ATI RN Fundamentals 2019 Updated 2023 Exam
Total Questions : 55
Showing 25 questions, Sign in for moreA nurse is delegating client care tasks to an assistive personnel. Which of the following tasks should the nurse delegate?
Explanation
Choice A reason: Inserting an NG tube is a complex and invasive procedure that requires the nurse's assessment and judgment. It is not appropriate to delegate this task to an assistive personnel.
Choice B reason: Performing a simple dressing change is a routine and non-invasive task that can be delegated to an assistive personnel. The nurse should provide clear instructions and monitor the outcome of the task.
Choice C reason: Evaluating the healing of an incision is a skill that requires the nurse's knowledge and expertise. It is not appropriate to delegate this task to an assistive personnel.
Choice D reason: Changing IV tubing is a sterile and technical procedure that involves the administration of fluids and medications. It is not appropriate to delegate this task to an assistive personnel.

A nurse is providing teaching to a client who is at risk for thrombus formation. Which of the following statements made by the client indicates an understanding of the teaching?
Explanation
Choice A reason: Keeping the legs crossed while sitting can impair blood circulation and increase the risk of thrombus formation. This statement indicates a lack of understanding of the teaching.
Choice B reason: Massaging the legs when they hurt can dislodge a thrombus and cause a pulmonary embolism or a stroke. This statement indicates a lack of understanding of the teaching.
Choice C reason: Limiting the time that one spends sitting in a chair can prevent venous stasis and promote blood flow. This statement indicates an understanding of the teaching.
Choice D reason: Performing leg exercises once every 4 hours while awake is not enough to prevent thrombus formation. The client should perform leg exercises at least every hour or as prescribed by the nurse. This statement indicates a lack of understanding of the teaching.
A nurse is documenting client care. Which of the following abbreviations should the nurse use?
Explanation
Choice A reason: SS for sliding scale is not a standard abbreviation and can be confused with other meanings. The nurse should spell out sliding scale or use the abbreviation SSI for sliding scale insulin.
Choice B reason: OJ for orange juice is not a standard abbreviation and can be confused with other meanings. The nurse should spell out orange juice or use the abbreviation OJU for orange juice unit.
Choice C reason: SQ for subcutaneous is a standard abbreviation and is widely used in nursing documentation. It is clear and concise and does not pose any risk of confusion.
Choice D reason: BRP for bathroom privileges is not a standard abbreviation and can be confused with other meanings. The nurse should spell out bathroom privileges or use the abbreviation BPR for bathroom privileges requested.
A nurse is planning care for a client who is concerned about her tobacco smoking habits and is in the contemplation stage of health behavior change. Which of the following actions should the nurse plan to take during this stage?
Explanation
Choice A reason: Recommending small changes for the client to make to change her behavior over time is an action that the nurse should plan to take during the preparation stage of health behavior change, not the contemplation stage.
Choice B reason: Assisting the client in setting goals to make the change is an action that the nurse should plan to take during the preparation stage of health behavior change, not the contemplation stage.
Choice C reason: Developing a plan for the client to integrate the change into her lifestyle is an action that the nurse should plan to take during the action stage of health behavior change, not the contemplation stage.
Choice D reason: Presenting information about the benefits of quitting smoking is an action that the nurse should plan to take during the contemplation stage of health behavior change, as it can help the client to weigh the pros and cons of changing her behavior and increase her motivation to quit.
A nurse is caring for a client who is receiving continuous enteral feeding via NG tube. Which of the following is an unexpected finding?
Explanation
Choice A reason: A weight gain of 0.91 kg (2 lb) in 2 days is an expected finding for a client who is receiving continuous enteral feeding via NG tube, as it indicates that the client is meeting his or her nutritional needs.
Choice B reason: A blood glucose level of 110 mg/dL is an expected finding for a client who is receiving continuous enteral feeding via NG tube, as it indicates that the client's blood glucose is within the normal range.
Choice C reason: Diarrhea one time in a 24-hr period is an expected finding for a client who is receiving continuous enteral feeding via NG tube, as it can be a common side effect of enteral feeding due to the osmolality or composition of the formula.
Choice D reason: A gastric residual of 300 mL at the end of the shift is an unexpected finding for a client who is receiving continuous enteral feeding via NG tube, as it indicates that the client has delayed gastric emptying and is at risk for aspiration. The nurse should stop the feeding and notify the provider.
A nurse is caring for a client who is receiving continuous enteral feedings through a gastrostomy tube. Which of the following actions should the nurse take?
Explanation
Choice A reason: Heating the formula to 40.5°C (105°F) is not an appropriate action for the nurse to take, as it can cause thermal injury to the client's gastrointestinal mucosa. The formula should be at room temperature or slightly warmed.
Choice B reason: Aspirating residual volume every 4 hr is not an appropriate action for the nurse to take, as it can increase the risk of aspiration and infection. The nurse should aspirate residual volume before each feeding or every 6 to 8 hr.
Choice C reason: Flushing the tubing with 10 mL of water every 2 hr is an appropriate action for the nurse to take, as it can prevent clogging and maintain patency of the tube.
Choice D reason: Changing the tubing set every 72 hr is not an appropriate action for the nurse to take, as it can increase the risk of contamination and infection. The nurse should change the tubing set every 24 hr.
A nurse is planning care for a client who has a latex allergy and is scheduled for surgery. Which of the following actions is appropriate to include in the client's plan of care?
Explanation
Choice A reason: Cleansing the stoppers with povidone-iodine before withdrawing medication is not an appropriate action for the nurse to take, as it can cause an allergic reaction in the client who has a latex allergy. The nurse should use latex-free stoppers or avoid puncturing the stoppers.
Choice B reason: Scheduling the client as the first surgical procedure of the day is an appropriate action for the nurse to take, as it can reduce the exposure to latex particles in the air and on the equipment.
Choice C reason: Removing the stopcocks from IV tubing is not an appropriate action for the nurse to take, as it can compromise the sterility and integrity of the IV system. The nurse should use latex-free stopcocks or cover them with a latex-free barrier.
Choice D reason: Ensuring that the gloves in the surgical suite are powdered gloves is not an appropriate action for the nurse to take, as it can increase the risk of latex sensitization and reaction. The nurse should use latex-free or powder-free gloves.
A nurse is planning care for a female client who has an indwelling urinary catheter. Which of the following actions should the nurse include in the plan?
Explanation
Choice A reason: This is the correct action because it prevents backflow of urine and reduces the risk of infection.
Choice B reason: This is an incorrect action because it can cause tension on the catheter and increase the risk of trauma and infection.
Choice C reason: This is an incorrect action because it can cause the drainage bag to become too heavy and pull on the catheter. The drainage bag should be emptied at least every 8 hours or when it is half full.
Choice D reason: This is an incorrect action because it can cause kinking of the catheter and obstruct the flow of urine. The catheter should be taped to the upper thigh for female clients.
A nurse is documenting a dressing change for a client who has a pressure injury. Which of the following entries by the nurse demonstrates correct documentation?
Explanation
Choice A reason: This is an incorrect entry because it does not specify the dose and route of the medication.
Choice B reason: This is an incorrect entry because it uses subjective terms such as 'seems' and 'appear'. The nurse should use objective data to describe the wound.
Choice C reason: This is the correct entry because it provides clear and accurate information about the dressing change and the wound condition.
Choice D reason: This is an incorrect entry because it does not reflect the current assessment of the wound. The nurse should document any changes or progress of the wound healing.
A nurse is performing postural drainage with percussion and vibration for a client who has cystic fibrosis. Which of the following actions should the nurse take?
Explanation
Choice A reason: This is an incorrect action because percussion should be performed over the chest wall, not the back. Percussion helps loosen the mucus in the lungs.
Choice B reason: This is the correct action because covering the area of percussion with a towel reduces the discomfort and bruising of the skin.
Choice C reason: This is an incorrect action because postural drainage should be scheduled before meals or at least 2 hours after meals. Postural drainage after meals can cause nausea and vomiting.
Choice D reason: This is an incorrect action because the client should exhale slowly and deeply during vibration. Vibration helps move the mucus up the airways.
A nurse is caring for a client who has tuberculosis. Which of the following precautions should the nurse plan to implement when working with the client?
Explanation
Choice A reason: This is an incorrect precaution because droplet precautions are used for clients who have infections that are transmitted by large respiratory droplets, such as influenza or pertussis.
Choice B reason: This is the correct precaution because airborne precautions are used for clients who have infections that are transmitted by small respiratory particles that can remain suspended in the air, such as tuberculosis or measles.
Choice C reason: This is an incorrect precaution because protective precautions are used for clients who have compromised immune systems and are at risk of acquiring infections from others, such as clients who have had a bone marrow transplant.
Choice D reason: This is an incorrect precaution because contact precautions are used for clients who have infections that are transmitted by direct or indirect contact with the client or the client's environment, such as clients who have MRSA or C. difficile.
A nurse working on a medical-surgical unit is making client assignments for an upcoming shift. Which of the following tasks should the nurse assign to an assistive personnel?
Explanation
Choice A reason: This is an incorrect task to assign to an assistive personnel because inserting a glycerin suppository requires sterile technique and assessment of the client's bowel function, which are within the scope of practice of a nurse.
Choice B reason: This is an incorrect task to assign to an assistive personnel because showing a client how to use an incentive spirometer requires teaching and evaluation of the client's understanding and technique, which are within the scope of practice of a nurse.
Choice C reason: This is an incorrect task to assign to an assistive personnel because irrigating a client's infected surgical wound requires sterile technique and assessment of the wound healing and drainage, which are within the scope of practice of a nurse.
Choice D reason: This is the correct task to assign to an assistive personnel because assisting with ambulation is a basic activity of daily living that does not require advanced skills or judgment, and is within the scope of practice of an assistive personnel.
A nurse is caring for a client who is postoperative and has a new prescription to advance her diet to full liquids. Which of the following foods should the nurse offer the client as a part of a full liquid diet?
Explanation
Choice A reason: This is an incorrect food to offer the client because oatmeal is a solid food that requires chewing and digestion. A full liquid diet consists of foods that are liquid at room temperature or melt at body temperature, such as soups, milk, ice cream, and juices.
Choice B reason: This is the correct food to offer the client because plain yogurt is a liquid food that does not contain any solid particles or chunks. Plain yogurt also provides protein and calcium, which are important for wound healing and bone health.
Choice C reason: This is an incorrect food to offer the client because scrambled eggs are a solid food that requires chewing and digestion. Scrambled eggs are a part of a regular diet, not a full liquid diet.
Choice D reason: This is an incorrect food to offer the client because applesauce is a semi-solid food that contains some fiber and pulp. Applesauce is a part of a soft diet, not a full liquid diet.
A nurse is preparing to obtain informed consent from a client who speaks a different language than the nurse and is scheduled for surgery. Which of the following actions should the nurse take?
Explanation
Choice A reason: This is an incorrect action to take because using medical terminology can confuse and intimidate the client. The nurse should use simple and clear language when explaining the procedure and its risks and benefits.
Choice B reason: This is the correct action to take because recommending an interpreter who is the same gender as the client can help reduce the client's anxiety and discomfort, especially if the procedure involves sensitive or private areas of the body. The nurse should also respect the client's cultural and religious preferences when choosing an interpreter.
Choice C reason: This is an incorrect action to take because addressing all questions to the interpreter can make the client feel ignored and disrespected. The nurse should maintain eye contact and speak directly to the client, using the interpreter as a facilitator of communication, not a substitute.
Choice D reason: This is an incorrect action to take because having the client nod to indicate understanding is not a reliable way to assess the client's comprehension and consent. The nurse should ask the client to repeat back or demonstrate what they have learned, and document the client's verbal or written consent.
A nurse is implementing seizure precautions for a client who has a seizure disorder. Which of the following equipment should the nurse place at the client’s bedside? (Select all that apply.)
Explanation
Choice A reason: This is an incorrect equipment to place at the client's bedside because limb restraints can cause injury and increase the risk of aspiration during a seizure. The nurse should only use restraints if the client poses a danger to themselves or others, and only with a physician's order.
Choice B reason: This is a correct equipment to place at the client's bedside because oral suction equipment can help clear the airway of secretions and prevent choking during or after a seizure.
Choice C reason: This is a correct equipment to place at the client's bedside because supplemental oxygen supplies can help maintain adequate oxygenation and prevent hypoxia during or after a seizure.
Choice D reason: This is an incorrect equipment to place at the client's bedside because blood glucose monitor is not directly related to seizure precautions. The nurse should monitor the blood glucose level of the client who has diabetes or hypoglycemia, but this is not a priority during a seizure.
Choice E reason: This is a correct equipment to place at the client's bedside because oral airway can help keep the airway open and prevent tongue biting during a seizure. However, the nurse should not insert the oral airway until the seizure is over and the client is unconscious.
A nurse is providing teaching for a client who is scheduled for an allogeneic stem cell transplant. Which of the following information should the nurse include?
Explanation
Choice A reason: This is an incorrect information to include because a negative-airflow room is used for clients who have airborne infections, such as tuberculosis or chickenpox. A client who is undergoing an allogeneic stem cell transplant needs a positive-airflow room, which filters the air and prevents the entry of microorganisms.
Choice B reason: This is an incorrect information to include because a client who is undergoing an allogeneic stem cell transplant needs a private room, which reduces the exposure to other clients and staff who may carry infections.
Choice C reason: This is the correct information to include because a client who is undergoing an allogeneic stem cell transplant has a weakened immune system and is at risk of developing graft-versus-host disease, which is a reaction of the donor cells against the client's tissues. Therefore, the visitors need to wear protective gowns, gloves, and masks to prevent the transmission of infections.
Choice D reason: This is an incorrect information to include because a client who is undergoing an allogeneic stem cell transplant should avoid going outside of the room unless absolutely necessary, such as for diagnostic tests or procedures. A mask alone is not sufficient to protect the client from infections.
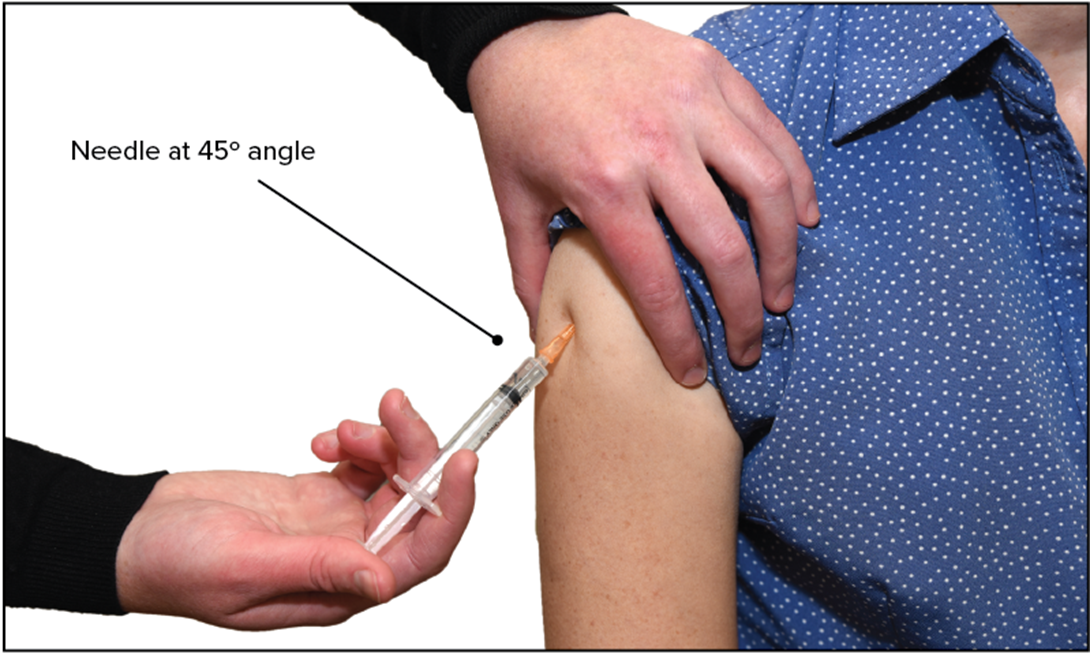
A nurse is preparing a medication from a vial for a subcutaneous injection for a client. Which of the following actions should the nurse take?
Explanation
Choice A reason: This is an incorrect action to take because injecting air into the vial with the eye of the needle immersed in the fluid can cause contamination and waste of the medication. The nurse should inject air into the vial with the needle above the fluid level.
Choice B reason: This is an incorrect action to take because holding the syringe at a 45° angle can distort the accuracy of the dosage. The nurse should hold the syringe at a 90° angle to verify dosage.
Choice C reason: This is the correct action to take because holding the syringe so that bubbles collect at the level of the plunger can help the nurse expel the bubbles and ensure the correct dosage of the medication.
Choice D reason: This is an incorrect action to take because holding the vial with the top facing upward while injecting air into the vial can create a positive pressure in the vial and make it difficult to withdraw the medication. The nurse should hold the vial with the top facing downward while injecting air into the vial.
A nurse is caring for a client who is postoperative and asks the nurse, "When will I get to go home? I'm not sure what happens next." Which of the following actions should the nurse take?
Explanation
Choice A reason: This is an incorrect action to take because assuring the client that the provider will come to talk to him when she gets the chance can make the client feel unimportant and neglected. The nurse should acknowledge the client's concerns and advocate for his right to information.
Choice B reason: This is an incorrect action to take because explaining that the client should trust the provider because she has an excellent reputation can make the client feel dismissed and patronized. The nurse should respect the client's autonomy and encourage him to ask questions and participate in his care.
Choice C reason: This is the correct action to take because informing the provider that the client is requesting information about his treatment plan can facilitate effective communication and collaboration between the client and the provider. The nurse should also provide the client with relevant and accurate information as appropriate.
Choice D reason: This is an incorrect action to take because telling the client that the provider will discharge him when she feels he is ready to leave can make the client feel powerless and dependent. The nurse should explain the criteria and goals for discharge and involve the client in the planning and evaluation of his care.
A nurse is caring for a client who has restraints to each extremity. Which of the following assessments should the nurse perform first?
Explanation
Choice A reason: This is an important assessment to perform for a client who has restraints, but not the first priority. The nurse should check the skin integrity of the restrained areas every 2 hours to prevent pressure ulcers and skin breakdown.
Choice B reason: This is the first assessment to perform for a client who has restraints, because restraints can impair the blood circulation and cause tissue ischemia and nerve damage. The nurse should check the peripheral pulses of the restrained extremities every 15 minutes to ensure adequate perfusion and sensation.
Choice C reason: This is an important assessment to perform for a client who has restraints, but not the first priority. The nurse should assess the comfort level of the client and provide pain relief and emotional support as needed. The nurse should also explain the rationale for the restraints and try to reduce the use of restraints as much as possible.
Choice D reason: This is an important assessment to perform for a client who has restraints, but not the first priority. The nurse should assess the elimination needs of the client and provide assistance with toileting and hygiene as needed. The nurse should also monitor the fluid intake and output of the client and prevent dehydration and urinary retention.
A nurse is caring for a client who is 2 days postoperative following bowel resection and reports sudden, severe abdominal pain. Which of the following actions should the nurse take first?
Explanation
Choice A reason: This is an important action to take for a client who is postoperative following bowel resection, but not the first priority. The nurse should use the diaphragm of a stethoscope to listen for bowel sounds in all four quadrants to assess the gastrointestinal motility and function. However, this action can be delayed until the nurse rules out any signs of complications, such as wound dehiscence or evisceration.
Choice B reason: This is an incorrect action to take for a client who is postoperative following bowel resection and reports sudden, severe abdominal pain. The nurse should avoid performing abdominal palpation, especially over the incision site, because it can cause more pain and increase the risk of wound disruption. The nurse should only palpate the abdomen gently and carefully if indicated by the provider.
Choice C reason: This is an important action to take for a client who is postoperative following bowel resection, but not the first priority. The nurse should determine areas of resonance across the abdomen using a systematic approach to assess the presence and distribution of gas in the abdominal cavity. However, this action can be delayed until the nurse rules out any signs of complications, such as wound infection or peritonitis.
Choice D reason: This is the first action to take for a client who is postoperative following bowel resection and reports sudden, severe abdominal pain. The nurse should expose the client’s abdomen to look for changes in appearance, such as swelling, redness, drainage, or protrusion of the bowel through the wound. These changes can indicate serious complications that require immediate intervention.
A nurse in an emergency department is assessing a client who reports right lower quadrant pain, nausea, and vomiting for the past 48 hr. Which of the following actions should the nurse take first?
Explanation
Choice A reason: This is an important action to take for a client who reports nausea and vomiting, but not the first priority. The nurse should administer an antiemetic as prescribed to relieve the symptoms and prevent dehydration and electrolyte imbalance.
Choice B reason: This is an important action to take for a client who reports right lower quadrant pain, but not the first priority. The nurse should offer pain medication as prescribed to reduce the discomfort and anxiety.
Choice C reason: This is an incorrect action to take for a client who reports right lower quadrant pain, especially as the first action. The nurse should avoid palpating the abdomen, especially the area of pain, because it can cause more pain and inflammation, and possibly rupture the appendix if the client has appendicitis.
Choice D reason: This is the first action to take for a client who reports right lower quadrant pain, nausea, and vomiting. The nurse should auscultate bowel sounds in all four quadrants to assess the gastrointestinal function and peristalsis. The nurse should also note the presence and quality of the bowel sounds, such as normal, hypoactive, hyperactive, or absent.
A nurse is providing care for a client who is to undergo a total laryngectomy. Which of the following interventions is the nurse's priority?
Explanation
Choice A reason: This is an important intervention to provide for a client who is to undergo a total laryngectomy, but not the priority. The nurse should schedule a support session for the client to help him cope with the emotional and psychological impact of losing his voice and facing a major surgery.
Choice B reason: This is an important intervention to provide for a client who is to undergo a total laryngectomy, but not the priority. The nurse should explain the techniques of esophageal speech, which is a method of producing sound by swallowing air and releasing it through the esophagus. The nurse should also refer the client to a speech therapist for further training and practice.
Choice C reason: This is an important intervention to provide for a client who is to undergo a total laryngectomy, but not the priority. The nurse should determine the client’s reading ability to assess his literacy level and educational needs. The nurse should also provide the client with written materials and resources that are appropriate for his reading level.
Choice D reason: This is the priority intervention to provide for a client who is to undergo a total laryngectomy. The nurse should review the use of an artificial larynx with the client, which is a device that produces sound by vibrating against the neck or cheek. The nurse should also teach the client how to operate, clean, and maintain the device, and encourage him to practice using it before and after the surgery.
A nurse is teaching a client how to self-administer daily low-dose heparin injections. Which of the following factors is most likely to increase the client’s motivation to learn?
Explanation
Choice A reason: This is the correct factor to increase the client’s motivation to learn because it reflects the client’s self-efficacy and perceived value of the education. The client who believes that his needs will be met through education is more likely to be engaged and receptive to the teaching.
Choice B reason: This is an important factor to provide for the client, but not the most likely to increase the client’s motivation to learn. The nurse explaining the need for education to the client can help the client understand the rationale and benefits of the education, but it does not necessarily address the client’s personal goals and preferences.
Choice C reason: This is an incorrect factor to increase the client’s motivation to learn because it reflects the client’s external motivation and compliance, not his intrinsic motivation and interest. The client who seeks family approval by agreeing to a teaching plan may not be fully committed or enthusiastic about the education.
Choice D reason: This is an important factor to provide for the client, but not the most likely to increase the client’s motivation to learn. The nurse’s empathy about the client having to self-inject can help the client feel supported and respected, but it does not necessarily enhance the client’s confidence and competence in the education.
A nurse is teaching a group of newly licensed nurses about the Braden scale. Which of the following responses by a newly licensed nurse indicates an understanding of the teaching?
Explanation
Choice A reason: This is an incorrect response by a newly licensed nurse because it does not reflect an understanding of the teaching. Each element of the Braden scale has a range from one to four points, not one to five points. The elements are sensory perception, moisture, activity, mobility, nutrition, and friction and shear.
Choice B reason: This is the correct response by a newly licensed nurse because it reflects an understanding of the teaching. The scale measures six elements that affect the risk of developing a pressure injury. The elements are sensory perception, moisture, activity, mobility, nutrition, and friction and shear.
Choice C reason: This is an incorrect response by a newly licensed nurse because it does not reflect an understanding of the teaching. The client’s age is not part of the measurement of the Braden scale. The scale does not consider the client’s age, gender, race, or diagnosis.
Choice D reason: This is an incorrect response by a newly licensed nurse because it does not reflect an understanding of the teaching. The higher the score, the lower the pressure injury risk, not the higher. The score ranges from 6 to 23, with 6 being the highest risk and 23 being the lowest risk.
A nurse is planning care for a client who has a new prescription for parenteral nutrition (PN) in 20% dextrose and fat emulsions. Which of the following is an appropriate action to include in the plan of care?
Explanation
Choice A reason: This is the appropriate action to include in the plan of care because a central venous line is required for PN solutions that have a high osmolarity, such as 20% dextrose and fat emulsions. A central venous line can deliver the PN solution into a large vein, such as the superior vena cava, and prevent complications such as thrombophlebitis and extravasation.
Choice B reason: This is an incorrect action to include in the plan of care because the PN infusion bag should be changed every 24 hr, not every 48 hr. Changing the PN infusion bag every 24 hr can reduce the risk of bacterial contamination and infection.
Choice C reason: This is an incorrect action to include in the plan of care because a random blood glucose is not sufficient to monitor the client's blood glucose level. The nurse should obtain a blood glucose level before starting the PN infusion and every 4 to 6 hr thereafter, or as prescribed by the provider. The nurse should also adjust the infusion rate and administer insulin as needed to prevent hyperglycemia or hypoglycemia.
Choice D reason: This is an incorrect action to include in the plan of care because the PN and fat emulsion can be administered together in the same infusion bag, as long as they are compatible and stable. Administering the PN and fat emulsion separately can increase the risk of infection and fluid overload.
Sign Up or Login to view all the 55 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

