ATI RN Custom MS2 Quiz 2 Fall 2023 HR MED SURG Cardiovascular
Total Questions : 25
Showing 25 questions, Sign in for moreA nurse is teaching a client with angina pectoris about starting therapy with nitroglycerin tablets. The nurse should include which of the following instructions regarding how to take the medication?
Explanation
Choice A rationale: Nitroglycerin tablets are typically taken sublingually (under the tongue) at the onset of chest pain. If the pain is not relieved, a second tablet may be taken 5 minutes after the first. If the pain continues for another 5 minutes, a third tablet may be used123.
Choice B rationale: Nitroglycerin tablets are not typically taken with water. They are designed to dissolve under the tongue for quick absorption into the bloodstream1.
Choice C rationale: Nitroglycerin is not typically taken after each meal and at bedtime. It is used as needed to relieve chest pain1.
Choice D rationale: While nitroglycerin can be taken every 5 minutes up to three times during an acute angina attack, it is not typically recommended to take one tablet every 10 minutes1.
So, the correct answer is A, after analysing all choices.
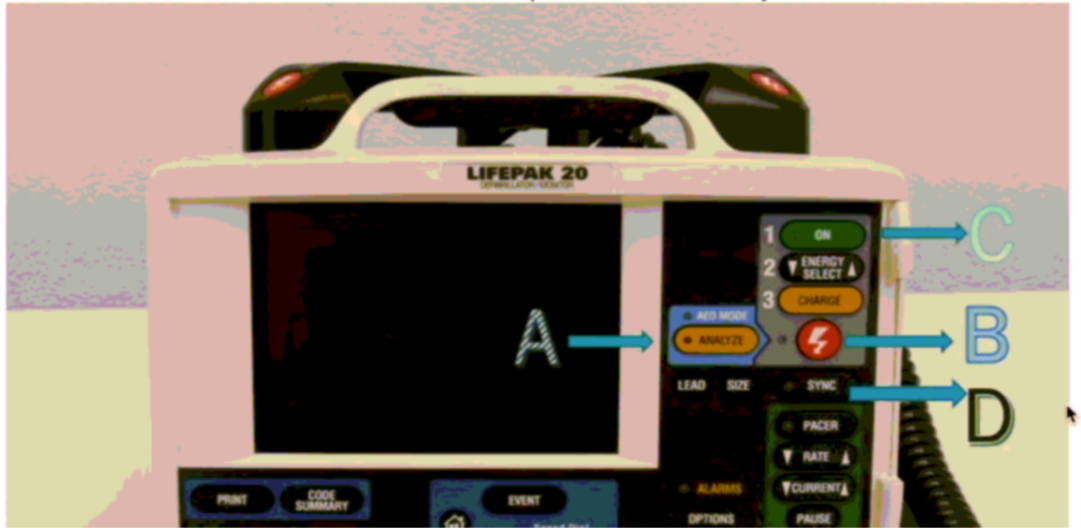
The nurse notes a client in supraventricular tachycardia. The patient has a pulse and the cardiac monitor is at the bedside. The nurse understands electrical intervention is indicated. What button does the nurse push to ensure the electricity is delivered on the R wave? Refer to the picture.
Explanation
Choice A rationale: The “ANALYZE” button is typically used to allow the defibrillator to analyze the heart rhythm. It would not ensure that the electricity is delivered on the R wave6.
Choice B rationale: The “SHOCK” button is used to deliver a shock during defibrillation or cardioversion. However, it does not specifically ensure that the shock is delivered on the R wave6.
Choice C rationale: The “ON” button is typically used to turn the device on or off. It does not control the timing of the electrical delivery6.
Choice D rationale: The “SYNC” button is used in synchronized cardioversion to match the delivery of the shock to the R wave of the ECG, which is the peak of the electrical wave during which the ventricular cells are depolarized6.
So, the correct answer is D, after analysing all choices.
A nurse is caring for a client that is post cardiopulmonary arrest. The nurse anticipates to administer which of the following medications if the client's restored rhythm is symptomatic bradycardia?
Explanation
Choice A rationale: Epinephrine is a potent vasoconstrictor and is typically used in emergency situations such as cardiac arrest. It is not the first-line treatment for symptomatic bradycardia1.
Choice B rationale: Atropine is the first-line medication for the treatment of bradycardia. It increases the heart rate by blocking the effects of the vagus nerve on the heart1.
Choice C rationale: Adenosine is primarily used to treat supraventricular tachycardia, not bradycardia1.
Choice D rationale: Verapamil is a calcium channel blocker used to treat high blood pressure, angina, and certain heart rhythm disorders, not typically used for bradycardia1.
A nurse is caring for a client who has a serum potassium level of 5.9 mEq/L. The provider prescribes polystyrene sulfonate. If this medication is effective, the nurse should expect which of the following changes on the client's ECG?
Explanation
Choice A rationale: Prolonged PR intervals are not typically associated with the use of polystyrene sulfonate2.
Choice B rationale: Widening of the QRS complex is not typically seen with the use of polystyrene sulfonate2.
Choice C rationale: Polystyrene sulfonate is used to treat hyperkalemia (high potassium levels). As potassium levels decrease, the peaked T wave seen in hyperkalemia may reduce234.
Choice D rationale: An increase in T wave amplitude is not typically associated with the use of polystyrene sulfonate2.
A client with a complaint of dehydration has been admitted into the medical floor. Sodium chloride 1000ml IV to infuse over 12 hrs has been ordered by the admitting Physician. How many ml/hr should you administer? (Round to the nearest whole number) ml/hr
Explanation
Step 1 is to use the formula for calculating the IV infusion rate: Infusion Rate (mL/hour) = Volume to be Infused (mL) ÷ Time for Infusion (hours)5.
So, Infusion Rate = 1000 mL ÷ 12 hours = 83.33 mL/hr.
Rounding to the nearest whole number gives 83 mL/hr.
So, the correct answer is 83 mL/hr, after calculating.
A client has with Angina has been ordered to take sublingual NTG tablets. Which of the following instructions should the nurse include?
Explanation
Choice A rationale: Nitroglycerin tablets are not typically taken with water. They are designed to dissolve under the tongue for quick absorption into the bloodstream6789.
Choice B rationale: It is not necessary to go to the hospital to take the medication. The medication can be taken at the onset of chest pain6789.
Choice C rationale: This is the correct instruction. At the onset of chest pain, the patient should lie or sit down and place one tablet under the tongue6789.
Choice D rationale: If one tablet does not relieve the pain in 5 minutes, a second tablet may be taken. If the pain continues for another 5 minutes, a third tablet may be used. If the patient still has chest pain after a total of 3 tablets, they should seek immediate medical attention6789.
So, the correct answer is C, after analysing all choices
A client has developed atrial fibrillation with a ventricular rate of 148 beats per minute. Which assessment findings does the nurse expect to find in this client? Select all that apply
(Select All that Apply.)
Explanation
Choice A rationale: Shortness of breath is a common symptom in atrial fibrillation due to the heart’s inability to pump blood effectively12.
Choice B rationale: Hypotension can occur in atrial fibrillation due to decreased cardiac output12.
Choice C rationale: Hypertension is not typically a direct result of atrial fibrillation. However, long-term untreated hypertension can be a cause of atrial fibrillation12.
Choice D rationale: Chest pain can occur in atrial fibrillation due to decreased blood flow to the heart12.
Choice E rationale: Dizziness is a common symptom in atrial fibrillation due to decreased blood flow to the brain12.
Choice F rationale: Bounding pulses are not typically associated with atrial fibrillation12.
A client on the cardiac telemetry unit goes into Ventricular fibrillation and is unresponsive. Following initiation of the emergency call system (code blue), what is the next priority for the nurse in caring for the client?
Explanation
Choice A rationale: While amiodarone is a medication used in the treatment of ventricular fibrillation, it is not the immediate priority in an unresponsive client34.
Choice B rationale: The immediate priority in a client who goes into ventricular fibrillation and is unresponsive is to prepare for defibrillation. This is a life-saving measure that can restore a normal heart rhythm34.
Choice C rationale: Synchronized cardioversion is not the immediate priority in a client who goes into ventricular fibrillation and is unresponsive34.
Choice D rationale: While epinephrine is a medication used in the treatment of ventricular fibrillation, it is not the immediate priority in an unresponsive client34.
So, the correct answer is B, after analysing all choices.
Which of the following medications does the nurse anticipate being ordered for a client admitted with the following tachycardic rhythm and complaints of palpitations and dizziness?
Explanation
Choice A rationale: Adenosine is primarily used to treat supraventricular tachycardia, not typically used for tachycardic rhythm with palpitations and dizziness5.
Choice B rationale: Atenolol is a beta-blocker that can be used to treat tachycardia, but it is not typically the first choice for acute symptoms5.
Choice C rationale: Metoprolol is a beta-blocker that is often used to treat tachycardia and can help alleviate symptoms such as palpitations and dizziness5.
Choice D rationale: Atropine is typically used to treat bradycardia, not tachycardia5.
So, the correct answer is C, after analysing all choices.
The charge nurse is making assignments for clients on a cardiac unit. Which client should the charge nurse assign to a new graduate nurse?
Explanation
Choice A rationale: A client newly diagnosed with myocardial infarction would require a nurse with more experience due to the complexity and potential instability of the condition678910.
Choice B rationale: A client complaining of crushing chest pain could be experiencing a serious condition such as a myocardial infarction. This client would require a nurse with more experience678910.
Choice C rationale: A client scheduled for a cardiac catheterization and requires patient teaching would be an appropriate assignment for a new graduate nurse. This client is stable and the task of patient teaching is within the scope of a new graduate678910.
Choice D rationale: A client admitted with unstable angina would require a nurse with more experience due to the potential for rapid changes in the client’s condition678910.
So, the correct answer is C, after analysing all choices.
A client comes to the emergency department with reports of three days of watery stools and emesis x 6 in the past hour. Upon assessment, the nurse notes vital signs are B/P 130/92 mmHg, heart rate 130 bpm, respiratory rate 18 bpm, and oxygen saturation of 98% in room air. The nurse puts the client on the cardiac monitor. What does the nurse anticipate will be the prescription by the medical provider?
Explanation
Choice A rationale: Heparin is an anticoagulant, not typically used to treat dehydration due to diarrhea and vomiting4.
Choice B rationale: Sodium Chloride IV bolus is often used to treat dehydration, which can be caused by three days of watery stools and emesis5.
Choice C rationale: Atenolol is a beta-blocker, used to manage heart conditions, not dehydration4.
Choice D rationale: Verapamil is a calcium channel blocker, not typically used to treat dehydration4.
So, the correct answer is Choice B, after analyzing all choices.
A patient on the telemetry unit develops atrial flutter with a heart rate of 150, respirations 26, b/p 118/64 and a o2 saturation of 90% while sitting down. Which action should the nurse do FIRST?
Explanation
Choice A rationale: Atropine is used to treat bradycardia, not atrial flutter6.
Choice B rationale: Reassessing the patient’s blood pressure is important, but not the first action when the patient has a low oxygen saturation7.
Choice C rationale: Adenosine is used to treat supraventricular tachycardia, not atrial flutter6.
Choice D rationale: Administering supplemental oxygen is the first action when a patient’s oxygen saturation is low7.
So, the correct answer is Choice D, after analyzing all choices.
A nurse is teaching a client with a new atrial fibrillation diagnosis on worsening signs and symptoms. The nurse should instruct the client to monitor for which of the following complications?
Explanation
Choice A rationale: An oxygen saturation reading of 99% on room air is normal8.
Choice B rationale: Slurred speech could indicate a stroke, which is a potential complication of atrial fibrillation due to the risk of clot formation8.
Choice C rationale: A decrease in intensity of chest pain is not typically a sign of worsening atrial fibrillation8.
Choice D rationale: While elevated blood pressure can be associated with atrial fibrillation, it is not a specific sign of worsening atrial fibrillation8.
So, the correct answer is Choice B, after analyzing all choices.
The nurse on the unit hears an alarm sound in the client's room. Arriving in the room, the client is unresponsive. pulseless and the nurse sees the flat rhythm on the monitor. What is the FIRST action by the nurse?
Explanation
Choice A rationale: Atropine is not typically used in the treatment of cardiac arrest91011.
Choice B rationale: Defibrillation is not the first step in the treatment of cardiac arrest. The first step is to start CPR91011.
Choice C rationale: Starting CPR is the first action when a patient is unresponsive and pulseless91011.
Choice D rationale: While epinephrine is used in the treatment of cardiac arrest, it is not the first step. The first step is to start CPR91011.
So, the correct answer is Choice C, after analyzing all choices.
A client with Sinus tachycardia has been admitted into the telemetry unit. The nurse identifies the following as possible causes of sinus tachycardia. Select all that apply (SATA)
(Select All that Apply.)
Explanation
Choice A rationale: Fever can cause an increase in metabolic rate which can lead to sinus tachycardia1.
Choice B rationale: Lisinopril is an ACE inhibitor used to treat hypertension, not a cause of sinus tachycardia1.
Choice C rationale: Albuterol is a bronchodilator that can cause sinus tachycardia as a side effect1.
Choice D rationale: Sleeping typically results in a slower heart rate, not sinus tachycardia1.
Choice E rationale: Dehydration can lead to low blood volume, causing the heart to beat faster to maintain blood pressure, resulting in sinus tachycardia1.
So, the correct answer is Choices A, C, and E, after analysing all choices.
A nurse is caring for a client who has developed a thrombus and is receiving heparin by continuous N infusion. The client asks the nurse how long will it take for the heparin to dissolve the clot. Which of the following responses should the nurse give?
Explanation
Choice A rationale: Heparin is an anticoagulant that prevents new clots from forming but does not dissolve existing clots23.
Choice B rationale: Heparin does not directly dissolve clots23.
Choice C rationale: While a pharmacist can provide medication information, it is incorrect to say they would be a better fit to answer this question as nurses are trained in medication education23.
Choice D rationale: While it’s true that it takes time for heparin to reach a therapeutic blood level, this statement could be misleading because heparin does not dissolve clots23.
So, the correct answer is Choice A, after analysing all choices.
A nurse is reviewing the EKG strip of a client who is hypotensive and is complaining of leg cramping. Which of the following abnormalities on the client's EKG should the nurse interpret as a sign of hypokalemia?
Explanation
Choice A rationale: An elevated ST segment is not typically associated with hypokalemia45.
Choice B rationale: A widened QRS complex is not a typical finding in hypokalemia45.
Choice C rationale: An inverted P wave is not a typical sign of hypokalemia45.
Choice D rationale: An abnormally prominent U wave is a common EKG finding in hypokalemia45.
So, the correct answer is Choice D, after analysing all choices.
Which action by the nurse will determine if therapies ordered for a patient with chronic constrictive pericarditis are effective?
Explanation
Choice A rationale: While changes in the ECG can indicate various heart conditions, they are not specific to the effectiveness of therapies for chronic constrictive pericarditis67.
Choice B rationale: Jugular venous distention is a common sign of chronic constrictive pericarditis, and its absence can indicate effective treatment67.
Choice C rationale: Changes in the sedimentation rate are not specific indicators of the effectiveness of therapies for chronic constrictive pericarditis67.
Choice D rationale: The presence of a paradoxical pulse is not a specific indicator of the effectiveness of therapies for chronic constrictive pericarditis67.
So, the correct answer is Choice B, after analyzing all choices.
A client is experiencing atrial fibrillation for 2 weeks and did not respond to medication therapy. The client is scheduled for an elective (outpatient) cardioversion. Which other procedure or test does the nurse anticipate this client will need?
Explanation
Choice A rationale: While a chest x-ray can provide useful information about the heart and lungs, it is not typically required before an elective cardioversion89.
Choice B rationale: A transesophageal echocardiogram is often performed before cardioversion to check for the presence of any clots in the heart891011.
Choice C rationale: An exercise stress test is not typically required before an elective cardioversion89.
Choice D rationale: A central line placement for thrombolytic medication administration is not typically required before an elective cardioversion89.
So, the correct answer is Choice B, after analyzing all choices.
A nurse in an urgent care center is assessing a client who reports a sudden onset of irregular palpitations, fatigue, and dizziness. The nurse finds a rapid and irregular heart rate on the cardiac monitor. Which dysrhythmias should the nurse expect to find on the EKG?
Explanation
Choice A rationale: First-degree AV block is a type of heart block, not a dysrhythmia associated with palpitations, fatigue, and dizziness12.
Choice B rationale: Sinus bradycardia is a slow heart rate, not a rapid and irregular one12.
Choice C rationale: Sinus tachycardia is a fast heart rate but it is regular, not irregular12.
Choice D rationale: Atrial fibrillation is a fast and irregular heart rate, which aligns with the symptoms described34.
So, the correct answer is Choice D, after analysing all choices.
As the registered nurse, which tasks below should you NOT delegate to the LPN?
Explanation
Choice A rationale: LPNs can reinforce education provided by RNs56.
Choice B rationale: LPNs can administer medications that are not high-risk56.
Choice C rationale: LPNs can obtain vital signs on stable patients56.
Choice D rationale: Starting a blood transfusion is a task that requires specific nursing judgment and decision-making skills, which should not be delegated to an LPN56.
So, the correct answer is Choice D, after analyzing all choices.
A nurse is educating a patient with a newly placed pacemaker about a variety of complementary and alternative therapies. What type of therapy is contraindicated in patients with pacemakers?.
Explanation
Choice A rationale: Imagery therapy is a mind-body intervention that does not interfere with pacemakers9.
Choice B rationale: Magnetic therapy can interfere with the functioning of pacemakers910.
Choice C rationale: Relaxation therapy is a mind-body intervention that does not interfere with pacemakers9.
Choice D rationale: Yoga therapy is a physical intervention that does not interfere with pacemakers9. So, the correct answer is Choice B, after analyzing all choices.
Read orders by the prescriber and answer the question.
Prescriber's orders
Labs: PT, PTT, INR
Unsupervised ambulation every 1 hr
Give protamine sulfate STAT
Give Aspirin orally daily
Continue unrestricted regular diet
Give vitamin K STAT
Initiate bleeding precautions
A nurse is admitting a client who has been in Atrial Fibrillation for 24 hours.
Which of the following interventions does the nurse plan to complete?
(Select All that Apply.)
Explanation
Choice A rationale: Vitamin K is given to counteract the effects of anticoagulants like warfarin, which might have been administered to manage atrial fibrillation1.
Choice B rationale: Heparin is an anticoagulant often used in the initial management of atrial fibrillation to prevent the formation of clots2.
Choice C rationale: PT, PTT, and INR are lab tests used to monitor the effectiveness of anticoagulation therapy1.
Choice D rationale: Coumadin (warfarin) is a long-term anticoagulant therapy often used in the management of atrial fibrillation1.
Choice E rationale: Verapamil is a calcium channel blocker, not typically the first line of treatment for atrial fibrillation3.
So, the correct answer is Choices A, B, C, and D, after analyzing all choices.
Read orders by the prescriber and answer the question.
Prescriber's orders
Labs: PT, PTT, INR
Unsupervised ambulation every 1 hr
Give protamine sulfate STAT
Give Aspirin orally daily
Continue unrestricted regular diet
Give vitamin K STAT
Initiate bleeding precautions
A nurse is admitting a client who has been in Atrial Fibrillation for 24 hours.
Which of the following interventions does the nurse plan to complete?
(Select All that Apply.)
Explanation
Choice A rationale: Vitamin K is given to counteract the effects of anticoagulants like warfarin, which might have been administered to manage atrial fibrillation1.
Choice B rationale: Heparin is an anticoagulant often used in the initial management of atrial fibrillation to prevent the formation of clots2.
Choice C rationale: PT, PTT, and INR are lab tests used to monitor the effectiveness of anticoagulation therapy1.
Choice D rationale: Coumadin (warfarin) is a long-term anticoagulant therapy often used in the management of atrial fibrillation1.
Choice E rationale: Verapamil is a calcium channel blocker, not typically the first line of treatment for atrial fibrillation3.
So, the correct answer is Choices A, B, C, and D, after analyzing all choices.
A nurse is reviewing medications prescribed for a client. For which of the following prescriptions should the nurse contact the provider for clarification?
Explanation
A. Docusate sodium 200 mg PO at bedtime:
This prescription seems appropriate. Docusate sodium is a stool softener commonly used to prevent or alleviate constipation. Taking it at bedtime can help ensure a regular bowel movement in the morning.
B. Meloxicam 15 mg PO daily:
This prescription is generally appropriate. Meloxicam is a nonsteroidal anti-inflammatory drug (NSAID) used for pain and inflammation. The daily dosing is common, but the nurse should assess for any contraindications or potential issues with the patient's renal function since NSAIDs can affect the kidneys.
C. Regular insulin 8 units subcutaneous before meals:
This prescription requires clarification. While the prescription indicates the correct medication and route (regular insulin subcutaneously), it lacks specificity regarding the timing in relation to meals. Regular insulin is typically given 30 minutes before meals to control postprandial blood glucose levels. The nurse should contact the provider to confirm the appropriate timing.
D. Fentanyl 25 mcg/hr transdermal patch:
This prescription seems appropriate. Fentanyl is a potent opioid analgesic, and a transdermal patch provides continuous pain relief over an extended period. The dose is specified in micrograms per hour (mcg/hr), which is a common method for administering continuous medications
Sign Up or Login to view all the 25 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

