ATI_RN_Fundamentals_2019_with_NGN
Total Questions : 71
Showing 25 questions, Sign in for moreExplanation
Leaving the drain until the end of the shift is not appropriate because it could lead to complications such as:
- Hematoma formation:Blood accumulation in the tissues surrounding the drain can put pressure on surrounding structures,potentially impairing blood flow and causing tissue damage.
- Infection:A reservoir containing blood provides a favorable environment for bacterial growth,increasing the risk of infection.
- Drain occlusion:Clotted blood can block the drain,preventing effective drainage and leading to fluid buildup and potential infection.
- Decreased wound healing:Excessive blood loss can delay wound healing by depriving the tissues of necessary oxygen and nutrients.
Removing the drain without the surgeon's order is not appropriate because:
- Premature removal:It could disrupt the healing process and lead to complications such as fluid collection or infection.
- Assessment limitation:Removing the drain would eliminate the ability to monitor ongoing blood loss and could mask potential complications.
A Jackson-Pratt drain works by creating suction when the bulb is squeezed and emptied¹. The bulb should be emptied before it is more than half full to avoid the discomfort of the weight of the drain pulling on the internal tubing and to maintain the suction
Notifying the surgeon about the blood loss is wrong because it is not an urgent situation unless there are signs of excessive bleeding, such as bright red blood, clots, or a sudden increase in the amount of drainage²³. The surgeon should be notified if the drainage is more than 100 ml in 24 hours or if the color changes from serosanguineous (pink) to sanguineous (red)
A nurse is caring for a client who has a prescription for a 250 mL IV fluid bolus. The nurse administers a 500 mL IV bolus.
Which of the following actions should the nurse take first?
Explanation
Notify the healthcare provider.
The nurse should first notify the healthcare provider of the error in administering the IV bolus.
This is important because the healthcare provider can assess the situation and provide guidance on how to proceed.
Choice A is not the correct answer because obtaining the client’s vital signs is important but not the first action the nurse should take.
Choice C is not the correct answer because documenting the incident in the client’s medical record is important but not the first action the nurse should take.
Choice D is not the correct answer because assessing the client for adverse reactions is important but not the first action the nurse should take.
A nurse is documenting client care.
Which of the following abbreviations should the nurse use?
Explanation
The nurse should use the abbreviation “BRP” for bathroom privileges.
This is a commonly accepted abbreviation in the medical field and is used to indicate that a client has permission to use the bathroom.
Choice A is not the correct answer because “SC” is not a commonly accepted abbreviation for subcutaneous.
Instead, “SQ” or “SubQ” are more commonly used.
Choice B is not the correct answer because “SS” is not a commonly accepted abbreviation for sliding scale.
Instead, “Sliding Scale” should be written out in full to avoid confusion.
Choice D is not the correct answer because “OJ” is not a commonly accepted medical abbreviation for orange juice.
Instead, “orange juice” should be written out in full to avoid confusion.
A nurse is caring for a client.
Exhibit 1 Vital Signs 0800: Exhibit 2 Temperature 37.6° C (99.7° F) Blood pressure 108/56 mm Hg Heart rate 66/min Respiratory rate 18/min Pulse oximetry 97% on room air 0830: Temperature 37.5° C (99.5° F) Blood pressure 88/56 mm Hg Heart rate 104/min Respiratory rate 24/min Pulse oximetry 93% on room air Select the 4 findings that require immediate follow-up.
Explanation
The blood pressure has dropped significantly from 108/56 mm Hg to 88/56 mm Hg.
The pulse oximetry has decreased from 97% to 93%, indicating a decrease in oxygen saturation.
The heart rate has increased from 66/min to 104/min.
The level of consciousness is always an important factor to monitor in a patient.
A. Temperature: The temperature has only changed slightly and is within the normal range.
C. Respiratory rate: The respiratory rate has increased but is still within normal range.
G. Skin color and temperature: This information is not provided in the exhibit.
A nurse is preparing to insert an IV catheter for an adult client.
Which of the following actions should the nurse take?
Explanation
The nurse should place the extremity in a dependent position before inserting an IV catheter.
This helps to dilate the veins and make them more visible and easier to access.
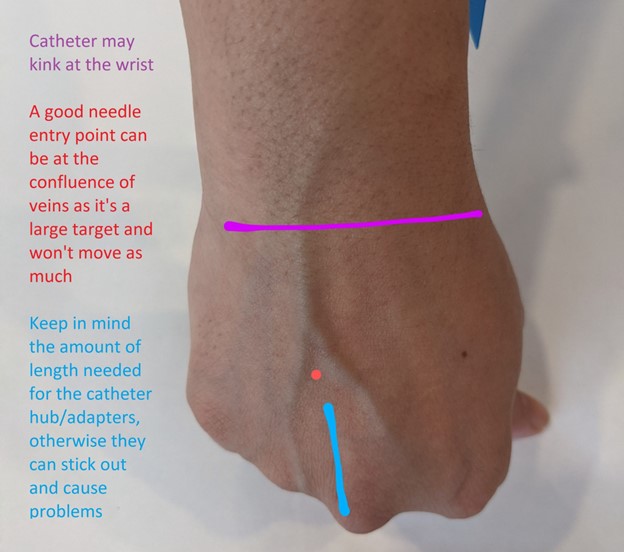
Choice A is wrong because the nurse should choose a site that is distal to the most proximal site on the extremity selected.
This helps to preserve more proximal sites for future use if needed.
Choice B is wrong because applying a cool compress before insertion of an IV catheter can cause vasoconstriction and make it more difficult to access the vein.
Instead, a warm compress can be applied to help dilate the veins.
Choice C is wrong because the tourniquet should be placed above, not below, the proposed insertion site to help dilate the vein and make it easier to access.
A nurse is implementing seizure precautions for a client who has a seizure disorder.
Which of the following equipment should the nurse place at the client's bedside? (Select all that apply.).
Explanation
An oral airway can help maintain an open airway during a seizure.
Supplemental oxygen supplies can be used to provide oxygen if the client’s breathing is compromised.
Oral suction equipment can be used to clear secretions from the client’s mouth and prevent aspiration.

Limb restraints: Restraints should not be used during a seizure as they can cause injury.
Blood glucose monitor: While it is important to monitor blood glucose levels in clients with seizures, it is not a priority during a seizure.
A nurse is teaching a group of newly licensed nurses about the Braden scale.
Which of the following responses by a newly licensed nurse indicates an understanding of the teaching?
Explanation
The Braden scale measures six elements: sensory perception, moisture, activity, mobility, nutrition, and friction/shear.
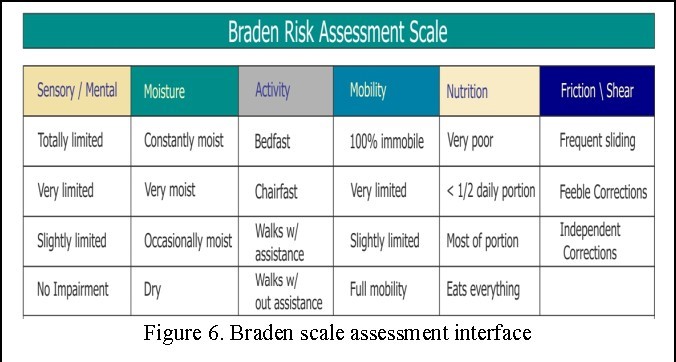
“The higher the score, the higher the pressure injury risk”: This statement is incorrect.
The lower the score on the Braden scale, the higher the risk for pressure injury.
“Each element has a range from one to five points”: This statement is incorrect.
Each element has a range from one to four points, except for friction/shear which has a range from one to three points.
“The client’s age is part of the measurement”: This statement is incorrect. Age is not one of the elements measured by the Braden scale.
A nurse is planning care for a female client who has an indwelling urinary catheter.
Which of the following actions should the nurse include in the plan?
Explanation
This is important to prevent urine from flowing back into the bladder, which can cause infection 1.
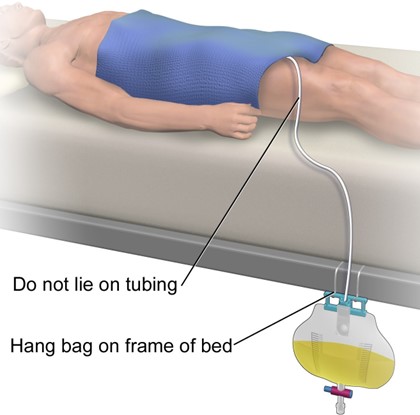
Choice A is incorrect because the catheter should be secured to the outer side of the thigh, not taped to the lower abdomen 2.
Choice B is incorrect because attaching the drainage bag to the side rails of the bed can cause it to be above the level of the bladder.
Choice C is incorrect because it is important to empty the drainage bag regularly, not just when it is three-quarters full.
A nurse is caring for a client who is receiving continuous enteral feeding via NG tube.
Which of the following is an unexpected finding?
Explanation
Gastric residual of 300 mL at the end of the shift is an unexpected finding.
Gastric residual volume refers to the volume of fluid remaining in the stomach during enteral feeding.
A gastric residual volume of less than or equal to 500 mL every 6 hours is considered safe and indicates that the gastrointestinal tract is functioning.
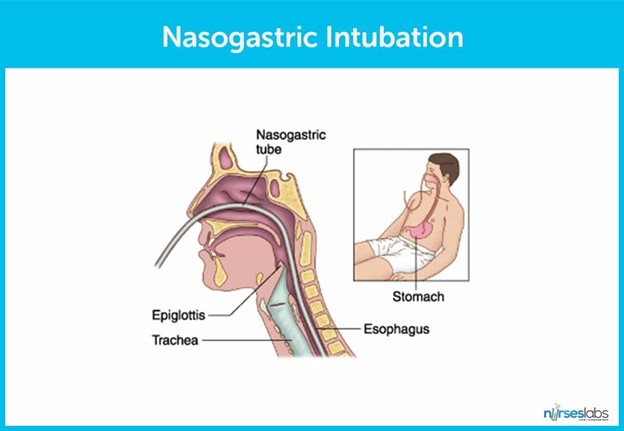
Choice B is wrong because weight gain is expected during enteral feeding.
Choice C is wrong because a blood glucose level of 110 mg/dL is within the normal range.
Choice D is wrong because diarrhea can be a common side effect of enteral feeding.
A nurse is caring for a client who has a tracheostomy.
Which of the following actions should the nurse take?
Explanation
Secure the tracheostomy ties to allow one finger to fit snugly underneath. This is important to ensure that the tracheostomy tube is secure and in place.
Choice B is wrong because normal saline is not typically used to cleanse the skin around the stoma.
Choice C is wrong because soaking the outer cannula in warm, soapy tap water is not a recommended method of cleaning.
Choice D is wrong because a cotton tip applicator should not be used to clean inside the inner cannula.
A nurse is providing teaching for a client who is scheduled for an allogeneic stem cell transplant.
Which of the following information should the nurse include?
Explanation
“Your visitors will need to wear protective gowns.” This is important to prevent the spread of infection to the patient.

Choice B is wrong because the client will be placed in a protective environment room, not a semi-private room.
Choice C is correct because the patient will need to wear respiratory protection when leaving their protective environment room during periods of construction 1.
Choice D is wrong because the client will be placed in a positive-pressure room, not a negative-airflow room.
A nurse is providing teaching to a client who is at risk for thrombus formation.
Which of the following statements made by the client indicates an understanding of the teaching?
Explanation
“I should limit the time that I spend sitting in a chair.” This is important because sitting for long periods of time can increase the risk of thrombus formation.
Choice A is wrong because crossing the legs while sitting can impede blood flow and increase the risk of thrombus formation.
Choice B is wrong because leg exercises should be performed more frequently than once every 4 hours while awake.
Choice D is wrong because massaging the legs when they hurt can dislodge a thrombus and cause it to travel to other parts of the body.
A nurse is planning care for a client who is concerned about her tobacco smoking habits and is in the contemplation stage of health behavior change.
Which of the following actions should the nurse plan to take during this stage?
Explanation
During the contemplation stage of health behavior change, the client is thinking about change and becoming motivated to get started.
The nurse should present information about the benefits of quitting smoking to help the client assess the benefits of change.

Choice A is not correct because developing a plan for the client to integrate the change into her lifestyle is more appropriate for the preparation stage.
Choice B is not correct because recommending small changes for the client to make to change her behavior over time is more appropriate for the action stage.
Choice C is not correct because assisting the client in setting goals to make the change is more appropriate for the preparation stage.
A charge nurse in a long-term care facility is preparing an educational program about delirium for newly hired nurses. Which of the following statements should the nurse plan to include?
Explanation
“Delirium has an abrupt onset.” Delirium is a serious change in mental abilities that results in confused thinking and a lack of awareness of someone’s surroundings.
The disorder usually comes on fast — within hours or a few days.
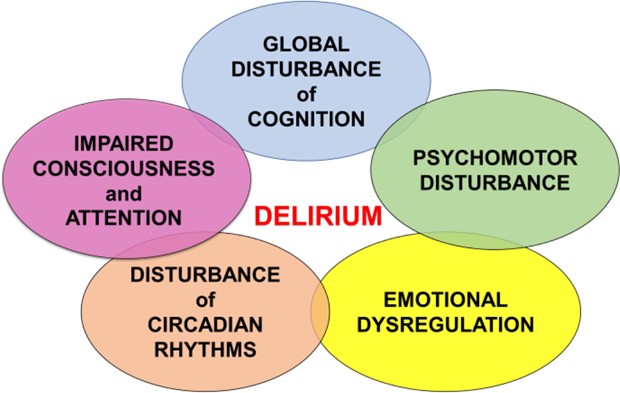
Choice A is wrong because delirium does affect a client’s perception of her environment.
Choice B is wrong because delirium does not have a slow progression, but rather an abrupt onset.
Choice C is wrong because delirium can affect a client’s sleep cycle.
A nurse is planning care for a client who has a new prescription for parenteral nutrition (PN) in 20% dextrose and fat emulsions.
Which of the following is an appropriate action to include in the plan of care?
Explanation
Prepare the client for a central venous line.
Parenteral nutrition (PN) with 20% dextrose and fat emulsions is a hypertonic solution that requires infusion through a central venous line to prevent damage to peripheral veins.
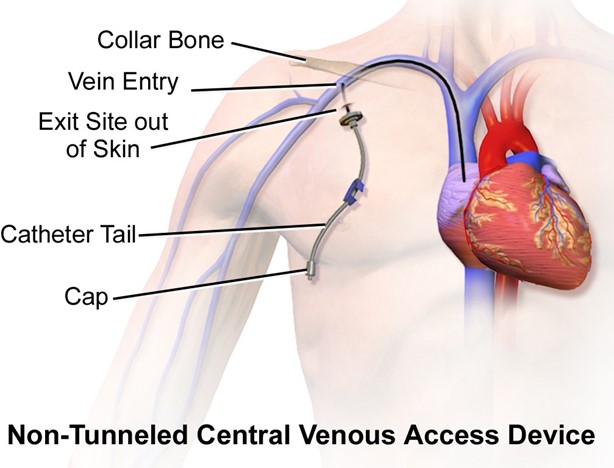
Choice A is wrong because the PN infusion bag should be changed every 24 hours, not every 48 hours.
Choice Cis wrong because blood glucose should be monitored more frequently than once daily when initiating PN therapy.
Choice Dis wrong because PN and fat emulsions can be administered together in a total nutrient admixture (TNA)1.
A nurse receives a new prescription over the telephone from a client's provider. Which of the following actions should the nurse take first?
Explanation
When receiving a new prescription over the telephone from a client’s provider, the nurse should first write down the complete prescription to ensure that all the details are accurately recorded.
Choice B is wrong because reading back the prescription to the provider should be done after writing down the complete prescription.
Choice C is wrong because documenting the prescription as a telephone prescription in the medical record should be done after writing down the complete prescription and reading it back to the provider.
Choice D is wrong because ensuring that the provider signs the prescription should be done after writing down the complete prescription, reading it back to the provider, and documenting it in the medical record.
A nurse is caring for a client who reports that she has insomnia.
Which of the following interventions is appropriate for the nurse to recommend?
Explanation
Eating a light carbohydrate snack before bedtime can help promote sleep by increasing the level of tryptophan in the brain.
Choice B is wrong because taking a 30-min nap daily can disrupt nighttime sleep and worsen insomnia.
Choice C is wrong because drinking a cup of hot cocoa before bedtime can interfere with sleep due to its caffeine content.
Choice D is wrong because exercising 1 hr before bedtime can increase alertness and make it more difficult to fall asleep.
A nurse is caring for a client who is 2 days postoperative following bowel resection and reports sudden, severe abdominal pain.
Which of the following actions should the nurse take first?
Explanation
After postoperative surgery, chances of infections are very high also discharges, color changes, etc.
So it is important to expose the client’s abdomen to look for changes in appearance.
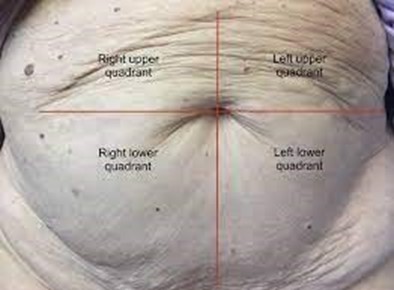
Choice B is not the answer because determining areas of resonance across the abdomen using a systematic approach is not the first action that should be taken 1.
Choice C is not the answer because using the diaphragm of a stethoscope to listen for bowel sounds is not the first action that should be taken 1.
Choice D is not the answer because performing abdominal palpation by pressing gently with the finger pads is not the first action that should be taken 1.
A nurse is planning care for a client who is scheduled for an intravenous pyelogram.
Which of the following actions is appropriate for the nurse to include?
Explanation
An intravenous pyelogram (IVP) is an X-ray exam of the urinary tract that involves intravenous injection of a radiopaque dye that is filtered by the kidney and excreted through the urinary tract12.
To prepare for the exam, the patient’s bowel must be cleared of gas and fecal matter because they may cause shadows in the X-ray film.
Cathartics are usually given the evening before the examination.
Choice B is wrong because monitoring for pain in the suprapubic region is not mentioned as a necessary action for an IVP.
Choice C is wrong because ensuring the client is free of metal objects is not mentioned as a necessary action for an IVP.
Choice D is wrong because administering oral contrast before the procedure is not mentioned as a necessary action for an IVP.
A nurse is conducting Weber's test on a client.
Which of the following is an appropriate action for the nurse to take?
Explanation
The Weber test is a screening test for hearing performed with a tuning fork that can detect unilateral conductive hearing loss and unilateral sensorineural hearing loss.
To perform Weber’s test, strike the fork against your knee or elbow, then place the base of the fork in the midline, high on the patient’s forehead.
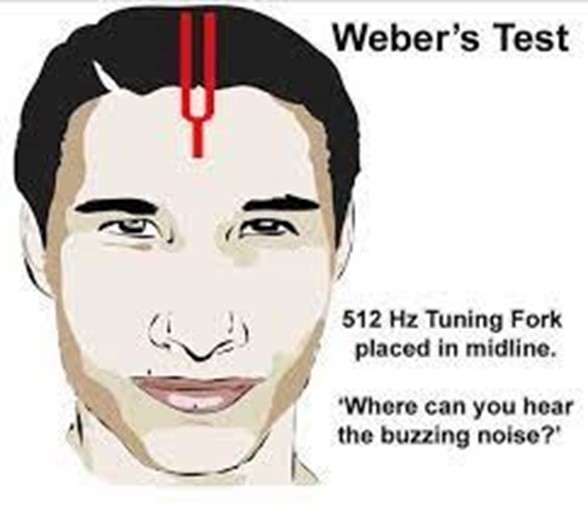
Choice A is wrong because delivering a series of high-pitched sounds at random intervals is not part of Weber’s test.
Choice B is wrong because holding an activated tuning fork against the client’s mastoid process is part of Rinne’s test, not Weber’s test.
Choice D is wrong because whispering a series of words softly into one ear is not part of Weber’s test.
A nurse is teaching a newly licensed nurse about the care of a client who has a methicillin-resistant Staphylococcus aureus (MRSA) infection.
Which of the following statements by the newly licensed nurse indicates an understanding of the teaching?
Explanation
A client with MRSA infection should be placed in a private room to prevent the spread of infection.
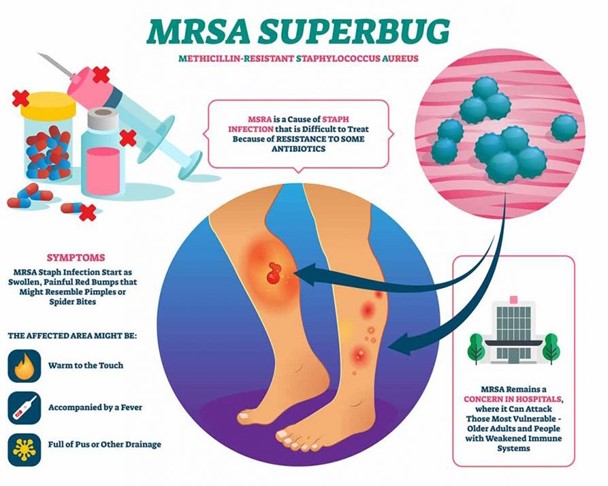
Choice A is wrong because an N95 respirator mask is not necessary when caring for a client with an MRSA infection.
Choice C is wrong because the proper sequence for removing personal protective equipment is to remove gloves first, then the gown.
Choice D is wrong because visitors do not need to wear a mask when they are within 3 feet of the client with an MRSA infection.
A community health nurse is teaching a group of clients about Kegel exercises to prevent urinary incontinence.
Which of the following instructions should the nurse include?
Explanation
“Contract your pelvic muscle when performing the exercises.” Kegel exercises strengthen the pelvic floor muscles, which support the uterus, bladder, small intestine, and rectum.
To do Kegels correctly, you need to contract and relax your pelvic floor muscles.
Choice A is wrong because you should avoid holding your breath while doing Kegel exercises.
Instead, breathe freely during the exercises.
Choice C is wrong because you should focus on tightening only your pelvic floor muscles and be careful not to flex the muscles in your buttocks.
Choice D is wrong because it takes time to strengthen pelvic floor muscles.
You should aim for at least three sets of 10 to 15 repetitions a day and give it 3 to 6 weeks before expecting improvement12.
A nurse is caring for an infant who is to undergo surgery.
The nurse should identify which of the following individuals should sign the consent form?
Explanation
In general, parental (or legal guardian) consent is required for any diagnostic or surgical procedure performed on a child under the age of 181.
Choice A is wrong because the mother’s 21-year-old sibling is not a parent or legal guardian of the infant.
Choice B is wrong because the infant’s provider cannot sign the consent form on behalf of the infant.
Choice C is wrong because the infant’s grandparent cannot sign the consent form unless they are a legal guardian of the infant.
A home health nurse is teaching a client about home safety.
Which of the following statements by the client indicates an understanding of the teaching? (Select all that apply.).
Explanation
“I need to have a fire escape plan with my family,” “I will use the grab bars when getting in and out of the bathtub,” and “I need to check my medications for expiration dates” are all important home safety measures.
Choice A is wrong because setting the hot water heater to 140 degrees Fahrenheit is too high and can increase the risk of scalding.
The recommended temperature for a hot water heater is 120 degrees Fahrenheit.
Choice B is wrong because applying tape over frayed areas of electrical cords is not a safe solution.
Frayed electrical cords should be replaced to prevent electrical hazards.
Explanation
The correct answers are:
- c."I need to have a fire escape plan with my family."
- d."I will use the grab bars when getting in and out of the bathtub."
Rationale for each choice:
Choice c:
Having a fire escape plan is crucial for home safety. It ensures that all family members know what to do in the event of a fire, which can save valuable time and lives. Here's a detailed explanation of why a fire escape plan is essential:
- Early Escape:A plan promotes quick evacuation,as everyone understands the escape routes and procedures.
- Reduced Panic:Knowing what to do in a crisis minimizes panic and confusion,allowing for calmer and more efficient actions.
- Accountability:The plan ensures that no one is left behind,especially children,older adults,or individuals with disabilities.
- Firefighter Assistance:It provides vital information to firefighters,aiding their rescue efforts.
- Regular Practice:Regularly practicing the plan familiarizes everyone with their roles and actions,ensuring smoother execution in a real fire.
Choice d:
Grab bars provide stability and support, reducing the risk of falls in bathrooms. Falls are a major safety hazard, especially for older adults, and can lead to serious injuries. Grab bars offer several benefits, including:
- Entering and Exiting:They facilitate safe entry and exit from the bathtub or shower,especially on slippery surfaces.
- Balance Support:They provide support when standing,reducing the likelihood of losing balance.
- Transfer Assistance:They assist individuals with mobility impairments in safely transferring between the bathtub,shower,or toilet.
- Confidence Boost:They offer a sense of security,allowing individuals to feel more confident and independent in the bathroom.
Rationale for incorrect choices:
Choice a:
Setting a hot water heater to 140 degrees Fahrenheit is unsafe. It can cause scalding burns within seconds, especially for children and older adults. The recommended temperature is 120 degrees Fahrenheit to balance safety and energy efficiency.
Choice b:
Taping over frayed electrical cords is a temporary and hazardous fix. It does not address the underlying issue of damaged wiring, which can lead to electrical shocks, fires, or electrocution. Frayed cords should be replaced immediately with new, undamaged ones.
Sign Up or Login to view all the 71 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

