ATI PN FUNDAMENTALS UPDATED 2023
Total Questions : 41
Showing 25 questions, Sign in for moreA nurse on a medical-surgical unit is caring for a group of clients. Which of the following findings should the nurse identify as a safety hazard?
Explanation
Choice A reason: A weight-sensitive sensor mat is a device that alerts the staff when a client tries to get out of bed. It is not a safety hazard, but rather a safety measure to prevent falls.
Choice B reason: A buzzing sensation at the application site of a transcutaneous electrical nerve stimulation unit is normal and expected. It indicates that the unit is delivering electrical impulses to the nerves and muscles. It is not a safety hazard, but rather a therapeutic intervention for pain relief.
Choice C reason: A capillary refill of less than 2 seconds is normal and indicates adequate blood circulation. It is not a safety hazard, but rather a sign of good perfusion.
Choice D reason: Raising all four side rails of a client's bed is a safety hazard because it increases the risk of injury if the client tries to climb over them. It also restricts the client's mobility and may cause feelings of isolation and imprisonment. It is a violation of the client's rights and dignity.
A nurse is preparing to insert an indwelling urinary catheter and is verifying the client’s express consent for this procedure. Which of the following actions should the nurse take?
Explanation
Choice A reason: Witnessing the client’s signature on a consent form is not necessary for an indwelling urinary catheter insertion, which is a routine and noninvasive procedure. The nurse only needs to witness the signature for invasive or high-risk procedures that require written consent.
Choice B reason: Obtaining verbal consent from the client is the appropriate action for the nurse to take before inserting an indwelling urinary catheter. The nurse should explain the purpose, benefits, risks, and alternatives of the procedure and ensure that the client understands and agrees to it.
Choice C reason: Having another nurse co-sign the client’s consent is not required for an indwelling urinary catheter insertion, which is a routine and noninvasive procedure. The nurse only needs to have another nurse co-sign the consent for procedures that involve blood transfusions, organ donations, or research participation.
Choice D reason: Checking the medical record for the client’s signature on a previous consent form is not sufficient for verifying the client’s express consent for an indwelling urinary catheter insertion. The nurse should obtain a new consent for each procedure, as the client has the right to change their mind or refuse the treatment at any time.
A nurse is collecting data regarding home safety from a client who is prone to falls. Which of the following findings should the nurse recognize as placing the client at additional risk?
Explanation
Choice Areason: Removing the wheels from rolling chairs is a good practice to prevent the chairs from sliding or moving unexpectedly. It is not a risk factor for falls, but rather a safety measure to prevent them.
Choice Breason: A stool riser is a device that elevates the toilet seat and makes it easier for the client to sit down and stand up. It is not a risk factor for falls, but rather a safety measure to prevent them.
Choice C reason: Having the mattress directly on the floor may make it harder for the client to get in and out of bed, but it does not increase the risk of falls. In fact, it may reduce the risk of injury if the client falls from the bed, as the height is lower.
Choice D reason: Covering electrical cords with throw rugs is a risk factor for falls, as the client may trip over them or get tangled in them. It is also a fire hazard, as the rugs may overheat or catch fire from the cords. The nurse should advise the client to remove the rugs and secure the cords away from the walking areas.
A nurse is reinforcing teaching with a client about the use of a peak flow meter. Which of the following actions should the nurse take first?
Explanation
Choice A reason: Showing the client a video demonstration of peak flow meter use is a helpful teaching strategy, but it is not the first action that the nurse should take. The nurse should first assess the client's baseline knowledge and readiness to learn before providing any information or instruction.
Choice B reason: Observing the client using the peak flow meter is a way to evaluate the client's learning and skill, but it is not the first action that the nurse should take. The nurse should first determine the client's knowledge of the use of the peak flow meter and then teach the client how to use it correctly.
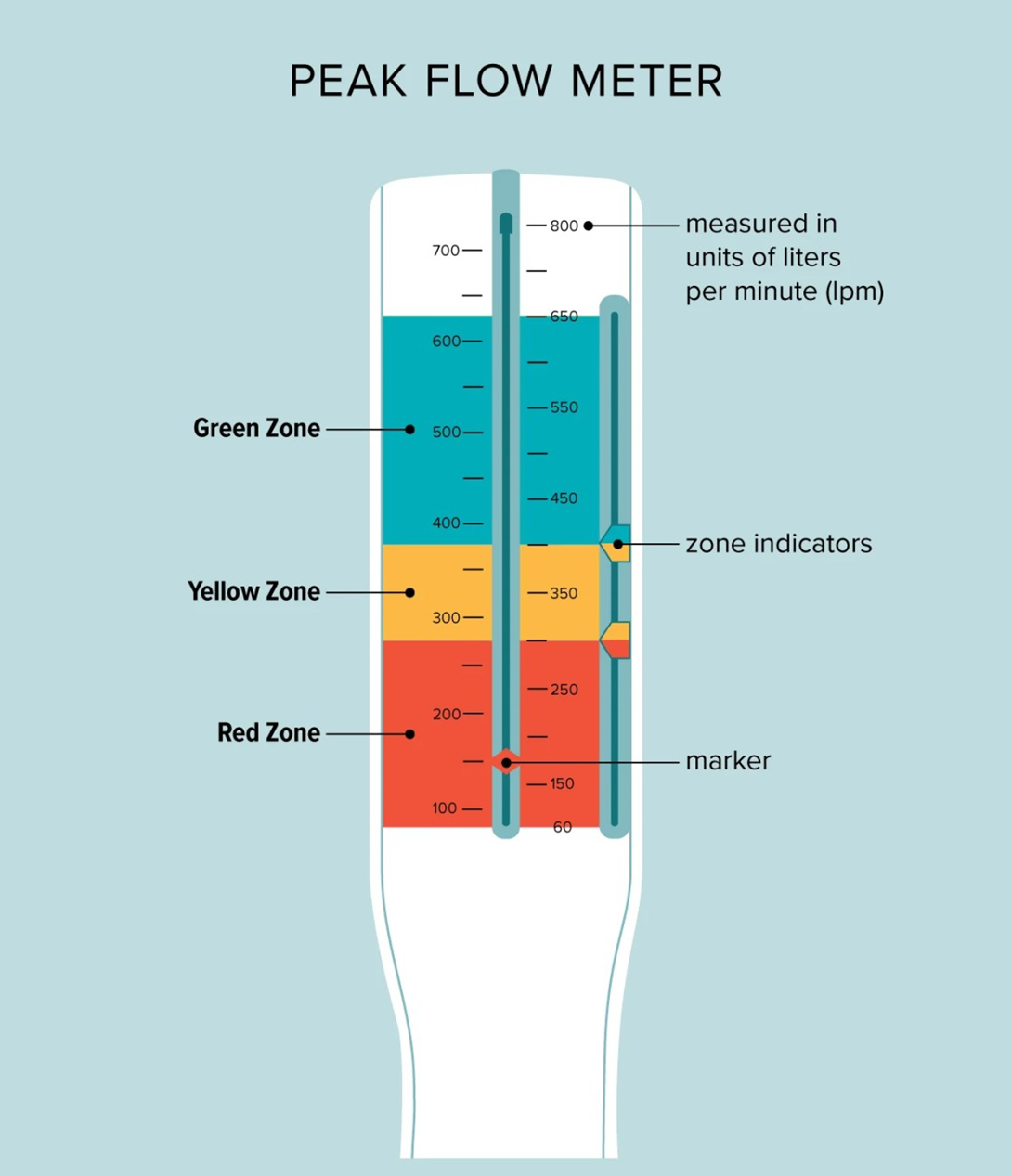
Choice C reason: Emphasizing the importance of the daily use of the peak flow meter is a way to motivate the client to adhere to the treatment plan, but it is not the first action that the nurse should take. The nurse should first assess the client's knowledge of the use of the peak flow meter and then explain the benefits and rationale of using it regularly.
Choice D reason: Determining the client's knowledge of the use of the peak flow meter is the first action that the nurse should take, as it follows the principle of the nursing process. The nurse should start with assessment, then proceed with planning, implementation, and evaluation. By assessing the client's knowledge, the nurse can identify the client's learning needs, gaps, and preferences, and tailor the teaching accordingly.
A nurse observes an assistive personnel (AP) perform mouth care for a client who is unconscious. Which of the following actions by the AP requires intervention by the nurse?
Explanation
Choice A reason: Using an oral care sponge swab moistened with cool water to clean the client's mouth is an appropriate action by the AP, as it helps to remove debris and bacteria from the oral cavity. It does not require intervention by the nurse.
Choice B reason: Wearing clean gloves to perform mouth care for the client is an appropriate action by the AP, as it protects the AP and the client from potential infection. It does not require intervention by the nurse.
Choice C reason: Lowering the side rail on the side of the bed where they will stand to perform mouth care is an inappropriate action by the AP, as it increases the risk of the client falling from the bed. It requires intervention by the nurse, who should instruct the AP to keep the side rails up at all times and use a tilt table or a pillow to support the client's head.
Choice D reason: Using two gloved fingers to open the client's mouth for cleaning is an appropriate action by the AP, as it allows the AP to access the oral cavity without causing injury to the client. It does not require intervention by the nurse.
A nurse on a medical-surgical unit is collecting data from a client who is postoperative following abdominal surgery. The client's BP was 125/85 mm Hg 15 min ago. The nurse now finds that the client’s BP is 176/96 mm Hg. Which of the following actions should the nurse take?
Explanation
Choice A reason: Using a narrower cuff to repeat the BP measurement is an incorrect action by the nurse, as it can result in a falsely high reading. The nurse should use a cuff that fits the client's arm size and circumference.
Choice B reason: Measuring the client's BP in the other arm is the correct action by the nurse, as it can help to confirm the accuracy of the reading and rule out any possible errors or variations. The nurse should compare the readings from both arms and report any significant differences to the provider.
Choice C reason: Deflating the cuff faster when repeating the BP measurement is an incorrect action by the nurse, as it can result in a falsely low reading. The nurse should deflate the cuff at a rate of 2 to 3 mm Hg per second.
Choice D reason: Requesting a prescription for an antihypertensive medication is an inappropriate action by the nurse, as it is premature and unnecessary. The nurse should first verify the BP reading and identify the possible causes of the elevation, such as pain, anxiety, or medication effects. The nurse should also implement nonpharmacological interventions, such as positioning, relaxation, and oxygen therapy, before administering any medication.
A nurse is performing a wound irrigation for a client who has methicillin-resistant Staphylococcus aureus. When removing personal protective equipment, which of the following pieces should the nurse remove first?
Explanation
Choice A reason: Gloves are the first piece of personal protective equipment that the nurse should remove, as they are the most contaminated and can transfer microorganisms to other surfaces. The nurse should remove the gloves by grasping the outside of one glove at the wrist and pulling it off inside out, then holding it in the gloved hand and sliding the fingers of the ungloved hand under the other glove at the wrist and pulling it off inside out over the first glove. The nurse should then discard the gloves in a biohazard container.
Choice B reason: Goggles are the second piece of personal protective equipment that the nurse should remove, as they can protect the eyes from splashes or droplets. The nurse should remove the goggles by grasping the earpieces or headband and lifting them away from the face. The nurse should then discard the goggles in a designated receptacle or place them in a designated area for reprocessing.
Choice C reason: Gown is the third piece of personal protective equipment that the nurse should remove, as it can protect the clothing and skin from contamination. The nurse should remove the gown by untying the neck and waist ties and pulling the gown away from the neck and shoulders, touching only the inside of the gown. The nurse should then turn the gown inside out, fold or roll it into a bundle, and discard it in a biohazard container.
Choice D reason: Mask is the last piece of personal protective equipment that the nurse should remove, as it can protect the nose and mouth from inhalation of microorganisms. The nurse should remove the mask by grasping the bottom ties or elastics and then the top ties or elastics and pulling the mask away from the face. The nurse should then discard the mask in a biohazard container.
A nurse is caring for a client who is 2 days postoperative following a below-the-knee amputation. Which of the following statements by the client should the nurse identify as indicating an acceptance of the limb loss?
Explanation
Choice A reason: This is the correct answer because it reflects acceptance of the limb loss and a positive coping strategy. This statement shows that the client is willing to take responsibility for the care of the residual limb and is ready to learn new skills. The other statements indicate denial, anger, or depression, which are normal stages of grief, but not acceptance.
Choice B reason: This is not the correct answer because it reflects denial of the limb loss and a reluctance to face the reality of the situation.
Choice C reason: This is not the correct answer because it reflects depression and a sense of helplessness and dependency.
Choice D reason: This is not the correct answer because it reflects anger and a difficulty in adjusting to the limb loss.
A nurse is providing teaching with a client who has severe arthritis and has difficulty with stairs. What should the nurse include in the teaching?
Explanation
Choice A reason: This is not the correct answer because it distracts the client from the surroundings and could cause loss of balance or coordination.
Choice B reason: This is the correct answer because it enables the client to use the handrails as a support and reduces the stress on the arms and shoulders.
Choice C reason: This is not the correct answer because it creates an uneven distribution of weight and could cause instability or pain.
Choice D reason: This is not the correct answer because it requires the client to shift the body weight abruptly and could cause muscle strain or joint damage.
A nurse is collecting data from a client who has an NG tube in place for gastric decompression. Which of the following findings should the nurse report to the provider?
Explanation
Choice A reason: This is not the correct answer because greenish-yellow drainage is a normal color for gastric secretions and does not indicate a problem.
Choice B reason: This is not the correct answer because a report of hunger is common for a client with an NG tube and does not require intervention.
Choice C reason: This is the correct answer because gastric contents in the air vent mean that the NG tube is clogged or kinked and needs to be flushed or replaced. This is the correct answer because it indicates that the NG tube is not functioning properly and could cause aspiration or infection. The other findings are expected or normal for a client with an NG tube.
Choice D reason: This is not the correct answer because abdominal distention is a common reason for placing an NG tube and should improve with gastric decompression.
A nurse is caring for a client who speaks a different language than the nurse and is 5 hours postoperative. Which of the following actions should the nurse take to determine the client's level of pain?
Explanation
Choice A reason: This is not the correct answer because the FLACC scale is designed for infants and children who are unable to verbalize their pain, not for adults who speak a different language.
Choice B reason: This is not the correct answer because asking an assistive personnel to interpret is not a reliable or ethical way of communicating with the client. The nurse should use a professional interpreter or a certified bilingual staff member.
Choice C reason: This is the correct answer because a communication board is a simple and effective way of assessing the client's pain level and location.
Choice D reason: This is not the correct answer because the FACES pain scale is based on facial expressions that may vary across cultures and languages. The client may not understand or relate to the pictures on the scale.
A nurse is reinforcing teaching with a client who has a new Westerly syndrome. Which of the following statements by the client demonstrates an understanding of the teaching?
Explanation
Choice A reason: Broccoli is a good source of vitamin K, which is essential for blood clotting. However, it also contains vitamin C, which can interfere with the action of warfarin, a medication used to treat Westerly syndrome. Therefore, broccoli should be consumed in moderation and with caution.
Choice B reason: Bananas are high in potassium, which can affect the heart rhythm and cause arrhythmias in people with Westerly syndrome. Therefore, bananas should be avoided or limited in the diet.
Choice C reason: Mushrooms are low in vitamin K and do not interact with warfarin. They are also a good source of protein, fiber, and antioxidants. Therefore, mushrooms can be safely consumed by people with Westerly syndrome.
Choice D reason: Popcorn is high in sodium, which can increase blood pressure and worsen the symptoms of Westerly syndrome. Therefore, popcorn intake should be limited or avoided.
A nurse is assisting in the transfer of a client who has left-sided weakness from a bed to a chair. Which of the following actions should the nurse take?
Explanation
Choice A reason: Standing on the client's stronger side may cause the client to lean or fall toward the weaker side. The nurse should stand on the client's weaker side and support the client's trunk and affected arm.
Choice B reason: Raising the bed to waist level may make it harder for the client to move their legs over the edge of the bed. The nurse should lower the bed to the lowest position and raise the head of the bed to a sitting position.
Choice C reason: Flexing hips and knees helps the client use their stronger leg muscles and maintain balance when standing up. The nurse should also place one arm under the client's axilla and the other arm around the client's waist.
Choice D reason: Pivoting on the foot farthest from the bed may cause the client to lose balance and fall. The nurse should pivot on the foot closest to the bed and guide the client to turn and sit on the chair.
A nurse is caring for a group of clients. For which of the following situations should the nurse complete an incident report? (Select all that apply.)
Explanation
Choice A reason: A client's dissatisfaction with the temperature of the meals is not an incident that requires a report. The nurse should inform the dietary staff and try to accommodate the client's preferences.
Choice B reason: A client's burns from a heating pad is an incident that requires a report. The nurse should document the cause, extent, and treatment of the burns, as well as the client's response and any actions taken to prevent recurrence.
Choice C reason: A client's disorientation and fall out of bed is an incident that requires a report. The nurse should document the circumstances, injuries, and interventions related to the fall, as well as the client's response and any changes in the plan of care.
Choice D reason: A client's inability to afford the physical therapy is not an incident that requires a report. The nurse should refer the client to a social worker or a financial counselor who can assist with finding resources and options.
Choice E reason: A client's visitor's dizziness and fainting in the client's room is an incident that requires a report. The nurse should document the event, the visitor's condition, and any actions taken to assist the visitor.
A nurse is assisting with the postmortem care of a client whose partner is at the bedside. Which of the following actions should the nurse take?
Explanation
Choice A reason: Directing the partner to leave and return once postmortem care is complete is not respectful of the partner's feelings and wishes. The nurse should allow the partner to stay and participate in the postmortem care if they desire.
Choice B reason: Instructing the partner not to touch the client’s body is not compassionate or supportive of the partner's grief. The nurse should encourage the partner to touch, hold, or kiss the client’s body as a way of saying goodbye.
Choice C reason: Placing the client’s personal belongings in a safe location in the facility is a necessary action, but not the priority. The nurse should first ask the partner if they want to keep any of the belongings or give them to the nurse for safekeeping.
Choice D reason: Asking the partner about any rituals they would like to be performed is the most appropriate action. The nurse should respect and facilitate the partner's cultural, religious, or personal preferences for postmortem care.
A nurse in a provider’s office receives a telephone call from a client’s sibling requesting current information about the client’s condition. Which of the following actions should the nurse take?
Explanation
Choice A reason: Requesting that the caller contact the client’s provider directly for information is not the best action. The nurse should first determine if the caller has the client’s consent to receive information and if the caller is authorized to do so.
Choice B reason: Asking the caller to contact the client directly for information is not appropriate. The client may not be able to communicate or may not want to share information with the caller. The nurse should respect the client’s privacy and confidentiality.
Choice C reason: Gathering additional information from the caller to verify their identity is the most appropriate action. The nurse should ask the caller for their name, relationship to the client, and other details that can confirm their identity. The nurse should also check the client’s record for any written or verbal consent to disclose information to the caller.
Choice D reason: Providing the caller with a brief update about the client’s condition is not advisable. The nurse should not share any information without verifying the caller’s identity and the client’s consent. The nurse should also follow the provider’s office policy and the Health Insurance Portability and Accountability Act (HIPAA) guidelines for disclosing information.
A nurse is assisting in creating a plan to reduce environmental stressors for clients in an acute care unit. Which of the following actions should the nurse include in the plan?
Explanation
Choice A reason: Turning on loud music in client care areas is not a good action. Loud music can increase noise levels, disrupt sleep, and cause agitation and anxiety for clients. The nurse should keep the noise level low and provide earplugs or headphones for clients who want to listen to music.
Choice B reason: Assigning different nurses to provide care for clients each day is not a good action. Different nurses may have different styles, routines, and expectations, which can confuse and frustrate clients. The nurse should maintain consistency and continuity of care by assigning the same nurses to the same clients as much as possible.
Choice C reason: Offering the clients many choices regarding care is a good action. Choices can enhance the clients' sense of control, autonomy, and involvement in their care. The nurse should respect the clients' preferences and involve them in decision making as much as possible.
Choice D reason: Restricting the number of visitors for clients is not a good action. Visitors can provide social support, comfort, and companionship for clients, which can reduce stress and improve well-being. The nurse should encourage and facilitate visitation, unless it is contraindicated by the client's condition or preference.
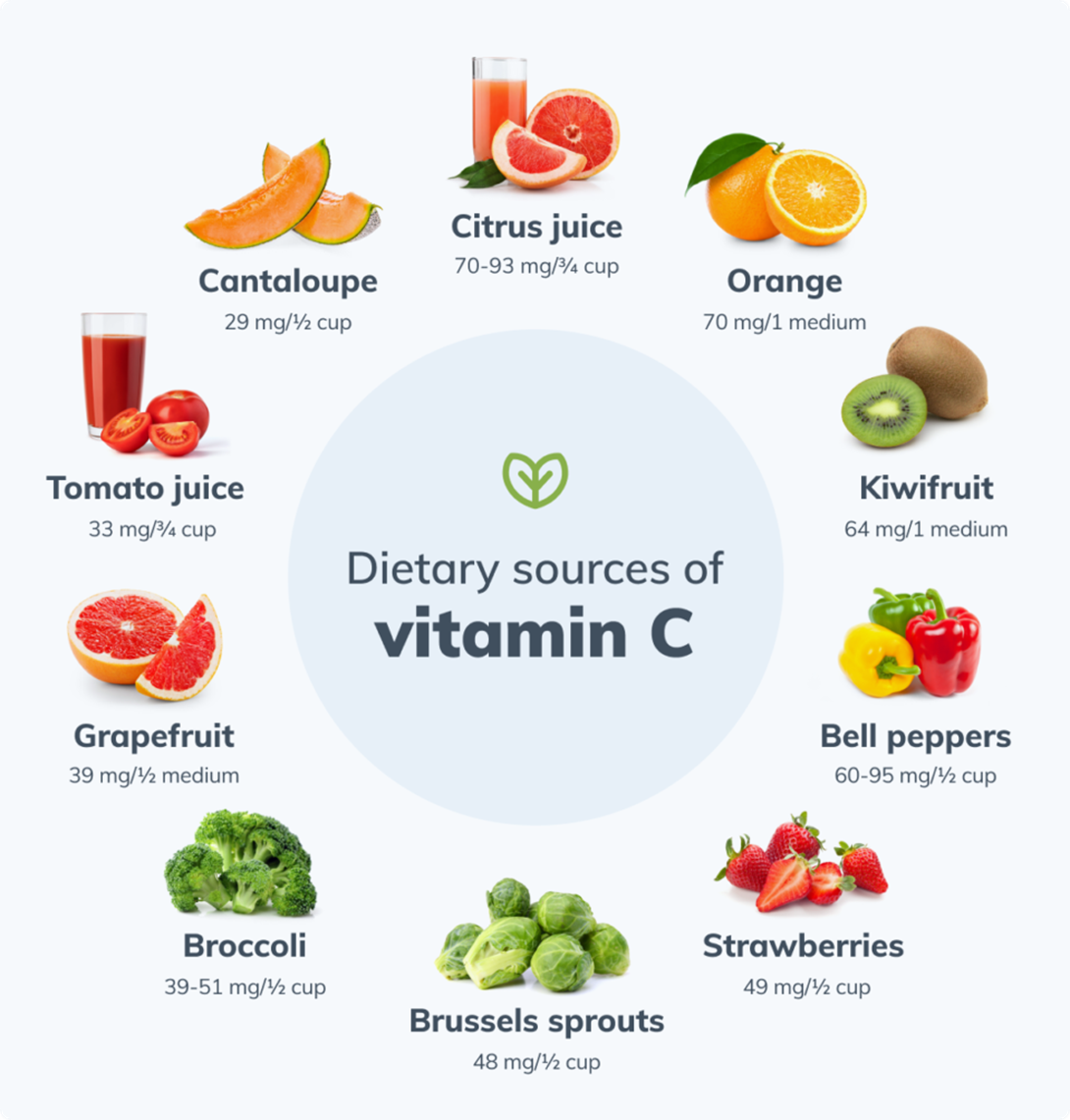
A nurse is reinforcing teaching with a client who needs to increase vitamin C intake to promote wound healing. Which of the following foods should the nurse recommend as the best source of vitamin C?
Explanation
Choice A reason: A small banana contains about 8.7 mg of vitamin C, which is only 10% of the recommended daily intake for adults.
Choice B reason: A medium fresh green pear contains about 4.3 mg of vitamin C, which is only 5% of the recommended daily intake for adults.
Choice C reason: A small pink grapefruit contains about 38.4 mg of vitamin C, which is 43% of the recommended daily intake for adults. This is the highest amount of vitamin C among the four choices.
Choice D reason: A small apple with the skin contains about 8.4 mg of vitamin C, which is only 9% of the recommended daily intake for adults.
A nurse is reinforcing teaching with the adult children of a client who is receiving palliative care. Which of the following statements by one of the adult children indicates an understanding of the teaching?
Explanation
Choice A reason: Receiving emotional support during the mother’s illness is a sign of understanding the teaching. Palliative care is a holistic approach that aims to improve the quality of life of clients and their families who are facing life-threatening illnesses. It provides physical, psychological, social, and spiritual support to address their needs and preferences.
Choice B reason: Providing resuscitation to the mother if necessary is a sign of misunderstanding the teaching. Palliative care focuses on relieving symptoms and suffering, not curing the illness or prolonging life. It respects the client’s wishes and goals of care, which may include a do-not-resuscitate (DNR) order or an advance directive.
Choice C reason: Not discussing the illness in the presence of the mother is a sign of misunderstanding the teaching. Palliative care encourages open and honest communication between the client and the family, as well as the health care team. It helps the client and the family cope with the illness, express their emotions and concerns, and make informed decisions.
Choice D reason: Not allowing the mother’s spiritual advisor to visit during this time is a sign of misunderstanding the teaching. Palliative care recognizes the importance of spirituality and religion for some clients and their families. It supports the client’s right to practice their faith and receive spiritual guidance and comfort from their chosen source.
A nurse is caring for a client who is postpartum. Which of the following documentations should the nurse include in the client’s health record?
Explanation
Choice A reason: Client instructed on self-care needs is not a specific or accurate documentation. The nurse should include the details of the instruction, such as the topics covered, the teaching methods used, the client's response, and the evaluation of learning.
Choice B reason: Oral temperature elevated at 0800 is a specific and accurate documentation. The nurse should include the vital signs and any abnormal findings, such as fever, in the client's health record. The nurse should also report the elevation to the provider and monitor the client for signs of infection.
Choice C reason: Episiotomy approximated, 3 cm (1.18 in) in length is not a specific or accurate documentation. The nurse should include the type, location, and degree of the episiotomy, as well as the condition of the wound, the presence of edema, erythema, or drainage, and the interventions performed.
Choice D reason: Client drank adequate amounts of fluid with meals is not a specific or accurate documentation. The nurse should include the exact amount and type of fluid intake, as well as the output, in the client's health record. The nurse should also assess the client for signs of dehydration or fluid overload.
A nurse is reinforcing teaching with a client who needs to increase vitamin C intake to promote wound healing. Which of the following foods should the nurse recommend as the best source of vitamin C?
Explanation
Choice A reason: A small banana contains about 8.7 mg of vitamin C, which is only 10% of the recommended daily intake for adults.
Choice B reason: A medium fresh green pear contains about 4.3 mg of vitamin C, which is only 5% of the recommended daily intake for adults.
Choice C reason: A small pink grapefruit contains about 38.4 mg of vitamin C, which is 43% of the recommended daily intake for adults. This is the highest amount of vitamin C among the four choices.
Choice D reason: A small apple with the skin contains about 8.4 mg of vitamin C, which is only 9% of the recommended daily intake for adults.
A nurse is assisting with the admission of a client. Which of the following statements should the nurse make to demonstrate the principle of advocacy?
Explanation
Choice A reason: "I will keep your personal information private." is not a statement of advocacy, but a statement of confidentiality. Confidentiality is the ethical and legal obligation of the nurse to protect the client's privacy and information. Advocacy is the act of supporting and protecting the client's rights and interests.
Choice B reason: "I will do my best to fulfill my promises to you." is not a statement of advocacy, but a statement of accountability. Accountability is the responsibility of the nurse to answer for their actions and outcomes. Advocacy is the act of supporting and protecting the client's rights and interests.
Choice C reason: "I will speak with your provider on your behalf." is not a statement of advocacy, but a statement of communication. Communication is the exchange of information and ideas between the nurse and the client, the provider, and other members of the health care team. Advocacy is the act of supporting and protecting the client's rights and interests.
Choice D reason: "I will let you make decisions about your health care." is a statement of advocacy. Advocacy is the act of supporting and protecting the client's rights and interests, such as the right to informed consent, self-determination, and autonomy. The nurse should respect the client's choices and preferences, and assist them in making informed decisions.
A nurse is reinforcing information with a client who wishes to complete their advance directives. Which of the following statements should the nurse make?
Explanation
Choice A reason: You do not need to have advance directives in place in order to refuse recommended treatment. Advance directives are legal documents that allow you to express your wishes for your health care in case you are unable to communicate or make decisions for yourself. You have the right to accept or refuse any treatment at any time, as long as you are competent and informed.
Choice B reason: An attorney is not needed in order for you to name a designee in your health care proxy. A health care proxy is a type of advance directive that allows you to appoint a person to make health care decisions for you if you are unable to do so. You can choose anyone you trust, such as a family member or a friend, as your designee. You do not need a lawyer to complete a health care proxy form, but you need to sign it in front of two witnesses.
Choice C reason: You can decline to have certain medical procedures performed in your living will. A living will is another type of advance directive that allows you to state your preferences for life-sustaining treatments, such as CPR, artificial ventilation, or feeding tubes. You can specify which treatments you want or do not want, and under what circumstances. You can also include your values and beliefs about your quality of life and end-of-life care.
Choice D reason: A living will cannot be an oral statement that you agree upon with your provider. A living will must be a written document that is signed by you and witnessed by two people. An oral statement may not be legally valid or enforceable, and it may not reflect your current wishes. You should review and update your living will periodically, and share it with your provider, your designee, and your family.
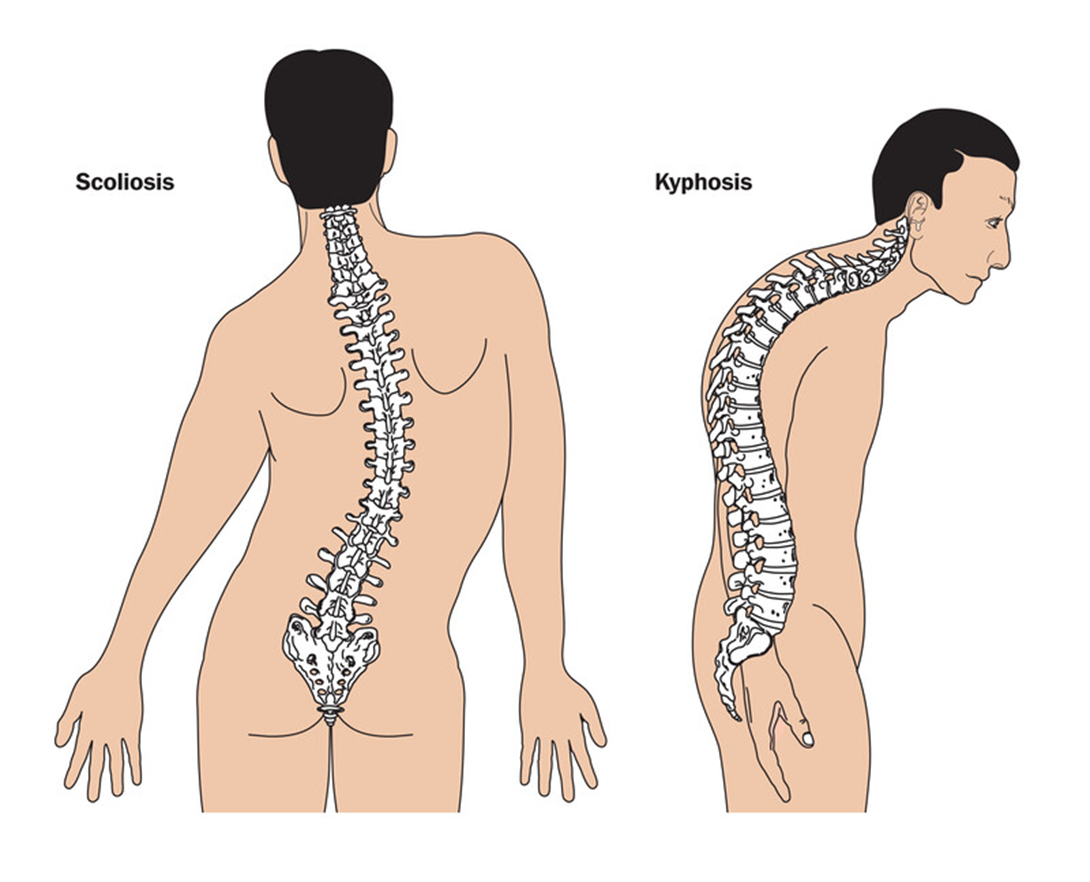
A nurse is assisting with scoliosis screenings for students at a public school. Which of the following findings should the nurse recognize as an indication of scoliosis?
Explanation
Choice A reason: Increased convex curve of the cervical spine is not an indication of scoliosis, but of kyphosis. Kyphosis is a condition that causes a forward rounding of the upper back, resulting in a hunched posture.
Choice B reason: Increased concave curve of the thoracic spine is not an indication of scoliosis, but of lordosis. Lordosis is a condition that causes an excessive inward curvature of the lower back, resulting in a swayback posture.
Choice C reason: Expansion of the upper intercostal spaces is not an indication of scoliosis, but of emphysema. Emphysema is a lung disease that causes the air sacs to become damaged and enlarged, resulting in difficulty breathing and a barrel chest.
Choice D reason: Unequal height of the shoulders is an indication of scoliosis. Scoliosis is a condition that causes a sideways curvature of the spine, resulting in an asymmetrical appearance of the shoulders, hips, and waist.
A nurse is reinforcing a teaching plan regarding proper lifting with a client. Which of the following strategies should the nurse include to prevent back injury when lifting an object?
Explanation
Choice A reason: Tightening the abdominal muscles is a good strategy to prevent back injury when lifting an object. The abdominal muscles support the spine and help maintain a neutral posture. Tightening them can reduce the stress on the back and prevent muscle strain or disc herniation.
Choice B reason: Bending at the waist is a bad strategy to prevent back injury when lifting an object. Bending at the waist can cause the spine to curve and lose its alignment. This can increase the pressure on the intervertebral discs and the spinal nerves, and lead to pain, inflammation, or nerve damage.
Choice C reason: Keeping legs straight is a bad strategy to prevent back injury when lifting an object. Keeping legs straight can limit the range of motion and the leverage of the lower body. This can force the back to do most of the work and increase the risk of injury. The nurse should bend the knees and hips and use the legs to lift the object.
Choice D reason: Holding the object away from the body is a bad strategy to prevent back injury when lifting an object. Holding the object away from the body can create a lever effect and increase the load on the back. This can cause the back muscles to overwork and fatigue, and lead to injury. The nurse should hold the object close to the body and keep it at the center of gravity.
Sign Up or Login to view all the 41 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

