ATI PN Fundamentals 2020 NGN Exam 1
Total Questions : 51
Showing 25 questions, Sign in for moreA nurse is preparing to administer medication to a preschooler and must convert the child's weight from pounds to kilograms. The child weighs 30 lb. How many kilograms does the child weigh?
(Round the answer to the nearest tenth. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
The correct answer is 13.6 kg.
To convert pounds to kilograms, the formula is weight in pounds divided by 2.2. Given the child's weight is 30 lb, the calculation would be 30 / 2.2 ≈ 13.64 kg. Rounding to the nearest tenth gives us 13.6 kg.
A nurse is preparing to obtain a client's vital signs. Which of the following actions should the nurse take when washing their hands?
Explanation
The correct answer is choice D.
Choice A rationale:
Rinsing forearms with running water before applying soap is not a recommended step in the handwashing procedure. The primary step is to wet the hands, apply soap, and create a lather.
Choice B rationale:
Holding hands above elbow level while washing and rinsing is not a standard practice for handwashing. The hands should be washed thoroughly, and the focus is on scrubbing the hands, not their positioning.
Choice C rationale:
Generating a lather by rubbing hands together vigorously for 5 seconds is insufficient for effective handwashing. Proper handwashing involves rubbing hands together for at least 20 seconds to ensure thorough cleaning.
Choice D rationale:
The correct answer. After washing and drying hands, turning off the faucet with a clean paper towel is recommended to avoid recontaminating the clean hands. Touching the faucet directly with clean hands could potentially transfer pathogens back onto the hands.

A nurse is preparing to perform a wound irrigation for a client who has a stage 3 pressure injury. Which of the following supplies should the nurse plan to use?
Explanation
Choice A rationale:
The correct answer. A piston syringe is used for wound irrigation to deliver a controlled and directed flow of fluid to clean the wound. It helps remove debris and promote healing. This choice aligns with wound irrigation best practices.
Choice B rationale:
Barrier ointment is not typically used for wound irrigation. Its purpose is to protect intact skin from moisture, friction, and other irritants, rather than to clean wounds.
Choice C rationale:
Chilled irrigation solution is not commonly used for wound irrigation. Room temperature or warm sterile saline is usually recommended for wound cleansing as cold solutions can cause discomfort and vasoconstriction.
Choice D rationale:
Sterile cotton balls are not used for wound irrigation. They may leave fibers in the wound, potentially leading to infection. Wound irrigation is usually performed using sterile syringes, solutions, and appropriate irrigation devices.
A nurse is caring for a client who reports itching 30 min after receiving a newly prescribed medication. Which of the following data should the nurse document in the client's medical record?
Explanation
The correct answer is choice B. Client states, "I started to itch after taking that medication."
Choice A rationale:
"Client is itching from medication." This statement is not a comprehensive description of the situation and lacks specific information. It doesn't provide any context about when the itching occurred or the client's own observation.
Choice B rationale:
"Client states, 'I started to itch after taking that medication.'" This choice is the correct answer because it accurately documents the client's own statement about the itching and the timing in relation to taking the medication. It includes a direct quote, which helps in maintaining accurate and patient-centered documentation.
Choice C rationale:
"It appears that the client has a rash from the medication." This statement includes an assumption and subjective language ("It appears"), which can be misleading in documentation. It's essential to provide factual and objective information in medical records.
Choice D rationale:
"Rash from medication noted." This choice lacks detail and doesn't capture the client's perspective or the timing of the symptom. It's important to include the client's statement and the time frame in which the symptom occurred.
A nurse is reinforcing teaching with a new parent who is concerned about sudden infant death syndrome (SIDS). Which of the following statements by the client indicates an understanding of the teaching?
Explanation
The correct answer is choice C. "I will remove all stuffed animals from my baby's crib."
Choice A rationale:
"I will place my baby on her side to sleep." Placing a baby on their side to sleep is not recommended as it increases the risk of sudden infant death syndrome (SIDS). The back sleep position is the safest for infants to reduce the risk of SIDS.
Choice B rationale:
"I should avoid giving my baby a pacifier." Using a pacifier during sleep actually has a protective effect against SIDS. It's recommended to offer a pacifier at naptime and bedtime after breastfeeding is well-established.
Choice C rationale:
"I will remove all stuffed animals from my baby's crib." This is the correct answer as it demonstrates an understanding of safe sleep practices. Soft bedding, including stuffed animals, can pose a suffocation hazard for infants. A clear and uncluttered crib is recommended for safe sleep.
Choice D rationale:
"I will cover my baby with a light blanket when she is sleeping." The use of blankets, even lightweight ones, in an infant's sleep environment is associated with an increased risk of SIDS. It's advised to keep the crib free from blankets, pillows, and other loose items.
A nurse is assisting with the admission of a client to a medical-surgical unit. Which of the following findings should the nurse identify as an indication that the client is malnourished?
Explanation
The correct answer is choice C. Pallor with scaly skin.
Choice A rationale:
"Heart rate 89/min." Heart rate within the range of 60-100 beats per minute is generally considered normal for adults at rest. This value doesn't specifically indicate malnourishment.
Choice B rationale:
"Pink mucous membranes." Pink mucous membranes indicate adequate oxygenation and hydration but don't necessarily reflect nutritional status or malnourishment.
Choice C rationale:
"Pallor with scaly skin." Pallor (pale skin) along with scaly skin can be indicative of malnourishment. Malnourished individuals may not receive adequate n
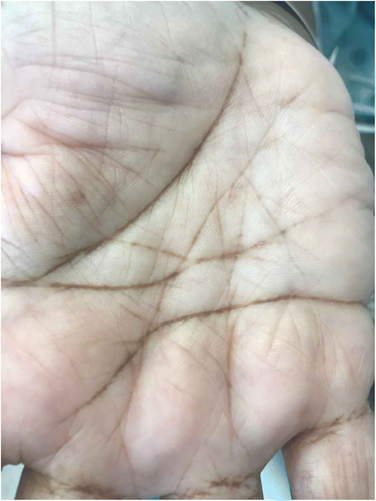
Choice D rationale:
"Body mass index 23." A body mass index (BMI) of 23 falls within the normal range (18.5-24.9), so it doesn't necessarily indicate malnourishment. However, BMI alone may not fully capture malnourishment, as it doesn't consider other factors like muscle mass and specific nutrient deficiencies.
A nurse is collecting data from a client following a lumbar puncture. The nurse should identify which of the following findings as a potential adverse effect of this procedure?
Explanation
The correct answer is choice C. Headache.
Choice A rationale:
Fluid overload is not a potential adverse effect of a lumbar puncture. A lumbar puncture involves the removal of cerebrospinal fluid (CSF) from the spinal canal, which wouldn't lead to fluid overload. This choice is not relevant to the procedure.
Choice B rationale:
Diarrhea is not a common adverse effect of a lumbar puncture. The procedure involves accessing the spinal canal and collecting CSF, which is not directly connected to the gastrointestinal system. Diarrhea is unrelated to the procedure.
Choice C rationale:
Headache is a potential adverse effect of a lumbar puncture. This is caused by the leakage of cerebrospinal fluid (CSF) through the puncture site, leading to a decrease in CSF pressure. This drop in pressure can cause a headache, particularly when the client sits or stands up. The headache is often described as severe and may be accompanied by neck pain and sensitivity to light. It usually resolves within a few days but can be managed with pain relief medications and plenty of fluids.
Choice D rationale:
Difficulty voiding is not a common adverse effect of a lumbar puncture. The procedure involves the lower back and spinal canal, and it doesn't directly affect the urinary system. This choice is unrelated to the procedure and its potential complications.
A nurse is caring for a client who has limited mobility. Which of the following actions should the nurse take to maintain the client's skin integrity?
Explanation
The correct answer is choice B. Place a donut-shaped cushion in the client's chair.
Choice A rationale:
Using warm water when bathing the client can be beneficial for maintaining skin integrity, as it helps in preventing excessive drying and irritation. However, for a client with limited mobility, the key concern is pressure ulcer prevention, which is not directly addressed by using warm water for bathing.
Choice B rationale:
Placing a donut-shaped cushion in the client's chair is an appropriate action to maintain the client's skin integrity. Donut-shaped cushions help relieve pressure on bony prominences like the coccyx (tailbone), reducing the risk of pressure ulcers. These cushions distribute the weight more evenly and prevent prolonged pressure on vulnerable areas of the skin.
Choice C rationale:
Massaging reddened areas over bony prominences is contraindicated for maintaining skin integrity. Massaging areas with signs of pressure can cause further damage to the already compromised skin and potentially lead to the development of pressure ulcers. This choice is not suitable for preventing skin breakdown.
Choice D rationale:
Maintaining the client in high-Fowler's position can be beneficial for respiratory and cardiac function, but it does not directly address the issue of maintaining skin integrity. High-Fowler's position may increase pressure on the sacrum and heels, making the client more susceptible to pressure ulcers. It's important to address pressure distribution specifically to prevent skin breakdown.
A nurse is collecting data from a client who is 1 day postoperative following abdominal surgery. Which of the following findings is the priority for the nurse to report to the provider?
Explanation
The correct answer is choice D. The client has tenderness and warmth in their calf.
Choice A rationale:
The client's self-reported incisional pain level of 7 on a scale of 0 to 10 is important information to assess postoperative recovery, but it is not the priority finding to report among the choices. Pain management is crucial, but potential complications that could be more urgent should be addressed first.
Choice B rationale:
Increased nausea and chills are concerning postoperative findings, but they could be related to the body's response to surgery, anesthesia, or pain medications. While these symptoms should be monitored and managed, they are not as high-priority as potential complications involving the calf.
Choice C rationale:
An oral temperature of 38.5°C (101.3°F) indicates a fever and is also a concerning finding in the postoperative period. Infection could be a possible cause, and the provider should be informed. However, compared to tenderness and warmth in the calf, which could suggest deep vein thrombosis (DVT), the fever is of slightly lower priority.
Choice D rationale:
Tenderness and warmth in the calf are the priority findings to report. These symptoms raise concern about the possibility of deep vein thrombosis (DVT), a serious complication after surgery. DVT occurs when a blood clot forms in a deep vein, commonly in the legs. If left untreated, it can lead to a pulmonary embolism, a life-threatening condition where the clot travels to the lungs. Immediate assessment and intervention are necessary to rule out or address this potentially critical complication.

A nurse is caring for a client who is scheduled for surgery the following day. During the night, the client is unable to sleep and is restless. Which of the following statements should the nurse make?
Explanation
The correct answer is choice D: "I can request a sleeping pill if you think that will help."
Choice A rationale:
Telling the client that "It must be difficult facing this type of surgery" acknowledges the client's emotions but does not address the issue of restlessness and difficulty sleeping. The nurse should focus on addressing the client's immediate concern.
Choice B rationale:
Mentioning that "Other clients who have had this surgery have done just fine" might minimize the client's feelings but does not provide a solution to the current problem of restlessness and difficulty sleeping. It also fails to acknowledge the individuality of the client's experience.
Choice C rationale:
Stating that "This facility is known for providing excellent care for people who need this type of surgery" is positive, but it does not directly address the client's current issue of restlessness and difficulty sleeping. The client needs a practical solution to their immediate problem.
Choice D rationale:
The nurse should choose choice D because it directly addresses the client's inability to sleep and offers a potential solution. Offering a sleeping pill shows that the nurse is responsive to the client's needs and is willing to take action to improve their comfort. However, it's important to consider the client's medical history and any contraindications before administering medication.
Explanation
Answer to Question
Here's the analysis of each option and the correct answer(s):
a. Place immunocompromised clients in the same room.
- Rationale:This action wouldincreasethe risk of infection for immunocompromised clients as they are more susceptible to infections from other residents.
b. Wash hands after removing gloves.
- Rationale:This action is crucial forpreventing the spread of pathogensfrom gloves to hands and subsequently to other clients or surfaces.This aligns with WHO's hand hygiene recommendations for healthcare settings.
c. Use antimicrobial hand gel after refilling a client's water pitcher.
- Rationale:While hand hygiene is essential,usingantimicrobial gel might not be necessaryin this specific scenario.Soap and water are generally sufficient for routine tasks like refilling a water pitcher unless there is visible contamination or a high risk of infection.
d. Clean the stethoscope with an antimicrobial wipe after obtaining vital signs.
- Rationale:Cleaning the stethoscope after each use helpsprevent the transmission of pathogensbetween clients.This aligns with CDC guidelines for preventing HAIs in long-term care facilities.
Therefore, the correct answers are b and d.
In summary:
- Avoid placing immunocompromised clients together.
- Always wash hands after removing gloves and between client contacts.
- Clean stethoscopes after each use.
- Antimicrobial gel may not be necessary for routine tasks like refilling water pitchers.
A nurse is caring for a client who reports difficulty sleeping at home. Which of the following recommendations should the nurse provide to promote a restful home sleep environment?
Explanation
The correct answer is choice A: "Perform muscle relaxation before bedtime."
Choice A rationale:
Suggesting to the client to "Perform muscle relaxation before bedtime" is a helpful recommendation. Muscle relaxation techniques, such as progressive muscle relaxation or deep breathing exercises, can help calm the body and mind, making it easier to fall asleep.
Choice B rationale:
Advising the client to "Exercise vigorously 1 hour prior to going to bed" is not recommended. Vigorous exercise close to bedtime can actually stimulate the body and make it harder to fall asleep. Gentle, non-strenuous activities are more suitable before bedtime.
Choice C rationale:
Recommending the client to "Drink a cup of hot chocolate at bedtime" is not ideal. Hot chocolate contains caffeine, which is a stimulant that can interfere with sleep. It's better to avoid caffeine-containing beverages close to bedtime.
Choice D rationale:
Suggesting the client to "Change the time you go to sleep each day" disrupts the body's internal clock and sleep-wake cycle. Maintaining a consistent sleep schedule, even on weekends, helps regulate the body's natural sleep patterns.
A nurse is preparing to remove staples from a client's incision. Which of the following actions should the nurse take?
Explanation
The correct answer is choice C: Expect the staples to bend at each outer side of the staple.
Choice A rationale:
The nurse should not lift the staple remover while squeezing the handle. Lifting the remover may cause the staple to become unsteady and increase the risk of injury or tearing the skin.
Choice B rationale:
The nurse should avoid completely closing the handle after squeezing. Completely closing the handle might result in crushing the staple, making it difficult to remove. Leaving a slight gap allows the staple to be easily extracted from the skin.
Choice C rationale:
This is the correct action to take. When removing staples, the nurse should expect the staples to bend slightly at each outer side as they are being lifted. This bending action helps to loosen the staple's grip on the skin, making it easier to remove without causing unnecessary discomfort to the patient.
Choice D rationale:
The nurse should remove the staple from the skin after both sides are visible. This ensures that the staple is not partially pulled or tugged, which could lead to pain or tearing of the skin. Having both sides visible indicates that the staple is ready to be extracted safely.
A nurse manager is reinforcing teaching with a group of newly licensed nurses about the disclosure of client health information. A nurse can disclose health information without the client's written permission to which of the following entities?
Explanation
The correct answer is choice C: A physical therapist who is involved in the client's care.
Choice A rationale:
Disclosing health information to an insurance agency offering a life insurance policy typically requires the client's written permission due to the sensitive nature of the information being shared, including medical history and conditions.
Choice B rationale:
Revealing a client's diagnosis to a family member without written consent would violate the client's privacy rights. Health information is protected by privacy laws, and disclosure should only occur with the client's explicit permission.
Choice C rationale:
This is the correct entity to whom health information can be disclosed without the client's written permission. Health professionals who are actively involved in the client's care, such as a physical therapist, are considered part of the healthcare team and may need access to relevant health information for proper treatment.
Choice D rationale:
Disclosing health information to an employer completing a pre-employment screening generally requires the client's consent, as pre-employment screenings often involve sharing medical information that could impact the employment decision.
A nurse is preparing a client for a Romberg test. Which of the following statements should the nurse make?
Explanation
The correct answer is choice A: "Stand with your feet together and your arms at your sides."
Choice A rationale:
This statement is correct. The nurse should instruct the client to stand with their feet together and their arms at their sides for a Romberg test. This position helps to assess the client's ability to maintain balance with minimal sensory input, evaluating their proprioception and vestibular function.
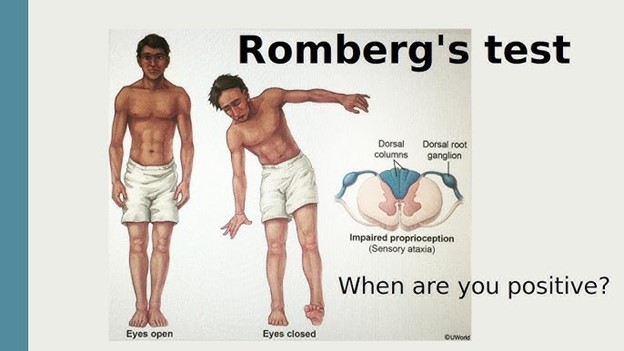
Choice B rationale:
The instruction about the tuning fork is unrelated to the Romberg test. The tuning fork is commonly used to assess hearing and vibratory sensations, not balance.
Choice C rationale:
This statement is unrelated to the Romberg test. Mentioning the lateral side of the foot suggests a neurological examination related to assessing reflexes, such as the Babinski reflex.
Choice D rationale:
This instruction pertains to a different test known as the "finger-to-nose" test, which is used to assess coordination, not balance.
A nurse is reinforcing teaching with the caregiver of a client who is near death. Which of the following instructions should the nurse provide?
Explanation
The correct answer is choice D: "Provide mouth care to them at least every 2 hours."
Choice A rationale:
Encouraging meals at least three times daily is not appropriate for a client who is near death. As clients approach the end of life, their appetite often decreases, and they may be unable to tolerate regular meals. It's more important to focus on providing comfort and relief.
Choice B rationale:
Keeping the room warm to help them breathe easier is not necessarily true. While a comfortable room temperature can be important for the client's overall comfort, warmth alone does not significantly impact breathing in the context of impending death. Breathing difficulties at this stage are usually related to physiological changes rather than room temperature.
Choice C rationale:
Helping the client onto their left side if they are experiencing nausea is not a universally applicable instruction. While left-side positioning can help alleviate nausea for some clients, it might not be suitable for everyone. Nausea can be caused by various factors, and the caregiver should assess the client's comfort and preferences before changing their position.
Choice D rationale:
Providing mouth care to the client at least every 2 hours is the most appropriate instruction among the choices. Near the end of life, many clients become less able to maintain their oral hygiene due to various factors, including weakness and reduced consciousness. This can lead to discomfort and potential complications. Regular mouth care helps keep the client's mouth moist and clean, enhancing their overall comfort.
A nurse is reinforcing teaching about advance directives with a client who has end-stage renal disease. Which of the following client statements indicates an understanding of the teaching?
Explanation
The correct answer is choice A: "I know that I can change my advance directives if I need to in the future."
Choice A rationale:
This statement indicates an understanding of advance directives. Advance directives are legal documents that allow individuals to communicate their preferences for medical treatment in case they become unable to make decisions themselves. It's important for clients to know that they can update or change their advance directives if their wishes or circumstances change over time.
Choice B rationale:
The statement that the health care surrogate will make decisions as soon as the power of attorney is signed is not accurate. Generally, a health care surrogate's authority to make decisions comes into effect when the primary individual is no longer able to make decisions themselves. Signing a power of attorney alone does not grant immediate decision-making power to the surrogate.
Choice C rationale:
The family generally cannot overrule the decisions made by a designated health care surrogate. Once an individual designates a surrogate and provides clear instructions through advance directives, the surrogate's decisions are legally binding and typically override the family's input.
Choice D rationale:
Advance directives are not universally valid across states. Laws and regulations regarding advance directives can vary significantly from state to state. It's important for clients to understand that if they relocate, they may need to update their advance directives to comply with the laws of the new state.
A nurse is contributing to the plan of care for a client who is at risk for developing foot drop due to immobility. Which of the following interventions should the nurse recommend to include in the plan?
Explanation
The correct answer is choice B: "Support the client's feet with foot boots."
Choice A rationale:
Flexing the client's feet using pillows might not be sufficient to prevent foot drop. Foot drop is a condition where the client is unable to dorsiflex their foot, and using pillows alone may not provide adequate support to prevent this condition.
Choice B rationale:
Supporting the client's feet with foot boots is the most appropriate intervention to prevent foot drop due to immobility. Foot boots are specifically designed to hold the foot in a dorsiflexed position, preventing the calf muscles from tightening and causing foot drop.
Choice C rationale:
Placing a hand roll under the client's heels might offer some relief, but it's not the most effective intervention for preventing foot drop. Hand rolls are generally used to prevent footdrop by keeping the ankles in a neutral position, rather than solely supporting the heels.
Choice D rationale:
Removing ankle-foot orthotic devices at bedtime is not recommended if the client is at risk for developing foot drop. Ankle-foot orthotic devices are designed to provide continuous support to the feet and prevent muscle contractures. Removing them at bedtime could compromise the effectiveness of the intervention.
A nurse is preparing to document information about a client's lower legs, which are swollen with 6 mm edema. Which of the following information should the nurse document?
Explanation
The correct answer is Choice C: 3+ pitting edema.
Choice A rationale:
1+ pitting edema refers to mild pitting edema. It is characterized by a slight indentation that disappears rapidly. A measurement of 6 mm edema is beyond the scope of 1+ pitting edema.
Choice B rationale:
2+ pitting edema indicates moderate pitting edema. It is characterized by a deeper indentation that takes a few seconds to rebound. While 6 mm edema might be associated with 2+ pitting edema, it is not the most accurate description.
Choice C rationale:
3+ pitting edema signifies moderately severe pitting edema. It is characterized by a noticeable indentation that remains for a short duration. A measurement of 6 mm edema aligns with 3+ pitting edema, making it the correct choice.

Choice D rationale:
4+ pitting edema represents severe pitting edema. It is characterized by a deep indentation that persists for a significant amount of time. 6 mm edema is not typically associated with 4+ pitting edema.
A nurse is caring for a client who has been vomiting and has diarrhea. Which of the following findings should the nurse identify as an indication of fluid volume deficit?
Explanation
The correct answer is choice B: A thready pulse.
Choice A rationale:
BUN (blood urea nitrogen) level of 18 mg/dL falls within the normal range, which is typically around 7-20 mg/dL. An elevated BUN might indicate dehydration or kidney dysfunction, but a value of 18 mg/dL does not necessarily suggest fluid volume deficit.
Choice B rationale:
A thready pulse is a weak and easily compressible pulse that indicates poor circulation and reduced fluid volume in the circulatory system. Vomiting and diarrhea lead to fluid loss, which can result in fluid volume deficit. Thus, a thready pulse is a significant finding in this context.
Choice C rationale:
Hemoglobin level of 15 g/dL is within the normal range for hemoglobin (usually around 12-16 g/dL for women and 14-18 g/dL for men). While vomiting and diarrhea can lead to mild dehydration, a hemoglobin level of 15 g/dL alone does not strongly suggest fluid volume deficit.
Choice D rationale:
Prominent neck veins are typically associated with increased central venous pressure, which can indicate fluid volume overload rather than fluid volume deficit. In the context of vomiting and diarrhea, neck veins are unlikely to become prominent due to volume depletion.
A nurse in a provider's office is providing care for a client who has minimal exposure to sunlight. Which of the following interventions should the nurse recommend?
Explanation
The correct answer is Choice C: Take vitamin D supplements.
Choice A rationale:
Reducing intake of calcium-rich foods would not be a suitable recommendation. Calcium is essential for bone health, and a client with minimal sunlight exposure is at risk of vitamin D deficiency, which affects calcium absorption. Therefore, this choice would worsen the client's situation.
Choice B rationale:
Using sunscreen with an SPF of 8 is unlikely to provide adequate protection against the harmful effects of sunlight. Moreover, the client's issue is vitamin D deficiency due to minimal sunlight exposure, and using sunscreen would further hinder vitamin D synthesis.
Choice C rationale:
Taking vitamin D supplements is the most appropriate intervention. Vitamin D is synthesized in the skin upon exposure to sunlight, and since the client has minimal sunlight exposure, supplements are necessary to prevent vitamin D deficiency. This choice addresses the root cause of the issue.
Choice D rationale:
Using a tanning bed is not recommended for increasing vitamin D levels. Tanning beds emit ultraviolet (UV) radiation, which can increase the risk of skin cancer. Moreover, excessive UV exposure is not a safe or controlled method for addressing vitamin D deficiency.
A nurse is caring for a client who has chronic kidney disease. The nurse should identify that which of the following findings is the priority to report to the provider?
Explanation
The correct answer is choice C: The client's WBC count is 11,000/mm².
Choice A rationale:
Client reports voiding three times during the night. Voiding three times during the night could be indicative of nocturia, a common symptom in chronic kidney disease due to decreased kidney function. While this symptom should be monitored and addressed, it is not the highest priority among the options provided. Nocturia is related to fluid balance and can be managed through dietary and medication adjustments.
Choice B rationale:
Client reports burning and discomfort with urination. Burning and discomfort with urination are suggestive of a urinary tract infection (UTI), which can be a concern in individuals with chronic kidney disease due to their compromised immune system. However, while this symptom requires attention, it is not as urgent as some other options in the list.
Choice C rationale:
The client's WBC count is 11,000/mm². An elevated white blood cell (WBC) count could indicate an infection, which is a significant concern for someone with chronic kidney disease. Kidney disease compromises the body's ability to fight infections, and if not promptly treated, an infection can lead to sepsis and further kidney damage. Thus, an elevated WBC count is the priority finding to report, as it requires immediate attention to prevent complications.
Choice D rationale:
The client's output was 60 mL for the past 3 hr. Low urine output could indicate decreased kidney function, but a single reading of low urine output is not as critical as an elevated WBC count, which signals a potential infection. Chronic kidney disease can lead to decreased urine output over time, but an acute drop in output is not as urgent as managing an infection.
A nurse is reinforcing teaching with a client about self-administration of ophthalmic drops. Which of the following instructions should the nurse include?
Explanation
The correct answer is choice A: "You will need to look to the side when you put the drops in your eye."
Choice A rationale:
"You will need to look to the side when you put the drops in your eye." This is the correct choice. Looking to the side helps to create a pocket between the eyeball and eyelid, which prevents the drops from immediately spilling out and allows the medication to be absorbed effectively.
Choice B rationale:
"You should put the drops directly in the center of your eyeball." Placing drops directly in the center of the eyeball can cause discomfort and may lead to less effective medication absorption. The goal is to place the drops in the conjunctival sac, which is the space between the eyeball and the lower eyelid.
Choice C rationale:
"You should cleanse your eye from the inner to the outer edge prior to putting in the drops." While it's important to keep the eye area clean, cleansing from the inner to the outer edge isn't directly relevant to administering ophthalmic drops. Proper hand hygiene and avoiding contamination of the dropper tip are more crucial to prevent infection.
Choice D rationale:
"You should avoid pressing on your tear duct after putting the drops in your eye." Avoiding pressure on the tear duct after instilling drops is a key point. Pressing on the tear duct can cause the medication to drain into the nasal passages, reducing its effectiveness. Therefore, this instruction is valid, but it's not the primary focus of proper administration.
A nurse is reinforcing teaching with a client who has hypertension and a prescription to measure their blood pressure daily. Which of the following client statements indicates an understanding of the teaching?
Explanation
The correct answer is choice C: "I should remove constrictive clothing prior to measuring my blood pressure."
Choice A rationale:
"I will wait 15 minutes after drinking coffee to measure my blood pressure." Caffeine intake can temporarily elevate blood pressure, so waiting 15 minutes after drinking coffee is a good practice. However, this is not the most relevant instruction to ensure accurate blood pressure measurement.
Choice B rationale:
"I will measure my blood pressure while my arm is elevated above my heart." Measuring blood pressure with the arm elevated above the heart can result in artificially low readings. The arm should be supported at heart level for accurate results. Therefore, this statement is incorrect.
Choice C rationale:
"I should remove constrictive clothing prior to measuring my blood pressure." This is the correct choice. Constrictive clothing can impact blood flow and give inaccurate readings. Removing tight clothing ensures the blood pressure cuff can be appropriately placed and that the measurements are reliable.
Choice D rationale:
"I should measure my blood pressure immediately after eating breakfast." Blood pressure can be affected by food intake, so it's recommended to wait at least 30 minutes after eating before measuring blood pressure. This choice is not accurate as immediate post-breakfast measurements may not provide accurate results.
A nurse is caring for a client who has an indwelling urinary catheter. Which of the following actions should the nurse take?
Explanation
The correct answer is choice B: Empty the drainage bag when it is three-fourths full.
Choice A rationale:
Cleaning the perineal area at least once a day is important for maintaining hygiene, but it is not the most relevant action in this scenario. The focus here is on managing the urinary catheter and its drainage bag.
Choice B rationale:
Emptying the drainage bag when it is three-fourths full is the correct action. An indwelling urinary catheter requires regular drainage to prevent the risk of infection and blockages. Allowing the bag to become too full could lead to backflow and increase the likelihood of urinary tract infections.
Choice C rationale:
Flushing the catheter with sterile water daily is not typically part of routine catheter care. Catheter flushing might be done for specific medical reasons, but it is not a general guideline for indwelling catheters.
Choice D rationale:
Disconnecting the drainage bag when emptying and measuring urine is incorrect. Maintaining a closed system is crucial to prevent introducing bacteria into the urinary tract. Disconnecting the bag could increase the risk of infection.
Sign Up or Login to view all the 51 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

