ATI PN Fundamentals of Nursing 2020 with NGN Exam 2
Total Questions : 49
Showing 25 questions, Sign in for moreA nurse is reinforcing teaching with a newly hired nurse about cultural sensitivity during death and dying. Which of the following information should the nurse include?
Explanation
A. Devout practitioners of Buddhism prefer a ritual bath prior to burial.
Explanation: In Buddhism, the funeral customs can vary widely depending on the cultural and regional practices. Some Buddhists may prefer cremation, while others may choose burial. There isn't a strict requirement for a ritual bath, and practices can differ.
B. Devout practitioners of Judaism prefer to be buried 5 days after death.
Explanation: In Judaism, there is a tradition of burying the deceased as soon as possible, ideally within 24 hours. Waiting for 5 days is not consistent with Jewish burial practices.
C. Devout practitioners of Hinduism prefer to be buried after death and not cremated.
Explanation: In Hinduism, cremation is a common practice. Hindus believe in the cycle of reincarnation, and cremation is seen as a way to release the soul from the body. Burial is not a typical practice in Hinduism.
D. Devout practitioners of Islam prefer to have their heads turned toward Mecca at death.
Explanation: In Islam, it is a common practice to bury the deceased with their right side facing the Qiblah, which is the direction of the Kaaba in Mecca. This is part of the Islamic funeral rites.
A nurse is caring for a client who has experienced a cerebrovascular accident with resulting dysphagia. Which of the following therapists assists clients to learn to eat with less risk of aspiration?
Explanation
Choice Reason:
Occupational Therapist is incorrect. Occupational therapists focus on helping individuals regain or enhance their ability to perform daily activities and tasks. While they might not directly address dysphagia or swallowing concerns, they could assist in modifying the environment or providing adaptive equipment to facilitate eating, such as recommending specialized utensils or adapting seating positions to support safe eating practices.
Choice B Reason:
Physical Therapist is incorrect. Physical therapists primarily concentrate on restoring mobility, strength, and function in individuals who have experienced injuries or illnesses affecting movement. While they might not directly address dysphagia, they could be involved in helping patients with postural adjustments or exercises that indirectly support safe eating and swallowing.
Choice C Reason:
Respiratory Therapist is incorrect. Respiratory therapists specialize in assessing and treating breathing problems and disorders related to the lungs and respiratory system. While they may not focus directly on dysphagia, they can be involved in managing respiratory complications that can arise from aspiration, such as pneumonia. They might assist in suctioning, breathing exercises, or respiratory treatments in cases where aspiration has led to lung issues.
Choice D Reason:
Speech therapists, also known as speech-language pathologists, is correct because it specializes in evaluating and treating communication and swallowing disorders. They work with individuals who have experienced strokes or other conditions affecting swallowing abilities to improve their swallowing function and reduce the risk of aspiration (when food or liquid enters the airway instead of the digestive tract).
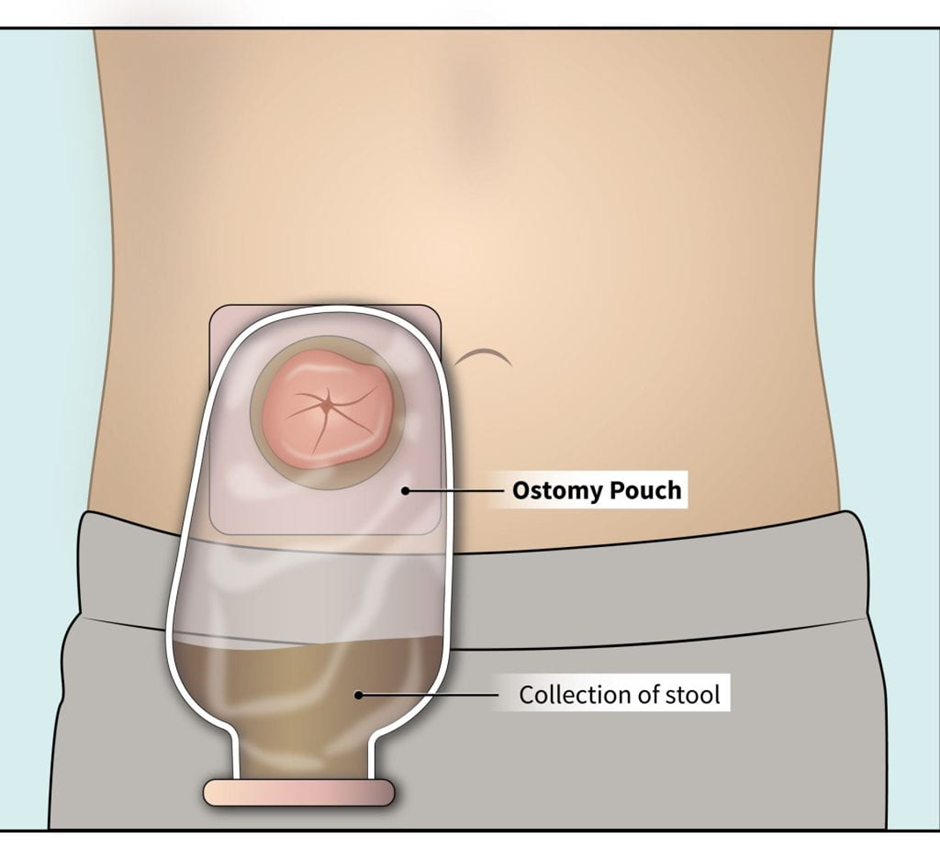
A nurse is reinforcing teaching with a client who has an ostomy. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A Reason:
"I will press on the skin barrier for 30 seconds to ensure that it adheres." This statement does not indicate the understanding of the teaching. While pressing on the skin barrier is essential to ensure proper adhesion, the duration of 30 seconds might not be sufficient. It's usually recommended to press and hold the barrier for a longer duration (around a minute) to ensure it adheres securely.
Choice B Reason:
"I will clean around the stoma with a moisturizing soap ."This statement does not indicate the understanding of the teaching. Using a moisturizing soap isn't typically recommended for cleaning around the stoma. Instead, gentle cleansing with mild soap and water or specialized ostomy cleansing products is preferred. Moisturizing soaps may contain ingredients that could irritate the skin or interfere with the adhesion of the barrier.
Choice C Reason:
"I will apply a thin layer of talc powder around the stoma before placing the appliance. "This statement does not indicate the understanding of the teaching. Using talc powder or other powders around the stoma area is generally discouraged. These powders can lead to complications such as clogging the ostomy appliance's filter or causing skin irritation.
Choice D Reason:
"I will cut an opening in the skin barrier that is 1⁄2 inch larger than the stoma." This statement indicates the understanding of the teaching. Ensuring the skin barrier has an opening that is slightly larger than the stoma helps in preventing irritation and ensures a proper fit, allowing the stoma to function without causing damage to the surrounding skin.
A nurse is performing postmortem care for a client who was a devout Muslim. Which of the following actions should the nurse take?
Explanation
Choice A Reason:
Allowing the family to participate in washing the client's body is appropriate. In Islamic tradition, it's customary for family members or individuals of the same gender to participate in washing the deceased's body. This practice is a part of the Islamic ritual of ghusl (ritual washing). It's respectful and important to honor the religious and cultural customs of the deceased and their family.
Choice B Reason:
Providing the family with an eagle feather for the client's hair is inappropriate. In Islamic traditions, the use of eagle feathers or any specific animal-related items isn't a part of postmortem care rituals. Additionally, incorporating items from other traditions or cultures might not align with the religious practices or beliefs of the deceased and their family.
Choice C Reason:
Encouraging the family to chant a mantra before moving the body is inappropriate. Chanting mantras isn't a practice in Islamic postmortem care. Islamic rituals involve specific prayers and actions according to the teachings of Islam, and chanting mantras isn't a part of this tradition.
Choice D Reason:
Dressing the client in a special amulet provided by the family is inappropriate. The use of amulets or charms isn't typically part of Islamic postmortem rituals. Islamic customs emphasize modesty in dress and following specific rites for the deceased, but incorporating special amulets or charms isn't a common practice.
A nurse is reinforcing teaching with a client who has recurrent back injuries related to lifting. Which of the following lifting instructions should the nurse include?
Explanation
Choice A Reason:
Keeping the knees straight is not appropriate. It's advisable to bend the knees while lifting to engage the leg muscles and reduce strain on the back.
Choice B Reason:
Standing with the feet close together is not appropriate. Having a wider stance provides better stability and balance while lifting heavy objects, which is preferable to standing with the feet close together.
Choice C Reason:
Holding objects away from the torso is not appropriate. Keeping objects close to the body while lifting helps maintain control and reduces strain on the back. Holding objects away from the torso can increase the load on the back muscles and lead to injury.
Choice D Reason:
Aligning the back with the neck and feet is appropriate. This instruction emphasizes maintaining proper alignment of the body during lifting to reduce strain on the back muscles and minimize the risk of injury.
A nurse is reinforcing teaching about advance directives with a client who has terminal colorectal cancer. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A Reason:
"I'll need to sign a separate consent form first." This statement might indicate a misunderstanding of the process or a belief that signing an advance directive requires a separate consent form, which might not be accurate.
Choice B Reason:
“the opportunity to choose what kind of care I receive while I still can. "This statement reflects the understanding that advance directives allow individuals to make decisions about the type of care they wish to receive while they are still capable of expressing their preferences. Advance directives, such as a living will, enable individuals to outline their healthcare preferences in advance, especially in situations where they might not be able to communicate their wishes later due to illness or incapacity.
Choice C Reason:
“living will, there will be a 1-month delay before it is legally binding. “There typically isn't a standard delay before a living will becomes legally binding. Once the living will be properly completed and witnessed according to legal requirements, it becomes effective.
Choice D Reason:
“have my mind about the care I will receive once I sign my living will." The purpose of a living will be to express one's healthcare preferences in advance. While it's possible to update or change a living will if one's preferences change, signing a living will doesn't inherently mean one can easily alter care preferences once it's in place. Amendments or revocations might require specific legal steps.
A nurse is assisting with discharge planning for an older adult client who has vision loss. Which of the following instructions about home safety should the nurse include in the plan?
Explanation
Choice A Reason:
Setting the maximum water heater temperature to 54.4° C (130° F) is appropriate. This temperature is too high and could pose a burn risk, especially for someone with impaired vision who might not easily detect very hot water.
Choice B Reason:
Painting the edges of steps for contrast is appropriate. This measure helps increase visibility by creating a visual contrast between the edges of steps and the surrounding area, aiding the individual in identifying the steps more easily, even with reduced vision.
Choice C Reason:
Securing extension cords across walkways is inappropriate. Placing extension cords across walkways can create tripping hazards, particularly for someone with vision loss who may have difficulty seeing these obstacles.
Choice D Reason:
Using 40-watt bulbs to light hallways is inappropriate. While adequate lighting is crucial for individuals with vision impairment, using only 40-watt bulbs might not provide sufficient illumination. It's recommended to use higher-wattage bulbs or brighter lighting sources to ensure better visibility in the home.
A home health nurse is reinforcing teaching about dietary needs with the son of a client. The son states, "I don't know what to do because he's not eating." Which of the following responses should the nurse make?
Explanation
Choice A Reason:
"He may need a feeding tube" is inappropriate response. Suggesting a feeding tube without further assessment or information might be premature and could cause unnecessary concern or anxiety for the son. It's essential to explore the situation more before proposing such an intervention.
Choice B Reason:
"Tell me more about what happens at mealtime” is appropriate response. This response encourages the son to provide further details about the situation, allowing the nurse to gather more information about the specific issues or challenges related to the client's eating habits. Understanding the circumstances around mealtime can help the nurse identify potential reasons for the lack of appetite or eating difficulties and offer more targeted guidance or solutions.
Choice C Reason:
"Why do you think he's not eating?" This response is inappropriate. While asking about the son's thoughts is valuable, this question might not directly address the situation at hand or provide immediate assistance or guidance to address the client's eating difficulties.
Choice D Reason:
"I'm sure it's nothing serious and his appetite will return soon” is inappropriate response. Offering reassurance without understanding the underlying cause may downplay a potentially concerning issue. It's crucial to investigate the reasons behind the lack of appetite before assuming it will resolve without further action.
A nurse is caring for a client who is angry and states, "The doctor gave me the wrong information. I was lied to!" Which of the following responses by the nurse is appropriate?
Explanation
Choice A Reason:
"Your doctor has an excellent reputation for being honest with clients." This response is incorrect. While intending to provide reassurance, this statement may come across as dismissive of the client's feelings and might not address their immediate concern.
Choice B Reason:
"Why do you think the doctor is lying?" This response is incorrect. This response might come off as confrontational or defensive. It could potentially escalate the client's emotions and not effectively address their feelings of being misled.
Choice C Reason:
"You feel as if the doctor hasn't been honest with you?" This response acknowledges the client's emotions and concerns without making assumptions about the doctor's actions. It demonstrates empathy and allows the client to express their feelings and concerns further.
Choice D Reason:
"I am certain the doctor would not lie to you." This response might be perceived as dismissive or invalidating of the client's feelings and beliefs, as it asserts the nurse's certainty without fully understanding the client's perspective.
A nurse is caring for a client who is pulling on his NG tube. Which of the following actions should the nurse take first?
Explanation
Choice A Reason:
Administering sedative medication should not be the first action. It is important to assess the client's level of comfort and understand the reason for pulling on the NG tube before considering sedation. Sedation may mask underlying issues, and the goal is to address the cause of the behavior.
Choice B Reason:
Assessing the client's level of comfort is the priority. Understanding the reason for pulling on the NG tube is crucial before implementing interventions. The client may be experiencing pain, discomfort, anxiety, or another issue that needs to be addressed.
Choice C Reason:
Applying a restraint should be a last resort and is not the initial action. Restraints are used to ensure safety when other measures have failed. The priority is to address the underlying cause and promote comfort without resorting to restraint.
Choice D Reason:
Documenting the client's behavior is important for the medical record, but it comes after assessing and addressing the immediate needs of the client. Understanding the context and reasons for the behavior is crucial for accurate documentation.
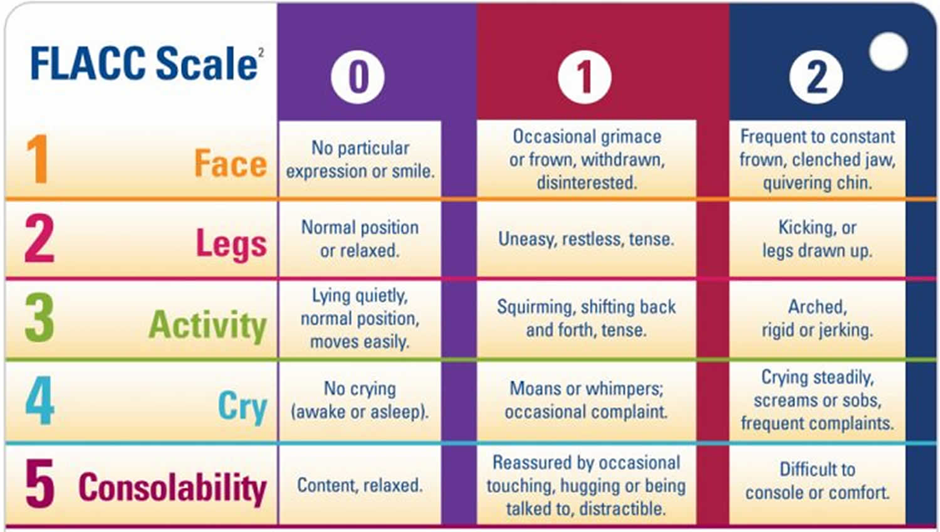
A nurse is caring for a who speaks a different language than the nurse and is 6 hr postoperative. Which of the following actions should the worse take to determine the client's level of pain?
Explanation
Choice A Reason:
Using the FACES pain scale to gauge the client's level of pain is appropriate. This scale relies on the client's ability to understand and communicate using a specific language, which might not be possible if there is a language barrier.
Choice B Reason:
Using a communication board to interact with the client is inappropriate. While communication boards can be helpful, they might not effectively gauge the client's level of pain, especially if the client's primary language isn't available on the board.
Choice C Reason:
Using the Face, Legs, Activity, Cry, Consolability (FLACC) scale to measure the client's pain level is appropriate. The FLACC scale is a pain assessment tool that evaluates pain in nonverbal patients or those who can't communicate effectively. It assesses facial expressions, leg movement, activity level, crying, and consolability to determine the level of pain the patient is experiencing.
Choice D Reason:
Asking an assistive personnel who speaks the same language as the client to interpret is inappropriate. Relying on an interpreter, even if they speak the same language as the client, might not be the best approach for pain assessment, as nuances related to pain expression and interpretation might be better captured through a standardized pain assessment tool like the FLACC scale.
A nurse is performing eye care for a client who is in a coma. Which of the following actions should the nurse take? (Select all that apply.)
Explanation
Choice A Reason:
Wiping the eyes from the outer to the inner canthus is inappropriate. This direction of wiping might risk introducing contaminants into the eyes. It's generally advised to wipe from the inner to the outer canthus to minimize the risk of introducing potential eye irritants.
Choice B Reason:
Applying eye patches over the eyes if the eyelids do not close completely is appropriate. Eye patches help protect the eyes from potential damage, dryness, or exposure to light if the eyelids do not close fully.
Choice C Reason:
Cleansing the eyes with a chlorhexidine solution is inappropriate. Chlorhexidine solution might be too harsh for use around the delicate eye area and could cause irritation or damage to the eyes. Using a gentler and specifically formulated eye cleansing solution or sterile saline is usually recommended for eye care.
Choice D Reason:
Placing moist compresses over the eyes every 2 to 4 hours is appropriate. Moist compresses can help maintain moisture and prevent dryness in the eyes, reducing the risk of corneal damage due to the inability to blink.
Choice E Reason:
Instilling lubricating eye drops into the lower lid of each eyeis appropriate. Lubricating eye drops help prevent dryness and maintain eye moisture, offering protection to the cornea.
A nurse is coordinating care of a group of clients with an assistive personnel (AP). Which of the following tasks should the nurse assign to the AP?
Explanation
A. Check a client's peripheral IV site for redness or swelling.
This task involves assessing the client's IV site for signs of complications. While it requires observation and reporting, it may involve some interpretation and judgment. This task is better suited for a licensed nurse.
B. Measure the intake and output of a client who has received furosemide.
Measuring intake and output is a routine task that involves quantifying the fluids a client consumes and eliminates. This is a task that can be appropriately delegated to an assistive personnel (AP) under the supervision and direction of the nurse.
C. Reinforce teaching with a client about crutch-gait walking.
Teaching requires a level of education, explanation, and clarification that goes beyond routine tasks. This is typically a nursing responsibility and should not be delegated to an AP.
D. Assess the pain level of a client who has received acetaminophen.
Pain assessment involves subjective information, and determining the appropriate response may require clinical judgment. This task is better suited for a licensed nurse.
A nurse is reinforcing teaching about end-of-life care with the partner of a client. Which of the following statements should the nurse make?
Explanation
Choice A Reason:
"Opioids will be restricted if your partner develops respiratory distress." This statement might cause unnecessary concern or confusion. While opioid use might be adjusted based on the client's condition and symptoms, framing it in terms of restriction might not be the most appropriate way to communicate about pain management in end-of-life care.
Choice B Reason:
"Encourage your partner to eat three large meals each day." Encouraging large meals might not align with the typical dietary approach for someone in end-of-life care, especially if they have reduced appetite or are unable to eat comfortably. End-of-life care often focuses on providing smaller, more manageable meals based on the individual's preferences and capabilities.
Choice C Reason:
"Assume your partner can hear you, even if they do not respond. “This statement encourages the partner to communicate with their loved one, acknowledging the potential for the person to hear even if they are not responsive. Many studies suggest that hearing may persist even in individuals who are unresponsive or in a comatose state, so speaking to them can provide comfort and connection.
Choice D Reason:
"We will use an electric blanket to keep your partner warm." The use of an electric blanket might not be suitable, as the client's sensitivity to temperature might change in end-of-life care. Other methods, such as blankets or adjusting the room temperature, could be more appropriate to ensure comfort without the risks associated with electric blankets.
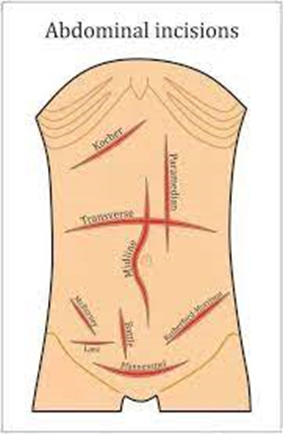
A nurse is replacing a dressing for a client who has an abdominal incision with a closed wound drain. Which of the following actions should the nurse take?
Explanation
Choice A Reason:
Pushing the skin down while gently removing the tape is incorrect. Pushing the skin while removing tape could cause unnecessary discomfort or trauma to the skin and the incision area. Gentle removal of tape without pulling the skin is recommended to avoid skin injury.
Choice B Reason:
Drying the incision with sterile gauze pads is incorrect. Generally, it's advisable not to dry the incision site with sterile gauze pads as this might cause trauma or disruption to the healing tissues. Patting the incision site dry or allowing it to air dry gently after cleansing is preferable.
Choice C Reason:
Lifting the soiled dressing so that the underside faces the client is correct. Lifting the soiled dressing in a manner that the underside faces the client helps prevent potential contamination of the wound by minimizing contact between the external surface of the dressing and the incision site. This technique reduces the risk of introducing pathogens into the wound during the dressing change.
Choice D Reason:
Cleaning around the drain site using horizontal strokes is incorrect. When cleaning around the drain site, it's typically recommended to use gentle and careful motions without specific emphasis on strokes, as this might cause friction or trauma to the area around the drain. Instead, using gentle circular motions or dabbing around the site is often advised for wound care.
A nurse observes an assistive personnel (AP) perform mouth care for a client who is unconscious. Which of the following actions by the AP requires intervention by the nurse?
Explanation
Choice A Reason:
Lowering the side rail on the side of the bed where the AP will stand to perform mouth care is a safety measure. It provides better access to the client and allows the AP to perform the task more comfortably and effectively. This action helps prevent the AP from leaning over an elevated side rail, reducing the risk of injury to themselves or the client.
Choice B Reason:
Wearing clean gloves to perform mouth care for the client is a safety measure. Wearing gloves is crucial to maintain hygiene and prevent the transmission of microorganisms during mouth care.
Choice C Reason:
Using an oral care sponge swab moistened with cool water to clean the client's mouth is a safety measure. Using a moistened oral care sponge swab is a suitable method for providing mouth care to an unconscious client, helping to keep the mouth clean and moist.
Choice D Reason:
Using two gloved fingers to open the client's mouth for cleaning is NOT a safety measure. In this situation, using fingers to open the client's mouth poses a risk of injury or discomfort to the client. It's important to handle an unconscious patient's mouth with care and avoid using fingers to open the mouth forcibly.
A nurse is caring for a client who has chronic constipation. Which of the following actions should the nurse recommend to the client?
Explanation
Choice A Reason:
Consuming probiotic sources is recommendable. Probiotics are beneficial bacteria that can promote gut health. Including probiotic sources in the diet, such as yogurt with live cultures or other fermented foods, can help maintain a healthy balance of gut bacteria and alleviate constipation.
Choice B Reason:
Using a laxative every day is not recommendable. Regular use of laxatives is generally not recommended for chronic constipation, as it can lead to dependence and may not address the underlying causes.
Choice C Reason:
Baking with white flour is not recommendable. Consuming refined white flour may not contribute significantly to relieving constipation. Whole grains, high-fiber foods, and adequate fluid intake are more beneficial.
Choice D Reason:
Taking a calcium supplement is not recommendable. While calcium is important for overall health, taking a calcium supplement is not typically recommended as the primary intervention for chronic constipation. Dietary and lifestyle measures, such as increasing fiber intake and staying hydrated, are more commonly recommended.
A nurse is preparing to set up a sterile field to change a sterile dressing on a client's abdominal wound. Identify the sequence of steps the nurse should take. (Move the steps into the box on the right, placing them in the order of performance. Use all the steps.)
Explanation
Choice E Reason:
Preparing a dry work surface above the waist level. It's crucial to start by selecting and preparing an appropriate area for setting up the sterile field. This surface needs to be clean, dry, and above the waist level to maintain sterility and prevent contamination.
Choice C Reason:
Opening the outside cover of the sterile kit and remove the dust cover. This step involves opening the sterile kit without touching the inside contents to maintain sterility. Removing the outer cover exposes the sterile packaging and prepares for further steps.
Choice D Reason:
Grasping the outermost flap of the sterile kit while opening away from the body. By carefully opening the outermost flap, the nurse ensures that the sterile contents remain protected. Opening away from the body helps prevent accidental contamination from clothing or movements.
Choice B Reason:
Opening each side flap of the sterile kit individually while pulling to the side. Sequentially opening the side flaps maintains the sterile field and allows access to the inner contents without compromising sterility.
Choice A Reason:
Opening the innermost lower flap of the sterile kit while standing away from the sterile field. This final step involves accessing the innermost contents of the sterile kit while maintaining a safe distance to avoid accidental contamination. It ensures the contents within the sterile field remain protected until needed for the dressing change.
A nurse is caring for a client who fell while walking to the bathroom. Which of the following actions should the nurse take when completing the incident report?
Explanation
Choice A Reason:
Using direct quotes made by the client to describe the incident is inappropriate action.
Using direct quotes from the client might introduce subjectivity or personal bias into the incident report. It's important to maintain objectivity and describe the incident based on factual observations.
Choice B Reason:
Making a notation in the client's medical record that an incident report was completed is appropriate action. This action ensures that there is documentation within the client's medical record indicating that an incident report was filed. However, incident reports themselves are typically kept separate from the medical record to maintain confidentiality and prevent potential legal ramifications.
Choice C Reason:
Drawing a conclusion regarding the cause of the incident is inappropriate action. While it's important to document factual details, drawing conclusions about the cause of the incident in the report might be premature or speculative. Incident reports should focus on describing the event itself without making assumptions or conclusions about causation.
Choice D Reason:
Placing a copy of the incident report in the client's medical record is inappropriate action. As mentioned earlier, incident reports are usually kept separate from the medical record to maintain confidentiality and to ensure that they are used internally for quality improvement and risk management purposes rather than becoming part of the client's permanent medical record.
A nurse at a long-term care facility is reinforcing teaching with a newly licensed nurse about incident reporting. The nurse should identify that it is necessary to complete an incident report for which of the following situations?
Explanation
A. A family member is napping in the client's room.
This situation, while not ideal, doesn't involve harm or potential harm to a client, staff, or visitor. It may be addressed through communication and policy reminders but may not require an incident report.
B. A client refuses to eat at mealtime.
Client refusal to eat, while concerning, is not an unexpected or unusual event. It is a common aspect of care, and incident reports are not typically used for such situations.
C. A client's bed alarm is malfunctioning.
This situation involves a malfunction in equipment designed to ensure client safety. It has the potential to compromise the safety of the client and may require an incident report to document the issue and address it appropriately.
D. An assistive personnel is late for the upcoming shift.
Lateness may be an issue that needs addressing, but it's not typically considered an incident requiring a formal incident report. This situation may be addressed through workplace policies and communication.
A nurse is caring for a client who is terminally ill and has a do-not-resuscitate order on his medical record. The client asks, "What should I do if I have difficulty breathing?" Which of the following responses should the nurse make?
Explanation
Choice A Reason:
"Call me so that I can help you change your position." This response offers practical assistance and comfort to the client. Repositioning can sometimes alleviate discomfort associated with breathing difficulties, and the nurse can offer guidance or physical help to adjust the client's position for improved comfort.
Choice B Reason:
"Try to close your eyes and get some sleep." This response doesn't directly address the client's immediate concern about difficulty breathing and may not offer practical help.
Choice C Reason:
"It is common for breathing to become more difficult as time goes on." While this statement acknowledges the situation, it might not provide the client with actionable guidance or support on how to manage the difficulty in breathing.
Choice D Reason:
"Therapy choices are limited for clients who do not want resuscitation." This response might be interpreted as dismissive or unrelated to the client's immediate needs, focusing more on the DNR order rather than addressing the current concern about breathing difficulties.
A nurse on a medical-surgical unit is caring for a postoperative client who reports difficulty sleeping due to noise. Which of the following interventions is appropriate for the nurse to implement?
Explanation
Choice A Reason:
Avoid entering the client's room unless requested during the night is inappropriate. While minimizing entries can reduce disruptions, it's important for the nurse to perform necessary checks and care interventions. Avoiding the room completely might compromise the client's safety or care.
Choice B Reason:
Turn off alarms on bedside monitoring equipment is inappropriate. Disabling alarms can jeopardize patient safety as these alarms often indicate critical changes in the client's condition. Adjusting alarm settings or investigating if noise levels can be reduced without compromising safety would be more appropriate.
Choice C Reason:
Conduct staff communications away from the client's room is appropriate. This intervention helps minimize noise levels near the client's room, creating a quieter environment conducive to sleep. Staff conducting communications away from the room reduces unnecessary disturbances that might affect the client's rest.
Choice D Reason:
Turn on the client's TV to distract from hallway noise is inappropriate. Introducing more noise, such as from a TV, might not effectively address the issue of sleep disturbance due to external noise. Additionally, it's essential to respect the client's preferences, and some may prefer a quiet environment for sleep rather than additional noise from a TV.
A nurse is reinforcing teaching with a client about using guided imagery to manage chronic pain. Which of the following statements by the client indicates an understanding of this technique?
Explanation
Choice A Reason:
"I'll listen to my favorite music to take my mind off the pain." This statement refers to distraction techniques, like listening to music, which can help manage pain but isn't specifically guided imagery.
Choice B Reason:
"I'll think about my grandfather's farm to reduce pain." This statement indicates an understanding of this technique. Guided imagery involves creating a detailed mental image or scenario that promotes relaxation and diminishes pain perception. In this case, the client visualizing a familiar, pleasant place like their grandfather's farm can be an effective form of guided imagery to alleviate pain by diverting attention and inducing relaxation.
Choice C Reason:
"I'll use focused breathing to control my pain." This statement does not indicate an understanding of this technique.
Focused breathing, while beneficial for relaxation and pain management, is a different technique from guided imagery.
Choice D Reason:
"I'll learn to notice the sensation of muscle tension." This statement refers to progressive muscle relaxation, a technique involving systematically tensing and relaxing muscle groups, which isn't guided imagery.
A nurse is caring for a client who is scheduled for a CT scan that requires contrast dye. Which of the following actions is the priority for the nurse to take?
Explanation
Choice A Reason:
Questioning the client about allergies before the procedure is appropriate. It is crucial to assess the client for any allergies, especially to contrast dye, before the procedure. Allergic reactions to contrast dye can range from mild to severe, and prompt identification of potential allergies is essential to prevent adverse reactions. If the client has a known allergy to the contrast dye, alternative imaging methods or pre-medication may be considered.
Choice B Reason:
Telling the client to increase fluid intake following the procedure is inappropriate. This instruction is relevant post-procedure for the elimination of the contrast dye from the body. However, it is not the priority at this moment, and the client's safety during the procedure takes precedence.
Choice C Reason:
Evaluating the client for claustrophobia is appropriate. Assessing for claustrophobia is important, especially if the CT scan involves an enclosed space. However, this assessment can typically be conducted in advance of the procedure during the pre-procedure preparations.
Choice D Reason:
Informing the client about the steps of the procedure is inappropriate. Providing information about the procedure is important for the client's understanding and cooperation. However, ensuring the client's safety during the procedure by assessing for potential allergies to the contrast dye comes first.
A nurse is reinforcing teaching with a group of newly licensed nurses regarding client confidentiality. In which of the following situations nurse disclose health information without the client's written consent?
Explanation
Choice A Reason:
To an insurance agency in regard to a life insurance policy . This situation is incorrect. Generally, disclosure of health information to an insurance agency requires the client's written consent.
Choice B Reason:
To a medical interpreter service on behalf of a client. This situation is correct. In healthcare settings, it is generally acceptable to share limited health information with a medical interpreter service to facilitate communication with the client, especially if the client has limited proficiency in the primary language spoken in the healthcare setting. The interpreter is bound by confidentiality rules similar to healthcare providers.
Choice C Reason:
To a family member when the client is not available. This situation is incorrect. Disclosing health information to a family member typically requires the client's consent unless there are specific circumstances, such as emergencies, where the healthcare provider may need to act in the best interest of the client.
Choice D Reason:
To an employer for a pre-employment screening. This situation is incorrect. Disclosing health information to an employer typically requires the client's written consent. Employment-related health information is usually protected by privacy laws.
Sign Up or Login to view all the 49 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

