ATI RN Fundamentals - Exam 2
Total Questions : 46
Showing 25 questions, Sign in for moreThe nurse is performing a respiratory assessment on a client. Which of the following findings should the nurse report to the practitioner?
Explanation
A. Clear and equal breath sounds bilaterally
Explanation: Clear and equal breath sounds bilaterally indicate normal lung sounds, suggesting proper air exchange in both lungs. This is a normal finding and does not require immediate reporting.
B. Oxygen saturation of 98% on room air
Explanation: An oxygen saturation level of 98% on room air indicates adequate oxygenation of the blood. This is a normal and healthy oxygen saturation level and does not require immediate reporting.
C. Cough producing clear, thin sputum
Explanation: A cough producing clear, thin sputum is indicative of a non-infected or non-inflammatory condition in the respiratory system. Clear and thin sputum is often normal, especially in the absence of other symptoms. It does not require immediate reporting unless the client has other concerning symptoms.
D. Visible use of accessory muscles during inhalation
Explanation: Visible use of accessory muscles, such as neck or intercostal muscles, during inhalation suggests that the client is working hard to breathe. This could indicate respiratory distress, potentially due to conditions like asthma, COPD (Chronic Obstructive Pulmonary Disease), or other severe lung problems. It's a concerning sign and should be reported to the healthcare practitioner promptly for further evaluation and intervention.
Which of the following assessment findings should the nurse report to the practitioner? (Select all that apply)
Explanation
A. Use of accessory muscles
Explanation: Using accessory muscles during breathing indicates increased effort to breathe, which can be a sign of respiratory distress. It suggests that the client is having difficulty breathing and is using additional muscles to aid in the process. This finding should be reported to the practitioner for further evaluation.
B. Nail bed greater than 160 degrees
Explanation: A nail bed angle greater than 160 degrees, also known as clubbing, is an abnormal finding and can be associated with chronic respiratory or cardiovascular conditions. It may indicate insufficient oxygenation and should be reported to the practitioner for evaluation.
C. Circumoral cyanosis
Explanation: Circumoral cyanosis, which is a bluish discoloration around the mouth, indicates inadequate oxygenation. It can be a sign of respiratory or cardiac problems and should be reported to the practitioner for further assessment and intervention.
D. Pursed lip breathing
Explanation: Pursed lip breathing is a technique often used by individuals with respiratory difficulties to improve oxygen exchange. However, if it's observed in a person who does not normally use this technique, it could indicate respiratory distress and should be reported to the practitioner for evaluation.
E. Anteroposterior-to-transverse diameter of 1:1
Explanation: An anteroposterior-to-transverse diameter of 1:1 (also known as barrel chest) is an abnormal finding often associated with chronic obstructive pulmonary disease (COPD). It suggests overinflation of the lungs and can impair effective breathing. This finding should be reported to the practitioner for further evaluation.
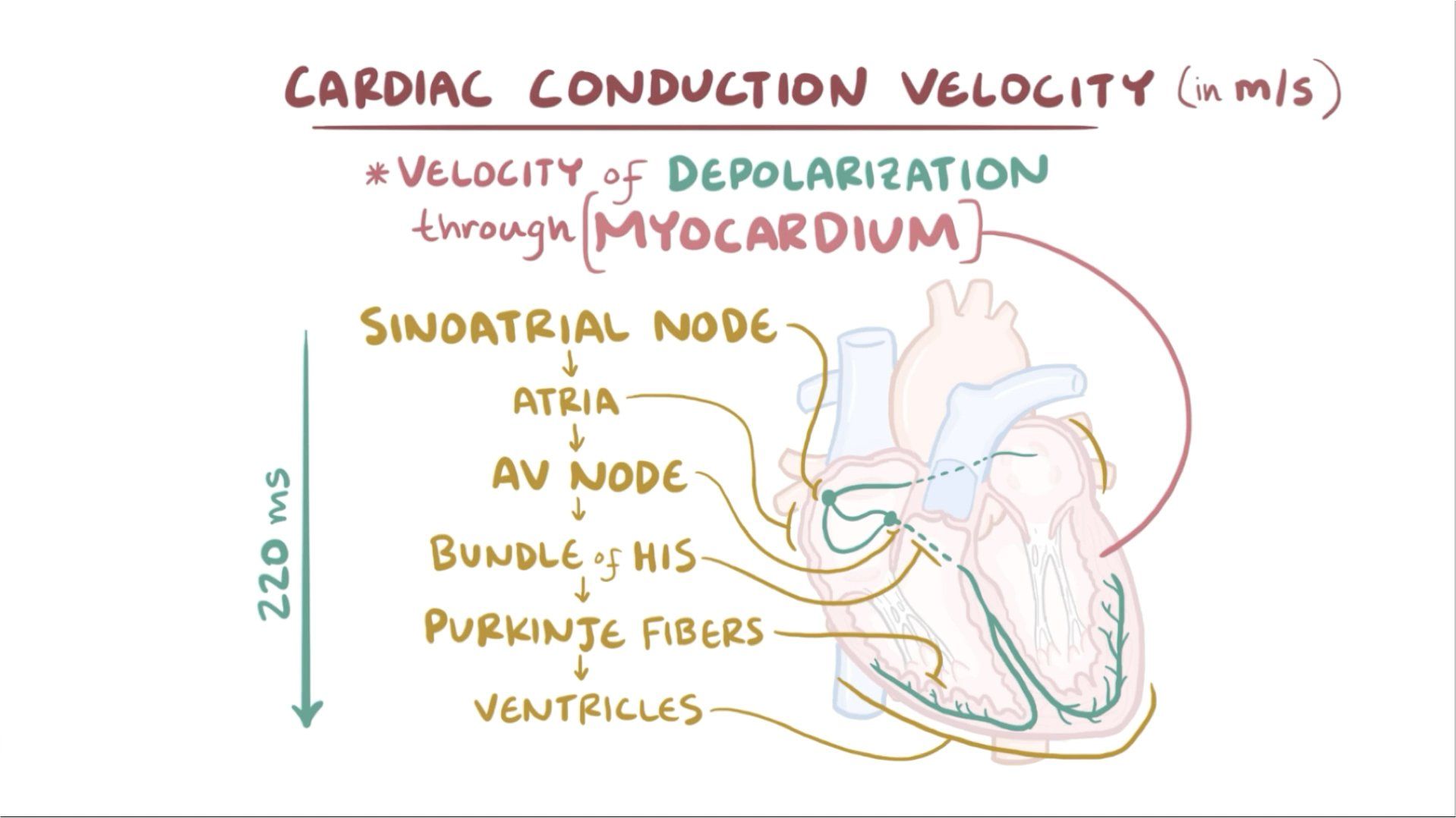
A group of nursing students are studying the conduction system of the heart. The nursing students should recognize that the pacemaker of the heart is known as ____________________
Explanation
The pacemaker of the heart is known as the sinoatrial (SA) node. The SA node is a specialized group of cells located in the right atrium of the heart. It generates electrical impulses that initiate each heartbeat and set the rhythm for the entire heart.
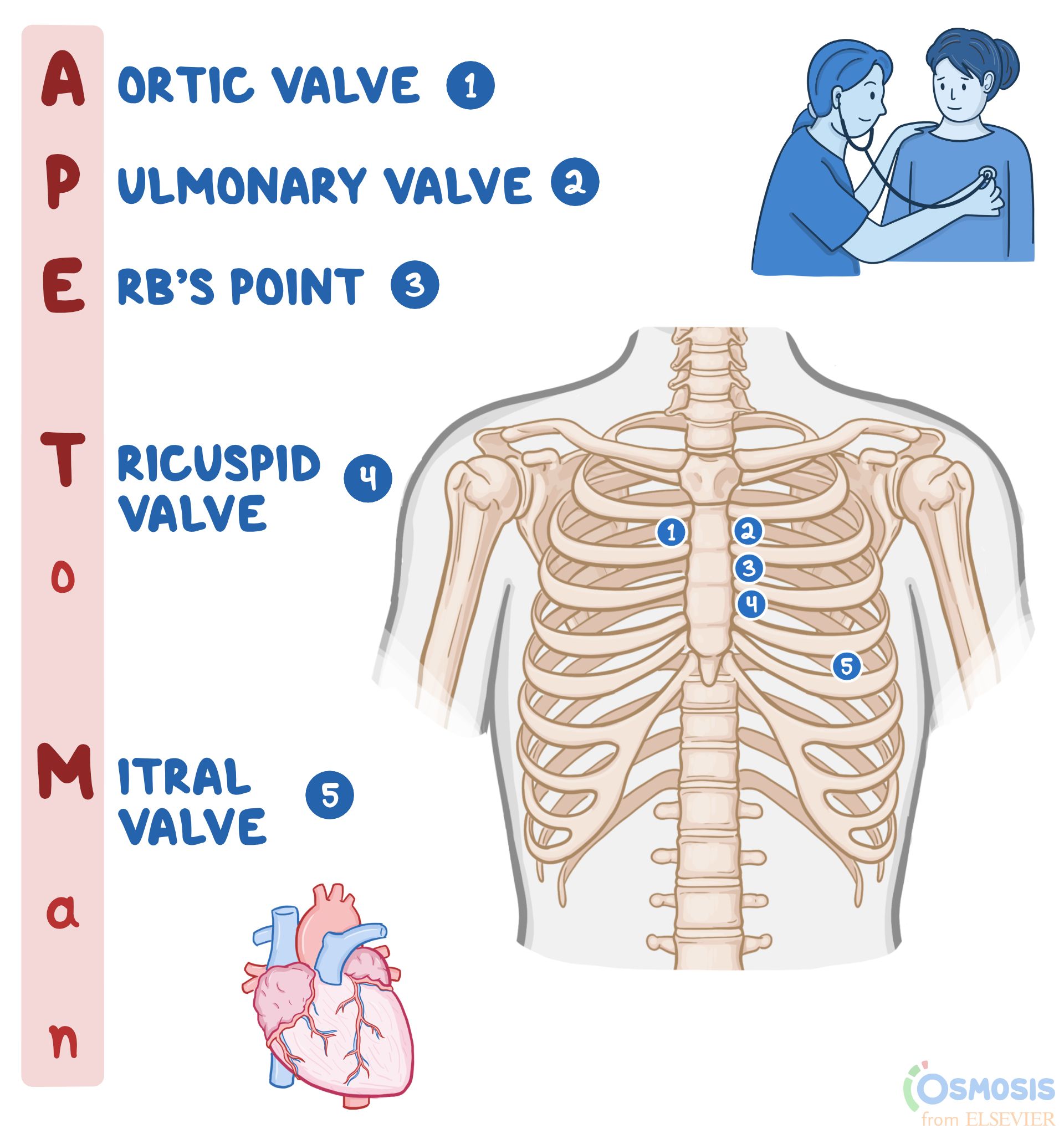
The nurse is assessing the heart sounds of a client. The nurse understands that to listen to the pulmonic valve, the stethoscope should be placed where?
Explanation
A. Fifth intercostal space, left of the midclavicular line: This placement is used to auscultate the mitral valve, which is best heard at the apex of the heart. The mitral valve sounds are typically heard around the fifth intercostal space, midclavicular line.
B. Left lower sternal border: This placement is used to auscultate the tricuspid valve, which is best heard at the lower left sternal border.
C. Second left intercostal space: This is the correct placement for auscultating the pulmonic valve. The pulmonic valve sounds are best heard at the second left intercostal space, which is close to the upper left sternal border.
D. Second right intercostal space: This placement is used to auscultate the aortic valve, which is best heard at the second right intercostal space, close to the upper right sternal border.
The nurse is caring for an older adult client who has recently had a stroke. The nurse assesses that the right side of the client's face is drooping. The nurse might also expect which of the following assessment findings?
Explanation
A. Xerostomia: Xerostomia refers to dry mouth, which is caused by reduced saliva production. While it can be a symptom of various conditions, it is not directly associated with facial drooping after a stroke.
B. Epistaxis: Epistaxis is a medical term for a nosebleed. It occurs due to the rupture of small, delicate blood vessels within the nose. While it can happen independently of a stroke, it is not directly related to facial drooping caused by a stroke.
C. Dysphagia: Dysphagia refers to difficulty in swallowing, which can occur after a stroke due to muscle weakness, including the facial muscles. Facial drooping on one side can be indicative of stroke-related muscle weakness and can contribute to difficulties in swallowing.
D. Rhinorrhea: Rhinorrhea is the medical term for a runny nose, where the nasal cavity is filled with a significant amount of mucus. It is usually caused by various factors such as allergies, infections, or irritants. Rhinorrhea is not directly associated with facial drooping after a stroke.
The nurse is inspecting the anterior chest of an adult client. The nurse recognizes that which of the following should be included in the assessments?
Explanation
. Presence of breath sounds: While assessing the anterior chest, the nurse should listen for breath sounds over various areas of the lungs. However, this is related to auscultation, not inspection.
B. Diaphragmatic excursion: Diaphragmatic excursion involves assessing the movement of the diaphragm during breathing. This is typically done by percussing the level where dullness changes to resonance during inhalation and exhalation. It is more related to percussion, not inspection.
C. Symmetric chest expansion: Symmetric chest expansion refers to the equal expansion of both sides of the chest during inhalation. The nurse can observe and palpate the chest to assess if it expands symmetrically on both sides. This is a crucial aspect of the inspection of the anterior chest.
D. Shape and configuration of the chest wall: The shape and configuration of the chest wall, including abnormalities or deformities, should be assessed during inspection. This includes observing for any asymmetry, deformities, masses, or scars on the anterior chest.
The nurse is performing a breast exam on a client. The client asks the nurse why the left breast is slightly larger than the right breast. Which of the following should be the appropriate response by the nurse?
Explanation
A. A slight asymmetry in breast size can be expected: This response is accurate. It acknowledges the natural variation in breast size that many women experience. It's common for one breast to be slightly larger or shaped differently than the other. It assures the client that this asymmetry is normal and not a cause for concern.
B. Asymmetry of breast size and shape is probably due to breastfeeding and is nothing to worry about: While breastfeeding can cause temporary changes in breast size and shape, not all cases of breast asymmetry are related to breastfeeding. This statement might not cover all situations, making it less accurate.
C. A sudden uneven increase in breast size is normal in adults: This statement is not accurate. Sudden changes in breast size should always be investigated, as they can indicate underlying health issues and may not be considered normal.
D. Breasts should always be symmetric: This statement is not accurate. Perfect symmetry in breast size and shape is rare. Most women have some degree of asymmetry, which is entirely normal. It's important to reassure the client that slight differences are common and not a cause for concern.
The nurse is listening to the heart sounds of a client. The nurse recognizes that the S2:
Explanation
A. Indicates the beginning of diastole: This statement is not accurate. S2, the second heart sound, indicates the end of systole and the beginning of diastole. It is specifically associated with the closure of the aortic and pulmonary valves.
B. Coincides with the carotid artery pulse: This statement is not accurate. S2 is associated with the closure of the aortic and pulmonary valves in the heart, not with the carotid artery pulse.
C. Is louder than an S1: This statement is not accurate. S1, the first heart sound, is usually louder than S2. S1 is associated with the closure of the mitral and tricuspid valves and marks the beginning of systole.
D. Is caused by the closure of the semilunar valves: This statement is accurate. S2 is caused by the closure of the aortic and pulmonary valves, which are the semilunar valves in the heart. It marks the end of systole and the beginning of diastole.

The nurse is doing an assessment of an adult client and noticed unequal chest expansion. The nurse recognizes that unequal chest expansion occurs:
Explanation
A. When part of the lung is obstructed or collapsed: This statement is accurate. Unequal chest expansion can occur when part of the lung is obstructed or collapsed, preventing the affected area from expanding normally during inhalation.
B. When bulging of the intercostal spaces is present: This statement is not accurate. Unequal chest expansion typically refers to decreased expansion on one side, not bulging of intercostal spaces.
C. In an obese patient: This statement is not accurate. Obesity can affect breathing patterns and lung function, but it is not the primary cause of unequal chest expansion.
D. When accessory muscles are used to augment respiratory effort: This statement is not accurate. The use of accessory muscles to augment respiratory effort can be a sign of respiratory distress, but it doesn't directly cause unequal chest expansion. Unequal expansion is more indicative of specific lung conditions or issues with lung mechanics.
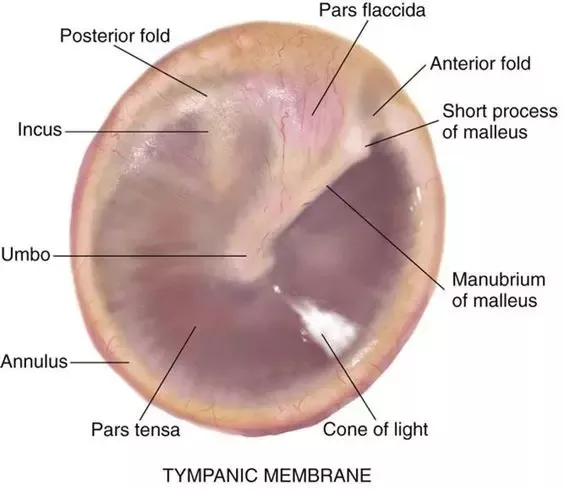
The nurse examines a client's auditory canal and tympanic membrane with an otoscope. The nurse recognizes that which of the following is considered an abnormal finding?
Explanation
A. A shiny, pearly white color tympanic membrane: This is a normal finding. A healthy tympanic membrane often appears shiny and pearly white.
B. The presence of cerumen: This is a normal finding. Cerumen, or earwax, is a natural substance that helps protect the ear canal.
C. The presence of a cone of light: This is a normal finding. The cone of light is a reflection of the otoscope light on the tympanic membrane and is a normal variation.
D. A yellow or amber color to the tympanic membrane: This is considered an abnormal finding. A yellow or amber coloration of the tympanic membrane can indicate the presence of fluid or infection behind the eardrum, which may be a sign of otitis media or other ear conditions.
The nurse is assessing the symmetry of the client's chest. The nurse recognizes that a client's symmetric expansion of the chest is best confirmed by:
Explanation
A. Percussion of the posterior chest: Percussion helps assess the underlying structures of the chest but does not directly confirm symmetric chest expansion.
B. Inspection of the shape and configuration of the chest wall: Inspection is a crucial part of assessing chest symmetry. Any deformities, asymmetry, or abnormalities in the shape and configuration of the chest wall can be visually identified.
C. Placing the palmar surface of the fingers of one hand against the chest and having the client repeat "ninety-nine": This technique, known as tactile fremitus, involves feeling for vibrations or tremors while the client repeats a phrase. While it can provide information about underlying lung conditions, it's not primarily used to confirm symmetric chest expansion.
D. Placing hands sideways on the posterolateral chest wall with thumbs pointing together at the level of T9 or T10: This technique, known as chest expansion measurement, is used to assess symmetric chest expansion. Placing hands in this manner allows the nurse to feel for bilateral chest expansion during inspiration, ensuring that both sides of the chest expand symmetrically.

The nurse is examining an adult client within normal weight limit. The nurse notices that he has bilateral gynecomastia. Which of the following describes the nurse's best course of action?
Explanation
A. Inform the client that his breast enlargement is benign, and normal for a man of his age:
This choice is not appropriate because while gynecomastia can be benign, it should not be assumed without a proper medical evaluation. Gynecomastia can have various causes, including hormonal imbalances or underlying medical conditions. It's crucial to identify the cause through a medical assessment.
B. Explain that this condition may be the result of hormonal changes, and recommend that he see his physician:
This is the correct choice. Gynecomastia can indeed be caused by hormonal changes, but it can also be due to medications, certain health conditions, or hormonal imbalances. Therefore, the nurse should recommend a medical evaluation to determine the underlying cause and appropriate management.
C. Recommend that he alter his diet to include fewer fats and more lean proteins:
This choice is not relevant to gynecomastia. Gynecomastia is not typically caused by dietary factors, so altering the diet would not be a suitable response to this situation.
D. Explain that gynecomastia in men is usually associated with prostate enlargement and recommend that he be thoroughly screened:
This choice is incorrect. Gynecomastia is not directly associated with prostate enlargement. While both conditions can occur in older men, they are distinct medical issues. Screening for prostate enlargement is not indicated based solely on the presence of gynecomastia. Proper evaluation and assessment of each condition are necessary.
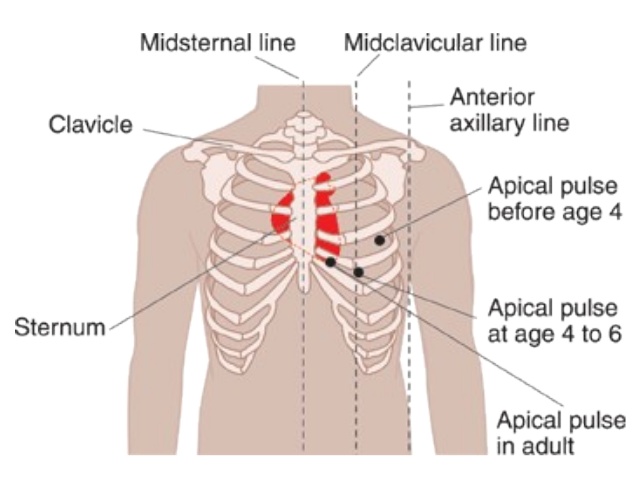
The nurse is preparing to assess the heart rate on an adult female client. The nurse recognizes that the apical pulse can be assessed in an adult female at which of the following anatomical position?
Explanation
A. Fifth left intercostal space at the midclavicular line:
Explanation: The apical pulse, or the point of maximal impulse (PMI), is typically located at the fifth intercostal space at the midclavicular line on the chest. This is the area where the heartbeat is best heard using a stethoscope in most adults.
B. Third left intercostal space at the midclavicular line:
Explanation: This location is too high for the apical pulse. The heart's apex is generally not found at the third intercostal space; it's lower, closer to the fifth intercostal space.
C. Fourth left intercostal space at the sternal border:
Explanation: This location is not the typical site for auscultating the apical pulse. The PMI is usually heard at the midclavicular line, not at the sternal border.
D. Under the left breast at the midclavicular line:
Explanation: This position is not precise enough for auscultating the apical pulse. The specific intercostal space (fifth) and midclavicular line are crucial for accurate assessment.
A client comes into the clinic complaining of facial pain, fever, and malaise. On examination, the nurse notes swollen turbinates and purulent discharge from the nose. The client also complains of dull, throbbing pain in his cheeks and teeth on the right side and pain when the nurse palpates the areas. The nurse recognizes that this client has manifestations of:
Explanation
A. Maxillary sinusitis:
Explanation: The client's symptoms of facial pain, fever, malaise, swollen turbinates, purulent nasal discharge, and dull, throbbing pain in the cheeks and teeth on the right side, especially when palpated, are indicative of maxillary sinusitis. Maxillary sinusitis refers to the inflammation of the maxillary sinuses, which are located in the cheek area. The symptoms described align with a bacterial infection in this sinus.
B. Nasal polyps:
Explanation: Nasal polyps are soft, noncancerous growths on the lining of the nasal passages or sinuses. While they can cause nasal congestion and a runny nose, they do not typically present with the specific symptoms mentioned in the scenario, such as facial pain, fever, and purulent discharge.
C. Frontal sinusitis:
Explanation: Frontal sinusitis involves inflammation of the frontal sinuses located in the forehead area. Symptoms may include forehead pain, headache, and nasal discharge. However, the described symptoms in the scenario (dull, throbbing pain in the cheeks and teeth on the right side) are more characteristic of maxillary sinusitis.
D. Posterior epistaxis:
Explanation: Posterior epistaxis refers to a nosebleed that originates from the back of the nose, often due to bleeding from the sphenopalatine artery. While nosebleeds can cause blood drainage into the throat and result in a metallic taste, the other symptoms described in the scenario, such as facial pain, fever, and purulent discharge, are not indicative of posterior epistaxis.
The nurse is assessing the carotid arteries of a client with cardiovascular disease. What action should be performed next by the nurse?
Explanation
A. Discuss that a light will be directed at the neck to observe for pulsations of the artery:
This choice is incorrect. Directing light at the neck is not a standard method for assessing carotid artery pulsations. The carotid artery is usually assessed by palpation to feel the pulse rather than visual observation.
B. Instruct the client to take a deep breath and "hold" while the nurse briefly auscultates:
This choice is incorrect. Auscultation is typically not used to assess carotid artery pulsations. Palpation (feeling the pulse) is the primary method used for this assessment.
C. Demonstrate that both arteries will be palpated simultaneously to compare amplitude:
This choice is correct. Palpating both carotid arteries simultaneously allows the nurse to compare the amplitude (strength) of the pulses. This comparison helps in assessing the symmetry of the pulses and ensures there are no significant differences between the two sides, which could indicate vascular abnormalities.
D. Show the client the diaphragm of the stethoscope that will be placed on the neck:
This choice is incorrect. The diaphragm of the stethoscope is not typically used for palpating pulses. Palpation involves using the fingertips to feel the pulse and assess its strength and regularity.
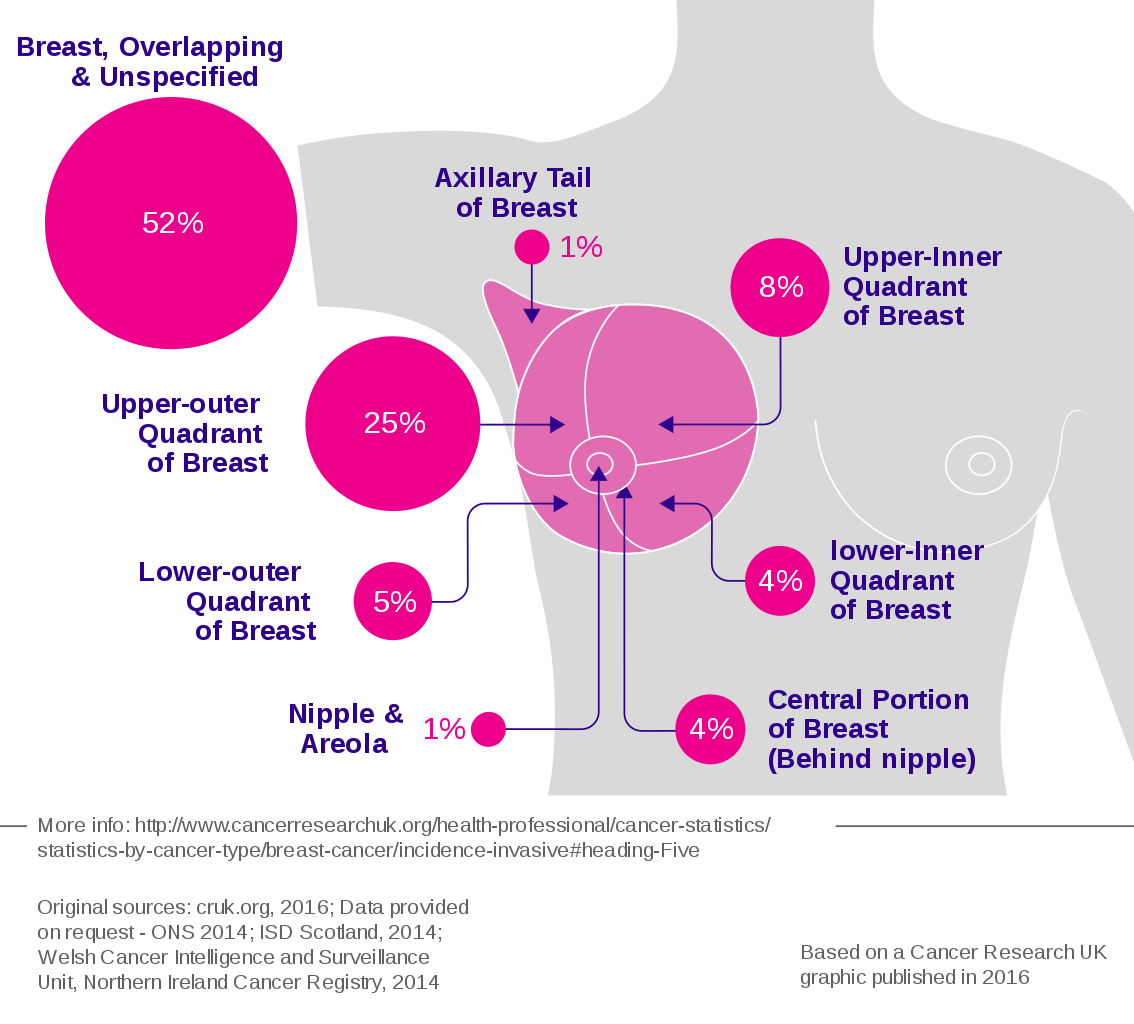
The nurse is performing a breast examination on a client. The nurse understands that examining the upper outer quadrant of the breast is especially important because this part is:
Explanation
A. The location of most breast tumors: This choice is correct. The upper outer quadrant of the breast is the most common site for breast tumors. This area has a higher concentration of glandular tissue, making it more susceptible to the development of tumors. Therefore, thorough examination of this area is crucial during breast examinations.
B. More prone to Injury and calcifications than other locations in the breast: While injuries can occur in any part of the breast, the statement about calcifications is not accurate. Calcifications in breast tissue can occur in various areas and are not specific to the upper outer quadrant.
C. The largest quadrant of the breast: This statement is not accurate. The breast quadrants are not distinguished by size; they are anatomical divisions used for reference during breast examinations. Each quadrant has its significance for examination purposes, but none is considered the largest.
D. Where most of the suspensory ligaments attach: The suspensory ligaments, also known as Cooper's ligaments, provide structural support to the breast tissue. While they are essential for breast anatomy, they are not concentrated in the upper outer quadrant exclusively. These ligaments are distributed throughout the breast tissue.
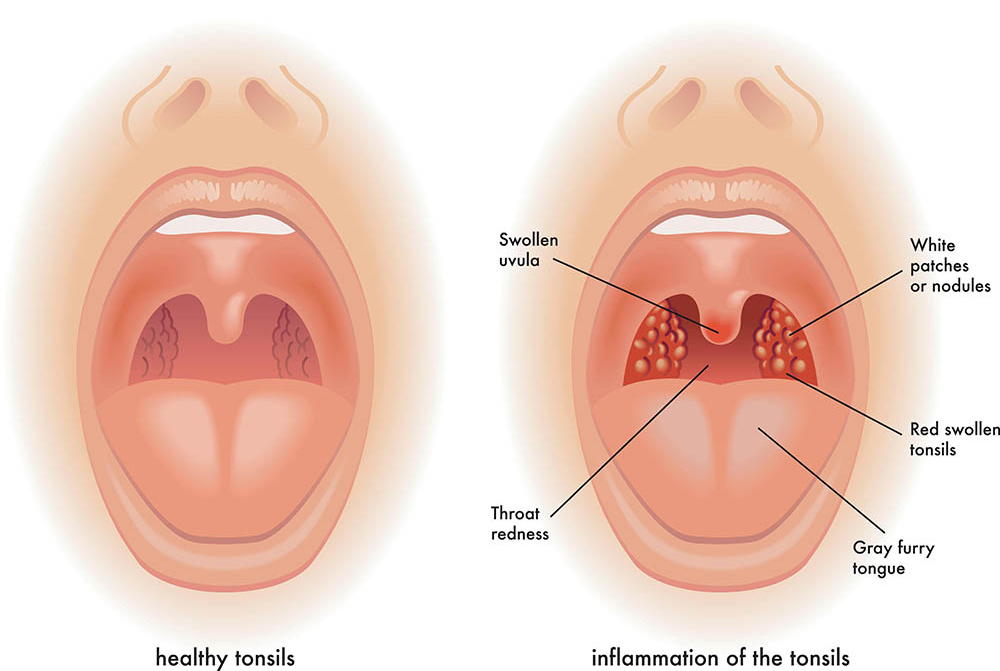
The nurse is assessing the tonsils of an adult client. The nurse notices that the tonsils are involuted, granular in appearance, and has deep crypts. The nurse recognizes that which of the following is the correct response to these findings?
Explanation
A. Continue with the assessment, looking for any other abnormal findings: This is the correct response. Tonsils in adults can have various appearances, and a granular appearance with deep crypts is within the range of normal. It's essential for the nurse to continue the assessment and observe for other signs or symptoms that might indicate an issue.
B. Refer the patient to a throat specialist: Referring the patient based solely on the appearance of the tonsils, especially if it's a normal variant, might be unnecessary and could cause undue concern for the patient. It's important to assess the patient comprehensively before considering a specialist referral.
C. No response is needed; this appearance is normal for the tonsils: This is the correct explanation. In adults, tonsils often appear granular with deep crypts, which is considered a normal variation. No further action is required regarding the tonsils.
D. Obtain a throat culture on the patient for possible streptococcal (strep) infection: Based on the description provided (involution, granular appearance, and deep crypts), there's no specific indication of a streptococcal infection. Conducting a throat culture should be based on the presence of specific symptoms and signs indicative of a streptococcal infection, such as sore throat, fever, and swollen tonsils with white patches, rather than just the appearance of the tonsils.
The nurse is assessing a client diagnosed with fluid overload. The nurse should implement priority interventions for which of the following assessment findings? (Select all that apply.)
Explanation
A. Increased temperature: Fluid overload typically doesn't cause an increased temperature. Infections or other inflammatory processes are more likely causes of elevated body temperature.
B. Increased hematocrit: Fluid overload usually results in dilution of blood components, leading to a decreased hematocrit (lower concentration of red blood cells in the blood). An increased hematocrit is not a typical finding in fluid overload.
C. Blood pressure 180/100: Elevated blood pressure can be associated with fluid overload, especially if the overload is chronic. This is a correct assessment finding that requires intervention and monitoring.
D. Respiratory rate 32: An increased respiratory rate can be a sign of respiratory distress, which may occur in severe cases of fluid overload, especially if it leads to pulmonary edema. This is a correct assessment finding that requires intervention and further evaluation.
E. Heart rate 120 bpm: An increased heart rate can be a compensatory mechanism in response to fluid overload, especially if the heart is trying to maintain cardiac output. However, this heart rate alone is not specific enough to confirm fluid overload. Other signs and symptoms, such as edema, increased blood pressure, and respiratory distress, are more indicative of fluid overload.
The nurse is performing the diagnostic positions test. The nurse recognizes that normal findings from the diagnostic positions test should be which of these results?
Explanation
A. Nystagmus in extreme superior gaze: Nystagmus is an involuntary eye movement and is not a normal finding, especially in extreme superior gaze. Nystagmus can be indicative of neurological issues and requires further evaluation.
B. Slight amount of lid lag when moving the eyes from a superior to an inferior position: Lid lag refers to a delay in the downward movement of the upper eyelid during eye movement. This can be a sign of hyperthyroidism and is not a normal finding.
C. Parallel movement of both eyes: This is the correct answer. During the diagnostic positions test, the nurse should observe parallel movement of both eyes in all directions, indicating normal extraocular muscle function and coordination.
D. Convergence of the eyes: Convergence refers to the inward movement of both eyes when focusing on a close object. While convergence is a normal phenomenon, it is not specifically assessed during the diagnostic positions test, which primarily evaluates the range of motion and coordination of the extraocular muscles.
A client diagnosed with pleuritis has been admitted to the hospital and complains of pain with breathing. Which of the following assessment findings should the nurse expect when auscultating a client with pleuritis?
Explanation
A. Wheezing: Wheezing is a continuous, high-pitched whistling sound usually heard during expiration. It is often associated with narrowed airways, such as in asthma or chronic obstructive pulmonary disease (COPD). Wheezing occurs due to the turbulent airflow through narrowed bronchi or bronchioles and is not typically associated with pleuritis.
B. Friction rub: Pleuritis, or inflammation of the pleura, can cause a friction rub. This sound occurs when the inflamed pleural layers rub against each other during breathing. It's a grating or rubbing sound heard on auscultation and is a hallmark sign of pleuritis.
C. Stridor: Stridor is a high-pitched, harsh sound heard during inspiration and sometimes expiration. It is often a sign of upper airway obstruction, such as in croup or anaphylaxis. Stridor results from turbulent airflow through a partially obstructed or narrowed larynx or trachea.
D. Crackles: Crackles, also known as rales, are brief, discontinuous, popping sounds heard on inspiration. They can be fine or coarse and are often associated with conditions that cause fluid or secretions in the alveoli or small airways, such as pneumonia or heart failure. Crackles are not typically associated with pleuritis.
The nurse is auscultating the lungs of a sleeping client and hears short, popping, crackling breath sounds that stop after a few breaths. The nurse recognizes that these breath sounds are:
Explanation
A. Atelectatic crackles that do not have a pathologic cause:
Atelectatic crackles are short, popping, crackling sounds heard during auscultation. They occur in individuals who are in a supine position and disappear after a few breaths. These crackles are not indicative of any pathological condition; they are common when the lungs are not fully aerated, especially when a person is lying down.
B. Vesicular breath sounds:
Vesicular breath sounds are normal lung sounds heard over the peripheral lung areas. They are soft, low-pitched, and continuous throughout inspiration and part of expiration. Vesicular breath sounds are the typical sounds heard during routine breathing and are not associated with crackling or popping noises.
C. Fine wheezes:
Wheezes are high-pitched whistling sounds heard during expiration. They occur due to narrowed airways and are commonly associated with conditions like asthma or bronchoconstriction. Fine wheezes suggest a partial obstruction in the smaller airways, causing turbulent airflow, leading to the characteristic sound.
D. Fine crackles and may be a sign of pneumonia:
Fine crackles are high-pitched, discontinuous, crackling sounds heard during inspiration. They can occur due to the sudden opening of small airways, and their presence may indicate fluid in the lungs or lung inflammation. Fine crackles are often associated with conditions such as pneumonia, heart failure, or interstitial lung diseases.
A nurse is teaching a client's partner about how to obtain a blood pressure reading. Which of the following actions by the partner indicates a need for further instruction?
Explanation
A. Checks the instrument gauge to ensure the reading starts at zero:
This action is correct. Before taking a blood pressure reading, it's essential to ensure that the instrument's gauge starts at zero. This ensures accurate measurement as the reading reflects the pressure above zero.
B. Centers the cuff bladder over the client's brachial artery:
This action is correct. Proper placement of the blood pressure cuff over the brachial artery is crucial for accurate readings. Centering the cuff ensures that the artery is correctly compressed for measurement.
C. Places the client's arm above the level of the client's heart:
This action is incorrect. Placing the arm above heart level can result in a falsely low blood pressure reading. The arm should be at the same level as the heart to obtain an accurate measurement.
D. Wraps the blood pressure cuff around the client's arm using firm pressure:
This action is correct, but it's important to note that while the cuff should be snug, it should not be too tight or too loose. Wrapping the cuff with firm, even pressure ensures proper compression of the artery for an accurate measurement.
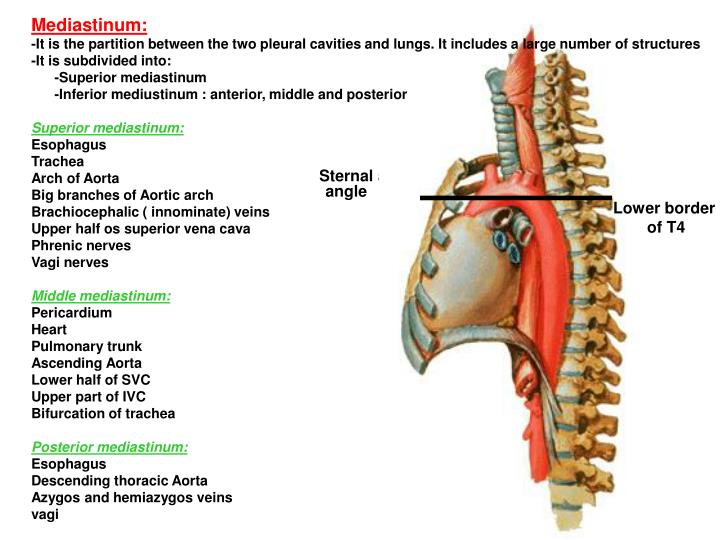
The nurse is doing an examination of a client's anterior thorax. The nurse recognizes that the trachea bifurcates anteriorly at the:
Explanation
A. Xiphoid process:
The xiphoid process is a small, cartilaginous extension at the inferior end of the sternum (breastbone). It does not play a role in the bifurcation of the trachea.
B. Suprasternal notch:
The suprasternal notch, also known as the fossa jugularis sternalis or jugular notch, is the visible dip in the superior part of the manubrium of the sternum between the clavicular notches. It is an important anatomical landmark for assessing the position of the trachea during emergency situations but is not the location of tracheal bifurcation.
C. Sternal angle (Angle of Louis):
The sternal angle, or Angle of Louis, is a palpable notch located at the articulation of the manubrium and the body of the sternum. It is where the second rib attaches and serves as a useful reference point for counting ribs and locating internal structures like the tracheal bifurcation.
D. Costal angle:
The costal angle is the acute angle formed by the junction of the costal margins at the xiphoid process. It is not related to the tracheal bifurcation.
The nurse is preparing to auscultate for heart sounds on a client. Which of the following technique should be used by the nurse?
Explanation
A. Listening for all possible sounds at a time at each specified area: This approach does not allow for specific localization of different heart sounds and murmurs, making it difficult to accurately assess the heart's condition.
B. Listening to the sounds at the aortic, tricuspid, pulmonic, and mitral areas: This option is close but lacks the systematic approach of method D. Listening at specific anatomical locations (aortic, tricuspid, pulmonic, mitral) is important, but the Z pattern allows for thorough coverage and precise localization of any abnormal sounds.
C. Listening to the sounds only at the site where the apical pulse is felt to be the strongest: This method does not cover all the important auscultation sites on the heart and may miss significant findings.
D. Listening by inching the stethoscope in a rough Z pattern, from the base of the heart across and down, then over to the apex: This technique involves a systematic approach where the nurse listens at specific locations in a structured manner, ensuring comprehensive coverage of the heart sounds and murmurs.
The nurse is completing an assessment on a client suspected of having a transient ischemic attack. Which of the following techniques should the nurse use to assess the client's carotid arteries?
Explanation
A. Simultaneously palpating both arteries to compare amplitude: While comparing amplitudes is important, using the diaphragm of the stethoscope to listen for bruits (abnormal whooshing sounds indicating turbulent blood flow) is a more specific and accurate method for assessing the carotid arteries for potential vascular issues.
B. Listening with the diaphragm of the stethoscope to assess for bruits: This technique allows the nurse to detect abnormal sounds (bruits) that could indicate partial blockages or stenosis in the carotid arteries, suggesting a risk of stroke or transient ischemic attack.
C. Instructing the patient to take slow deep breaths during auscultation: Deep breaths are more relevant during lung auscultation. Carotid artery assessment focuses on detecting abnormal sounds and assessing blood flow rather than respiratory patterns.
D. Palpating the artery at the base of the neck: Palpation alone does not provide enough information about potential blockages or abnormalities in the carotid arteries. Listening with a stethoscope allows for a more detailed assessment of blood flow and the presence of bruits.
Sign Up or Login to view all the 46 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

