social interaction and communication, making unsupervised play with peers potentially challenging. It's important to provide appropriate supervision and guidance to support positive social interactions and ensure the child's safety and comfort.
C) Provide a flexible schedule that adjusts to the child's interests:
This is a key intervention. Many children with ASD thrive in structured and routine environments. However, flexibility within that structure, especially to accommodate the child's interests, can enhance engagement and motivation. Adapting activities to align with the child's preferences can help maintain their attention and participation.
D) Establish a reward system for positive behavior:
This is another important intervention. Children with ASD often respond well to visual cues and rewards for positive behavior. A well-structured reward system can reinforce desired behaviors and provide motivation for the child to engage and interact more effectively.

A nurse in a special education program is planning care for a child who has autism spectrum disorder. Which of the following interventions should the nurse include in the plan of care?
Explanation
Autism Spectrum Disorder (ASD) is a complex neurodevelopmental disorder that affects communication, social interaction, and behavior. When planning care for a child with ASD, it's important to consider their individual needs and strengths.
A) Allow for adjustment of rules to correlate with the child's behavior:
Children with ASD often benefit from consistent routines and clear expectations. Adjusting rules based on behavior might confuse the child and undermine the structure they rely on for understanding their environment.
B) Allow for imaginative play with peers without supervision:
Children with ASD can struggle with social interactions and may need guidance to engage in play with peers successfully. Unsupervised imaginative play might lead to challenges or misunderstandings, making supervision and support important.
C) Provide a flexible schedule that adjusts to the child's interests:
This is a crucial intervention. Many children with ASD find comfort in routines, but rigidity can be detrimental. A flexible schedule that incorporates the child's interests can enhance engagement, motivation, and learning. It provides structure while accommodating the child's preferences.
D) Establish a reward system for positive behavior:
Reward systems can be effective for motivating positive behaviors in children with ASD. Visual cues and rewards are often helpful in reinforcing desired behaviors. This intervention can encourage appropriate social interactions and communication.
A nurse is teaching a school-age child who has type 1 diabetes mellitus and his parents about illness management. Which of the following instructions should the nurse include?
Explanation
A) "Limit fluid intake during mealtime":
Limiting fluid intake during meals is not a standard practice for managing type 1 diabetes. Proper hydration is important for overall health, and fluids should be consumed as needed.
B) "Notify the provider if blood glucose levels are over 350 milligrams/deciliter":
This is a crucial instruction. Blood glucose levels over 350 mg/dL can indicate hyperglycemia, which requires prompt attention. High blood glucose levels can lead to complications if not addressed promptly. Contacting the healthcare provider is an appropriate step.
C) "Test the urine for ketones":
Testing urine for ketones is an important instruction. Ketones are produced when the body breaks down fat for energy, often in the absence of sufficient insulin. High ketone levels can indicate diabetic ketoacidosis (DKA), a serious complication. Regular ketone testing, especially during illness or high blood glucose levels, helps monitor for DKA.
D) "Withhold insulin dose if feeling nauseous":
This instruction is not accurate. Nausea could be a sign of various conditions, including illness. Insulin should not be withheld without consulting a healthcare provider. Managing insulin doses appropriately is crucial to maintaining blood glucose control
A nurse is orienting a newly licensed nurse in the care of an infant who has myelomeningocele. Which of the following actions by the new nurse indicates the teaching has been effective?
Explanation
A) Places the infant in a side-lying position:
Positioning is important in the care of an infant with myelomeningocele. The infant is usually placed in a prone (on the abdomen) position to prevent pressure on the sac and protect the neural tissue. Placing the infant in a side-lying position may not provide the needed protection.
B) Maintains a dry dressing over the sac:
This action indicates effective teaching. The sac should be covered with a sterile, non-stick dressing to protect the exposed neural tissue from infection and trauma. Keeping the dressing dry is important to prevent complications
C) Performs range of motion on the infant's hips:
Range of motion exercises are not typically performed on the hips of an infant with myelomeningocele. The focus of care is primarily on protecting the exposed neural tissue, preventing infection, and ensuring proper positioning.
D) Takes an axillary temperature:
Taking an axillary temperature is a common method for measuring an infant's body temperature. However, in the case of an infant with myelomeningocele, it's important to avoid any pressure or friction on the sac area. The nurse should use care to prevent disturbing the dressing or causing discomfort to the infant.
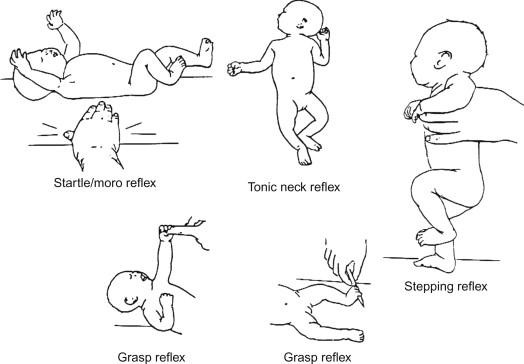
The nurse is doing a neurologic assessment on a 2-month-old infant after a car accident. Moro, tonic neck, and withdrawal reflexes are present. The nurse should recognize that these reflexes are:
Explanation
Reflexes play a crucial role in evaluating the neurological status of infants.
Moro reflex: Also known as the startle reflex, the Moro reflex is a normal response in infants. It occurs when an infant is startled by a sudden noise or movement. The baby responds by extending their arms and legs, followed by a quick contraction. This reflex usually disappears around 4-6 months of age.
Tonic neck reflex (fencer's reflex): This reflex involves turning an infant's head to one side, causing the arm on that side to extend and the opposite arm to flex. It's a normal reflex that typically disappears around 4-6 months of age.
Withdrawal reflex: The withdrawal reflex is a normal response to a stimulus, such as touching a baby's foot with a cold object. The baby will pull their leg away in response to the stimulus.
Symptomatic of decorticate or decerebrate posturing (options A and B):
Decorticate and decerebrate posturing are abnormal postures seen in individuals with severe brain damage or injury. Decorticate posturing involves the arms being flexed and held close to the body, while decerebrate posturing involves the arms being extended and the wrists being pronated. These reflexes are typically indicative of significant neurological dysfunction and are not expected in a 2-month-old infant after a car accident.
Indicators of severe brain damage (option C):
The reflexes described (Moro, tonic neck, and withdrawal reflexes) are not indicative of severe brain damage in a 2-month-old infant. These reflexes are normal for an infant of this age and are part of their typical neurological development.
Normal findings (option D):
The reflexes described are normal findings in a 2-month-old infant and are expected as part of their developmental milestones.
A nurse is caring for a child who has a suspected diagnosis of bacterial meningitis. Which of the following actions is the nurse's priority?
Explanation
A) Document intake and output:
Documenting intake and output is an important nursing task, but it is not the top priority in a suspected case of bacterial meningitis. Timely administration of antibiotics to treat the infection takes precedence over documentation of intake and output.
B) Administer antibiotics when available.
Explanation:
Bacterial meningitis is a serious and potentially life-threatening infection of the membranes covering the brain and spinal cord. Rapid administration of antibiotics is crucial to effectively treat the infection and prevent its spread. Delay in antibiotic administration can lead to worsening symptoms and complications. Therefore, getting the appropriate antibiotics to the child as soon as they are available is the nurse's priority.
C) Reduce environmental stimuli:
Reducing environmental stimuli can be helpful in managing symptoms and providing comfort to the child with meningitis, but it is not the priority action. The immediate concern in a suspected case of bacterial meningitis is to treat the infection.
D) Maintain seizure precaution:
While maintaining seizure precautions is important, especially if the child has a history of seizures, it is not the top priority in a suspected case of bacterial meningitis. Administering antibiotics to treat the infection and prevent its progression is the primary concern.
Sign Up or Login to view all the 50 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

