ATI PN Capstone Proctored Comprehensive Assessment 2020 B
Total Questions : 58
Showing 25 questions, Sign in for moreA nurse is caring for a client who has dementia.
Which of the following actions should the nurse take to promote communication?
Explanation
Face the client at eye level when communicating.

This is because eye contact helps to establish rapport and trust with the client who has dementia and shows respect and attention. Facing the client at eye level also reduces distractions and background noise that might interfere with communication.
Choice B is wrong because offering correction of incorrect client statements can increase confusion, frustration, and agitation in the client who has dementia. Instead of correcting the client, the nurse should acknowledge their feelings and try to understand their perspective.
Choice C is wrong because reorienting the client to date and time with each encounter can be stressful and ineffective for the client who has dementia. Reorientation may work in the early stages of dementia, but as the disease progresses, the client may lose their ability to retain new information and may become more disoriented. Instead of reorienting the client, the nurse should use orienting names or labels whenever possible, such as “Your son, Jack” .
Choice D is wrong because avoiding using gestures when communicating with the client who has dementia can limit the nurse’s ability to convey meaning and emotion. Gestures can help to supplement verbal communication and provide cues for the client who has difficulty understanding words. However, the nurse should avoid using gestures that might be misinterpreted or threatening to the client, such as pointing or waving .
A nurse is contributing to the plan of care for a client who is postoperative following a below-the-knee amputation.
Which of the following strategies should the nurse include to help the client progress toward acceptance of this body image alteration?
Explanation
Encourage the client to visit with someone who has had an amputation.

This strategy can help the client cope with the loss of a body part and learn from the experience of others who have gone through a similar situation.
Choice A is wrong because suggesting that the client wear facility clothing until the prosthesis fitting can delay the client’s acceptance of the body image alteration and increase the risk of infection.
Choice C is wrong because discouraging the client from touching the residual limb for the first week can interfere with the healing process and prevent the client from becoming familiar with the new body part.
Choice D is wrong because reassuring the client that the rehabilitation program is optional can discourage the client from participating in physical therapy and hinder the recovery and adaptation.
A nurse in a provider’s office is reinforcing teaching with a client about performing testicular self-examination.
Which of the following instructions should the nurse include?
Explanation
Examine your testicles after a warm shower.
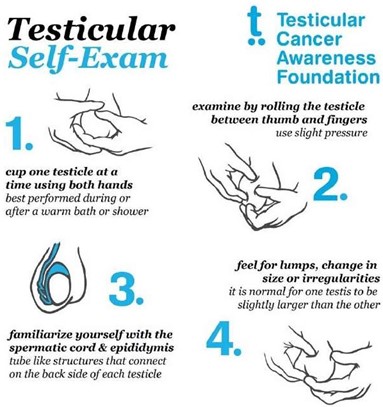
This is because a warm shower will relax the scrotum and the muscles holding the testicles, making an exam easier. You should gently roll the scrotum with your fingers to feel the surface of each testicle and check for any lumps, bumps, swelling, hardness or other changes.
Choice A is wrong because you should perform the self-examination every month, not every 3 months.
This will help you notice any changes over time.
Choice C is wrong because you should not palpate both testicles firmly with your fingertips. You should use a gentle touch and avoid squeezing or pressing too hard.
Choice D is wrong because you should not apply a cool compress to the scrotum prior to examination. This will make the scrotum contract and tighten, making an exam more difficult.
A nurse is caring for a client who is receiving oxygen via nasal cannula at 4 L/min. Which of the following actions should the nurse take?
Explanation
Clean the cannula prongs daily.

This is because the nasal cannula can become contaminated with bacteria and mucus, which can cause infection and irritation of the nasal mucosa. Cleaning the cannula prongs daily with soap and water can prevent these complications.
Choice A is wrong because humidifiers can help moisten the dry oxygen and prevent nasal dryness and bleeding. Humidifiers should be used for oxygen flow rates higher than 4 L/min.
Choice B is wrong because the cannula prongs should be positioned curving downward in the nose, not upward. This allows for better alignment with the natural direction of airflow and reduces the risk of dislodgement.
Choice D is wrong because keeping the oxygen tubing off the floor is not a specific action for nasal cannula use. It is a general safety measure to prevent tripping and contamination of the tubing.
A nurse on a postpartum unit is caring for a group of clients. Which of the following clients is the nurse’s priority?
Explanation
A client who is 1 day postpartum and has not voided in 8 hr. This client is at risk of urinary retention, bladder distension, and infection due to the effects of epidural anesthesia, perineal trauma, and fluid shifts after delivery. The nurse should assess the client’s bladder and catheterize if necessary.
Choice A is wrong because a client who is 2 days postpartum and whose fundus is 2 to 4 cm below the umbilicus is showing a normal finding.
The fundus should descend about 1 to 2 cm per day after delivery and be nonpalpable by day 10.
Choice B is wrong because a client who is 3 days postpartum and has not had a bowel movement since prior to admission is not uncommon.
Constipation is a common problem after delivery due to decreased peristalsis, dehydration, and fear of pain.
The nurse should encourage fluid intake, fiber intake, and early ambulation to promote bowel function.
Choice C is wrong because a client who is 4 days postpartum and has lochia serosa is also showing a normal finding.
Lochia serosa is the pinkish-brown discharge that occurs from day 4 to 10 after delivery.
It consists of old blood, serum, leukocytes, and tissue debris.
A nurse is assisting with the care of a client who is in labor with ruptured membranes and has herpes simplex virus with active lesions.
Which of the following actions should the nurse take?
Explanation
Prepare the client for a cesarean birth.

This is because the client has herpes simplex virus with active lesions, which can be transmitted to the newborn during vaginal delivery and cause serious complications such as neonatal herpes infection. A cesarean birth can prevent this transmission and protect the newborn’s health.
Choice A is wrong because an amnioinfusion is a procedure that involves infusing fluid into the amniotic cavity to increase the volume of amniotic fluid and reduce cord compression.
It is not indicated for a client with herpes simplex virus with active lesions.
Choice C is wrong because ampicillin is an antibiotic that is used to treat bacterial infections, not viral infections such as herpes simplex virus.
Ampicillin will not prevent the transmission of herpes simplex virus to the newborn.
Choice D is wrong because oxytocin is a hormone that stimulates uterine contractions and can be used to augment or induce labor.
It is not indicated for a client with herpes simplex virus with active lesions, as it can increase the risk of transmission to the newborn by prolonging the exposure to infected genital secretions.
A nurse is administering the inactivated influenza vaccine to a group of clients at a health clinic.
The nurse should recognize that which of the following conditions is a contraindication for this vaccine?
Explanation

The correct answer is choice C. Allergy to gelatin is a contraindication for the inactivated influenza vaccine because gelatin is one of the ingredients in the vaccine. People with severe, life-threatening allergies to any ingredient in a flu vaccine (other than egg proteins) should not get that vaccine.
Choice A is wrong because pregnancy is not a contraindication for the inactivated influenza vaccine. In fact, pregnant people are recommended to get a flu shot because they are at higher risk of developing serious flu complications.
Choice B is wrong because immunosuppression is not a contraindication for the inactivated influenza vaccine. People with weakened immune systems can get a flu shot, but they should avoid the nasal spray flu vaccine which contains live viruses.
Choice D is wrong because moderate illness with fever is not a contraindication for the inactivated influenza vaccine. People who are moderately ill can still get a flu shot, but they should wait until they recover if they have a severe illness.
A nurse is caring for a client who is postpartum and asks the nurse why her newborn received a vitamin K injection.
The nurse should explain that the injection is administered in order to prevent which of the following complications in the newborn?
Explanation
The nurse should explain that the injection is administered in order to prevent vitamin K deficiency bleeding (VKDB) in the newborn. Vitamin K is needed for blood clotting, but newborn babies have very low levels of vitamin K in their bodies at birth because only small amounts of the vitamin pass through the placenta and breast milk. VKDB can cause life-threatening bleeding in various parts of the body, such as the brain, intestines, or skin. VKDB can be classified into early-onset, classic, or late- onset depending on the time of presentation after birth. The most effective way to prevent VKDB is to give a single intramuscular dose of 0.5 to 1 mg of vitamin K to all newborn infants within 6 hours of birth.
Choice A is wrong because sepsis is not caused by vitamin K deficiency, but by bacterial infection.
Choice B is wrong because tachypnea is not caused by vitamin K deficiency, but by respiratory distress or other conditions.
Choice D is wrong because jaundice is not caused by vitamin K deficiency, but by high levels of bilirubin in the blood.
A nurse is collecting data from a client who is recovering from a recent stroke.
Which of the following findings should indicate to the nurse the need for a referral to a speech-language pathologist?
Explanation
Coughing while eating after a stroke may be caused by dysphagia, a swallowing disorder that can lead to aspiration, pneumonia and infection. A speech-language pathologist can assess and treat dysphagia and help the client improve their swallowing function.
Choice B is wrong because fine motor tremors are not related to speech or language problems.
They may be caused by damage to the cerebellum or basal ganglia, parts of the brain that control movement and coordination.
Choice C is wrong because facial flushing is not related to speech or language problems.
It may be caused by high blood pressure, fever, anxiety or other conditions.
Choice D is wrong because urinary incontinence is not related to speech or language problems.
It may be caused by damage to the spinal cord, bladder, pelvic floor muscles or nerves that control urination.
A nurse is preparing to give change-of-shift report to the oncoming nurse. Which of the following information should the nurse include?
Explanation
A bone scan that is scheduled for today. The nurse should include this information in the change-of-shift report because the oncoming nurse might have to modify the client’s care to accommodate leaving the unit.
Choice A is wrong because the client’s input and output for the shift are routine data that can be found in the client’s chart and do not need to be verbally reported.
Choice B is wrong because the client’s blood pressure from the previous day is not relevant to the current condition of the client and does not reflect any changes or interventions.
Choice D is wrong because the medication routine from the medication administration record is also routine data that can be accessed by the oncoming nurse and does not indicate any special needs or concerns.
A nurse is caring for a client who is at 10 weeks of gestation and reports nausea and vomiting on most days.
Which of the following recommendations should the nurse make?
Explanation
Keep your environment well ventilated. This can help reduce nausea and vomiting by eliminating odors that might trigger them.
Some additional explanations are:
Choice B is wrong because eating three large meals each day can increase nausea and vomiting by overloading the stomach. It is better to eat small, frequent meals and avoid spicy, greasy, or strong-smelling foods.
Choice C is wrong because restricting intake of high-carbohydrate foods can lead to ketosis, which can worsen nausea and vomiting. High-carbohydrate foods can also help settle the stomach and provide energy.
Choice D is wrong because brushing your teeth immediately after eating can stimulate the gag reflex and cause nausea and vomiting. It is better to rinse your mouth with water or mouthwash after eating and brush your teeth at least an hour later.
Normal ranges for nausea and vomiting in pregnancy are:
- Nausea and vomiting usually start around 6 weeks of gestation and peak around 9 weeks. They usually subside by 16 to 20 weeks, but some women may experience them throughout pregnancy.
- Nausea and vomiting are considered mild if they do not interfere with daily activities or nutrition. They are considered moderate if they cause some difficulty with daily activities or nutrition. They are considered severe if they prevent adequate intake of fluids and nutrients, cause weight loss, dehydration, electrolyte imbalance, or ketonuria.
- Nausea and vomiting that are severe or persist beyond 20 weeks of gestation may indicate a complication such as hyperemesis gravidarum, molar pregnancy, multiple gestation, or infection.
A nurse is preparing a room for a client who has a tracheostomy tube. Which of following supplies should the nurse place in the room?
Explanation
Obturator.
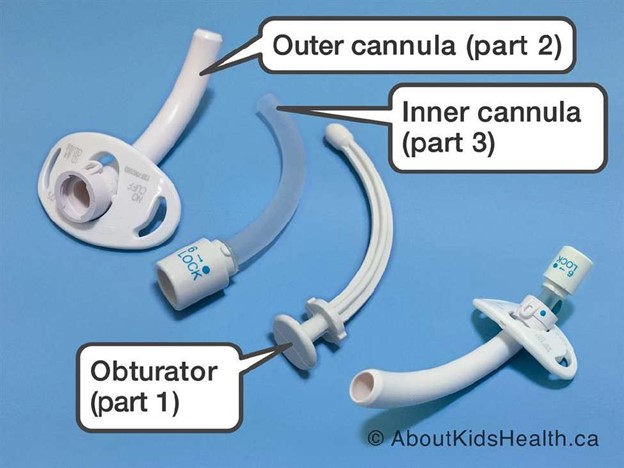
An obturator is a device that is inserted into the tracheostomy tube to guide it through the stoma and prevent tissue damage. It should be removed after the tube is inserted and kept near the bedside in case of accidental decannulation.
Choice A is wrong because povidone-iodine is an antiseptic solution that is not routinely used for tracheostomy care. It can cause skin irritation and damage to the mucous membranes.
Choice C is wrong because an irrigation set is not needed for a tracheostomy tube.
Irrigation can introduce bacteria and increase the risk of infection. It can also cause coughing and bleeding.
Choice D is wrong because hemostats are not used for a tracheostomy tube.
Hemostats are surgical instruments that are used to clamp blood vessels or tissues. They have no role in tracheostomy care.
Some other supplies that the nurse should place in the room are a trach tube the same size as the current tube and one size smaller, a portable suction machine with battery backup, and tubing that connects to the suction machine. Other supplies may include saline solution, syringes, gauze squares, gloves, a trachea tube brush, a waterproof drape, non-woven sponges, pipe cleaners, cotton tipped applicators, a T-drain sponge, twill tape, a trach holder, a speaking valve, a stoma cover, and a nebulizer.
A nurse is reinforcing teaching with a client who has a newly diagnosed latex allergy.
Which of the following foods should the nurse instruct the client to avoid?
Explanation
The nurse should instruct the client to avoid bananas because they are one of the foods that can cause a cross-reaction with latex allergy. This means that people who are allergic to latex may also have an allergic reaction to bananas because they contain similar proteins.
Choice A is wrong because wheat is not a latex cross-reactive food.
Choice B is wrong because strawberries are a low or undetermined cross- reactive food.
Choice C is wrong because peanuts are a low or undetermined cross-reactive food.
Some other foods that the nurse should instruct the client to avoid are avocado, kiwi, chestnut, papaya, and potato. These foods have a high or moderate association with latex cross-reactions. The client should also be careful with other fruits and vegetables that may contain similar proteins to latex.
A nurse is reviewing the laboratory results of a client who has nephrotic syndrome.
Which of the following results should the nurse expect?
Explanation
Proteinuria is the presence of excess protein in the urine, which is a hallmark of nephrotic syndrome. Nephrotic syndrome is a kidney disorder that causes increased permeability of the glomerular basement membrane, leading to loss of protein and other substances in the urine.
Choice B is wrong because hypolipidemia is a low level of lipids in the blood, which is not expected in nephrotic syndrome. On the contrary, nephrotic syndrome causes hyperlipidemia, which is a high level of lipids in the blood, due to increased synthesis and decreased clearance of lipoproteins.
Choice C is wrong because hyperalbuminemia is a high level of albumin in the blood, which is not expected in nephrotic syndrome. On the contrary, nephrotic syndrome causes hypoalbuminemia, which is a low level of albumin in the blood, due to loss of albumin in the urine and decreased synthesis by the liver.
Choice D is wrong because increased hemoglobin is not expected in nephrotic syndrome. On the contrary, nephrotic syndrome can cause anemia, which is a low level of hemoglobin in the blood, due to loss of iron and erythropoietin in the urine and decreased production of red blood cells by the bone marrow.
Normal ranges for proteinuria are less than 150 mg per day or less than 10 mg per deciliter on a random urine sample. Normal ranges for serum lipids are total cholesterol less than 200 mg per deciliter, LDL cholesterol less than 100 mg per deciliter, HDL cholesterol more than 40 mg per deciliter for men and more than 50 mg per deciliter for women, and triglycerides less than 150 mg per
deciliter. Normal ranges for serum albumin are 3.5 to 5.0 grams per deciliter.
A nurse is reviewing a client’s laboratory results prior to administering the client’s medications. The nurse notes that the client’s lithium level is 2.0 mEq/L.
Which of the following findings should the nurse expect?
Explanation
Muscle irritability. A client with a lithium level of
2.0 mEq/L has severe lithium toxicity, which can cause muscle irritability, tremors, seizures, and other neurological symptoms. The normal therapeutic range for lithium is 0.8-1.2 mEq/L.
Choice B is wrong because constipation is not a sign of lithium toxicity, but rather a possible side effect of lithium therapy at lower doses.
Choice C is wrong because hypoglycemia is not a sign of lithium toxicity, but rather a possible complication of diabetes or other conditions that affect blood sugar levels.
Choice D is wrong because increased blood pressure is not a sign of lithium toxicity, but rather a possible risk factor for cardiovascular disease or other conditions that affect blood vessels.
A nurse is collecting data from a client who is at 29 weeks of gestation.
Which of the following findings should the nurse identify as a potential indication of a prenatal complication?
Explanation
This can be a sign of preeclampsia, a serious complication of pregnancy that causes high blood pressure and proteinuria.
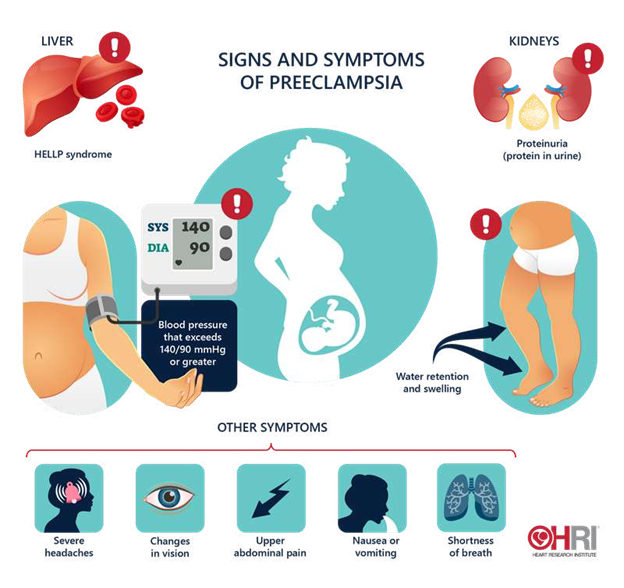
The nurse should report this finding to the provider and monitor the client’s blood pressure, urine protein, and reflexes.
Choice A is wrong because leg cramps are a common discomfort during pregnancy and are not usually a sign of a complication.
Choice B is wrong because ptyalism, or excessive salivation, is a normal physiological change during pregnancy and does not indicate a problem.
Choice D is wrong because melasma, or darkening of the skin on the face, is also a normal physiological change during pregnancy and does not pose a risk to the mother or the fetus.
A nurse is reinforcing teaching with a newly licensed nurse about discharge planning.
Which of the following statements by the newly licensed nurse indicates an understanding of the teaching?
Explanation
The nurse should begin discharge planning upon the client’s admission. This is because discharge planning is a key aspect of effective care that reduces the length of stay, emergency readmissions and pressure on hospital beds. Discharge planning involves considering what support might be required by the client in the community, referring the client to these services, and liaising with these services to manage the client’s discharge.
Choice A is wrong because the nurse is not responsible for providing a written prescription for a client home care referral. This is the role of the provider or another authorised prescriber.
Choice C is wrong because a home hazard appraisal does not include an assessment of the client’s financial resources. A home hazard appraisal is an evaluation of the safety and accessibility of the client’s home environment.
Choice D is wrong because a medication reconciliation is not required 24 hours prior to the client’s discharge. A medication reconciliation is a process of comparing the medications a client is taking with those prescribed for them to avoid errors or discrepancies. A medication reconciliation should be done at every transition of care, including admission, transfer and discharge.
A nurse is using an interpreter to communicate with a client who speaks a different language than the nurse.
Which of the following actions should the nurse take?
Explanation
Observe the client’s body language during the conversation. This action will help the nurse to assess the client’s nonverbal cues and emotions, which can enhance communication and understanding. The nurse should also determine the client’s understanding several times during the conversation and use lay terms if possible.
Choice A is wrong because avoiding asking the client personal questions can hinder rapport building and prevent the nurse from obtaining important information about the client’s health and needs.
Choice C is wrong because maintaining eye contact with the interpreter when asking questions can show disrespect and disinterest to the client and his family. The nurse should look at the client and his family when asking questions, not at the interpreter.
Choice D is wrong because including medical terminology when discussing the client’s condition can confuse the client and his family and create barriers to communication. The nurse should use simple and clear language that the client and his family can understand.
A nurse on an inpatient unit is assisting with the discharge plan for a client who has schizophrenia.
Which of the following resources should the nurse include in the plan?
Explanation
Contact information for a community mental health center. A community mental health center can provide ongoing outpatient care and support services for a client who has schizophrenia after discharge from an inpatient unit. A community mental health center can also help the client access other resources such as medication, housing, and vocational training.
Choice B is wrong because a list of primary prevention activities is not relevant for a client who already has schizophrenia. Primary prevention aims to prevent the occurrence of a disease or disorder in the first place.
Choice C is wrong because contact information for enrollment in a 12-step program is not appropriate for a client who has schizophrenia unless they also have a substance use disorder. A 12-step program is a self-help group that follows a set of principles to achieve and maintain sobriety.
Choice D is wrong because a referral for respite care services is not necessary for a client who has schizophrenia unless they also have a caregiver who needs temporary relief from their caregiving duties. Respite care services provide short-term care for clients who are dependent on others for their daily needs.
A nurse at a long-term care facility is caring for a client who has AIDS. The client accidentally spills the contents of their urinal on the floor.
After cleaning up the spill with soap and water, the nurse should apply a solution of water and which of the following disinfectants to the floor?
Explanation
Bleach.
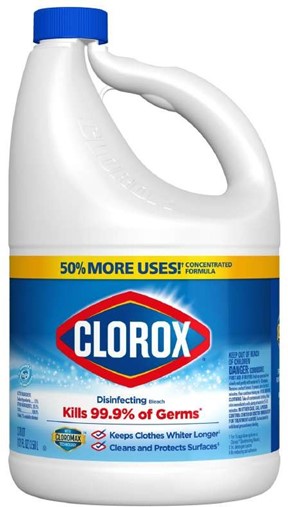
According to the CDC, bleach is an effective disinfectant for environmental surfaces contaminated with blood or body fluids from a person with AIDS or other bloodborne pathogens. Bleach can kill HIV and hepatitis viruses when used in a 1:10 dilution with water.
Choice A is wrong because isopropyl alcohol is not recommended for disinfecting environmental surfaces. It can evaporate quickly and may not have enough contact time to kill the pathogens.
Choice B is wrong because chlorhexidine is an antiseptic, not a disinfectant. It is used for skin cleansing or wound irrigation, but it is not effective against spores or non-enveloped viruses.
Choice C is wrong because hydrogen peroxide is a low-level disinfectant that can be inactivated by organic matter.
It is not suitable for disinfecting surfaces contaminated with blood or body fluids.
A nurse is collecting data for a client’s health history and physical examination.
Which of the following information should the nurse identify as a risk factor for type 2 diabetes mellitus?
Explanation
BMI 32.2.
A high body mass index (BMI) is a major risk factor for type 2 diabetes mellitus, as it indicates overweight or obesity.
Overweight or obesity can cause insulin resistance, which means the body cells do not respond well to insulin and cannot take up glucose from the blood. This leads to high blood sugar levels and diabetes.
Choice A is wrong because history of exercise-induced asthma is not a risk factor for type 2 diabetes mellitus.
Asthma is a respiratory condition that causes inflammation and narrowing of the airways, but it does not affect the metabolism of glucose or insulin.
Choice B is wrong because age 35 years is not a risk factor for type 2 diabetes mellitus.
Although the risk of diabetes increases with age, especially after 45 years, it can also occur in younger people.
Age alone is not enough to cause diabetes.
Choice C is wrong because history of mumps is not a risk factor for type 2 diabetes mellitus.
Mumps is a viral infection that affects the salivary glands, but it does not damage the pancreas or impair insulin production.
Some other risk factors for type 2 diabetes mellitus are family history, race or ethnicity, physical inactivity, prediabetes, gestational diabetes, polycystic ovarian syndrome, and smoking.
A nurse is collecting data from a client who has hypothyroidism.
When reviewing the findings and the client’s medical record, which of the following interventions should the nurse suggest to the provider?
Explanation
This is because the client has hypothyroidism, which means their thyroid gland does not produce enough thyroid hormone. Levothyroxine is a synthetic form of thyroid hormone that can replace the missing hormone and normalize the TSH level. The client’s TSH level is 8.9 mIU/L, which is above the normal range of 0.4 to 4.0 mIU/L. This indicates that the client’s current dosage of levothyroxine is insufficient and needs to be increased.
Choice A is wrong because thyroid ablation therapy is a treatment for hyperthyroidism, not hypothyroidism.
Thyroid ablation therapy involves destroying part or all of the thyroid gland with radioactive iodine or surgery, which reduces the production of thyroid hormone.
This would worsen the client’s condition and symptoms.
Choice C is wrong because lovastatin is a statin drug that lowers cholesterol levels. Hypothyroidism can cause high cholesterol levels, but this is usually corrected by levothyroxine therapy. Replacing lovastatin with cholestyramine, a bile acid sequestrant that also lowers cholesterol levels, would not address the underlying cause of hypothyroidism and would not improve the client’s TSH level.
Choice D is wrong because restricting the intake of iodized salt would not help the client with hypothyroidism. Iodine is an essential element for the synthesis of thyroid hormone, but most people in developed countries get enough iodine from their diet.
Hypothyroidism is usually caused by autoimmune disease, not iodine deficiency.
A nurse is collecting data from a client who has recently stopped smoking.
Which of the following findings should the nurse recognize as a manifestation of acute nicotine withdrawal?
Explanation
It occurs because nicotine stimulates the release of dopamine, a neurotransmitter that regulates mood and pleasure. When nicotine intake is stopped, dopamine levels drop and cause anxiety and irritability.
Choice A is wrong because tachycardia, or rapid heart rate, is not a symptom of nicotine withdrawal. In fact, smoking can increase blood pressure and heart rate, so quitting smoking may lower them.
Choice C is wrong because weight loss is not a symptom of nicotine withdrawal. On the contrary, weight gain is more likely to occur after quitting smoking, because nicotine suppresses appetite and increases metabolism.
Choice D is wrong because vomiting is not a symptom of nicotine withdrawal. Vomiting may be a side effect of some nicotine replacement therapies, such as patches or gum, but it is not caused by the lack of nicotine itself.
A nurse is caring for a preschooler immediately following a tonsillectomy and notices the child swallowing frequently.
Which of the following actions should the nurse take?
Explanation
Administer analgesia. The child is likely experiencing pain and discomfort after the tonsillectomy, which can cause frequent swallowing. Analgesia can help relieve the pain and reduce the risk of bleeding.
Choice A is wrong because checking the back of the throat with a pen light can cause trauma and bleeding to the surgical site. The nurse should avoid using any instruments or objects in the mouth of the child after a tonsillectomy.
Choice B is wrong because obtaining the child’s vital signs in 15 min is not a priority action. The nurse should monitor the child’s vital signs more frequently, especially for signs of bleeding such as increased pulse and decreased blood pressure.
Choice D is wrong because offering the child a drink of water can cause irritation and bleeding to the throat. The nurse should avoid giving the child any fluids or foods by mouth until the gag reflex returns and the child is fully awake. The nurse should also avoid giving the child any fluids or foods that are acidic, carbonated, hot, or spicy, as they can cause pain and bleeding.
A nurse is reinforcing teaching about HbA1c with a client who has type 1 diabetes mellitus.
Which of the following information should the nurse include?
Explanation
The HbA1c value determines long-term blood glucose control for the past 120 days. This is because the HbA1c test measures what percentage of hemoglobin proteins in your blood are coated with sugar (glycated). Hemoglobin proteins in red blood cells live for around 120 days, so the test reflects your average blood sugar level for the past two to three months.
Choice A is wrong because an HbA1c value greater than 8% indicates poor diabetic control of blood sugar. The HbA1c target for most people with type 1 diabetes is 48 mmol/mol (or 6.5%) or lower.
Choice B is wrong because the HbA1c value is not altered by eating habits the day before the test. The test does not require fasting and can be done at any time of the day.
Choice D is wrong because an HbA1c test should be performed more than once per year.
The frequency of the test depends on the type of diabetes, your treatment plan and your blood sugar level. For example, you may need the test twice a year if you have good blood sugar control, or four times a year if you take insulin or have trouble keeping your blood sugar level within your target range.
Sign Up or Login to view all the 58 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

