ATI PN Adult Medical Surgical 2020 with NGN
Total Questions : 78
Showing 25 questions, Sign in for moreA nurse is caring for a client who is at risk for anaphylaxis due to bee stings. When reinforcing teaching about the use of an automatic epinephrine injector, which of the following actions is the priority?
Explanation
Choice A: Instructing the client to store the injector at room temperature is not the priority because it is not a life-saving action. Storing the injector at room temperature is important to maintain its effectiveness and prevent damage from heat or cold. However, it is not as urgent as seeking medical attention or recognizing anaphylaxis.
Choice B: Informing the client to seek medical attention following administration of the injection is the priority because it is a life-saving action. Seeking medical attention following administration of the injection is essential to prevent further complications or recurrence of anaphylaxis. Anaphylaxis is a severe allergic reaction that can cause symptoms such as difficulty breathing, swelling, rash, or shock. It can be fatal if not treated promptly and properly. Epinephrine is a medication that can reverse some of the symptoms of anaphylaxis by constricting blood vessels, relaxing airways, and increasing heart rate. However, epinephrine is not a cure for anaphylaxis and its effects may wear off after 15 to 20 minutes. Therefore, the client should seek medical attention as soon as possible after using the injector.
Choice C: Having the client perform a return demonstration of the equipment is not the priority because it is not a life-saving action. Having the client perform a return demonstration of the equipment is important to assess the client's understanding and ability to use the injector correctly. However, it is not as urgent as seeking medical attention or recognizing anaphylaxis.
Choice D: Reviewing the signs of anaphylaxis with the client is not the priority because it is not a life-saving action. Reviewing the signs of anaphylaxis with the client is important to educate the client about how to identify and respond to an allergic reaction. However, it is not as urgent as seeking medical attention or using the injector.
A nurse is assisting in the care of a client who has a pulmonary embolism and is experiencing dyspnea. Which of the following actions should the nurse take first?
Explanation
Choice A reason: Administering heparin to the client is an important intervention, but it is not the first action the nurse should take. Heparin is an anticoagulant that prevents further clot formation, but it does not dissolve existing clots or improve oxygenation.
Choice B reason: Encouraging the client to cough and deep breathe is a helpful measure to promote lung expansion and expectoration of secretions, but it is not the first action the nurse should take. Coughing and deep breathing may also increase the client's dyspnea and anxiety.
Choice C reason: Obtaining the client's vital signs is a necessary step to monitor the client's condition, but it is not the first action the nurse should take. Vital signs may indicate hypoxia, tachycardia, hypotension, or other signs of shock, but they do not address the immediate problem of impaired gas exchange.
Choice D reason: Placing the client in high-Fowler's position is the first action the nurse should take. This position allows for maximum lung expansion and improves oxygenation. It also reduces venous return and cardiac workload, which may decrease pulmonary artery pressure and right ventricular strain.
A nurse is caring for a client who has pneumonia with dyspnea. The client's ABG results are pH 7.30, PaCO2 50 mm Hg, HCO3 26 mEq/L. The nurse should recognize that the client has which of the following acid-base imbalances?
Explanation
Choice A reason: Metabolic alkalosis is a condition in which the pH is high and the HCO3 is high. This can be caused by excessive vomiting, diuretic use, or ingestion of antacids. The client's ABG results do not indicate metabolic alkalosis.
Choice B reason: Respiratory alkalosis is a condition in which the pH is high and the PaCO2 is low. This can be caused by hyperventilation, anxiety, or fever. The client's ABG results do not indicate respiratory alkalosis.
Choice C reason: Metabolic acidosis is a condition in which the pH is low and the HCO3 is low. This can be caused by diabetic ketoacidosis, renal failure, or diarrhea. The client's ABG results do not indicate metabolic acidosis.
Choice D reason: Respiratory acidosis is a condition in which the pH is low and the PaCO2 is high. This can be caused by hypoventilation, airway obstruction, or lung disease. The client's ABG results indicate respiratory acidosis, which means that the client has impaired gas exchange and retention of carbon dioxide.
A nurse is reviewing laboratory values of a client who has severe dyspnea. Which of the following laboratory values indicates heart failure?
Explanation
Choice A reason: Potassium 4.0 mEq/L is a normal value for serum potassium. Potassium is an electrolyte that regulates nerve and muscle function, cardiac rhythm, and fluid balance. Abnormal levels of potassium can indicate renal dysfunction, dehydration, or acid-base imbalance, but not heart failure.
Choice B reason: Calcium 9.0 mg/dL is a normal value for serum calcium. Calcium is an electrolyte that regulates bone health, muscle contraction, blood clotting, and nerve transmission. Abnormal levels of calcium can indicate parathyroid dysfunction, vitamin D deficiency, or malignancy, but not heart failure.
Choice C reason: Sodium 140 mEq/L is a normal value for serum sodium. Sodium is an electrolyte that regulates fluid balance, blood pressure, and nerve and muscle function. Abnormal levels of sodium can indicate dehydration, fluid overload, or hormonal imbalance, but not heart failure.
Choice D reason: Brain natriuretic peptide (BNP) 275 pg/mL is an elevated value for serum BNP. BNP is a hormone that is released by the heart when it is stretched or stressed due to increased pressure or volume overload. BNP causes diuresis, vasodilation, and decreased blood pressure to reduce the workload of the heart. Elevated levels of BNP indicate heart failure, which means that the heart cannot pump enough blood to meet the body's needs.
A nurse is contributing to the plan of care for a client who has heart failure. Which of the following actions should the nurse include in the plan?
Explanation
Choice A reason: Obtaining weight weekly is not sufficient for monitoring fluid status in a client who has heart failure. The nurse should obtain weight daily at the same time using the same scale and compare it with the baseline weight. A weight gain of more than 2 kg (4.4 lb) in a week or more than 1 kg (2.2 lb) in a day indicates fluid retention and worsening heart failure.
Choice B reason: Measuring vital signs every 8 hr may not be frequent enough for detecting changes in a client who has heart failure. The nurse should measure vital signs at least every 4 hr or more often as needed based on the client's condition and response to treatment. Vital signs may indicate hypoxia, tachycardia, hypotension, or other signs of shock.
Choice C reason: Allowing frequent rest periods is an appropriate action for a client who has heart failure. Rest periods reduce oxygen demand and cardiac workload and prevent fatigue and dyspnea. The nurse should schedule rest periods between activities and provide assistance as needed.
Choice D reason: Encouraging fluids is not advisable for a client who has heart failure. Fluid intake should be restricted to prevent fluid overload and pulmonary edema. The nurse should monitor the client's fluid intake and output, assess for signs of fluid retention, and educate the client about limiting sodium and fluid intake.
A nurse is performing tracheostomy care for a client who has a chronic tracheostomy. Which of the following actions should the nurse take?
Explanation
Choice A reason: Allowing space for one finger to be placed under the tube ties is a correct action for tracheostomy care. This ensures that the tube ties are not too tight, which can cause skin breakdown, pressure necrosis, or impaired circulation. The tube ties should also not be too loose, which can cause accidental dislodgement of the tube.
Choice B reason: Applying suction pressure while inserting the catheter into the trachea is an incorrect action for tracheostomy care. This can cause trauma to the tracheal mucosa and increase the risk of infection and bleeding. The nurse should apply suction pressure only while withdrawing the catheter and rotate it gently to remove secretions.
Choice C reason: Suctioning the client for 20 seconds with each pass is an incorrect action for tracheostomy care. This can cause hypoxia, bradycardia, or cardiac arrest due to vagal stimulation. The nurse should suction the client for no more than 10 to 15 seconds with each pass and allow at least 30 seconds between passes for oxygenation.
Choice D reason: Cleansing around the stoma with povidone-iodine is an incorrect action for tracheostomy care. Povidone-iodine is a strong antiseptic that can irritate the skin and cause allergic reactions. The nurse should cleanse around the stoma with normal saline or sterile water and apply a thin layer of water-soluble lubricant to protect the skin.
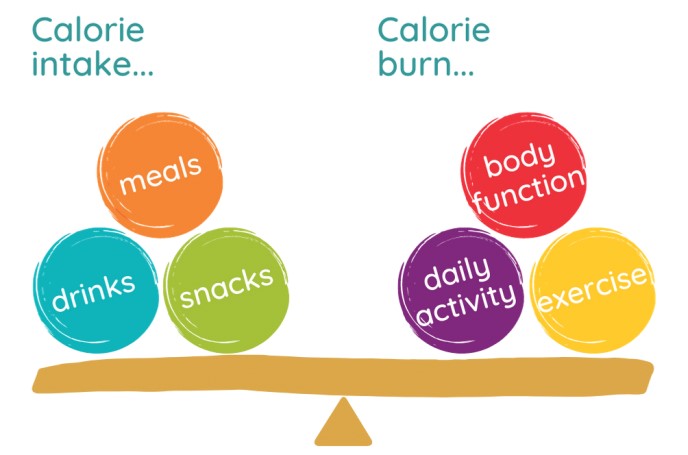
A nurse is reinforcing teaching with a client who wants to lose 0.9 kg (2 lb) of body fat per week. The nurse knows that 0.45 kg (1 lb) of body fat is equal to 3,500 calories. The nurse should instruct the client to reduce his daily caloric intake by how many calories? (Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
To lose 0.9 kg (2 lb) of body fat per week, the client needs to create a weekly caloric deficit of 7,000 calories (3,500 x 2).
This means that the client needs to consume 7,000 calories less than he burns in a week.
To achieve this, the client needs to reduce his daily caloric intake by 1,000 calories (7,000 / 7).
For example, if the client normally consumes 2,500 calories per day, he should reduce it to 1,500 calories per day.
A nurse is reinforcing teaching with a client who will undergo a colonoscopy the following week. Which of the following instructions should the nurse include?
Explanation
Choice A reason: Administering enemas 2 days before the procedure is not necessary for colonoscopy preparation. Enemas are usually given on the day of or the night before the procedure to empty the bowel and improve visibility.
Choice B reason: Restricting the diet to clear liquids for 1 to 3 days before the procedure is an important instruction for colonoscopy preparation. Clear liquids include water, broth, tea, coffee, juice without pulp, and gelatin. This helps to prevent solid food from remaining in the colon and interfering with the examination.
Choice C reason: Expecting the provider to schedule another procedure to remove any polyps is not a valid instruction for colonoscopy preparation. Polyps are abnormal growths in the lining of the colon that can be benign or malignant. The provider can usually remove any polyps during the colonoscopy using a snare or a biopsy forceps.
Choice D reason: Not eating or drinking anything except water for 12 hr before the procedure is not enough for colonoscopy preparation. The client should stop eating or drinking anything at least 4 hr before the procedure or as instructed by the provider. This helps to prevent aspiration and vomiting during sedation.
A nurse is reinforcing teaching with a client who is 24 hr postoperative following a total hip arthroplasty. Which of the following instructions should the nurse include in the teaching?
Explanation
Choice A reason: Performing range of motion by adducting the hip is an incorrect instruction for a client who had a total hip arthroplasty. Adduction is moving the leg toward the midline of the body, which can cause dislocation of the prosthesis. The nurse should instruct the client to perform range of motion by abducting (moving away from midline), flexing (bending), and extending (straightening) the hip as prescribed by physical therapy.
Choice B reason: Sitting in a straight-backed chair is a correct instruction for a client who had a total hip arthroplasty. This position helps to maintain proper alignment and stability of the hip joint and prevents excessive flexion or rotation that can cause dislocation. The nurse should also instruct the client to avoid crossing legs, bending forward more than 90 degrees, or twisting at the waist.
Choice C reason: Cleansing the surgical incision with hydrogen peroxide is an incorrect instruction for a client who had a total hip arthroplasty. Hydrogen peroxide is a harsh agent that can damage healthy tissue and delay healing. The nurse should instruct the client to cleanse the incision with mild soap and water or as directed by the provider and keep it dry and covered with sterile dressing.
Choice D reason: Applying moist heat to the incision while in bed is an incorrect instruction for a client who had a total hip arthroplasty. Moist heat can increase swelling, inflammation, and infection risk at the incision site. The nurse should instruct the client to apply ice packs or cold compresses to the incision as needed to reduce pain and swelling.
A nurse is reviewing vital signs obtained by an assistive personnel on a group of clients. The previous vital signs for each of the clients were obtained 4 hr earlier. Which of the following changes should the nurse identify as the priority finding?
Explanation
Choice A reason: Temperature change from 36.6° C (97.8° F) to 38.8° C (101.9° F) is a significant finding that indicates fever, which can be caused by infection, inflammation, or other conditions. However, this is not the priority finding because fever is usually a secondary response to an underlying problem and can be treated with antipyretics and fluids.
Choice B reason: Heart rate change from 110/min to 68/min is a notable finding that indicates bradycardia, which can be caused by medication, vagal stimulation, hypothermia, or cardiac dysfunction. However, this is not the priority finding because bradycardia may not be symptomatic or life-threatening unless it is accompanied by hypotension, chest pain, or altered mental status.
Choice C reason: Blood pressure change from 118/78 mm Hg to 86/50 mm Hg is the priority finding that indicates hypotension, which can be caused by blood loss, dehydration, shock, or medication. Hypotension can impair tissue perfusion and oxygenation and lead to organ failure and death if not corrected promptly. The nurse should assess the client for signs of shock, such as tachycardia, tachypnea, pallor, diaphoresis, or confusion, and initiate interventions to restore blood pressure and circulation.
Choice D reason: Respiratory rate change from 12/min to 20/min is a minor finding that indicates tachypnea, which can be caused by anxiety, pain, fever, or respiratory distress. However, this is not the priority finding because tachypnea may be a compensatory mechanism to increase oxygen delivery or eliminate carbon dioxide and may not affect gas exchange or acid-base balance unless it is severe or prolonged.
A nurse is caring for a client who has partial-thickness burns on 50% of his body and is receiving total parenteral nutrition. The nurse should actively monitor the client for which of the following?
Explanation
Choice A reason: Increased serum glucose levels are a common complication of total parenteral nutrition (TPN), which is a form of intravenous feeding that provides high amounts of calories, proteins, and other nutrients. TPN can cause hyperglycemia, especially in clients who have stress, infection, or diabetes. The nurse should monitor the client's blood glucose levels regularly and adjust the infusion rate or insulin dosage as prescribed.
Choice B reason: Intermittent abdominal pain is not a typical complication of TPN, but it may indicate other problems such as bowel obstruction, perforation, or ischemia. The nurse should assess the client's abdomen for distension, tenderness, rigidity, or guarding and report any abnormal findings to the provider.
Choice C reason: Absent bowel sounds are not a direct complication of TPN, but they may indicate paralytic ileus, which is a temporary loss of bowel motility. Paralytic ileus can occur after surgery, trauma, or burns and can cause nausea, vomiting, constipation, or abdominal distension. The nurse should auscultate the client's bowel sounds every 4 hr and encourage early ambulation and oral intake as tolerated.
Choice D reason: Decreased calcium levels are not a common complication of TPN, but they may occur in clients who have hypoparathyroidism, renal failure, or malabsorption. Low calcium levels can cause muscle cramps, tetany, seizures, or cardiac arrhythmias. The nurse should monitor the client's serum calcium levels and administer calcium supplements as prescribed.
A nurse is reinforcing teaching with a client who has angina. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A reason: Taking four nitroglycerin sublingual tablets if having chest pain is an incorrect statement that indicates a lack of understanding of the teaching. Nitroglycerin is a medication that dilates the coronary arteries and relieves angina by improving blood flow to the heart. The client should take one nitroglycerin tablet every 5 minutes for up to three doses if having chest pain. If the pain persists after three doses, the client should call emergency response.
Choice B reason: Notifying emergency response if having sudden jaw pain is a correct statement that indicates an understanding of the teaching. Jaw pain is one of the possible signs of a heart attack, which is a life-threatening condition that occurs when the blood supply to the heart is blocked. Other signs of a heart attack include chest pain, arm pain, shortness of breath, nausea, sweating, or dizziness. The client should seek immediate medical attention if experiencing any of these symptoms.
Choice C reason: Waiting 30 minutes before taking action if having heartburn is an incorrect statement that indicates a lack of understanding of the teaching. Heartburn is a burning sensation in the chest or throat that can be caused by acid reflux, gastritis, or other gastrointestinal disorders. However, heartburn can also mimic or mask angina or a heart attack, especially in women, elderly, or diabetic clients. The client should not ignore or delay seeking help if having chest discomfort that may be related to cardiac problems.
Choice D reason: Having hot, dry, and flushed skin if having a heart attack is an incorrect statement that indicates a lack of understanding of the teaching. Hot, dry, and flushed skin is not a typical sign of a heart attack, but it may indicate fever, dehydration, or allergic reaction. The client should monitor his temperature and hydration status and report any abnormal findings to the provider.
A nurse in an urgent care facility is collecting data from a client who was stung by a wasp. Which of the following findings indicates the client is experiencing anaphylaxis?
Explanation
Choice A reason: Hypertension is not a typical symptom of anaphylaxis, which usually causes hypotension due to vasodilation and fluid leakage from the blood vessels.
Choice B reason: Difficulty swallowing is a typical symptom of anaphylaxis, which causes swelling of the throat and tongue due to histamine release and inflammation. This is a sign of airway obstruction, which can be life-threatening in anaphylaxis. The other choices are not specific to anaphylaxis and could be caused by other conditions.
Choice C reason: Bilateral tinnitus is not a typical symptom of anaphylaxis, which usually causes ear pain or itching due to allergic inflammation of the ear canal.
Choice D reason: Petechial rash on the abdomen is not a typical symptom of anaphylaxis, which usually causes urticaria (hives) or angioedema (swelling) on the skin. Petechiae are small red or purple spots caused by bleeding under the skin, which can be a sign of a blood disorder or infection.
A nurse is caring for a client in hospice care who is dying. The client's partner expresses concern that the client is sleeping more than in the previous week. Which of the following is an appropriate response by the nurse?
Explanation
Choice A reason: This is not an appropriate response because it implies that the nurse does not acknowledge or validate the partner's feelings. The nurse should provide emotional support and education to the partner about the normal changes that occur at the end of life.
Choice B reason: This is not an appropriate response because it may cause more distress and fatigue to the client and the partner. The nurse should respect the client's need for rest and allow them to sleep as much as they want.
Choice C reason: This is not an appropriate response because it may interfere with the client's comfort and quality of life. The nurse should avoid unnecessary interventions and medications that may have adverse effects or cause more harm than benefit.
Choice D reason: This is the correct answer because it shows empathy and compassion to the partner and the client. The nurse should encourage the partner to spend time with the client and offer nonverbal communication such as holding hands, stroking hair, or playing soft music.
A nurse is reinforcing teaching with a client who has psoriasis. Which of the following treatment options should the nurse include in the teaching?
Explanation
Choice A reason: This is not an appropriate treatment option for psoriasis because oil-based ointments can occlude the skin and worsen the inflammation and scaling.
Choice B reason: This is the correct answer because phototherapy, or exposure to ultraviolet light, can help reduce the symptoms of psoriasis by slowing down the growth of skin cells and decreasing the immune response.
Choice C reason: This is not an appropriate treatment option for psoriasis because benzoyl peroxide is used for acne and can irritate and dry out the skin.
Choice D reason: This is not an appropriate treatment option for psoriasis because dermabrasion, or removal of the outer layer of the skin, can cause scarring and infection.
A nurse is collecting data from a client about her current pain status. Which of the following questions should the nurse ask to determine the quality of the client's pain?
Explanation
Choice A reason: This question does not assess the quality of the pain, but the intensity or severity of the pain.
Choice B reason: This question assesses the quality of the pain, which is how the client describes or characterizes the pain, such as sharp, dull, burning, throbbing, etc.
Choice C reason: This question does not assess the quality of the pain, but the presence or absence of pain.
Choice D reason: This question does not assess the quality of the pain, but the consistency or variability of pain.
A nurse is reinforcing teaching with a client about strategies to prevent hypertension. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A reason: This is not an accurate statement because a BMI of 30 indicates obesity, which is a risk factor for hypertension. The client should aim to lose weight and achieve a healthy BMI of 18.5 to 24.9.
Choice B reason: This is an accurate statement because reducing sodium intake can help lower blood pressure and prevent hypertension. The American Heart Association recommends consuming no more than 2,300 milligrams of sodium per day and ideally less than 1,500 milligrams.
Choice C reason: This is not an accurate statement because the client should exercise for at least 30 minutes most days of the week, not just three times per week. Physical activity can help lower blood pressure and prevent hypertension by improving cardiovascular health and reducing stress.
Choice D reason: This is not an accurate statement because the client should consume fish at least twice per week, not just once per week. Fish is a good source of omega-3 fatty acids, which can help lower blood pressure and prevent hypertension by reducing inflammation and improving blood vessel function.
A nurse is reinforcing teaching with a client who is recovering from gastroenteritis and is beginning oral intake. Which of the following foods should the nurse recommend?
Explanation
Choice A reason: This is the correct answer because lime ice popsicle is a clear liquid that can help hydrate the client and soothe the stomach. Clear liquids are recommended for the first 24 hours after gastroenteritis to prevent dehydration and nausea.
Choice B reason: This is not a good choice because vanilla pudding is a dairy product that can be hard to digest and cause diarrhea or cramps. Dairy products should be avoided until the client has no symptoms for at least 48 hours.
Choice C reason: This is not a good choice because orange juice is acidic and can irritate the stomach and cause vomiting or heartburn. Acidic foods and drinks should be avoided until the client has no symptoms for at least 48 hours.
Choice D reason: This is not a good choice because cream of broccoli soup is high in fat and fiber that can be hard to digest and cause gas or bloating. High-fat and high-fiber foods should be avoided until the client has no symptoms for at least 48 hours.
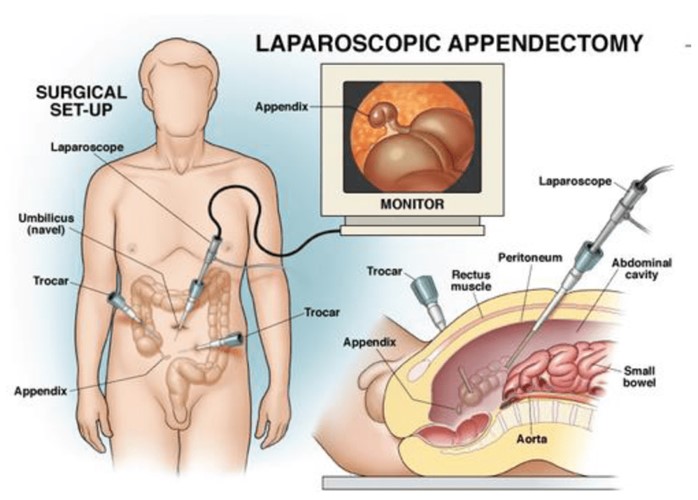
A nurse is caring for a client who is 1 day postoperative following an appendectomy. Which of the following findings should the nurse report?
Explanation
Choice A reason: This finding does not need to be reported because it is within the normal range of temperature for adults (36.5° C to 37.5° C or 97.7° F to 99.5° F). A mild elevation in temperature may occur after surgery due to inflammation or dehydration and does not indicate infection unless it exceeds 38° C (100.4° F).
Choice B reason: This finding does not need to be reported because it is expected after abdominal surgery due to anesthesia, pain medication, or decreased mobility that can slow down bowel motility. Hypoactive bowel sounds are defined as less than five sounds per minute. The nurse should encourage the client to ambulate, drink fluids, and eat high-fiber foods to stimulate bowel function.
Choice C reason: This finding needs to be reported because it indicates a possible infection at the surgical site. Red streaks along the incision are a sign of cellulitis, which is a bacterial infection of the skin and underlying tissue that can spread rapidly and cause serious complications. The nurse should also check for other signs of infection such as warmth, swelling, pain, pus, or foul odor at the incision site.
Choice D reason: This finding does not need to be reported because it is normal during the first few days after surgery. Serosanguineous drainage is a mixture of blood and clear fluid that leaks from the wound as part of the healing process. The nurse should monitor the amount, color, and consistency of the drainage and change the dressing as needed.
A nurse is contributing to the plan of care for a client who has disuse syndrome following cast removal from a lower extremity. Which of the following referrals should the nurse include in the plan of care?
Explanation
Choice A reason: This is the correct answer because an occupational therapist can help the client regain function and mobility in the affected limb, prevent contractures and muscle atrophy, and provide adaptive equipment and strategies to perform daily activities.
Choice B reason: This is not an appropriate referral for this client because a social worker can help with psychosocial issues, financial resources, and community services, but not with physical rehabilitation.
Choice C reason: This is not an appropriate referral for this client because a herbalist can provide alternative or complementary therapies using plants or herbs, but not with evidence-based interventions for disuse syndrome.
Choice D reason: This is not an appropriate referral for this client because a dietitian can help with nutritional counseling and dietary modifications, but not with physical rehabilitation.
A nurse is reinforcing teaching with a client who has a BMI of 32 and wants to lose weight. Which of the following statements should the nurse make to promote the client's weight loss?
Explanation
Choice A reason: This is not a good statement because refined grains are processed carbohydrates that have low nutritional value and high glycemic index, which can increase blood sugar and insulin levels and promote fat storage. The nurse should advise the client to choose whole grains instead, which are rich in fiber, vitamins, minerals, and antioxidants.
Choice B reason: This is not a good statement because rewarding oneself with special foods can undermine the weight loss efforts and create a negative association between food and achievement. The nurse should suggest other ways of rewarding oneself that are not food-related, such as buying new clothes, going to the movies, or getting a massage.
Choice C reason: This is not a good statement because planning meals so up to 40 percent of calories come from fats can exceed the recommended intake of fats, which is 20 to 35 percent of total calories. The nurse should also emphasize the importance of choosing healthy fats, such as monounsaturated and polyunsaturated fats, over saturated and trans fats, which can increase the risk of cardiovascular disease.
Choice D reason: This is a good statement because consuming 500 fewer calories per day than the estimated calorie needs can create a moderate energy deficit that can lead to a gradual and sustainable weight loss of about one pound per week. The nurse should also encourage the client to increase physical activity to burn more calories and preserve lean muscle mass.
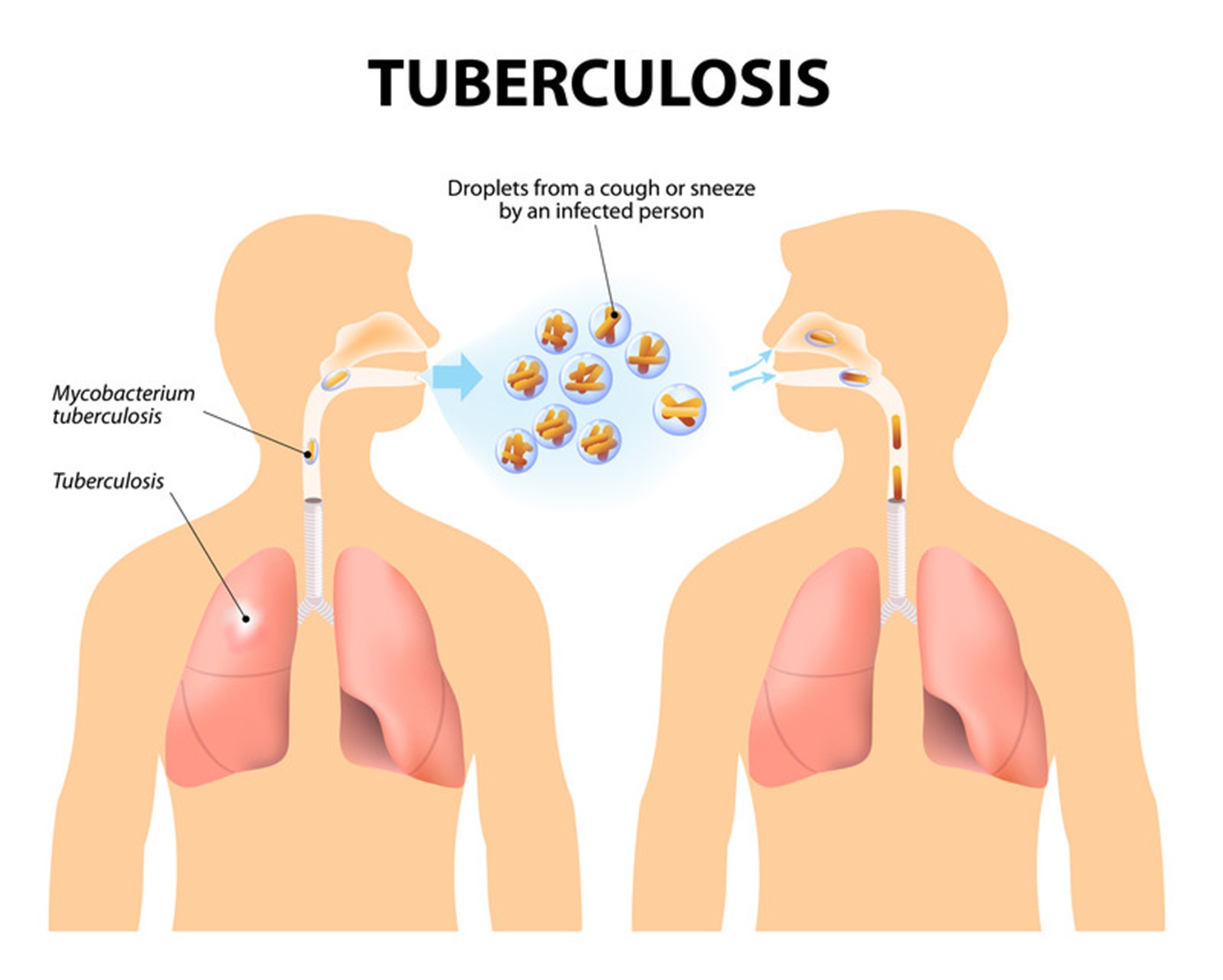
A nurse is collecting admission history data from a client who is in a semi-private room. Which of the following data is the priority for the nurse to address?
Explanation
Choice A reason: This data is not the priority for the nurse to address because it does not pose an immediate threat to the client's health or safety. However, the nurse should assess the client's anxiety level and provide coping strategies and emotional support as needed.
Choice B reason: This data is the priority for the nurse to address because it indicates a potential infection that can be contagious and harmful to the client and others in the room. The nurse should isolate the client in a private room with negative pressure ventilation and wear personal protective equipment when entering the room. The nurse should also notify the infection control team and obtain sputum samples for testing.
Choice C reason: This data is not the priority for the nurse to address because it does not pose an immediate threat to the client's health or safety. However, the nurse should ask about the frequency, severity, duration, triggers, and treatment of the migraine headaches and provide pain relief and comfort measures as needed.
Choice D reason: This data is not the priority for the nurse to address because it does not pose an immediate threat to the client's health or safety. However, the nurse should inquire about the possible causes, such as urinary tract infection, diabetes mellitus, prostate enlargement, or medication side effects, and monitor the client's fluid intake and output and urine characteristics.
A nurse is assisting with discharge teaching for a client who requires oropharyngeal suctioning at home. The nurse should ensure that which of the following equipment is available for use at home?
Explanation
Choice A reason: This is the correct answer because a Yankauer catheter is a rigid, curved suction device that is used to remove secretions from the mouth and throat. It is easy to handle and control and can be attached to a portable suction machine at home.
Choice B reason: This is not an appropriate equipment for oropharyngeal suctioning at home because sterile gloves are not necessary for this procedure. The nurse should instruct the client to use clean gloves and wash their hands before and after suctioning.
Choice C reason: This is not an appropriate equipment for oropharyngeal suctioning at home because water-soluble lubricant is not needed for this procedure. The nurse should instruct the client to moisten the tip of the catheter with sterile saline or water before inserting it into the mouth.
Choice D reason: This is not an appropriate equipment for oropharyngeal suctioning at home because oropharyngeal airway is not used for this procedure. An oropharyngeal airway is a device that keeps the tongue from blocking the airway and is used for unconscious clients who are not intubated.
A nurse is reinforcing teaching with a client who is scheduled to have a colonoscopy. Which of the following information should the nurse include in the teaching?
Explanation
Choice A reason: This is an accurate information because moderate sedation, also known as conscious sedation, is a type of anesthesia that reduces anxiety and pain during the colonoscopy without causing loss of consciousness. The nurse should inform the client that they will need someone to drive them home after the procedure and that they may experience some drowsiness, nausea, or sore throat.
Choice B reason: This is not an accurate information because the client should drink only clear liquids, such as water, tea, broth, or juice, until 4 hours before the procedure. Full liquids, such as milk, cream, or soup, can interfere with the bowel preparation and obscure the visibility of the colon.
Choice C reason: This is not an accurate information because the client should drink the liquid bowel preparation as prescribed by the provider, usually cold or at room temperature. Warming the liquid bowel preparation may alter its effectiveness and taste.
Choice D reason: This is not an accurate information because the client will lie on their left side for the procedure, not on their right side. Lying on the left side allows better access and visualization of the colon by the endoscope.
A nurse is obtaining a medication history from a client who is to start taking nitroglycerin for chest discomfort with activity. Which of the following medications should the nurse instruct the client to avoid taking within 24 hours of using nitroglycerin?
Explanation
Choice A reason: This medication does not need to be avoided within 24 hours of using nitroglycerin because it does not interact with nitroglycerin. Metformin is an oral antidiabetic drug that lowers blood glucose levels by decreasing hepatic glucose production and increasing insulin sensitivity.
Choice B reason: This medication does not need to be avoided within 24 hours of using nitroglycerin because it does not interact with nitroglycerin. Atorvastatin is a statin drug that lowers blood cholesterol levels by inhibiting an enzyme involved in cholesterol synthesis.
Choice C reason: This medication does not need to be avoided within 24 hours of using nitroglycerin because it does not interact with nitroglycerin. Omeprazole is a proton pump inhibitor drug that lowers stomach acid levels by blocking an enzyme involved in acid secretion.
Choice D reason: This medication needs to be avoided within 24 hours of using nitroglycerin because it can interact with nitroglycerin and cause severe hypotension and syncope. Sildenafil is a phosphodiesterase inhibitor drug that treats erectile dysfunction by increasing blood flow to the penis by relaxing smooth muscle cells.

Sign Up or Login to view all the 78 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

