ATI PEDIATRICS EXAM 4
Total Questions : 35
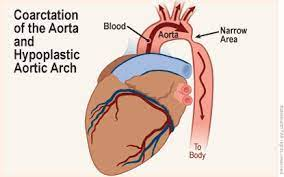
Showing 25 questions, Sign in for moreAn 8-year-old patient presents to his clinic, complaining of dizziness, headaches, and epistaxis. The nurse took the patient's vital signs and noticed that he had high blood pressure in his arms and bounding upper extremity pulses; however, when she proceeded to check his lower extremity pulses, they were weak, and his legs were pale and cool to touch. What does this patient present signs of?
Explanation
Coarctation of the aorta is a congenital heart defect where the aorta, the major blood vessel that carries oxygenated blood from the heart to the body, is narrowed. As a result, blood pressure tends to be higher in the arms and upper body but lower in the lower body, including the legs. This condition can lead to symptoms such as dizziness, headaches, and even nosebleeds due to high blood pressure. Weak or absent lower extremity pulses, as well as pale and cool legs, are characteristic physical findings in coarctation of the aorta.
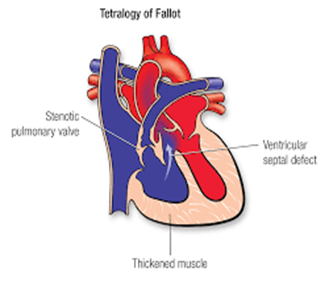
A. Tetralogy of Fallot: This is a different congenital heart defect characterized by a combination of four specific heart defects, including ventricular septal defect, right ventricular hypertrophy, pulmonary stenosis, and an overriding aorta. It typically does not cause the symptoms described in the scenario.
C. Pulmonic Stenosis: This condition involves the narrowing of the pulmonary valve or artery, leading to restricted blood flow from the right ventricle to the pulmonary artery. While it can cause various symptoms, it typically doesn't cause the specific blood pressure discrepancies described.
D. Tricuspid Atresia: This is a congenital heart defect where the tricuspid valve is absent or abnormally developed. It leads to the mixing of oxygenated and deoxygenated blood in the heart. While it can cause cyanosis (bluish skin due to low oxygen levels), it doesn't typically cause the specific blood pressure findings mentioned.
An 8-month-old infant has a hypercyanotic spell while blood is being drawn. What is the priority nursing action?
Explanation
Hypercyanotic spells, also known as "Tet spells," can occur in infants with congenital heart defects, particularly tetralogy of Fallot. During these spells, there is a sudden decrease in oxygen saturation, leading to cyanosis (blueness) of the infant's skin and lips, as well as respiratory distress and possible loss of consciousness.
The knee-chest position is a specific technique used to manage hypercyanotic spells. Placing the child in this position helps improve oxygenation by increasing systemic vascular resistance and reducing the degree of right-to-left shunting of blood in the heart. It also increases venous return to the heart, which can help improve cardiac output.
Now, let's discuss why the other options are incorrect:
A. Prepare family for imminent death: This is not the priority action. While hypercyanotic spells can be life-threatening, the immediate focus should be on managing the spell to improve oxygenation and prevent further deterioration. Preparing the family for death should only be considered if resuscitation measures fail, which is not the first-line intervention.
C. Assess for neurologic defects: Assessing for neurologic defects is important but not the immediate priority during a hypercyanotic spell. The primary concern at this moment is addressing cyanosis and respiratory distress to ensure the infant receives adequate oxygen.
D. Begin cardiopulmonary resuscitation: Initiating CPR is not the initial priority during a hypercyanotic spell. CPR would be indicated if the infant's condition deteriorates to the point of cardiac arrest, but it should not be the first step. Placing the child in the knee-chest position is a non-invasive intervention that should be attempted before considering CPR.
Which of the following options gives a nurse the most accurate diagnostic picture of a cardiac issue?
Explanation
B. Cardiac Catheterization.
Cardiac Catheterization (B): Cardiac catheterization is an invasive procedure that involves threading a catheter into the heart's chambers and major blood vessels. It allows direct visualization of the coronary arteries, measurement of blood pressure within the heart, assessment of blood flow, and the ability to perform interventions such as angioplasty or stent placement. Cardiac catheterization is considered the gold standard for diagnosing coronary artery disease, evaluating heart valve function, and detecting congenital heart abnormalities.
Explanation:
A. Echocardiogram (A): An echocardiogram is a non-invasive imaging test that uses sound waves to create images of the heart. It is excellent for assessing the structure and function of the heart, including heart valve function and blood flow patterns. While it is a valuable tool for cardiac assessment, it may not provide the level of detail and direct visualization that cardiac catheterization offers.
C. Chest X-Ray (CXR) (C): A chest X-ray can provide information about the size and shape of the heart and detect certain abnormalities such as an enlarged heart or fluid in the lungs. However, it may not offer the level of detail required to diagnose specific cardiac issues accurately.
D. Electrocardiogram (ECG) (D): An ECG records the electrical activity of the heart and is useful for diagnosing arrhythmias and certain conduction abnormalities. While it provides essential information about cardiac rhythm, it does not directly visualize the structural aspects of the heart or blood flow.
In summary, while each of these diagnostic tools plays a crucial role in assessing cardiac issues, cardiac catheterization is the most accurate and comprehensive option for diagnosing a wide range of cardiac conditions due to its direct visualization and intervention capabilities. However, the choice of diagnostic test should always be made based on the patient's specific clinical presentation and the suspected cardiac problem.
in a non-potty trained child with nephrotic syndrome is the best way to detect fluid retention?
Explanation
A. Weighing the child daily (A) is the most accurate and objective method for monitoring fluid retention in a child with nephrotic syndrome. Nephrotic syndrome can lead to significant fluid retention due to proteinuria and hypoalbuminemia. Daily weight measurements can detect even small changes in body weight, which may be indicative of fluid accumulation. It is a sensitive and specific measure for assessing fluid status.
B. Measuring the abdominal girth weekly (B) can provide some information about abdominal distension, but it is not as precise or sensitive as daily weight measurements. Weight gain or loss can occur without significant changes in abdominal girth, especially in children.
C. Counting the number of wet diapers (C) may provide some information about urinary output, but it does not directly measure overall fluid retention or body weight changes. It is not as reliable as daily weight measurements for assessing fluid status.
D. Testing the urine for hematuria (D) is a valuable diagnostic test to assess kidney function and the presence of blood in the urine, but it does not directly measure fluid retention. Hematuria is not typically the primary indicator of fluid overload in nephrotic syndrome.
In summary, daily weight measurements are the best way to monitor fluid retention in a child with nephrotic syndrome, as they provide a direct and objective assessment of changes in fluid status. This allows healthcare providers to make timely adjustments to the child's treatment plan if necessary.
A 10-year-old has undergone a cardiac catheterization. At the end of the procedure, the nurse should first assess
Explanation
Assessing pulses is a critical step immediately after a cardiac catheterization procedure because it helps determine the adequacy of blood flow to the extremities and any potential vascular complications. Cardiac catheterization involves the insertion of a catheter through blood vessels, which can temporarily affect blood flow. Checking pulses in the affected limb (e.g., the leg or arm where the catheter was inserted) is essential to detect any signs of vascular compromises, such as decreased or absent pulses, which could indicate complications like arterial thrombosis or embolism. Prompt recognition of such issues is crucial for timely intervention to prevent potential complications or limb damage.
The other options are also important but should be addressed after the initial assessment of pulses:
A. Pain: Assessing pain is important, but it should come after checking pulses. If the child reports pain, it could indicate discomfort or complications related to the procedure, which may require further evaluation and intervention.
C. Catheterization report: Reviewing the catheterization report is necessary for a comprehensive understanding of the procedure and its findings, but it is not the immediate priority when assessing the child's post-procedure condition.
D. Hemoglobin and hematocrit levels: Checking hemoglobin and hematocrit levels is important to monitor for potential bleeding complications that may occur during or after the procedure, but it is a secondary assessment compared to evaluating pulses. If there are significant changes in these levels, they may require further investigation and intervention.
In summary, assessing pulses is the initial priority after a cardiac catheterization procedure in order to promptly identify any vascular issues or complications that need immediate attention.
Nick was diagnosed with Hypoplastic Left Heart Syndrome. Which of the following responses should the nurse educate his parents regarding the treatment of this disease?
Explanation
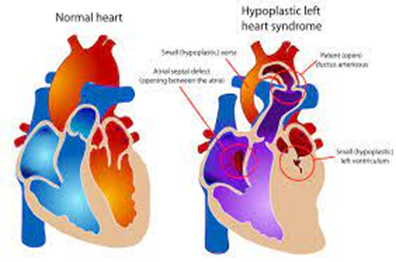
Hypoplastic Left Heart Syndrome is a complex congenital heart defect in which the left side of the heart (left ventricle and aorta) is underdeveloped, making it unable to pump oxygenated blood effectively to the body. The treatment of HLHS typically involves a series of surgical interventions because it cannot be cured with a single surgery. The ultimate goal of treatment is to provide palliative care, which means managing the condition to improve the child's quality of life while waiting for a heart transplant. The surgical procedures are typically performed in stages, with the first surgery usually performed shortly after birth, followed by additional surgeries as the child grows.
Option B is not accurate because HLHS cannot be cured with a single surgery, and creating an opening between the atria and ventricles (e.g., the Norwood procedure) is one step in the staged surgical treatment, but it doesn't completely "cure" the condition.
Option C is not accurate because HLHS is primarily characterized by an underdeveloped left ventricle and aorta, not the displacement of the pulmonary and aortic arteries.
Option D refers to the use of prostaglandin to maintain a patent ductus arteriosus (PDA) and improve blood flow to the lungs, which can be part of the initial management of HLHS but is not a definitive treatment. Prostaglandin is used to stabilize the infant before surgical interventions are performed.
Archie who weighs 44 tb has been given an order for amoxilin 500 mg bid to take before a dentist appointment based on his history of infective endocans. The drug test shows that the daily dose of amoecitin is 50 mg/kg/day in two divided doses. What dose in milligrams is safest for this child?
Explanation
To calculate the safest dose of amoxicillin for Archie based on his weight of 44 pounds (lbs) and the recommended dose of 50 mg/kg/day in two divided doses, you should follow these steps:
Step 1: Convert Archie's weight from pounds (lbs) to kilograms (kg).
1 pound = 0.453592 kilograms
44 lbs * 0.453592 kg/lb = 19.504 kg (rounded to the nearest tenth)
Step 2: Calculate the total daily dose based on his weight.
Total daily dose = Weight (kg) * Dose (mg/kg/day)
Total daily dose = 19.504 kg * 50 mg/kg/day = 975.2 mg/day
Step 3: Divide the total daily dose into two equal doses since it's to be administered in two divided doses.
Each dose = Total daily dose / 2
Each dose = 975.2 mg/day / 2 = 487.6 mg/dose
Since it's not possible to administer a fraction of a milligram accurately, you would round the dose to the nearest available dosage strength.
Therefore, the safest dose for Archie would be:
500 mg
So, Archie should take 500 mg of amoxicillin before his dentist appointment.
Which of the following would Nurse Tony supposed to regard as a cardinal manifestation or symptom of digoxin toxicity to his patient Clay diagnosed with heart failure?
Explanation
Digoxin is a medication commonly used to treat heart failure and certain heart rhythm disorders. However, it has a narrow therapeutic window, and digoxin toxicity can occur if the drug accumulates in the body to excessive levels. One of the hallmark signs of digoxin toxicity is severe bradycardia, which means an abnormally slow heart rate. Bradycardia can result from the effects of digoxin on the electrical conduction system of the heart, leading to an irregular or slowed heartbeat.
While other symptoms can occur in digoxin toxicity, such as gastrointestinal symptoms (like nausea and vomiting), neurological symptoms (like confusion and visual disturbances), and even respiratory distress in severe cases, extreme bradycardia is a key and often life-threatening sign that requires immediate medical attention.
Constipation (A) and headache (C) can also occur as side effects of digoxin but are less specific to digoxin toxicity and may not be considered cardinal manifestations.
Respiratory distress (B) may occur if the bradycardia leads to inadequate cardiac output, causing pulmonary congestion, but it is not a primary or cardinal symptom of digoxin toxicity. Extreme bradycardia is typically the more immediate and prominent concern.
The nurse is evaluating a female child with acute post-streptococcal glomerulonephritis for signs of improvement. Which finding typically is the earliest sign of improvement?
Explanation
APSGN is characterized by inflammation of the glomeruli in the kidneys, which can lead to decreased kidney function and impaired urine output. As the condition begins to improve, one of the first signs is an increase in urine output. This is because the inflammation in the glomeruli starts to resolve, allowing the kidneys to filter blood more effectively and produce a higher volume of urine.
Now, let's discuss why the other options are incorrect:
A. Increased energy levels: While improved energy levels can be a positive sign in a child recovering from an illness, they are not typically the earliest sign of improvement in APSGN. Energy levels may improve as the child's overall condition gets better, but this improvement often follows an increase in urine output.
B. Decreased diarrhea: APSGN primarily affects the kidneys, not the gastrointestinal tract. Therefore, diarrhea is not a direct symptom of this condition. Improving kidney function and urine output would not directly impact diarrhea.
D. Increased appetite: Like increased energy levels, an improved appetite can be a positive sign in recovery, but it is not typically the earliest sign of improvement in APSGN. It is generally more related to overall recovery and feeling better after the acute phase of the illness.
In summary, while all of these signs can be positive indicators of a child's recovery, increased urine output is usually the earliest and most specific sign of improvement in acute post-streptococcal glomerulonephritis, as it directly reflects the resolution of kidney dysfunction.
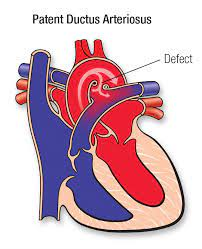
Surgical repair for patent ductus arteriosus (PDA) is done to prevent the complication of
Explanation
PDA is a congenital heart defect where a blood vessel called the ductus arteriosus, which is supposed to close shortly after birth, remains open. This allows oxygenated blood from the aorta to flow back into the pulmonary artery, leading to increased pulmonary blood flow and congestion. Over time, this can lead to increased pulmonary vascular congestion and potentially cause complications such as pulmonary hypertension and heart failure.
Surgical repair of PDA, often through a procedure known as ligation or closure of the ductus arteriosus, is performed to stop this abnormal blood flow and prevent the associated complications, particularly the increase in pulmonary vascular congestion.
The other options (B, C, and D) are not the primary complications associated with PDA and surgical repair is not performed primarily to address these issues:
B. Decreased workload on the left side of the heart is not a primary reason for surgical repair of PDA, although it can be a potential benefit of closing the ductus arteriosus.
C. Pulmonary infection is not a direct complication of PDA, but the increased pulmonary blood flow associated with a large PDA can make the lungs more susceptible to respiratory infections.
D. Right-to-left shunt of blood is not a typical complication of PDA. PDA typically involves left-to-right shunting of blood, with oxygenated blood flowing back into the pulmonary circulation, leading to complications related to increased pulmonary blood flow.
The nurses admiting a school-age child in acute renal failure o reduced glomerular filtration rate. Which urine test is the most useful clinical indication of glomerular filtration rate?
Explanation
Creatinine is a waste product generated by muscle metabolism and excreted by the kidneys. It is commonly used as a marker of renal function because it is filtered by the glomeruli and almost entirely excreted in the urine. When there is a reduction in GFR, as in acute renal failure, creatinine levels in the blood tend to rise. Elevated serum creatinine levels are indicative of impaired kidney function and a decreased GFR.
The other options are not direct indicators of GFR:
A. Protein level: While proteinuria (elevated protein levels in urine) can be a sign of kidney dysfunction, it is not a direct measurement of GFR. Proteinuria can occur for various reasons, including glomerular damage, but it doesn't provide a precise assessment of GFR.
C. Osmolality: Urine osmolality reflects the concentration of solutes in urine but is not a direct measure of GFR. It can provide information about the concentrating ability of the kidneys, but it doesn't assess the overall filtration rate.
D. pH: Urine pH is a measure of the acidity or alkalinity of urine and is not a direct indicator of GFR. It can be influenced by factors such as diet and renal tubular function but does not directly measure the filtration rate of the glomeruli.
A 1000 mL 0.9% NS bag is to be administered to a patient at 20 mL/hr. The patient is to receive this solution for hours. How many mi will the patient receive? (Round to the nearest whole number)
Explanation
To calculate the total volume the patient will receive, you can use the formula:
Total Volume = Rate x Time
In this case, the rate is 20 mL/hr, and the time is 24 hours. Now, calculate:
Total Volume = 20 mL/hr x 24 hr = 480 mL
So, the patient will receive a total of 480 mL of the 0.9% NS solution.
The nurse notes that a child has lost 8 pounds after 4 days of hospitalization for acute glomerulonephritis. What is most likely the cause of the weight loss?
Explanation
Weight loss in a child with acute glomerulonephritis is often due to a reduction in edema (fluid retention and swelling). Acute glomerulonephritis can lead to significant edema, as the kidneys may not effectively filter excess fluid and waste products from the body. During hospitalization and treatment, interventions such as diuretics and improved kidney function may result in the gradual removal of excess fluid, leading to a decrease in edema and overall body weight.
The other options are less likely to be the primary cause of the weight loss:
A. Poor appetite: While acute glomerulonephritis can affect appetite, especially due to nausea or other symptoms, it is not typically the primary reason for significant weight loss over a short period.
B. Restriction to bed rest: While being on bed rest can lead to muscle atrophy and loss of lean body mass over an extended period, it is unlikely to result in an 8-pound weight loss in just 4 days unless there are additional factors at play.
C. Increased potassium intake: Increased potassium intake alone would not be a primary cause of significant weight loss. High potassium levels in the blood (hyperkalemia) can occur in kidney disease, but it is not typically associated with rapid weight loss.
A pediatric nurse is seeing a B-year-old following a post-cardiac catheterization procedure. Which of the following interventions ordered by the physician should be questioned by the nurse? [Select All that Apply)
Explanation
After a cardiac catheterization procedure, it is essential to restrict activity and keep the affected extremity immobilized to prevent complications such as bleeding and hematoma formation at the catheter insertion site. Encouraging play and activity can increase the risk of disrupting the catheter site or causing bleeding.
The other interventions are generally appropriate after a cardiac catheterization procedure:
A. Putting pressure above the catheter site for first signs of bleeding: This is a standard procedure to monitor for any bleeding at the catheter site and is an appropriate intervention.
B. Regularly check the pulses and temperature of the affected extremity: Monitoring pulses and temperature is important to assess for adequate circulation and early detection of any vascular complications.
D. Encouraging the parents to ambulate with the child 3 hours, or the soonest possible time, after the procedure to prevent blood clots: Early mobilization can help prevent blood clots, and it is generally a recommended intervention following cardiac catheterization.
E. Monitor cardiac function and oxygen saturation: Continuous monitoring of cardiac function and oxygen saturation is crucial to detect any immediate post-procedure complications and ensure the child's cardiovascular stability.
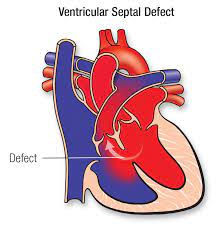
The nurse is caring for a 4-month-old with a history of ventricular septal defect. The infant is admitted for failure to thrive. What supportive measure would the nurse anticipate in an infant with congestive heart failure?
Explanation
Infants with congenital heart defects, including VSD, may have increased caloric needs due to the added work of their hearts. Congestive heart failure can lead to poor weight gain and failure to thrive. Therefore, increasing the caloric density of the formula is a common approach to providing the necessary nutrition for growth and development. This can be achieved by using specialized high-calorie infant formulas or fortifying breast milk.
The other options are not the primary supportive measures for an infant with congestive heart failure in this context:
B. Oxygen therapy to ensure oxygen saturation is > 98%: While oxygen therapy may be necessary for infants with congenital heart defects, it is not the primary supportive measure to address failure to thrive. Oxygen therapy primarily aims to ensure adequate oxygenation but does not directly address caloric intake.
C. Sedatives to keep the infant from crying: The use of sedatives is not a typical approach to managing congestive heart failure in infants. Addressing the underlying cause, optimizing nutrition, and providing supportive care are more appropriate strategies.
D. Emergent surgical correction of the defect: Surgical correction of a VSD is typically considered for specific indications, such as significant hemodynamic compromise, but it is not the first-line intervention for all cases of VSD, especially if the primary concern is failure to thrive. Treatment decisions for VSD are made based on the specific clinical presentation and severity of the defect.
A 5-year-old girl Hannah is recently diagnosed with Kawasaki disease. Apart from the identified symptoms of the disease, she may also likely develop which of the following?
Explanation
Kawasaki disease is a rare but serious condition that primarily affects children, particularly those under the age of 5. It is characterized by inflammation of the blood vessels throughout the body, including the coronary arteries. If left untreated, Kawasaki disease can lead to the development of aneurysms in the coronary arteries. These aneurysms can put the child at risk for complications such as thrombosis (clot formation) or rupture of the affected arteries, which can be life-threatening.
The other options (A, C, and D) are not typically associated with Kawasaki disease:
A. Sepsis: Kawasaki disease is not an infectious disease, and it does not directly lead to sepsis. It is an inflammatory condition believed to have an autoimmune component.
C. Meningitis: Kawasaki disease primarily affects blood vessels and does not lead to the development of meningitis.
D. Mitral valve disease: While Kawasaki disease can affect the cardiovascular system, it is not a direct cause of mitral valve disease. The development of mitral valve disease would be a separate cardiac issue unrelated to Kawasaki disease.
The Foley Family is caring for their youngest child, Justin, who is suffering from tetralogy of Fallot. Which of the following are defects associated with this congenital heart condition?
Explanation
Tetralogy of Fallot is a congenital heart defect characterized by four specific abnormalities:
Ventricular septal defect (VSD): This is a hole in the wall (septum) between the two lower chambers (ventricles) of the heart.
Overriding aorta: The aorta is positioned over both the left and right ventricles, which allows oxygen-poor (deoxygenated) blood from the right ventricle to be pumped into the aorta and to the body.
Pulmonic stenosis (PS): This is a narrowing of the pulmonary valve or artery that restricts blood flow from the right ventricle to the lungs.
Right ventricular hypertrophy: The right ventricle becomes thicker and more muscular as it works harder to pump blood against the narrowed pulmonary valve or artery.
Options A, C, and D describe different congenital heart conditions and defects, but they are not associated with Tetralogy of Fallot:
A. Coarctation of aorta, aortic valve stenosis, mitral valve stenosis, and patent ductus arteriosus are not part of the constellation of defects seen in the Tetralogy of Fallot.
C. Describing the aorta exiting from the right ventricle and pulmonary artery exiting from the left ventricle with two noncommunicating circulations is characteristic of transposition of the great arteries, not Tetralogy of Fallot.
D. Tricuspid valve atresia, atrial septal defect, ventricular septal defect, and hypoplastic right ventricle describe a different congenital heart condition, not Tetralogy of Fallot.
Which of the following disorders leads to cyanosis from deoxygenated blood entering the systemic arterial circulation?
Explanation
Tetralogy of Fallot is a congenital heart defect characterized by a combination of four specific heart abnormalities:
Ventricular septal defect (VSD): A hole in the wall (septum) between the two lower chambers (ventricles) of the heart.
Overriding aorta: The aorta is positioned over both the left and right ventricles, allowing oxygen-poor (deoxygenated) blood from the right ventricle to mix with oxygen-rich (oxygenated) blood from the left ventricle.
Pulmonic stenosis: Narrowing of the pulmonary valve or artery, which restricts blood flow from the right ventricle to the lungs.
Right ventricular hypertrophy: The right ventricle becomes thicker and more muscular as it works harder to pump blood against the narrowed pulmonary valve or artery.
The combination of these defects results in deoxygenated blood from the right ventricle being pumped into the systemic circulation, leading to cyanosis (blueness of the skin) due to decreased oxygen levels in the arterial blood.
The other options (A, B, and C) describe different congenital heart defects but do not specifically result in cyanosis due to deoxygenated blood entering the systemic circulation:
A. Coarctation of the aorta results in the narrowing of the aorta but does not directly lead to cyanosis from the mixing of oxygen-poor blood.
B. Aortic stenosis involves narrowing of the aortic valve but does not typically result in cyanosis in the same way as Tetralogy of Fallot.
C. Patent ductus arteriosus (PDA) involves a connection between the aorta and pulmonary artery but does not cause cyanosis from mixing to the extent seen in the Tetralogy of Fallot.
A community health nurse is creating an educational pamphlet for a low-income area that has a high rate of obesity. What should the nurse include as recommended actions for a family with a child who has been diagnosed with obesity and hyperlipidemia?
Explanation
For a family with a child diagnosed with obesity and hyperlipidemia, the recommended actions in the educational pamphlet should focus on promoting a healthy lifestyle and managing these conditions effectively. The most appropriate recommendations are:
A. Children-specific heart-healthy diet: Emphasize the importance of a balanced and heart-healthy diet for the child. Include information on portion control, reducing high-fat and high-sugar foods, increasing fruit and vegetable intake, and incorporating whole grains. Encourage families to work with a registered dietitian or nutritionist for personalized dietary guidance.
C. Nutrition guidance from a pediatric specialist: Recommend seeking guidance from a pediatrician or pediatric specialist with expertise in nutrition to develop a personalized nutrition plan for the child. Individualized guidance can help address specific dietary needs and concerns related to obesity and hyperlipidemia.
In contrast, the following options should not be included:
B. Start on statin medication first: Statin medications are typically not the first-line treatment for children with hyperlipidemia, especially if lifestyle modifications can effectively manage the condition. Medication use in children is typically reserved for cases where lifestyle changes alone are insufficient or when there are other medical considerations.
D. Encourage more than 4 hours of screen time per day: Encouraging excessive screen time is not recommended, as it can contribute to a sedentary lifestyle, which is often associated with obesity. Limiting screen time and promoting physical activity are important components of managing obesity.
E. Exercise for at least 3 hours daily: While physical activity is important for managing obesity, recommending over 3 hours of exercise daily may not be realistic or sustainable for most children. Instead, it's better to encourage regular physical activity, such as at least 60 minutes of moderate to vigorous activity daily, as recommended by guidelines for children.
Overall, the focus should be on adopting a healthy lifestyle, including a balanced diet and appropriate physical activity, under the guidance of healthcare professionals, to manage obesity and hyperlipidemia in children.
Which of the following congenital heart diseases require multiple surgeries to correct? (Select All that Apply)
Explanation
The congenital heart diseases that often require multiple surgeries to correct are:
A. Tetralogy of Fallot: Tetralogy of Fallot usually requires staged surgical repairs, with multiple surgeries performed over time to address the various components of the defect.
B. Hypoplastic Left Heart Syndrome: Hypoplastic Left Heart Syndrome typically requires a series of staged surgeries, including the Norwood procedure, Glenn procedure, and Fontan procedure, to manage the condition.
E. Coarctation of the Aorta: Coarctation of the aorta may require multiple surgeries or interventions, depending on the severity of the coarctation and the associated cardiovascular abnormalities.
C. Atrial Septal Defect (ASD) and D. Ventricular Septal Defect (VSD) usually do not require multiple surgeries for correction. These defects can often be repaired with a single surgical intervention or may close spontaneously without surgery in some cases.
It's important to note that the necessity for multiple surgeries can vary based on the individual patient's condition and the specific anatomical details of the heart defect. Treatment plans are typically tailored to each patient's needs and can include a combination of surgical and medical interventions.
A mother calls her pediatrician's office concerned about her 7-month-old son. She gave him peanuts for the second time for lunch and he has vomited three times is coughing and looks flushed. What is the priority of the nurse?
Explanation
The symptoms described, including vomiting, coughing, and looking flushed, are concerning for a potentially severe allergic reaction, which can be life-threatening. This could be indicative of anaphylaxis, a severe allergic reaction that requires immediate medical attention.
Administering CPR (Option D) is not appropriate at this point unless the child becomes unresponsive and stops breathing, which would be a very late sign of anaphylaxis. In such a situation, CPR would be necessary, but the primary focus should be on calling 911 and obtaining immediate medical assistance.
Option A, giving Benadryl, can be part of the treatment for an allergic reaction, but it should not be the first or only action taken in a severe allergic reaction. Immediate medical evaluation and potential administration of epinephrine are more critical.
Option B, recommending symptomatic treatment for the cough, is not appropriate in this situation. The priority is recognizing the potential severity of the allergic reaction and seeking immediate emergency care.
Therefore, the nurse should advise the mother to call 911 to ensure that the child receives prompt medical attention and assessment for anaphylaxis.
Which of the following interventions is not recommended for a pediatric patient with supraventricular tachycardia (SVT)?
Explanation
Cardioversion involves delivering an electrical shock to the heart to restore a normal rhythm. While it may be used for certain types of tachyarrhythmias in adults, it is typically not the first-line treatment for SVT in pediatric patients.
In pediatric patients with SVT, the initial management options often include:
B. Vagal maneuvers: Non-invasive maneuvers like the Valsalva maneuver or carotid sinus massage can be attempted to try and break the SVT rhythm.
C. Adenosine: Adenosine is often the first-line medication used for terminating SVT in pediatric patients. It is given intravenously in a controlled setting under medical supervision.
D. Continue to monitor for 30 minutes: After successful termination of SVT, it's important to continue monitoring the child's heart rhythm and vital signs to ensure that the arrhythmia does not recur.
In pediatric patients, the decision to use cardioversion is usually reserved for situations where other methods, including medications and vagal maneuvers, have not been successful or if the child is unstable. Cardioversion in pediatric patients is performed under sedation or anesthesia to minimize discomfort.
Therefore, while cardioversion may be used in some cases, it is not the initial or most common approach for treating SVT in pediatric patients, making option A the answer to the question.
A 2-month-old patient has a history of phimosis What statement by the father indicates a need for further teaching?
Explanation
Phimosis is a condition in which the foreskin of the penis is tight or difficult to retract over the glans (head of the penis). It is normal for infants and young boys to have a non-retractable foreskin, and it usually resolves naturally as they grow. Pulling back the foreskin forcefully or attempting to clean under it in an infant can cause injury, pain, and even infection.
The correct approach is to gently clean the external genitalia with mild soap and water, but the foreskin should not be forcibly retracted in an infant. The foreskin will gradually become more retractable on its own as the child grows.
The other statements are generally appropriate:
A. "This is a normal finding as my son is uncircumcised": Phimosis is more common in uncircumcised males, and it is often a normal developmental variation in infants.
B. "This means that there is a narrowing of his torch that could lead to an infection": This statement recognizes the possibility of complications related to phimosis, such as the risk of infection, which is accurate.
D. "If this continues to be an issue, we may have him circumcised": Circumcision may be considered in cases where phimosis persists and causes problems, but it is usually not recommended during infancy unless medically necessary. This statement acknowledges a potential treatment option.
Which of the following should be included when developing a teaching plan to prevent urinary tract infection?
Explanation
When developing a teaching plan to prevent urinary tract infections (UTIs), the following recommendations should be included:
B. Emptying bladder with urination: It's important to encourage regular and complete emptying of the bladder to help flush out bacteria and prevent their buildup.
D. Avoiding bubble baths and tight clothing: Bubble baths and tight clothing can irritate the genital area and increase the risk of UTIs, especially in children. Recommending gentle hygiene practices and loose-fitting clothing can help reduce this risk.
F. Maintaining adequate fluid intake: Staying well-hydrated can help dilute urine and flush out bacteria from the urinary tract, reducing the risk of infection.
The following recommendations are not appropriate or effective for preventing UTIs:
A. Keeping urine alkaline by avoiding acidic beverages: While it's true that some individuals believe that altering urine pH can prevent UTIs, this is not a reliable or evidence-based approach. It's not recommended to manipulate urine pH in an attempt to prevent UTIs.
C. Wearing underwear made of synthetic material such as nylon: The choice of underwear material is not a primary factor in preventing UTIs. However, it's generally recommended to wear breathable cotton underwear as it can help maintain a dry environment in the genital area.
E. Avoiding urination before and after intercourse: On the contrary, urinating before and after sexual intercourse is a recommended practice to help flush out any bacteria that may have entered the urethra during sexual activity.
In summary, teaching about proper bladder emptying, avoiding irritants like bubble baths and tight clothing, and maintaining adequate hydration are key components of preventing UTIs.
Nurse Ashley is caring for a 6-year-old female patient in an outpatient doctor's office
Patient Results
Leukocytes:
Nitrates
Urobil
Protein
PH 6.5
Blood
Spec Gravity 1.020
Ketones
Bilirubin
Glucose
Based on the patient's presentation, what would the nurse anticipate her diagnosis to be?
Explanation
The presence of leukocytes, nitrates, and blood in the urine, along with a urinary pH of 6.5, is suggestive of a urinary tract infection (UTI). Additionally, symptoms such as frequent urination, pain or discomfort during urination, or other urinary symptoms may also be present in UTIs.
The other options (A, B, and D) are less likely based on the provided information:
A. Nephrotic syndrome typically presents with significant proteinuria and edema but may not show the specific findings seen in a UTI urinalysis.
B. Acute glomerulonephritis may have different urinalysis findings, including hematuria and proteinuria, but the presence of nitrates and leukocytes in the urine is not a typical feature.
D. Diabetes mellitus Type 1 may have glucose in the urine, but the presence of nitrates, leukocytes, and blood in the urine is more indicative of a UTI than diabetes.
Sign Up or Login to view all the 35 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

