ATI RN Leadership 2019
Total Questions : 62
Showing 25 questions, Sign in for moreA nurse manager observes an assistive personnel (AP) incorrectly transferring a client to the bedside commode. Which of the following actions should the nurse take first?
Explanation
A. The nurse should first help in patient transfer before insructing the AP to seek assistance when unsure
B. Demonstrating the correct technique is beneficial, but ensuring immediate safety takes precedence.
C. The first action the nurse should take is to help the AP assist the client with the transfer, as this will prevent any harm or injury to the client or the AP
D. Referring to the facility procedure manual doesn't immediately address the incorrect transfer and the potential risk to the client.
A nurse is providing an in-service about client rights for a group of nurses. Which of the following statements should the nurse include in the in- service?
Explanation
A. Restraints should be applied based on a specific, documented need, not on an as- needed (PRN) basis, to ensure client safety.
B. A nurse can disclose information to a family member with the client's permission. This statement respects the client's right to privacy and confidentiality.
C. It is the responsibility of the doctor and not nurses to inform clients about available treatment options.
D. Administering medications without consent for research purposes is ethically unacceptable and violates the client's rights to autonomy and informed consent.
A nurse is preparing to discharge a client who has end-stage heart failure. The client's partner tells the nurse she can no longer handle caring for the client. Which of the following actions should the nurse take?
Explanation
A. Contacting the case manager is crucial to explore various discharge options and ensure the client's needs are met appropriately.
B. Recommending long-term care should be considered after exploring other options and assessing the client's specific needs.
C. Requesting assistance from another family member is a potential option but should be explored in conjunction with other solutions.
D. Delaying discharge might not address the partner's inability to provide care and doesn't explore alternative solutions.
A nurse in the emergency department is assessing a client who is unconscious following a motor-vehicle crash. The client requires immediate surgery. Which of the following actions should the nurse take?
Explanation
A. Telephone consent from the facility administrator might not be sufficient for the specific informed consent required for surgery on an unconscious client.
B. Delaying surgery to ensure proper informed consent is obtained is essential to respect the client's autonomy and rights.
C. Asking the anesthesiologist to sign the consent is not appropriate as the responsibility for obtaining informed consent typically lies with the surgeon or responsible provider.
D. Transporting the client to the operating room without verified informed consent violates the client's rights and could lead to ethical and legal issues.
A nurse is assessing an older adult client who was brought to the emergency department by his adult son, who reports that the client fell at home. The nurse suspects elder abuse. Which of the following actions should the nurse take?
Explanation
A. Asking the client's son to go to the waiting area allows the nurse to have a private conversation with the client, which is crucial in suspected cases of elder abuse to gather information without potential interference or intimidation.
B. Asking about injuries with the son present might hinder the client from disclosing information due to fear or pressure.
C. Treating and discharging the client without addressing the suspected elder abuse could potentially put the client in further danger.
D. Filing an incident report might be necessary but should follow an assessment and investigation of the situation.
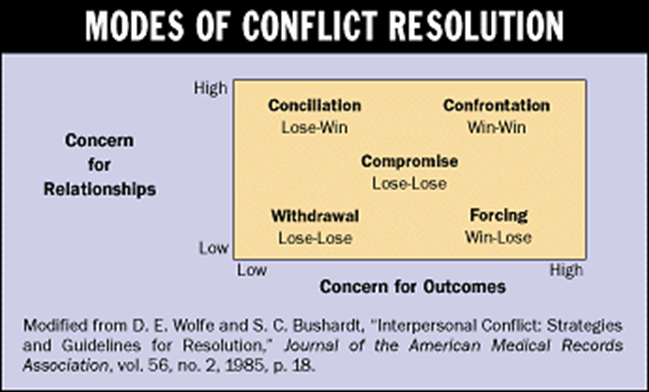
To resolve a conflict between staff members regarding potential changes in policy, a nurse manager decides to implement the changes she prefers regardless of the feelings of those who oppose those changes. Which of the following conflict resolution strategies is the nurse manager using?
Explanation
A. Cooperating involves finding a middle ground and working together, which isn't reflected in the manager's unilateral decision-making.
B. Collaborating involves working together toward a solution that accommodates various perspectives, which isn't the case here.
C. Competing involves asserting one's own concerns at the expense of others' viewpoints, which aligns with the manager's decision to implement changes regardless of opposition.
D. Compromising entails finding a middle ground that satisfies all parties involved, which isn't evident in the manager's decision-making process.
A nurse is preparing a client for an elective mastectomy. The client is wearing a plain gold wedding band. Which of the following is an appropriate procedure for taking care of this client's ring?
Explanation
A. Placing the client's ring in the facility safe might not be necessary and could cause anxiety for the client about the ring's safety.
B. Placing the ring in the bag with the client's clothing ensures it remains safe and with the client's belongings during the surgery.
C. Taping the ring to the client's finger is not advisable as it could cause circulation issues or discomfort.
D. Agreeing to keep the ring for the client might lead to misplacement or loss during the surgical process.
A nurse is preparing to complete an incident report regarding a medication error. Which of the following actions should the nurse plan to take? (Select all that apply.)
Explanation
A. Identify the medication name and dosage administered to the client in the report: Providing specific details about the medication involved is crucial for accurately documenting the incident.
B. Making a copy of the incident report for personal record keeping: While keeping a personal copy might seem practical, the official incident report should be filed according to institutional policies. Personal record keeping might not align with these policies.
C. Include the time the medication error occurred in the report: Documenting the time helps in understanding the sequence of events and aids in investigating the error.
D. Obtaining an order from the client's provider to complete the report: Typically, healthcare providers do not need to issue an order for a nurse to complete an incident report; it's part of the facility's standard reporting process.
E. Place a copy of the completed report in the client's medical record: Ensuring that the incident report is part of the client's medical record is important for maintaining a comprehensive history and allowing for future reference.
A nurse is conducting a disaster preparedness drill with a group of nurses who are orienting to the facility. Which of the following triage tag colors should the nurse instruct the group to apply to a client who has full-thickness burns on 72% of his body?
Explanation
A. Black tags are typically used for individuals who are deceased or expected to die imminently.
B. Yellow tags are used for those who require observation but are not in immediate danger.
C. Red tags are for those with severe injuries who require immediate treatment but have a chance of survival.
D. Green tags are used for individuals with minor injuries or those who require minimal medical assistance.
A nurse is preparing a client for surgery. The client has signed the consent form but tells the nurse that she has reconsidered because she is worried about the pain. Which of the following responses by the nurse is appropriate?
Explanation
A. Dismissing the client's concerns and suggesting pain medication without addressing the client's worries isn't an empathetic or helpful response.
B. Asking why the client didn't discuss concerns with the provider might make the client feel guilty or judged for their decision.
C. Pressuring the client by suggesting avoiding future pain and disability isn't respectful of the client's current concerns and decision-making.
D. Acknowledging the client's worries and affirming their ability to change their mind is an appropriate and supportive response.
A nurse is comparing the rate of medication errors on the medical unit to the rate from a medical unit in a magnet hospital. Which of the following quality improvement methods is the nurse using?
Explanation
A. Root cause analysis involves investigating errors to determine underlying causes and preventive measures.
B. Risk benefit analysis weighs the potential risks and benefits of a particular action or decision.
C. Structure audit evaluates the infrastructure and resources in place but doesn't involve comparison between different units.
D. Benchmarking involves comparing performance metrics to those of other organizations or units to identify best practices and areas for improvement, as in comparing medication error rates between units in different hospitals.
A nurse is preparing a teaching session with a client who speaks a different language than the nurse. Which of the following interventions should the nurse plan to include?
Explanation
A. Gestures and hand signals can be helpful but might not fully convey complex medical information.
B. Involving the client's partner can be beneficial but might not ensure accurate communication and understanding.
C. Interpreting body language is essential for communication but might not suffice for comprehensive teaching.
D. Providing an interpreter ensures accurate and complete communication during the teaching session, facilitating understanding and informed consent.
A nurse at a long-term care facility is planning a fall prevention program for the residents. Which of the following interventions should the nurse include?
Explanation
A. Keeping all four side rails up on beds can increase the risk of entrapment or injury and isn't recommended as a fall prevention strategy.
B. Instituting regular rounds during the day to offer toileting helps prevent falls related to residents attempting to get to the bathroom independently.
C. Accompanying older residents during ambulation is helpful but might not be feasible at all times and for all residents.
D. Using vest restraints can lead to physical and psychological complications and is not recommended due to ethical and safety concerns.
A nurse is receiving a verbal prescription from the provider for a client who is having increased pain. The nurse should transcribe which of the following prescriptions in the client's medical record?
Explanation
A. "MSO4 10 mg IVP q4° prn for pain" lacks clarity in abbreviation and dosing instructions.
B. "MS 10 mg IV every 4 pm for pain" contains an unclear frequency and timing.
C. "Morphine sulfate 10 mg IV q4h IV pm for pain" contains redundant dosing information and unclear timing.
D. "Morphine sulfate 10.0 mg every 4 hours IV prn for pain" provides clear and appropriate information regarding medication, dosage, route, frequency, and indication.

A nurse is assessing a client who has meningitis. Which of the following findings should the nurse report to the provider immediately?
Explanation
A. A generalized rash over the trunk might indicate various conditions but might not be an immediate concern in the context of meningitis.
B. An increased temperature is an expected finding in meningitis and should be
monitored but might not necessitate immediate reporting unless exceptionally high or coupled with other concerning symptoms.
C. Photophobia, or sensitivity to light, is a common symptom in meningitis but alone might not necessitate immediate reporting if the client's other symptoms are stable.
D. Decreased level of consciousness can indicate neurological deterioration and requires immediate attention as it could signal worsening of the client's condition.
A nurse is supervising an assistive personnel (AP) who is feeding a client who has dysphagia.Which of the following actions by the AP should the nurse identify as correct technique?
Explanation
A. Providing a rest period prior to meals might be beneficial for some individuals but isn't directly related to correct feeding technique for someone with dysphagia.
B. Elevating the head of the client's bed to 30° during mealtime helps prevent aspiration and promotes safer swallowing for someone with dysphagia.
C. Withholding fluids until the end of the meal is not appropriate as it can increase the risk of aspiration and dehydration.
D. Instructing the client to place her chin toward her chest when swallowing is not a recommended technique for someone with dysphagia as it can increase the risk of
A nurse in the emergency department is performing triage for a group of clients who were in a train crash. Which of the following clients should the nurse tag as emergent?
Explanation
A. A client with an open fracture of the femur requires immediate attention due to the risk of severe bleeding, infection, and potential damage to surrounding structures.
B. Periorbital ecchymosis (bruising around the eyes) might indicate facial trauma but may not immediately threaten life or limb.
C. A deep partial thickness burn on the lower extremities is serious but might not be immediately life-threatening.
D. An asymmetrical thorax could indicate various injuries, but the severity and immediate threat to life can vary widely based on the underlying cause.
A nurse is caring for a client who has a prescription for transcutaneous electrical nerve stimulation (TENS). Which of the following members of the interdisciplinary team should the nurse contact for assistance?
Explanation
A. A physical therapist can assist with the proper application and usage of transcutaneous electrical nerve stimulation (TENS) for pain management, providing guidance on its use and techniques for optimal outcomes.
B. Occupational therapists focus more on functional activities related to daily living.
C. Respiratory therapists specialize in respiratory care.
D. Pharmacists primarily handle medication-related concerns and may not specifically assist with TENS therapy.
A nurse in a prenatal clinic is caring for a group of clients. Which of the following clients should the nurse recommend for an interdisciplinary care conference?
Explanation
A. A client at 39 weeks of gestation with a negative contraction stress test is at term and might not require an interdisciplinary care conference if the test results are normal.
B. A client at 35 weeks of gestation with a biophysical profile of 6 might need further evaluation or interventions, making it appropriate to discuss the case in an
interdisciplinary care conference.
C. A client at 37 weeks of gestation with a specific US ratio might require attention, but the significance of the ratio in this context is unclear without additional information.
D. A client at 28 weeks of gestation with a negative Coombs' titer might not require an interdisciplinary care conference solely based on this information.
A nurse is caring for a client who reports acute pain but refuses IM medication. The nurse distracts the client and quickly administers the injection. This illustrates which of the following?
Explanation
A. Battery involves unauthorized or harmful physical contact, which administering the injection without consent would constitute.
B. False imprisonment involves restricting a person's freedom of movement unlawfully, which doesn't apply in this scenario.
C. Assault involves the threat of unwanted or harmful contact, and proceeding with the injection after the client refused constitutes assault.
D. Libel refers to written defamation or false statements that damage someone's reputation, which is not relevant in this situation involving administering medication.
A nurse is orienting a newly licensed nurse about client confidentiality. Which of the following statements by the newly licensed nurse indicates an understanding of the teaching?
Explanation
A. Posting a client's vital signs in their room violates their confidentiality by making private health information publicly accessible.
B. Discarding personal health information documents in the trash can expose sensitive information and is not a secure method of disposal.
C. Using another nurse's password compromises security and individual accountability, leading to potential breaches of confidentiality.
D. Encrypting personal health information when sending emails demonstrates an understanding of the importance of protecting sensitive client data during electronic communication.
A nurse manager is leading a discussion about ethical dilemmas. Which of the following situations should the nurse manager include as an example of an ethical dilemma?
Explanation
A. A client receiving an operation on the wrong side of the body is a serious medical error but might not inherently involve an ethical dilemma unless the decision-making process and accountability are in question.
B. A parent wanting a 14-year-old adolescent to receive radiation treatment against his will involves conflicting values of autonomy, beneficence, and parental rights,
constituting an ethical dilemma.
C. A visitor experiencing a minor burn is an incident but doesn't inherently pose an ethical dilemma.
D. A nurse witnessing another nurse administering an incorrect medication is a patient safety issue but might not inherently involve an ethical dilemma unless there are questions about reporting or intervening in the situation.
A charge nurse is making staff assignments on a medical-surgical unit. Which of the following tasks should the nurse plan to delegate to an assistive personnel?
Explanation
A. Pouching a client's ostomy bag for a new colostomy requires specialized training and should typically be performed by a nurse.
B. Performing nasal hygiene for a client with an NG tube involves basic hygiene tasks that can be safely delegated to an assistive personnel after proper training and supervision.
C. Measuring oxygen saturation for a client who has dyspnea requires a basic skill that can be delegated to an assistive personnel.
D. Inserting a rectal suppository for a vomiting client involves a nursing task that should be performed by a nurse due to the client's condition and the nature of the task.
A case manager is preparing a discharge plan for a client following coronary artery bypass grafting surgery. Which of the following client issues should the nurse address first?
Explanation
A. Inadequate food supply is important but might not be the most immediate concern following coronary artery bypass grafting surgery.
B. Limited social support is significant for the client's recovery but might not directly impact the immediate post-operative care.
C. Low pain tolerance after a major surgery like coronary artery bypass grafting can impede recovery, affect mobility, and hinder the client's ability to participate in rehabilitation exercises or manage post-operative pain effectively. Addressing pain
tolerance is crucial for post-operative recovery.
D. Decreased self-esteem, while important for the client's overall well-being, might not be an immediate priority in the early stages following surgery compared to managing physical recovery and pain tolerance.
A nurse is assisting with the orientation of a newly licensed nurse. The newly licensed nurse is having trouble focusing and has difficulty completing care for his assigned clients. Which of the following interventions is appropriate?
Explanation
A. Recommending that the newly licensed nurse take time to plan at the beginning of the shift can help improve focus and organization, allowing for better task completion.
B. Offering to take over care while he takes a break might provide immediate relief but doesn't address the underlying issue of focus and task completion.
C. Advising to complete less time-consuming tasks first might not necessarily address the root cause of the difficulty in focusing.
D. Asking other staff members to take over tasks doesn't encourage skill development or help the newly licensed nurse develop coping strategies for focus and task completion.
Sign Up or Login to view all the 62 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

