ATI PN Fundamentals 2020 with NGN Updated 2024
Total Questions : 41
Showing 25 questions, Sign in for moreA nurse in an acute care center is caring for a client who just died. The client’s family requests to perform the postmortem care. Which of the following is an appropriate response for the nurse to make?
Explanation
The correct answer is choice C. “I will assist you in any way I can during this process.” This response shows sensitivity and respect for the client’s family and their cultural or religious beliefs. Postmortem care involves caring for a deceased patient’s body with dignity and in a manner that is consistent with the patient’s and family’s wishes.The nurse should offer to assist the family in performing the postmortem care if they request to do so.
Choice A is wrong because the family does not need to sign a release form to perform the postmortem care themselves.
There is no legal requirement for this.
Choice B is wrong because a licensed health care worker does not have to perform postmortem care.
The family can perform the care themselves if they wish, with or without the assistance of a health care worker.
Choice D is wrong because postmortem care takes place before the client leaves the facility, not after.
Postmortem care should be provided as soon as possible to prevent tissue damage or disfigurement.
A nurse in a provider’s office performs a fecal occult blood test with a positive result on a client.
Which of the following clients may have a false positive result? A. A client who has a venous stasis ulcer.
Explanation
The correct answer is choice C. A client who underwent a barium swallow study may have a false positive result on a fecal occult blood test (FOBT).
This is because barium can interfere with the chemical reaction of the test and cause it to turn blue, indicating blood.
A client should avoid having a FOBT for at least four days after a barium swallow study.
Choice A is wrong because a client who has a venous stasis ulcer does not have bleeding in the gastrointestinal tract, which is what the FOBT detects.
Choice B is wrong because a client who has peripheral hematomas also does not have gastrointestinal bleeding.
Choice D is wrong because a client who takes an iron supplement does not have a false positive result on a FOBT, but may have a false negative result.
This is because iron can mask the presence of blood in the stool.
A nurse is caring for a client who refuses a prescribed medical procedure. Which of the following actions should the nurse take to act as a client advocate
Explanation
The correct answer is choice A. Evaluate the client’s concerns and communicate them to the provider.
This is because the nurse’s role as a patient advocate is to speak, act or behave in a way that benefits their patient, who may not be able to support or promote their own needs or interests.
The nurse should provide patients with information regarding their diagnoses, prognoses, treatments, and alternatives, and serve as a patient’s voice when necessary.
Choice B is wrong because contacting the unit’s social worker to report the client’s refusal is not an appropriate action for the nurse to take as a patient advocate.
The nurse should respect the patient’s autonomy and right to refuse treatment, and not involve other professionals without the patient’s consent.
Choice C is wrong because asking the client’s partner to find out why the client has refused the procedure is not an appropriate action for the nurse to take as a patient advocate.
The nurse should communicate directly with the patient and not rely on third parties to obtain information or influence the patient’s decision.
Choice D is wrong because explaining the necessity of the procedure to the client is not an appropriate action for the nurse to take as a patient advocate.
The nurse should not impose their own values or opinions on the patient, but rather provide unbiased and factual information and support the patient’s informed choice.
A nurse is planning to place a client into the Sims’ position.
Which of the following actions should the nurse plan to take?
Explanation
The correct answer is choice D. Placing a pillow under the client’s flexed leg is part of the Sims’ position, which is a way of lying on the left side, with the right hip and knee bent and the left arm behind the back.
It is used for vaginal and colonic examinations and natural childbirth.
Choice A is wrong because positioning the client’s arms at his sides is not part of the Sims’ position.
The left arm should be behind the back.
Choice B is wrong because elevating the client’s feet with two pillows is not part of the Sims’ position.
The lower leg should be straightened and the upper leg should be bent.
Choice C is wrong because raising the head of the client’s bed to a 30° angle is not part of the Sims’ position.
The bed should be flat or slightly tilted.
A nurse is collecting data from a client who had a stroke and is unable to name common items.
The nurse should recognize that the client is experiencing which of the following types of aphasia?
Explanation
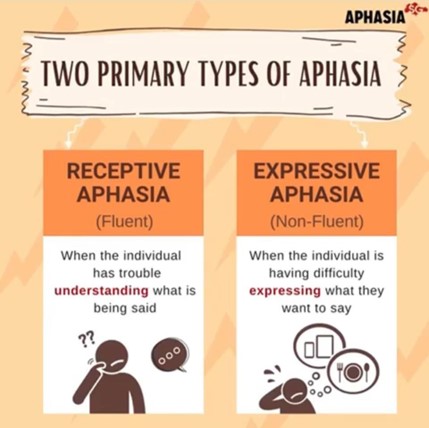
This type of aphasia is caused by damage to the frontal lobe of the brain, which affects the ability to produce language.
People with expressive aphasia can understand speech and know what they want to say, but they have difficulty saying words or forming sentences.
They may speak in short phrases that require a lot of effort.
Choice A is wrong because receptive aphasia is a type of fluent aphasia that affects the ability to comprehend language.
People with receptive aphasia have difficulty understanding speech and may produce meaningless words or sentences.
Choice C is wrong because global aphasia is the most severe type of aphasia that affects both the production and comprehension of language.
People with global aphasia cannot speak many words and do not understand speech.
They also cannot read or write.
Choice D is wrong because sensory aphasia is not a common term for a type of aphasia.
It may refer to Wernicke’s aphasia, which is another type of fluent aphasia that affects the ability to produce meaningful language.
People with Wernicke’s aphasia can speak fluently but often use incorrect or invented words or phrases.
A nurse is reinforcing information with a client who wishes to complete their advance directives.
Which of the following statements should the nurse make?
Explanation
The correct answer is choice D. A living will can specify which medical procedures a person wants or does not want to receive in certain situations, such as when they are terminally ill or permanently unconscious.
A living will is a type of advance directive, which is a legal document that provides instructions for medical care if a person is unable to make decisions for themselves.
Choice A is wrong because a person does not need to have advance directives in order to refuse recommended treatment.
They have the right to accept or decline any medical intervention at any time, as long as they are competent and able to communicate their wishes.
Choice B is wrong because a person does not need an attorney to name a designee in their health care proxy.
A health care proxy is another type of advance directive that appoints a person to make health care decisions for someone else if they are unable to do so.
A health care proxy can be completed without involving a lawyer, as long as it meets the state’s requirements for a valid document.
Choice C is wrong because a living will cannot be an oral statement that a person agrees upon with their provider.
A living will must be in writing and follow the state’s laws for creating legal documents.
Depending on the state, a living will may need to be signed by a witness or notarized.
A nurse is reviewing the laboratory results for a client who reports vomiting and diarrhea for 2 days.
Which of the following laboratory findings should the nurse expect?
Explanation
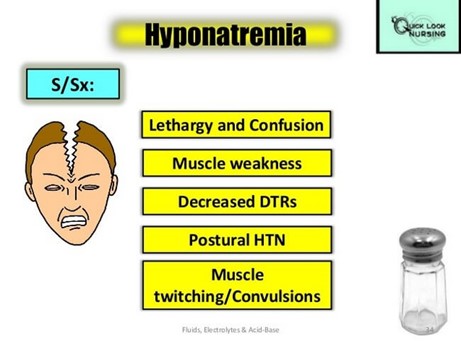
This means low sodium levels in the blood.
Sodium is an electrolyte that helps regulate fluid balance and nerve and muscle function.
Vomiting and diarrhea can cause dehydration and loss of sodium through fluids.
Normal sodium levels are between 135 to 145 millimole/Liter.
Choice A is wrong because hypermagnesemia means high magnesium levels in the blood.
Magnesium is another electrolyte that helps with nerve and muscle function, as well as blood pressure and blood sugar regulation.
Hypermagnesemia is rare and usually caused by kidney failure or excessive use of magnesium supplements or laxatives.
Normal magnesium levels are between 1.46 to 2.68 milligram/deciliter.
Choice C is wrong because hypocalcemia means low calcium levels in the blood.
Calcium is an electrolyte that helps with bone health, muscle contraction, blood clotting and nerve signaling.
Hypocalcemia can be caused by vitamin D deficiency, kidney disease, thyroid problems or certain medications.
Normal calcium levels are between 8.8 to 10.7 milligram/deciliter.
Choice D is wrong because hyperkalemia means high potassium levels in the blood.
Potassium is an electrolyte that helps with nerve and muscle function, especially the heart.
Hyperkalemia can be caused by kidney disease, diabetes, adrenal gland disorders or certain medications.
Normal potassium levels are between 3.6 to 5.5 millimole/Liter.
A nurse is showing a newly licensed nurse how to use a mechanical lift.
Which of the following statements by the newly licensed nurse indicates an understanding of this assistive device?
Explanation
The correct answer is choice D. This type of device is useful for a client who cannot assist.
A mechanical lift is used to transfer residents who cannot support their own weight.
It does not require the client to use upper body strength, as choice A suggests.
The lower end of the sling should go under the client’s thighs, not below the calves, as choice B states.
The sides of the sling are not for the client to hold on to, but for the caregiver to attach to the hooks on the lift, as choice C implies.
Therefore, choices A, B and C are wrong because they do not reflect the proper use of a mechanical lift.
A nurse is assisting with the admission of a client.
Which of the following statements should the nurse make to demonstrate the principle of advocacy?
Explanation
The correct answer is choice D. “I will let you make decisions about your health care.” This statement demonstrates the principle of advocacy in nursing, which is defined as a process aimed at promoting the independence and autonomy of users of health services, in addition to providing information on healthcare decision-making and offering support for decisions taken.
Choice A is wrong because it implies that the nurse will act on behalf of the client without their consent or involvement, which may violate their right to self-determination.
Choice B is wrong because it reflects the principle of fidelity, not advocacy.
Fidelity means keeping one’s promises and being faithful to one’s commitments. Choice C is wrong because it reflects
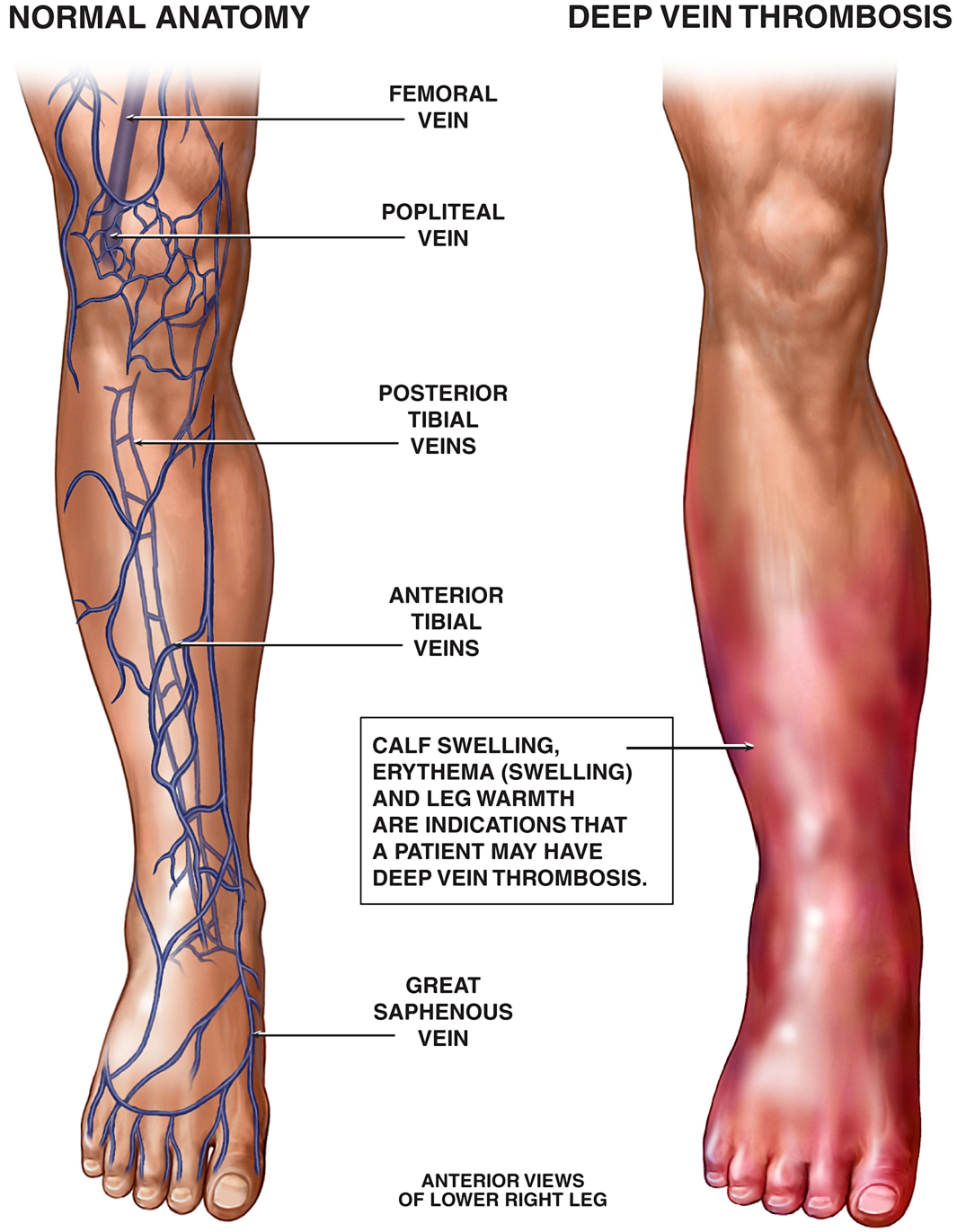
A nurse is collecting data from a client who is immobile and has a potential deepvein thrombosis.
Which of the following findings should the nurse report to the provider?
Explanation
A nurse is caring for a client who has experienced a cerebrovascular accident with resulting dysphagia.
Which of the following therapists assists clients to learn to eat with less risk of aspiration?
Explanation
Aspiration is when food or liquid enters the airway and causes choking or infection. Speech therapists can teach clients exercises to strengthen the muscles involved in swallowing, as well as strategies to prevent aspiration, such as changing the position of the head or the texture of the food.
Choice B is wrong because respiratory therapists help clients with breathing problems, not swallowing problems.
They may provide oxygen therapy, chest physiotherapy, or mechanical ventilation.
Choice C is wrong because physical therapists help clients with mobility problems, not swallowing problems.
They may provide exercises, massage, or assistive devices to improve movement and function.
Choice D is wrong because occupational therapists help clients with daily living activities, not swallowing problems.
They may provide training, adaptive equipment, or environmental modifications to enhance independence and quality of life.
Dysphagia is a medical term for swallowing difficulties.
It can be caused by various conditions that affect the nerves or muscles involved in swallowing, such as stroke, head injury, Parkinson’s disease, or esophageal cancer.
Dysphagia can lead to complications such as malnutrition, dehydration, or aspiration pneumonia.

A nurse is reinforcing teaching with a client about using guided imagery to manage chronic pain.
Which of the following statements by the client indicates an understanding of this technique?
Explanation
The correct answer is choice D. “I’ll think about my grandfather’s farm to reduce pain.” This statement indicates an understanding of guided imagery, which is a relaxation technique that aims to help lower the levels of stress hormones and pain perception by imagining a scene that involves each of the senses and positive emotions.
Guided imagery can help to distract from pain signals and reduce anxiety, which can also contribute to pain.
Choice A is wrong because it does not involve creating a specific imagined reality, but rather noticing the sensation of muscle tension, which may increase awareness of pain.
Choice B is wrong because it does not involve using all of the senses and emotions, but rather listening to music, which may be relaxing but not as effective as guided imagery for pain relief.
Choice C is wrong because it does not involve imagining a scene, but rather using focused breathing to control pain, which is another relaxation technique but not guided imagery.
A nurse is performing a wound irrigation for a client who has methicillin-resistant Staphylococcus aureus.
When removing personal protective equipment, which of the following pieces should the nurse remove first?
Explanation
The nurse should remove the gloves first because they are the most contaminated piece of personal protective equipment (PPE) and should be discarded as soon as possible.
The nurse should then remove the gown, which may also be soiled with blood or body fluids, by grasping it at the neck and peeling it off inside out.
The mask and goggles should be removed last, by touching only the straps or earpieces, and avoiding touching the front of the mask or the lenses of the goggles.
Choice A is wrong because goggles are not the most contaminated piece of PPE and should be removed after the gown.
Choice B is wrong because gown is not the most contaminated piece of PPE and should be removed after the gloves.
Choice C is wrong because mask is not the most contaminated piece of PPE and should be removed after the gown and goggles.
Normal ranges for wound irrigation pressure are between 4 and 15 psi (pounds per square inch).
Higher pressures may damage the wound tissue and increase the risk of infection.
Lower pressures may not be effective in removing debris and bacteria from the wound.
A nurse is collecting data about a client’s oral care. The client wears dentures and reports having mouth sores.
The nurse should identify which of the following oral care practices by the client as a possible cause of the mouth sores?
Explanation
It can also increase the risk of denture stomatitis and pneumonia.
Dentures should be removed overnight and soaked in a denture-cleansing solution.
Choice A is wrong because rinsing dentures after meals can help remove food debris and prevent plaque buildup.
Choice B is wrong because soaking dentures in water after removal can prevent them from drying out and losing their shape.

However, water alone is not enough to disinfect dentures, so a denturecleansing solution should also be used.
Choice C is wrong because applying an adhesive to seal dentures in place can improve the fit and comfort of dentures.
However, adhesive should not be used as a substitute for poorly fitting dentures, and any excess adhesive should be removed by brushing.
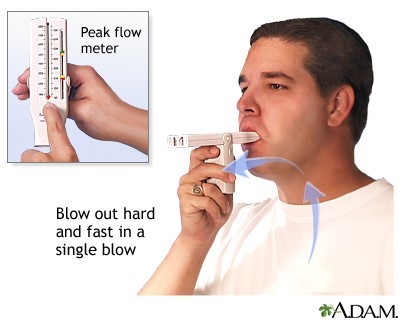
A nurse is reinforcing teaching with a client about the use of a peak flow meter.
Which of the following actions should the nurse take first?
Explanation
This is because the nurse should first assess the client’s baseline knowledge and readiness to learn before providing any teaching.
The nurse should also tailor the teaching to the client’s individual needs and preferences.
Choice B is wrong because showing the client a video demonstration of peak flow meter use may not be the most effective way of teaching if the client has different learning styles or needs.
The nurse should also involve the client in the learning process and not just rely on passive methods.
Choice C is wrong because observing the client using the peak flow meter is an evaluation step that should be done after teaching and reinforcing the correct technique.
The nurse should not assume that the client knows how to use the peak flow meter without assessing their knowledge first.
Choice D is wrong because emphasizing the importance of the daily use of the peak flow meter is a motivational strategy that should be done after assessing the client’s knowledge and providing teaching.
The nurse should also explain the rationale and benefits of using the peak flow meter, not just tell the client to do it.
A peak flow meter is a small device that measures how fast a person can forcefully blow air out of their lungs in one fast breath.
It is one indicator of airways changes that may occur in people with asthma or COPD.
To get a peak flow meter, speak to a doctor.
A nurse is wearing sterile gloves in preparation for assisting with a client’s sterile procedure.
While waiting for the procedure to begin, how should the nurse position her hands?
Explanation
The correct answer is choice A. Interlock her fingers and hold her hands away from her body above her waist.
This is because this position minimizes the risk of contaminating the sterile gloves by touching any non-sterile surfaces or objects.
The nurse should also keep her hands above her waistline to prevent contamination
Choice B is wrong because clasping the hands together behind the body at the waist could contaminate the gloves by touching the non-sterile gown or the skin
Choice C is wrong because placing one hand over the other against the part of the gown covering the upper body could contaminate the gloves by touching the non-sterile gown or the skin
Choice D is wrong because keeping the arms at the sides of the body with the hands in a relaxed position could contaminate the gloves by touching any nonsterile surfaces or objects
Sterile gloves are a type of disposable rubber gloves that are put through specific procedures to eliminate germs and microorganisms.
They are used to prevent and minimize infection during surgeries or invasive procedures
A nurse is reinforcing teaching with a newly hired nurse about cultural sensitivity during death and dying.
Which of the following information should the nurse include?
Explanation
The correct answer is choice B. Devout practitioners of Islam prefer to have their heads turned toward Mecca at death.
This is because Mecca is considered the holiest city in Islam and facing it is a sign of respect and devotion.
Choice A is wrong because devout practitioners of Buddhism prefer to be cremated rather than buried.
Cremation is seen as a way of releasing the soul from the body and preparing for rebirth.
Choice C is wrong because devout practitioners of Judaism prefer to be buried as soon as possible after death, usually within 24 hours.
This is based on the biblical commandment to bury the dead quickly and respect their dignity.
Choice D is wrong because devout practitioners of Hinduism prefer to be cremated after death and not buried.
Cremation is believed to help the soul detach from the body and achieve liberation.
A nurse is preparing to administer a medication from an ampule. Which of the following is an appropriate action for the nurse to take?
Explanation
The correct answer is choice C. Use a filter needle to aspirate the medication.
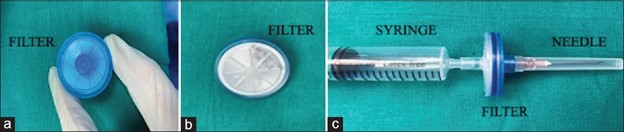
This is because a filter needle can prevent glass particles from being drawn into the syringe when aspirating medication from an ampule.
Glass particles can cause harm to the patient if injected.
Choice A is wrong because cleansing the tip of the ampule with an alcohol swab after opening is not necessary and may contaminate the medication.
Choice B is wrong because adding 0.5 mL of diluent to the medication may alter the concentration and dosage of the medication.
Choice D is wrong because injecting air into the ampule prior to drawing the medication into a syringe is not required and may create pressure that can cause the ampule to break.
A nurse is caring for a client who has a hip fracture and plans to administer pain medication prior to turning the client.
Which of the following ethical principles is the nurse implementing?
Explanation
Beneficence is the ethical principle of doing good and acting in the best interest of the patient. By administering pain medication prior to turning the client, the nurse is reducing the client’s suffering and promoting their well-being.
Choice A. Autonomy is wrong because autonomy is the ethical principle of respecting the patient’s right to self-determination and decision-making. The nurse is not asking for the client’s consent or preference before giving pain medication or turning them.
Choice B. Fidelity is wrong because fidelity is the ethical principle of being faithful and loyal to the patient and honoring one’s commitments and promises. The nurse is not demonstrating fidelity by giving pain medication or turning the client.
Choice C. Veracity is wrong because veracity is the ethical principle of telling the truth and being honest with the patient. The nurse is not providing any information or education to the client before giving pain medication or turning them.
A nurse on a medical-surgical unit is collecting data from a client who is postoperative following abdominal surgery.
The client’s BP was 126/72 mm Hg 15 min ago. The nurse now finds that the client’s BP is 176/96 mm Hg. Which of the following actions should the nurse take?
Explanation
It's common practice to check blood pressure in both arms when there is a significant discrepancy in blood pressure readings between the arms. This discrepancy could be due to factors like arterial blockages or other conditions. By measuring the blood pressure in the other arm, the nurse can confirm whether the high blood pressure is consistent on both sides or if there was an issue with the initial measurement. This step helps provide a more accurate assessment of the client's blood pressure.
- The other options are not appropriate at this stage:
Deflating the cuff faster may not resolve the issue and could lead to inaccurate measurements.
Requesting a prescription for an antihypertensive medication should only be done after confirming the blood pressure is consistently elevated and under the direction of a healthcare provider.
Using a narrower cuff is not indicated in this situation. It's more important to assess the other arm's blood pressure to identify any discrepancies.
While performing hygiene care for a client, a nurse notices a frayed electrical cord on the client’s electronic blood pressure monitor.
Which of the following actions should the nurse take first?
Explanation
This is because a frayed electrical cord can pose a serious risk of electric shock or fire to the client and the nurse.
The nurse should act quickly to eliminate the hazard and ensure the safety of the client and others.
Choice B is wrong because accessing the facility’s maintenance protocol is not the first action the nurse should take.
The nurse should prioritize removing the device from the room before following any protocol.
Choice C is wrong because reporting defective equipment is not the first action the nurse should take.
The nurse should prioritize removing the device from the room before reporting it to the appropriate authority.
Choice D is wrong because requesting a replacement device is not the first action the nurse should take.
The nurse should prioritize removing the device from the room before requesting a new one.
A nurse is preparing to administer sucralfate 80 mg/kg/day to divide into four doses per day to a child who weighs 35 kg.
The amount available is sucralfate oral suspension 1 g/10 mL. How many mL should the nurse administer per dose? (Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
A nurse is preparing to administer sucralfate 80 mg/kg/day to divide into four doses per day to a child who weighs 35 kg.
The amount available is sucralfate oral suspension 1 g/10 mL. How many mL should the nurse administer per dose? (Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.) mL.
Answer and explanation.
The correct answer is choice B. To calculate the dose per mL, we need to use the following formula:
Dose per mL=Amount availableDose per kg×Weight Plugging in the given values, we get:
Dose per mL=1 g/10 mL80 mg/kg×35 kg
Simplifying the units and converting grams to milligrams, we get:
Dose per mL=1000 mg/10 mL2800 mg Dividing both sides by 10, we get:
Dose per mL=0.28 mL
Multiplying both sides by 4, we get the dose per day:
Dose per day=1.12 mL
Rounding to the nearest whole number, we get 1 mL as the answer.
Choice A is wrong because it uses 40 mg/kg instead of 80 mg/kg as the dose per kg.
Choice C is wrong because it uses 20 kg instead of 35 kg as the weight.
Choice D is wrong because.
A nurse observes assistive personnel (AP) perform mouth care for a client who is unconscious.
Which of the following actions by the AP requires intervention by the nurse?
Explanation
The correct answer is choice A. Lowering the side rail on the side of the bed where they will stand to perform mouth care.
This action by the AP requires intervention by the nurse because it increases the risk of the patient falling out of the bed or injuring themselves on the rail. The side rail should be kept up at all times unless it is necessary to lower it for a specific procedure or transfer.
Choice B is wrong because using an oral care sponge swab moistened with cool water to clean the client’s mouth is an appropriate action by the AP.
Oral care sponge swabs are designed to gently clean and moisten the oral cavity of patients who are unconscious or have difficulty swallowing. Cool water can help to soothe and refresh the mouth.
Choice C is wrong because wearing clean gloves to perform mouth care for the client is an appropriate action by the AP.
Gloves are part of standard precautions to prevent cross-contamination and protect both the patient and the caregiver from infections.
Choice D is wrong because using two gloved fingers to open the client’s mouth for cleaning is an appropriate action by the AP.
This technique can help to access the oral cavity of an unconscious patient without causing injury or discomfort. The AP should also use a bite block or a padded tongue depressor to prevent the patient from biting their fingers.
A nurse is assisting in the transfer of a client who has left-sided weakness from a bed to a chair.
Which of the following actions should the nurse take?
Explanation
The correct answer is choice C. The nurse should stand on the client’s stronger side when moving the client into the chair. This will allow the nurse to support the client’s weaker side and prevent injury.
According to the search results, aligning the nurse’s knee with the client’s knees just before the transfer is a correct strategy that helps the nurse safely stabilize the client while moving to a standing position.
Choice A is wrong because raising the bed to waist level before moving the client can increase the risk of falls and make it harder for the client to stand up.
The bed should be in the lowest position throughout the procedure.
Choice B is wrong because pivoting on the foot farthest from the bed when assisting the client into the chair can cause twisting and strain on the client’s back and legs.
The nurse should pivot on the foot closest to the bed and instruct the client to do the same.
Choice D is wrong because grasping the client under the axillae to assist them to their feet can damage the client’s nerves and muscles in the shoulder area.
The nurse should use a gait belt around the client’s waist and grasp it firmly with both hands.
A nurse is reinforcing teaching with a client who needs to increase vitamin C intake to promote wound healing.
Which of the following foods should the nurse recommend as the best source of vitamin C?
Explanation
This food has the highest vitamin C content among the four options, with about 80 to 100 mg of vitamin C per fruit.
Vitamin C is a water-soluble vitamin that acts as an antioxidant and helps with wound healing, immune function, collagen synthesis, and iron absorption.
Choice A is wrong because 1 medium fresh green pear has only about 4 to 5 mg of vitamin C per fruit.
Pears are a good source of fiber and potassium, but not vitamin
C. Choice B is wrong because 1 small apple with the skin has only about 8 to 9 mg of vitamin C per fruit.
Apples are a good source of fiber and flavonoids, but not vitamin
C. Choice C is wrong because 1 small banana has only about 10 to 11 mg of vitamin C per fruit.
Bananas are a good source of potassium, magnesium, and vitamin B6, but not vitamin
Sign Up or Login to view all the 41 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

