ATI PN Medical Surgical Leadership
Total Questions : 51
Showing 25 questions, Sign in for moreA nurse is caring for several clients on a medical-surgical unit. Which of the following client care situations requires the nurse to complete an incident report?
Explanation
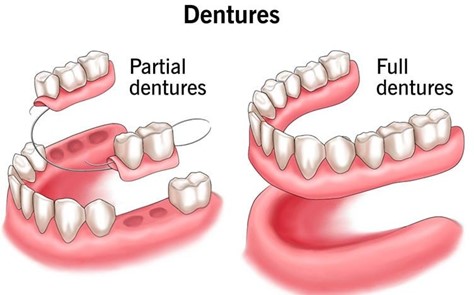
An incident report should be filed whenever an unexpected event occurs. The rule of thumb is that any time a patient makes a complaint, a medication error occurs, a medical device malfunctions, or anyone— patient, staff member, or visitor—is injured or involved in a situation with the potential for injury, an incident report is required ⁴. In this case, the client's missing dentures would be considered a complaint and would require the nurse to complete an incident report.
The other options do not require an incident report. Disagreeing with the nurse manager about inadequate staffing [a], a staff member not arriving at the facility to work an assigned shift [b], and discovering that the client does not have advanced directives [d] are not situations that would require an incident report according to the information provided in my sources.
The best source of information regarding the roles of the LPN in a med-surg setting is:
Explanation
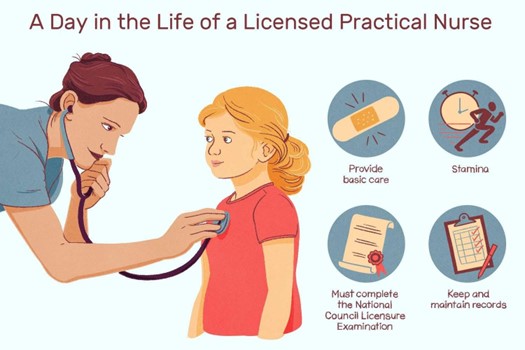
The State Board of Nursing is responsible for regulating the practice of nursing within a specific state. It establishes the scope of practice for LPNs and sets the standards for their education, licensure, and practice. Therefore, the State Board of Nursing would be the best source of information regarding the roles of an LPN in a med-surg setting.
The other options may provide some information about the roles of an LPN in a med-surg setting, but they are not the primary source. The facility Human Resources Department [a] may have information about job descriptions and responsibilities specific to that facility. Nursing textbooks [c] may provide general information about the roles of LPNs. Coworkers on your unit [d] may have personal experience and knowledge about the roles of LPNs in that specific unit, but their information may not be comprehensive or up-to-date.
Doing no harm is?
Explanation
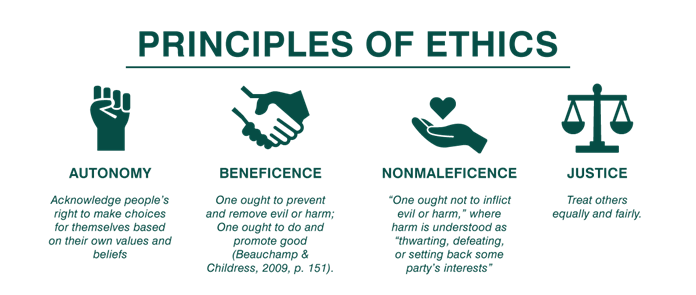
Nonmaleficence is the ethical principle of doing no harm. It requires healthcare providers to avoid causing harm to their patients and to take steps to prevent harm from occurring.
The other options are also important ethical principles in healthcare, but they do not specifically refer to doing no harm. Justice [a] refers to the fair distribution of benefits and burdens in society. Beneficence [c] refers to the obligation to do good and promote the well-being of others. Veracity [d] refers to the obligation, to tell the truth and not deceive others.
A nurse is assigning tasks for the upcoming shift. Which of the following tasks should the nurse delegate to assistive personnel (AP)? (Select all that apply.)
Explanation
The correct answers are Choices A, D, and E.
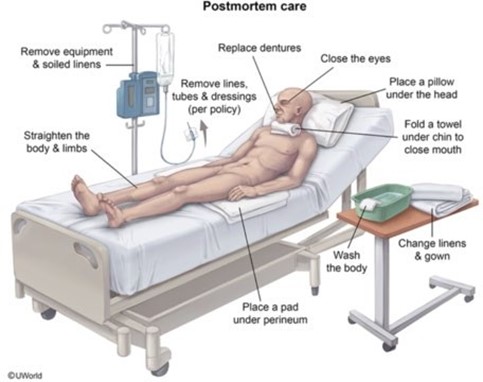
Choice A rationale:Providing postmortem care to a client who has just passed away is a task that can be delegated to assistive personnel (AP). Postmortem care involves cleaning and preparing the body after death and is not a task that requires the specialized skills or judgement of a nurse. It is important to note that while the physical task of postmortem care can be delegated, the nurse is still responsible for providing emotional support and information to the family, coordinating with the morgue or funeral home, and completing any required documentation.
Choice B rationale:Instructing a client about the use of a spirometer is not a task that should be delegated to assistive personnel. Patient education requires assessment and evaluation of the patient’s understanding, which are nursing responsibilities. A spirometer is a medical device used to measure lung function and is often used after surgery to help prevent complications like pneumonia. Proper use of the spirometer is crucial to its effectiveness, so it is important that the instruction is clear and understood by the patient.
Choice C rationale:Suctioning a client’s newly inserted tracheostomy is not a task that should be delegated to assistive personnel. Tracheostomy care, especially suctioning, requires specialized skills and knowledge, as well as the ability to assess the patient’s respiratory status. Improper suctioning can cause trauma to the trachea, hypoxia, or infection. Therefore, this task should be performed by a nurse or other licensed healthcare professional.
Choice D rationale:Transferring a client to radiology for x-rays is a task that can be delegated to assistive personnel. This task involves physical assistance and does not require specialized nursing skills or judgement. However, the nurse should provide the AP with any necessary information about the patient’s condition, mobility, and any precautions that need to be taken during the transfer.
Choice E rationale:Performing a simple dressing change on a client’s arm is a task that can be delegated to assistive personnel. This task involves changing the bandages on a wound, which is a task that does not require specialized nursing skills or judgement. However, the nurse should ensure that the AP has been properly trained in dressing changes, understands the importance of infection control, and knows when to report any changes in the wound’s appearance.
What is a nurse's best protection against negligence or malpractice?
Explanation
A nurse's best protection against negligence or malpractice is to follow the standards of practice. These standards define the acceptable level of care that a nurse is expected to provide and are based on current evidence and professional consensus. By adhering to these standards, a nurse can demonstrate that they have provided care that meets the expected level of quality and safety.
The other options are not the best protection against negligence or malpractice. Asking permission from the managing nurse prior to performing any duties [a] may be helpful in some situations, but it is not a guarantee against negligence or malpractice. Never being alone with a patient [c] is not practical or necessary for providing safe and effective care. Recording patient interactions with your phone [d] may violate patient privacy and is not an effective way to prevent negligence or malpractice.
A nurse is delegating tasks to an assistive personnel (AP). Which of the following tasks should the nurse assign to the AP?
Explanation
Assistive personnel (AP), also known as unlicensed assistive personnel (UAP), can perform tasks such as recording vital signs ¹. Obtaining vital signs on clients who are stable [d] is a task that can be delegated to an AP.
The other options are not tasks that should be delegated to an AP. Assisting the client to select a low-residue diet [a] and reviewing the steps of self-blood glucose monitoring with a client [c] involves patient education and dietary planning, which are typically the responsibility of a licensed nurse. Performing a complex dressing change [b] is a complex task that requires specialized knowledge and skills.
A nurse observes two assistive personnel (AP) arguing over who should go on break first. The nurse interrupts the conversation and states that one AP can take a break now, but the other AP will get to take an early lunch. Which of the following types of conflict management is the nurse demonstrating?
Explanation
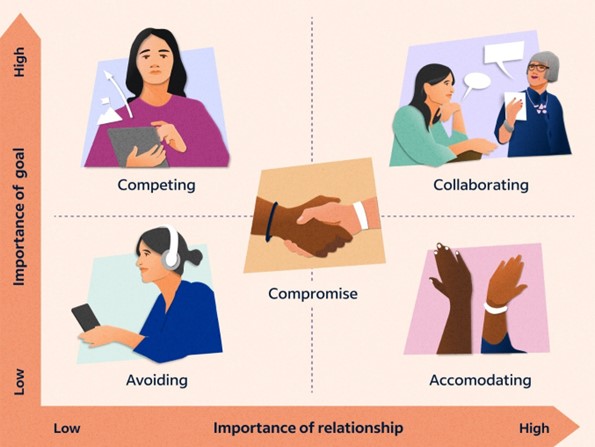
In this situation, the nurse is demonstrating the compromising style of conflict management. Compromising involves finding a middle ground where both parties give up something in order to reach a mutually acceptable solution. In this case, the nurse suggests that one AP can take a break now, but the other AP will get to take an early lunch. This solution allows both APs to have some of their needs met while also making concessions.
The other options are not the type of conflict management demonstrated by the nurse in this situation. Cooperating [a] involves one party giving in to the demands of the other party in order to maintain harmony. Competing [c] involves one party trying to win at the expense of the other party. Avoiding [d] involves avoiding or withdrawing from the conflict altogether.
A nurse requests that an assistive personnel (AP) change all the linens and give bed baths to four clients on the unit. The previous day, the AP was not able to complete these same tasks. Which of the following actions should the nurse take in addressing this situation?
Explanation
The correct answer is Choice C.
Choice A rationale: Offering to help the AP complete the tasks may seem like a good solution in the short term. However, this approach does not address the underlying issue, which is that the AP was not able to complete these tasks the previous day. The nurse’s role is to delegate tasks appropriately and ensure that all tasks are completed in a timely manner. If the nurse takes over the AP’s tasks, it could lead to an imbalance in the workload and could potentially overburden the nurse. Therefore, while this choice may seem helpful, it is not the most effective solution to the problem.
Choice B rationale: Assigning a more qualified staff member to the tasks could be a potential solution if the AP’s inability to complete the tasks was due to a lack of skills or knowledge. However, without more information, it’s not clear that this is the case. Furthermore, this approach could lead to resentment among staff if it appears that tasks are not being distributed fairly. Therefore, while this choice could be a potential solution, it is not the most effective solution given the information provided.
Choice C rationale: Planning a more reasonable job assignment is the most effective solution to this problem. If the AP was not able to complete the tasks the previous day, it suggests that the workload was too heavy or the tasks were too complex. By reassessing the job assignment and making it more manageable, the nurse can ensure that all tasks are completed in a timely manner. This approach respects the abilities and limitations of the AP, promotes a fair distribution of tasks, and ensures the best care for the clients.
Choice D rationale: Setting a time frame for the AP to complete the tasks could be a potential solution if the issue was that the tasks were not completed in a timely manner. However, if the AP was not able to complete the tasks at all, simply setting a time frame may not resolve the issue. This approach could also add unnecessary pressure on the AP, which could lead to rushed or substandard work. Therefore, while this choice could be a potential solution, it is not the most effective solution given the information provided.
A nurse is receiving a change-of-shift report for four clients. Which of the following findings should the nurse identify as the priority?
Explanation
The correct answer is Choice C.
Choice A rationale: A client who had a blood transfusion and has a blood pressure of 138/76 mm Hg. This client is stable. The blood pressure is within normal range, indicating that the client is not experiencing a transfusion reaction, which could cause hypotension. Therefore, this client is not the highest priority.
Choice B rationale: A client who has skeletal traction for a femur fracture and reports incisional discomfort of 4 on a scale of 0 to 10. While pain management is an important aspect of client care, a pain level of 4 indicates that the client’s pain is manageable. Therefore, this client is not the highest priority.
Choice C rationale: A client who is 4 hours postoperative following a total hip arthroplasty and has a urinary output of 15 mL/hr. This client is showing signs of oliguria, which could indicate a serious complication such as hypovolemia or acute kidney injury. This client is the highest priority because these complications can lead to further serious issues such as shock or end-organ damage if not addressed promptly.
A nurse is delegating client care assignments for the upcoming shift. Which of the following tasks should the nurse plan to delegate to the assistive personnel (AP)?
Explanation
Assistive personnel (AP), also known as unlicensed assistive personnel (UAP), can perform tasks such as recording vital signs ¹. Collecting intake and output [a] is a task that can be delegated to an AP.
The other options are not tasks that should be delegated to an AP.
Evaluating pain relief after administering pain medication [b] involves assessing the effectiveness of a medical intervention, which is typically the responsibility of a licensed nurse.
Providing a central line dressing change [c] is a complex task that requires specialized knowledge and skills.
Selecting a menu for a low-sodium diet [d] involves dietary planning, which is typically the responsibility of a licensed nurse or a registered dietitian.
A nurse is caring for a group of clients on a medical-surgical unit. Which of the following actions jeopardize client confidentiality? (Select all that apply.)
Explanation
Discussing clients at the table in the cafeteria [b], disposing of written report sheets into the facility trash receptacle [c], and sharing a personal password with a coworker [e] are all actions that jeopardize client confidentiality. Client information should be kept private and secure at all times. Discussing clients in public places or disposing of client information in an unsecured manner can result in unauthorized access to confidential information. Sharing personal passwords can also compromise the security of client information.
The other options do not jeopardize client confidentiality. Removing client information from fax machines immediately [a] helps to prevent unauthorized access to confidential information. Giving verbal reports at change of shift in a designated conference room [d] is a standard practice that allows for the secure transfer of client information between healthcare providers.
A nurse is reinforcing teaching with a client about advance directives. Which of the following topics should the nurse include? (Select all that apply.)
Explanation
When reinforcing teaching with a client about advance directives, the nurse should include topics such as organ donation [a], disclosure of personal health care information [b], durable power of attorney for health care [c], and cardiopulmonary resuscitation [e]. Advance directives are legal documents that allow individuals to communicate their wishes about medical treatment and end-of-life care in the event that they are unable to make decisions for themselves. These topics are all important components of advance directives and should be discussed with the client.
Enteral feeding tubes [d] are not a topic that is typically included in discussions about advance directives. While enteral feeding may be a component of end-of-life care, it is not a specific topic that is addressed in advance directives.
A charge nurse overhears a provider speaking to a staff nurse in anger concerning incorrect supplies that are available. Which of the following actions by the charge nurse displays conflict resolution?
Explanation
Addressing the situation as soon as possible [a] and assisting the provider in identifying alternative solutions [d] are actions that display conflict resolution. Conflict resolution involves finding a peaceful and mutually acceptable solution to a disagreement or dispute. By addressing the situation promptly and helping the provider to identify alternative solutions, the charge nurse can facilitate communication and collaboration between the provider and the staff nurse and help to resolve the conflict.
The other options do not display conflict resolution. Using aggressive communication skills [b] can escalate the conflict and make it more difficult to find a resolution. Fostering closed communication [c] can also hinder the resolution of the conflict by preventing open and honest dialogue between the parties involved.
A nurse on a pediatric unit is working with an assistive personnel (AP). Which of the following tasks should the nurse have the AP perform first?
Explanation
The nurse should have the AP perform the task of feeding a school-age client who has burns on both upper extremities first. This task is a high priority because it addresses the client's immediate need for nutrition and hydration. The client's burns may make it difficult for them to feed themselves, so the assistance of the AP is necessary to ensure that the client receives adequate nourishment.
The other tasks are also important, but they are not the highest priority in this situation. Collecting a stool sample for ova and parasites from a toddler [b] and bathing an adolescent client who is disabled [c] are routine tasks that can be performed as time permits. Ambulating a preschooler who is postoperative to the playroom [d] is also important for promoting mobility and recovery, but it is not as urgent as addressing the immediate need for nutrition and hydration.
A nurse is planning an in-service that encourages active member participation and feedback about decreasing nosocomial infections on the unit. Which of the following leadership styles does the nurse plan to use?
Explanation
The nurse is planning to use a democratic leadership style when conducting an in-service that encourages active member participation and feedback about decreasing nosocomial infections on the unit. A democratic leader values the input and opinions of team members and encourages participation and collaboration in decision-making. By encouraging active participation and feedback from team members, the nurse is demonstrating a democratic approach to leadership.
The other options are not the leadership style that the nurse plans to use in this situation. A laissez-faire leader [b] takes a hands-on approach and allows team members to make their own decisions without providing guidance or direction. An autocratic leader [c] makes decisions unilaterally without seeking input or feedback from team members. An open-door leader [d] maintains an open-door policy and is accessible to team members, but this does not necessarily involve active participation and feedback from team members.

A nurse is assigning care to an assistive personnel (AP). Which of the following tasks should the nurse delegate to the AP?
Explanation
Assistive personnel (AP), also known as unlicensed assistive personnel (UAP), can perform tasks such as assisting with activities of daily living, hygiene, and nutrition, as well as those tasks that support professional nursing assessments ². Providing postmortem care for a client who has died [d] is a task that can be delegated to an AP.
The other options are not tasks that should be delegated to an AP. Educating a client on the use of a blood glucose monitor [a] involves patient education, which is typically the responsibility of a licensed nurse.
Interpreting a client's vital signs [b] involves assessing the client's health status, which is also typically the responsibility of a licensed nurse. Performing a central line dressing change for a client [c] is a complex task that requires specialized knowledge and skills.
A nurse is working with two assistive personnel (AP). The nurse notes that one of the APs has been taking long breaks and making personal phone calls. Which of the following statements should the nurse make to resolve this conflict?
Explanation
The nurse should make the statement "I need to talk to you about unit expectations regarding timely completion of tasks" to resolve the conflict with the AP who has been taking long breaks and making personal phone calls. This statement is assertive and focuses on the issue at hand without blaming or attacking the AP. It also opens up a dialogue between the nurse and the AP to discuss the issue and find a resolution.
The other statements are not effective in resolving the conflict. Statements such as "Several staff members have commented that you don't do your fair share of the work" [a] and "You have been very inconsiderate of others by not completing your share of the work" [b] are accusatory and may make the AP defensive.
Threatening to inform the nurse manager [c] may also escalate the conflict and is not a constructive way to address the issue.
A nurse is caring for a client who has dementia and is scheduled for a procedure. Which of the following individuals should the nurse request to sign the client's informed consent?
Explanation
The nurse should request the client's son, who has a durable power of attorney, to sign the client's informed consent. A durable power of attorney is a legal document that allows an individual to appoint someone to make decisions on their behalf in the event that they become unable to do so. If the client has dementia and is unable to provide informed consent for the procedure, the individual with a durable power of attorney has the legal authority to make decisions on their behalf.
The other individuals are not the appropriate person to sign the client's informed consent. The client's sister [b] and daughter [c] may be involved in the client's care and decision-making, but they do not have the legal authority to provide informed consent on behalf of the client unless they have been designated as such in a legal document. Advance directives [d] are legal documents that allow individuals to communicate their wishes about medical treatment and end-of-life care, but they do not grant decision-making authority to another individual.
A nurse observes an unknown man in a laboratory coat making copies of a client's medical record. Which of the following actions should the nurse take?
Explanation
The nurse should approach the man and ask why he is making copies of the client's medical records. This action allows the nurse to directly address the situation and gather more information before taking further steps.
Option A, may not be the best initial action because it does not directly address the situation.
Option B may be premature without first gathering more information.
Option C, may also not be the best initial action because it does not directly address the situation.
A nurse enters a client's room and finds the client on the floor. Which of the following actions should the nurse take first?
Explanation
The first action the nurse should take is to collect data on the client. This includes assessing the client's condition and vital signs to determine if they require immediate medical attention.
Option b may not be appropriate without first assessing the client's condition.
Option c may be necessary after collecting data on the client, but it should not be the first action taken.
Option d may also be necessary, but it should not be the first action taken.
Essential elements of effective delegation by an LPN include: (SELECT ALL THAT APPLY)
Explanation
Effective delegation by an LPN includes compliance with state and institutional policies, evaluation of the patient's response to care, knowledge of each patient's condition, and determination of tasks that can be safely delegated.
Option Bmay not always be necessary as direct supervision may not always be required for all tasks assigned to others.
Mr. Smith did not receive his medication on time, as ordered, because his nurse forgot about it and went on her lunch break. Consequently, Mr. Smith's condition deteriorated, and he was sent to the emergency room. What legal term describes this form of professional negligence?
Explanation
In this situation, the nurse's failure to administer Mr. Smith's medication on time as ordered, resulting in harm to the patient, could be considered malpractice. Malpractice refers to a failure to meet the standard of care that results in harm to a patient.
Option A refers to legal responsibility for one's actions, but it does not specify the type of wrongdoing.
Option B refers to wrongdoing or misconduct, but it is not specific to the medical profession.
Option D refers to a failure to fulfill one's duties or obligations, but it does not necessarily imply harm to a patient.
A nurse is working with an assistive personnel (AP) who refuses a client assignment. When resolving this conflict, which of the following comments is appropriate for the nurse to make?
Explanation
When resolving a conflict with an assistive personnel (AP) who refuses a client assignment, it would be appropriate for the nurse to say "I need to talk to you about the unit policies regarding client assignments." This comment addresses the issue directly and professionally and provides an opportunity for the nurse to clarify the unit policies and expectations.
Option A is accusatory and unprofessional.
Option B may be necessary at some point, but it should not be the first response.
Option C is also accusatory and unprofessional.
A nurse is preparing to obtain consent from a client who has a tibia fracture. The client received IV morphine sulfate prior to arrival on the unit and is scheduled for surgery. Which of the following actions should the nurse take?
Explanation
If a client has received IV morphine sulfate prior to arrival on the unit and is scheduled for surgery, the nurse should delay the procedure. This is because the client may not be able to give informed consent due to the effects of the medication.
Option A may not be appropriate if the client is not able to give informed consent.
Option B is not appropriate as it is not within the nurse's scope of practice to sign consent on behalf of a client.
Option C may be necessary if the client is unable to give informed consent and a relative is available to provide consent.

When preparing to administer medications, the nurse carefully confirms the drug order and the patient's identity. This adherence to an essential ethical principle is:
Explanation
When preparing to administer medications, the nurse carefully confirms the drug order and the patient's identity. This adherence to an essential ethical principle is Non-maleficence. Non-maleficencerefers to the principle of "do no harm" and requires healthcare providers to avoid causing harm to their patients.
Option A refers to wrongdoing or misconduct and is not applicable in this situation.
Option C refers to truthfulness and honesty, but it is not the primary principle being demonstrated in this situation.
Option D refers to fairness and equality, but it is not the primary principle being demonstrated in this situation.
Sign Up or Login to view all the 51 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

