ATI RN maternal newborn 2019 with NGN Updated 2024 - Exam 2
Total Questions : 62
Showing 25 questions, Sign in for moreA nurse is assessing a client who is at 12 weeks of gestation. The nurse should report which of the following findings to the provider as an indication of an imminent spontaneous abortion?
Explanation
A spontaneous abortion (also called a miscarriage) is the unexpected ending of a pregnancy in the first 20 weeks of gestation. The major symptoms of a spontaneous abortion are abdominal cramps and bleeding from the vagina, sometimes with clots and/or bits of tissue³. A dilated cervix indicates that abortion is inevitable¹. Other symptoms may include low back ache, a decrease in pregnancy symptoms, and leaking amniotic fluid.
The other options are not answers because they are not indicative of an imminent spontaneous abortion.
b. Slight abdominal cramps
Slight abdominal cramps are a common symptom of early pregnancy and do not necessarily mean that a miscarriage is happening. However, if the cramps are severe, persistent, or accompanied by bleeding, then they could be a sign of a problem and should be reported to the provider.
c. Elevated hCG
hCG (human chorionic gonadotropin) is a hormone produced by the placenta during pregnancy. It can be measured in the blood or urine to confirm pregnancy or monitor its progress. Elevated hCG levels are not a sign of a spontaneous abortion, but rather a normal finding in early pregnancy. In fact, low or decreasing hCG levels may indicate a miscarriage or an ectopic pregnancy.
d. Scant bright red spotting
Scant bright red spotting is another common symptom of early pregnancy and does not necessarily mean that a miscarriage is happening. It may be caused by implantation bleeding, cervical irritation, or sexual intercourse. However, if the spotting is heavy, dark, or accompanied by cramps or pain, then it could be a sign of a problem and should be reported to the provider.
A nurse is caring for a client who is in active labor. The nurse administers butorphanol IV bolus for pain. Which of the following findings should the nurse report to the provider following this medication?
Explanation
This is the finding that the nurse should report to the provider following this medication. Butorphanol is an opioid analgesic that can cause respiratory depression as a serious side effect¹. A normal respiratory rate for an adult is 12 to 20 breaths per minute². A respiratory rate of 10/min is below the normal range and could indicate inadequate ventilation and oxygenation. The nurse should monitor the client's oxygen saturation, administer oxygen if needed, and notify the provider of this finding.
The other options are not correct because they are not signs of adverse effects from butorphanol. Let me
explain why:
a) Urinary Output 1 20 mL in 2 hr
This is a normal urinary output for an adult. A normal urinary output is 0.5 to 1 mL/kg/hr³. Assuming an average weight of 70 kg, this would be 35 to 70 mL/hr, or 70 to 140 mL in 2 hr. Therefore, a urinary output of 120 mL in 2 hr is within the normal range and does not need to be reported.
c) Moderate fetal heart rate variability
This is a reassuring sign of fetal well-being. Fetal heart rate variability is the amount of fluctuation in the fetal heart rate from the baseline. Moderate variability is defined as a fluctuation of 6 to 25 beats per minute (bpm) and indicates that the fetus is responsive and has adequate oxygenation⁴. Moderate variability does not need to be reported.
d) Blood pressure 136/88 mm Hg
This is a slightly elevated blood pressure, but not a sign of an adverse effect from butorphanol. Butorphanol does not cause significant changes in blood pressure¹. A normal blood pressure for an adult is less than 120/80 mm Hg⁵. A blood pressure of 136/88 mm Hg is considered elevated, but not hypertensive. The nurse should monitor the client's blood pressure and check for other signs of preeclampsia, such as proteinuria, headache, or visual changes. However, this finding does not need to be reported immediately.
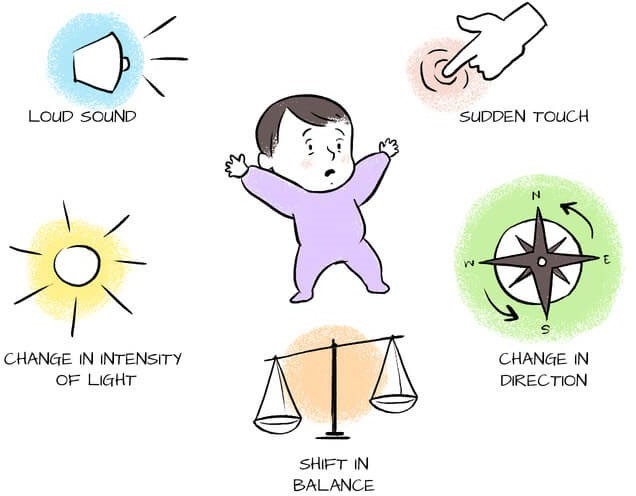
A nurse is assessing the reflexes of a term newborn. After placing the newborn in the supine position, which of the following methods should the nurse use to elicit the Moro reflex?
Explanation
This is the method that the nurse should use to elicit the Moro reflex. The Moro reflex, or startle reflex, is an involuntary motor response that infants develop shortly after birth. It is a response to a sudden loss of support or extremely sudden stimulation¹. A loud noise above the newborn can trigger the Moro reflex by startling the infant. The Moro reflex involves three distinct components: spreading out the arms (abduction), pulling the arms in (adduction), and crying (usually)².
The other options are not correct because they do not elicit the Moro reflex.
a) Turn the newborn's head to one side.
This does not elicit the Moro reflex, but rather the tonic neck reflex. The tonic neck reflex occurs when the infant turns their head to one side and assumes a "fencing" posture, with the arm and leg on the same side extended and the opposite arm and leg flexed.
b) Touch the newborn's cheek with a finger.
This does not elicit the Moro reflex, but rather the rooting reflex. The rooting reflex occurs when the infant turns their head and opens their mouth in response to a touch on their cheek or mouth. This reflex helps the infant locate and latch onto a nipple for feeding³.
d) Tap the newborn's forehead with a finger.
This does not elicit the Moro reflex, but rather the glabellar reflex. The glabellar reflex occurs when the infant blinks in response to a tap on their forehead or bridge of their nose. This reflex helps protect the eyes from injury³.
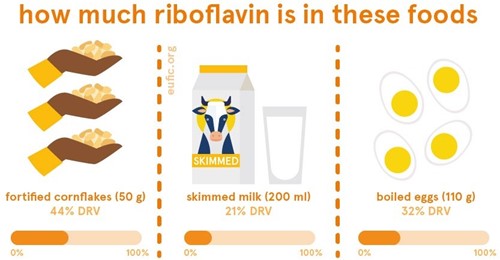
A nurse is providing prenatal teaching to a client who practices a vegan diet and is trying to increase intake of vitamin B2. Which of the following foods should the nurse recommend?
Explanation
This is the food that the nurse should recommend to the client who practices a vegan diet and is trying to increase intake of vitamin B2. Vitamin B2, also known as riboflavin, is an essential nutrient that is involved in energy metabolism, growth, and cell function¹. It is found in small amounts in a variety of plant foods, such as avocados, mushrooms, almonds, leafy green vegetables, and soybeans³. However, some of the best sources of riboflavin are animal products, such as dairy products and eggs¹. Therefore, vegans may need to consume fortified foods or supplements to meet their daily requirements of riboflavin.
Fortified soy milk is a good option for vegans because it contains added riboflavin, as well as other nutrients such as calcium, vitamin B12, and vitamin D. One cup of fortified soy milk can provide about 0.5 milligrams of riboflavin, which is about 45% of the recommended daily amount for women and 38% for men⁴. Other fortified vegan foods that may contain riboflavin include breakfast cereals, nutritional yeast, and plant- based meat alternatives²⁵.
The other options are not correct because they are not good sources of riboflavin.
a) Raw carrots
Raw carrots are a healthy vegetable that provide vitamin A, fiber, and antioxidants. However, they are not a good source of riboflavin. One medium carrot contains only 0.02 milligrams of riboflavin, which is less than 2% of the recommended daily amount⁴.
b) Fresh citrus fruits
Fresh citrus fruits are a great source of vitamin C, folate, and potassium. However, they are not a good source of riboflavin. One medium orange contains only 0.04 milligrams of riboflavin, which is about 4% of the recommended daily amount⁴.
c) Brown rice
Brown rice is a whole grain that provides complex carbohydrates, fiber, and minerals. However, it is not a good source of riboflavin. One cup of cooked brown rice contains only 0.05 milligrams of riboflavin, which is about 5% of the recommended daily amount⁴.
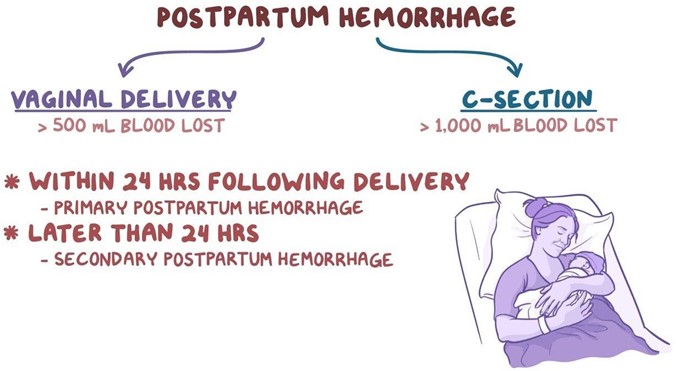
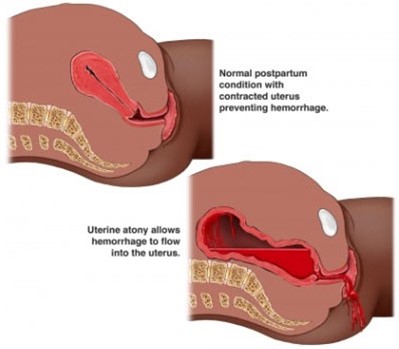
A nurse is reviewing the medical record of a client who had a vaginal delivery 3 hr ago. Which of the following findings place the client at risk for postpartum hemorrhage? (Select all that apply.)
Explanation
These are the findings that place the client at risk for postpartum hemorrhage. Postpartum hemorrhage (PPH) is severe vaginal bleeding after childbirth. It can be a life-threatening condition that requires prompt treatment. The most common cause of PPH is uterine atony, which is when the uterus does not contract enough to stop the bleeding from the placental site¹. Factors that can increase the risk of uterine atony include:
- History of uterine atony: Having a previous episode of PPH due to uterine atony makes it more likely to
happen again in subsequent deliveries.
- Labor induction with oxytocin: Oxytocin is a hormone that stimulates uterine contractions. However, prolonged or excessive use of oxytocin during labor can cause uterine fatigue and reduce its ability to contract after delivery.
- Vacuum-assisted delivery: A vacuum extractor is a device that helps deliver the baby by applying suction to the baby's head. This can cause trauma to the uterus and increase the risk of bleeding.
The other options are not correct because they are not risk factors for postpartum hemorrhage. Let me
explain why:
b) History of human papillomavirus
Human papillomavirus (HPV) is a common sexually transmited infection that can cause genital warts and cervical cancer. However, it does not increase the risk of postpartum hemorrhage. HPV may affect the cervix, but not the uterus or the placenta, which are the main sources of bleeding after delivery³.
c) Newborn weight 2.948 kg (6 Ib 8 oz)
This is a normal newborn weight and does not increase the risk of postpartum hemorrhage. A large baby (more than 4 kg or 8.8 Ib) may increase the risk of uterine atony by overdistending the uterus, but this is not the case for this newborn².
A nurse is assessing a full-term newborn upon admission to the nursery. Which of the following clinical findings should the nurse report to the provider?
Explanation
This is the clinical finding that the nurse should report to the provider following this medication. Rust- stained urine is a sign of urate crystals in the newborn's urine, which can indicate dehydration or inadequate fluid intake⁷. Urate crystals are made of uric acid, a waste product that is excreted in urine. They can cause a pink or red-orange stain in the diaper, which can be mistaken for blood⁷. Urate crystals are common in the first few days after birth, especially in breastfed babies who may not be getting enough milk⁷. However, if they persist or are accompanied by other signs of dehydration, such as decreased saliva, dry lips, lethargy, or reduced wet diapers, they should be reported to the provider⁷. The nurse should also monitor the baby's weight and feeding paterns and encourage the mother to breastfeed frequently or offer formula if needed.
The other options are not correct because they are not signs of an adverse effect from butorphanol. Let me
explain why:
a) Single palmar creases
Single palmar creases are single lines that cross the palm of the hand, formed by the fusion of two normal creases¹. They are present in about 1 out of 30 people, more often in males than females¹. They are usually harmless and do not affect the function of the hand¹. However, they may be associated with some genetic or developmental disorders, such as Down syndrome, fetal alcohol syndrome, or Aarskog syndrome¹³.
Therefore, the nurse should examine the baby for any other physical anomalies or signs of chromosomal abnormalities and refer them to a geneticist if needed.
c) Subconjunctival hemorrhage
Subconjunctival hemorrhage is a burst blood vessel in the white of the eye, causing a bright red spot on the eye[^10^]. It is usually painless and does not affect vision[^10^]. It is very common in newborns after a traumatic delivery, especially when forceps or vacuum extraction are used[^10^] ¹²¹⁴. It is usually benign and resolves on its own within 1-2 weeks[^10^]. The nurse should reassure the parents and monitor the baby for any signs of infection or bleeding disorders.
d) Transient circumoral cyanosis
Transient circumoral cyanosis is a blue discoloration around the mouth only, caused by low levels of oxygen in the blood vessels near the skin surface¹⁵. It is often seen in infants during the first few days after birth or when they are exposed to cold temperatures¹⁵. It is usually normal and harmless and goes away once they warm up¹⁵. However, if the cyanosis affects other parts of the face or body, such as the lips or tongue, it could be a sign of a serious lung or heart problem and should be reported immediately¹⁵. The nurse should check the baby's oxygen saturation, heart rate, and respiratory rate and look for any signs of distress.

A nurse is preparing to administer gentamicin 2 mg/kg IM to a client who has pelvic inflammatory disease and weighs 132 lb. Available is gentamicin injection 40 mg/mL. How many mL should the nurse administer?
(Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
Use the following formula to calculate the amount of gentamicin to administer:
Volume (mL) = Dose (mg) / Concentration (mg/mL)
First, I need to convert the client's weight from pounds to kilograms. One pound is equal to 0.4536 kilograms. Therefore, 132 lb is equal to 132 x 0.4536 = 59.8752 kg.
Next, I need to multiply the client's weight by the prescribed dose of gentamicin per kilogram. The prescribed dose is 2 mg/kg, so the total dose is 2 x 59.8752 = 119.7504 mg.
Finally, I need to divide the total dose by the concentration of gentamicin in the injection. The concentration is 40 mg/mL, so the volume is 119.7504 / 40 = 2.99376 mL.
To round the answer to the nearest whole number, I need to look at the first decimal place. If it is 5 or more, I round up; if it is less than 5, I round down. In this case, the first decimal place is 9, which is more than 5, so I round up. Therefore, the final answer is 3 mL.
The nurse should administer 3 mL of gentamicin injection to the client.
A nurse is caring for a client who is in active labor and is receiving oxytocin via IV infusion. The nurse has applied an internal fetal heart monitor and recognizes an early deceleration of the fetal heart rate tracing. Which of the following actions should the nurse take?
Explanation
This is the action that the nurse should take after recognizing an early deceleration of the fetal heart rate tracing. Early decelerations are symmetrical decreases and return-to-normal linked to uterine contractions¹. The decrease in heart rate occurs gradually, and the nadir of the deceleration occurs at the same time as the peak of the uterine contraction³. Early decelerations are caused by compression of the fetus's head during a uterine contraction, which can stimulate the vagus nerve and cause a decrease in the fetal heart rate⁴. Early decelerations are nothing to be alarmed about¹. They are considered normal and benign, as they do not affect fetal oxygenation or well-being³. Therefore, the nurse should continue to monitor the client and the fetal heart rate tracing and document the findings.
The other options are not correct because they are not appropriate actions for early decelerations.
a) Assist the client to lay on her right side.
This is not an appropriate action for early decelerations, as they are not caused by maternal position or uteroplacental insufficiency. Changing the maternal position may help improve fetal oxygenation and blood flow in cases of late or variable decelerations, which are signs of fetal distress¹. However, early decelerations do not indicate fetal distress and do not require any intervention.
c) Discontinue the oxytocin.
This is not an appropriate action for early decelerations, as they are not caused by oxytocin administration or uterine hyperstimulation. Oxytocin is a hormone that stimulates uterine contractions and can be used to induce or augment labor. However, excessive or prolonged use of oxytocin can cause uterine fatigue and reduce its ability to contract after delivery, leading to uterine atony and postpartum hemorrhage². Oxytocin can also cause late or variable decelerations, which are signs of fetal distress¹. However, early decelerations do not indicate fetal distress and do not require any intervention.
d) Administer oxygen at 8 L/min per mask.
This is not an appropriate action for early decelerations, as they are not caused by fetal hypoxia or acidosis. Oxygen administration may help improve fetal oxygenation and blood flow in cases of late or variable decelerations, which are signs of fetal distress¹. However, early decelerations do not indicate fetal distress and do not require any intervention.
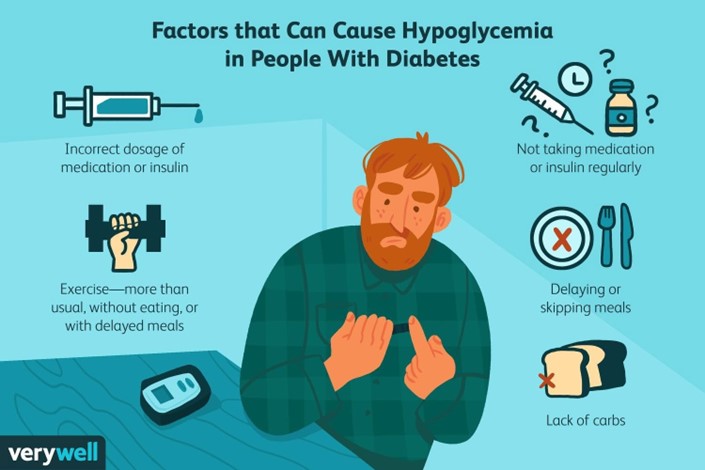
A nurse is providing teaching to a postpartum client who has type 1 diabetes mellitus and is breastfeeding her newborn. Which of the following instructions should the nurse give the client?
Explanation
A postpartum client who has type 1 diabetes mellitus and is breastfeeding her newborn should maintain
scheduled mealtimes for herself to prevent hypoglycemia and ensure adequate milk production¹. Breastfeeding may lower glucose levels in the parent and the risk of type 1 and type 2 diabetes in the child¹. Breastfeeding may also help the parent lose weight, prevent diabetes-related complications, and reduce the chances of some cancers¹.
The other options are incorrect because:
a) Taking more insulin with each meal than you did prior to pregnancy may cause hypoglycemia, especially if you are breastfeeding. You should adjust your insulin doses according to your blood glucose levels and carbohydrate intake, and consult your doctor or diabetes educator for guidance²³.
b) Checking your blood glucose levels every 8 hours is not frequent enough to monitor your diabetes during breastfeeding. You should check your blood glucose levels before and after each breastfeeding session, as well as before meals and snacks, at bedtime, and during the night if needed²³.
c) Limiting your carbohydrate intake to 30 grams per day is too restrictive and may impair your milk production and quality, as well as cause hypoglycemia or ketoacidosis. You should consume adequate carbohydrates from healthy sources, such as whole grains, fruits, vegetables, legumes, and dairy products, to meet your energy and nutritional needs²³.
A nurse is caring for a client who has maternal hypotension following the placement of an epidural. Which of the following actions should the nurse take?
Explanation
Maternal hypotension is a common complication of spinal anesthesia for cesarean section, and it can cause adverse effects on the mother and the fetus, such as nausea, vomiting, dizziness, decreased placental perfusion, fetal acidosis, and fetal distress¹². To prevent or treat maternal hypotension, various techniques have been used, such as fluid preloading or co-loading, vasopressors, lower limb compression devices, and left lateral tilt position¹². Among these, fluid administration is the most widely used and recommended
intervention¹²³. A bolus infusion of lactated Ringer's or other crystalloid solution can increase the intravascular volume and cardiac output, and counteract the decrease in blood pressure caused by spinal anaesthesia¹²³. The optimal timing and amount of fluid administration may vary depending on the individual patient's condition and response, but generally a bolus of 10 to 20 mL/kg is suggested before or during spinal anaesthesia¹²³.
The other options are incorrect because:
b) Applying oxygen via nonrebreather face mask at 2 L/min is not an effective intervention for maternal hypotension. Oxygen supplementation may be beneficial for improving fetal oxygenation in case of fetal distress, but it does not directly increase maternal blood pressure or cardiac output¹². Moreover, 2 L/min is a low flow rate for a nonrebreather face mask, which requires at least 10 L/min to deliver high concentrations of oxygen⁴.
c) Positioning the client in a knee-chest position is not a recommended intervention for maternal hypotension. This position may increase venous return and cardiac output in some cases, but it also increases intra-abdominal pressure and reduces uterine blood flow, which can compromise fetal oxygenation and well-being. A left lateral tilt position of 15 to 30 degrees is preferred to avoid aortocaval compression and improve placental perfusion¹².
d) Giving terbutaline subcutaneously is not an appropriate intervention for maternal hypotension. Terbutaline is a beta-agonist that relaxes the uterine smooth muscle and prevents preterm labor contractions. It has no direct effect on maternal blood pressure or cardiac output, and it may cause maternal tachycardia, palpitations, tremors, and hypokalemia as side effects. Vasopressors such as ephedrine or phenylephrine are more effective and safer drugs for treating maternal hypotension¹².

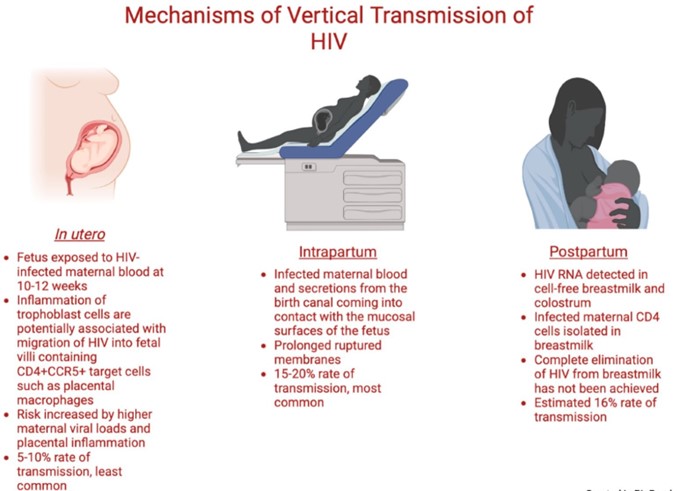
A nurse on the labor and delivery unit is planning care for a client who has human immunodeficiency virus (HIV). Which of the following is an appropriate action for the nurse to take following the birth of the newborn?
Explanation
A newborn who is exposed to HIV perinatally should be bathed and cleansed of maternal secretions as soon as possible after birth to reduce the risk of HIV transmission through the skin or mucous membranes¹². The newborn should also receive antiretroviral prophylaxis within six hours of delivery, preferably within two hours¹². The type and duration of prophylaxis depend on the maternal and infant factors that influence the risk of HIV transmission, such as maternal viral load, antiretroviral therapy, mode of delivery, and infant gestational age¹²³. The newborn should also undergo HIV testing at birth, at 14 to 21 days of age, at one to two months of age, and at four to six months of age¹².
The other options are incorrect because:
b) Initiating contact precautions for the newborn is not necessary or recommended. Contact precautions are used to prevent the spread of infections that are transmited by direct or indirect contact with the patient or the patient's environment. HIV is not transmited by casual contact, and standard precautions are sufficient to prevent exposure to blood or body fluids that may contain HIV¹².
c) Administering intravenous antibiotics to the newborn is not indicated for HIV prevention. Antibiotics are used to treat bacterial infections, not viral infections like HIV. Antibiotics may be given to the newborn for other reasons, such as suspected sepsis or chorioamnionitis, but they do not affect the risk of HIV transmission¹².
d) Encouraging the mother to breastfeed her newborn is contraindicated for HIV prevention. Breastfeeding can transmit HIV from the mother to the infant through breast milk, especially if the mother has a high viral load, mastitis, cracked nipples, or oral lesions in the infant. In resource-limited settings where formula feeding may not be feasible or safe, breastfeeding with maternal or infant antiretroviral therapy may be considered, but in developed countries where safe alternatives are available, breastfeeding is not recommended for mothers with HIV infection¹².
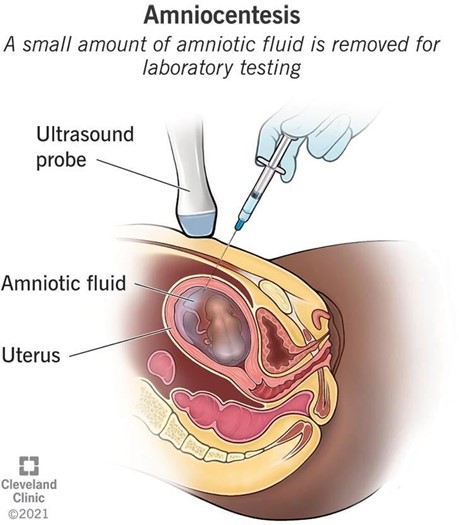
A nurse in a provider's office is caring for a 20-year-old client who is at 12 weeks of gestation and requests an amniocentesis to determine the sex of the fetus. Which of the following responses should the nurse make?
Explanation
Amniocentesis is a prenatal testing procedure that involves inserting a thin needle through the abdomen into the uterus and withdrawing a small amount of amniotic fluid, which contains fetal cells and other substances¹. The fluid is then analyzed in a laboratory to detect certain chromosomal conditions (such as Down syndrome or trisomy 18), genetic conditions (such as cystic fibrosis or Tay-Sachs disease), or neural tube defects (such as spina bifida or anencephaly) ¹². Amniocentesis can also be used to determine the sex of the fetus, but this is not the primary purpose of the test¹².
The other options are incorrect because:
a) Amniocentesis cannot be scheduled for later today if the client requests it. Amniocentesis requires informed consent, pre-test counseling, and preparation of the equipment and laboratory. Amniocentesis is usually performed between 14 and 20 weeks of gestation, and some medical facilities may perform it as early as 11 weeks, but not on the same day as the request¹²³.
c) The client cannot have an amniocentesis until she is at least 35 years of age. This is a common misconception, as advanced maternal age (35 years or older) is one of the risk factors for chromosomal abnormalities in the fetus, and therefore an indication for amniocentesis. However, amniocentesis can be offered to any pregnant woman who has a personal or family history of genetic conditions, abnormal prenatal screening results, or other indications for fetal diagnosis¹²³.
d) The provider will not schedule a chorionic villus sampling (CVS) to determine the sex of the baby. CVS is another prenatal testing procedure that involves taking a small sample of placental tissue, either through the cervix or the abdomen, and analyzing it for chromosomal or genetic conditions. CVS can also determine the sex of the fetus, but it is usually performed earlier than amniocentesis, between 10 and 13 weeks of gestation. CVS has some advantages over amniocentesis, such as earlier diagnosis and shorter waiting time for results, but it also has some disadvantages, such as higher risk of miscarriage, infection, bleeding, or limb defects¹²⁴. CVS is not routinely offered to all pregnant women, and it is not a substitute for amniocentesis.
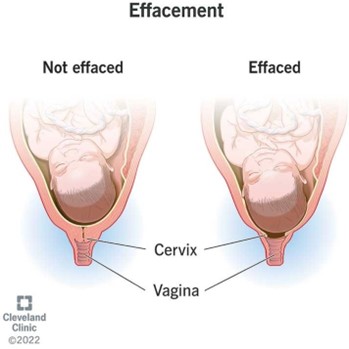
A nurse is admitting a client to the birthing unit who reports her contractions started 1 hr. ago. The nurse determines the client is 80% effaced and 8 cm dilated. The nurse realizes that the client is at risk for which of the following conditions?
Explanation
Postpartum hemorrhage (PPH) is severe vaginal bleeding after childbirth. It can occur within 24 hours of delivery (primary PPH) or up to 12 weeks postpartum (secondary PPH) ¹. PPH can cause serious complications and even death if not treated promptly and effectively¹.
The client in the question is at risk for PPH because she has a rapid labor and a high degree of cervical dilation. These factors can cause uterine atony, which is the failure of the uterus to contract and compress the blood vessels after delivery. Uterine atony is the most common cause of PPH, accounting for up to 80% of cases². Other risk factors for PPH include placental abruption, placenta previa, overdistended uterus, multiple pregnancy, prolonged labor, operative delivery, retained placenta, coagulation disorders, and infection²³.
a) Hyperemesis gravidarum is a condition of severe nausea and vomiting during pregnancy that can cause dehydration, electrolyte imbalance, weight loss, and nutritional deficiencies. It usually occurs in the first trimester and resolves by the second trimester. It is not related to PPH⁴.
b) Ectopic pregnancy is a condition where the fertilized egg implants outside the uterus, usually in the fallopian tube. It can cause abdominal pain, vaginal bleeding, and rupture of the tube. It is a medical emergency that requires prompt diagnosis and treatment. It occurs in early pregnancy and cannot be diagnosed at 12 weeks of gestation by amniocentesis.
d) Incompetent cervix is a condition where the cervix dilates prematurely and painlessly during pregnancy, leading to preterm labor and delivery or pregnancy loss. It usually occurs in the second trimester and can be treated with cervical cerclage or progesterone. It is not associated with PPH.
A nurse is caring for a newborn who is 1 hour old and has a respiratory rate of 50/min, a heart rate of 130/min, and an axillary temperature of 36.1°C (97°F). Which of the following actions should the nurse take?
Explanation
A newborn who is 1 hour old and has a respiratory rate of 50/min, a heart rate of 130/min, and an axillary temperature of 36.1°C (97°F) has normal vital signs for their age¹². However, the newborn is at risk of losing heat and developing hypothermia, which can cause serious complications such as hypoglycemia, metabolic acidosis, and respiratory distress³. Therefore, the nurse should take measures to prevent heat loss and maintain a neutral thermal environment for the newborn³⁴.
One of the effective ways to prevent heat loss in newborns is to apply a cap to their head. The head has a large surface area relative to the body mass and can account for up to 50% of heat loss in newborns³⁴. A cap can reduce heat loss through radiation, convection, and evaporation from the scalp³⁴. The cap should be dry, clean, and snug-fitting, and should not cover the eyes or ears of the newborn³⁴.
a) Giving the newborn a warm bath is not an appropriate action for the nurse to take. Bathing can increase heat loss through evaporation and conduction, especially if the water temperature is not optimal or the room temperature is too low³⁴. Bathing should be delayed until the newborn's temperature is stable and preferably after the first breastfeeding session³⁴.
b) Repositioning the newborn is not a sufficient action for the nurse to take. Repositioning may help reduce heat loss through conduction if the newborn is placed away from cold surfaces or objects, but it does not address heat loss through other mechanisms³⁴. Repositioning should be combined with other interventions, such as skin-to-skin contact, swaddling, or radiant warmers³⁴.
c) Obtaining an oxygen saturation level is not a relevant action for the nurse to take. Oxygen saturation is a measure of how much oxygen is carried by the hemoglobin in the blood. It is not directly related to temperature regulation or heat loss in newborns³⁴. Oxygen saturation should be monitored routinely in all newborns before discharge as part of screening for congenital heart disease, but it does not address the risk of hypothermia⁵.
A nurse is caring for a client who is in labor. Which of the following findings should prompt the nurse to reassess the client?
Explanation
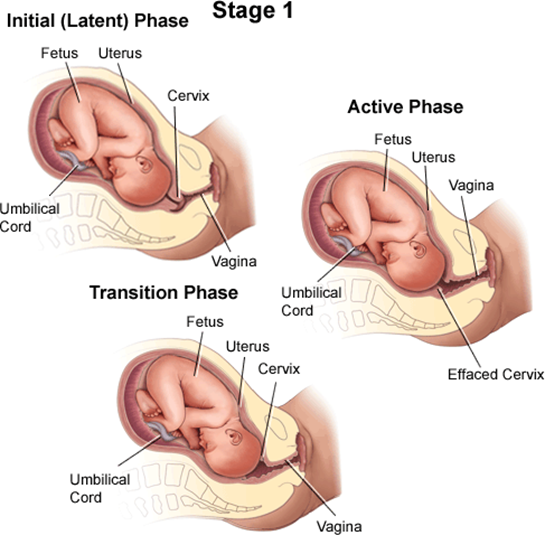
A client who is in labor and reports an urge to have a bowel movement during contractions may be experiencing the transition phase of labor, which is the last and most intense part of the first stage of labor¹². The transition phase occurs when the cervix dilates from 8 to 10 cm and the baby descends into the birth canal¹². The pressure of the baby's head on the rectum can cause a sensation of needing to defecate¹². The transition phase can last from 15 minutes to an hour or more, and it can be accompanied by other signs, such as strong, regular, and painful contractions lasting 60 to 90 seconds; increased bloody show; nausea and vomiting; shaking and shivering; and emotional changes such as irritability, anxiety, or excitement¹²³.
The nurse should reassess the client who reports an urge to have a bowel movement during contractions because this may indicate that the client is close to delivering the baby and needs to be prepared for the second stage of labor, which involves pushing and giving birth¹². The nurse should check the client's cervical dilation, fetal heart rate, and maternal vital signs, and notify the provider if the client is fully dilated or shows signs of fetal or maternal distress¹². The nurse should also support the client's coping strategies, such as breathing techniques, relaxation methods, or pain relief options, and encourage the client not to push until instructed by the provider¹².
b) A sense of excitement and warm, flushed skin are not signs that require reassessment by the nurse. These are normal emotional and physiological responses to labor that reflect increased adrenaline levels and blood flow¹⁴. They do not indicate any complications or imminent delivery.
c) Progressive sacral discomfort during contractions is not a sign that requires reassessment by the nurse. This is a common symptom of labor that results from the pressure of the baby's head on the sacrum and nerves in the lower back¹⁴. It does not indicate any problems or imminent delivery.
d) Intense contractions lasting 45 to 60 seconds are not signs that require reassessment by the nurse. These are typical characteristics of active labor contractions, which occur when the cervix dilates from 4 to 8 cm¹⁴. They do not indicate any complications or imminent delivery.
A nurse is caring for a client who has bladder distention following a vaginal birth. Which of the following actions should the nurse take first?
Explanation
Bladder distention is a common postpartum complication that can occur due to decreased bladder sensation, perineal edema, trauma, or pain after vaginal birth. Bladder distention can interfere with uterine contraction and involution, leading to increased bleeding and risk of infection. Therefore, it is important to assess and manage bladder distention promptly and effectively in postpartum clients.
The first action the nurse should take for a client who has bladder distention is to assist the client to the bathroom and encourage voiding. This is the least invasive and most natural way to empty the bladder and relieve the distention. The nurse should provide privacy, comfort, and support to the client, and help with perineal care after voiding. The nurse should also measure the urine output and monitor for signs of urinary retention or infection, such as dribbling, frequency, urgency, dysuria, hematuria, or foul-smelling urine.
b) Inserting a urinary catheter is not the first action the nurse should take for a client who has bladder distention. A urinary catheter is an invasive procedure that can introduce infection, trauma, or irritation to the urinary tract. It should be used only as a last resort when other methods of bladder emptying have failed or are contraindicated. The nurse should obtain a provider's order before inserting a urinary catheter and follow strict aseptic technique.
c) Offering the client a sitz bath is not the first action the nurse should take for a client who has bladder distention. A sitz bath is a warm water bath that covers only the hips and buttocks. It can provide comfort and promote healing for clients who have perineal lacerations, episiotomies, or hemorrhoids after vaginal birth. However, it does not directly address bladder distention or facilitate voiding. It may also increase the risk of infection or bleeding if done too soon or too frequently after delivery.
d) Pouring warm water over the client's perineum is not the first action the nurse should take for a client who has bladder distention. Pouring warm water over the perineum can help with perineal care and hygiene after vaginal birth. It can also stimulate voiding by creating a relaxing effect on the pelvic floor muscles. However, it does not ensure complete bladder emptying or relieve bladder distention. It may also cause discomfort or irritation if the water temperature or pressure is too high.
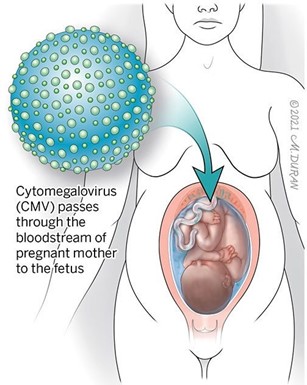
A nurse manager on the labor and delivery unit is teaching a group of newly licensed nurses about maternal cytomegalovirus. Which of the following information should the nurse manager include in the teaching?
Explanation
This is the only option that is true and relevant to maternal cytomegalovirus infection. CMV can be transmitted from the newborn to the mother or other caregivers through contact with the saliva and urine of the newborn, which may contain high amounts of the virus. Therefore, it is important to practice good hygiene and avoid contact with these body fluids when caring for a newborn with congenital CMV.
a) This infection does not require that airborne precautions be initiated for the newborn. Airborne precautions are used to prevent the spread of infections that are transmitted by small droplets that can remain suspended in the air and travel over long distances, such as tuberculosis, measles, or chickenpox. CMV is not transmitted by airborne route, and standard precautions are sufficient to prevent exposure to blood or body fluids that may contain CMV
b) Mothers will not receive prophylactic treatment with acyclovir prior to delivery. Acyclovir is an antiviral medication that is used to treat herpes simplex virus (HSV) infections, such as cold sores, genital herpes, or neonatal herpes. It has no effect on CMV infection, and it is not recommended for pregnant women or newborns with CMV.
c) Lesions are not visible on the mother's genitals. Lesions are a sign of HSV infection, not CMV infection. HSV can cause painful blisters or ulcers on the mouth or genitals, and it can be transmitted to the newborn during delivery. CMV does not cause any visible symptoms on the mother's genitals, and it can be transmitted to the newborn during pregnancy, delivery, or breastfeeding.
A nurse is caring for a client who is 1 day postpartum and breastfeeding her newborn. The client reports sore nipples. Which of the following actions should the nurse take?
Explanation
Sore nipples are a common problem for breastfeeding mothers, especially in the first few days or weeks after delivery. They can cause pain, discomfort, and frustration, and may interfere with breastfeeding success and satisfaction. The most common cause of sore nipples is poor latch, which means that the newborn does not attach to the breast correctly and does not suckle effectively. Poor latch can result from various factors, such as improper positioning, tongue-tie, inverted or flat nipples, engorgement, or thrush.
The nurse should assess the newborn's latch while breastfeeding to identify and correct any problems that may cause sore nipples. The nurse should observe the following signs of a good latch:
- The newborn's mouth is wide open and covers most of the areola (the dark area around the nipple).
- The newborn's chin and nose touch the breast, and the cheeks are rounded and not dimpled.
- The newborn's tongue is visible under the lower lip and curls around the breast.
- The newborn's lips are flanged outwards and not tucked inwards.
- The newborn's jaw moves rhythmically and smoothly, and swallowing sounds are audible.
- The mother feels a gentle tugging sensation on the nipple, but no pain or pinching.
The nurse should also teach the mother how to achieve a good latch by using different positions, supporting the breast with her hand, tickling the newborn's lower lip with her nipple, and bringing the newborn to the breast when their mouth is wide open. The nurse should also encourage the mother to seek help from a lactation consultant or a peer support group if she has persistent or severe nipple pain.
a) Instructing the client to wait 4 hours between daytime feedings is not an appropriate action for the nurse to take. This may reduce nipple soreness temporarily, but it can also cause breast engorgement, milk supply reduction, mastitis, or poor weight gain in the newborn. The nurse should advise the client to feed the newborn on demand, usually every 1.5 to 3 hours during the day and every 3 to 4 hours at night.
b) Offering supplemental formula between the newborn's feedings is not an appropriate action for the nurse to take. This may interfere with breastfeeding initiation and establishment, as it can reduce the mother's milk supply, confuse the newborn's sucking pattern, increase the risk of nipple preference or rejection, and expose the newborn to potential allergens or infections. The nurse should support exclusive breastfeeding for the first six months of life, unless there is a medical indication for supplementation.
c) Having the client limit the length of breastfeeding to 5 minutes per breast is not an appropriate action for the nurse to take. This may not be enough time for the newborn to get enough milk, especially the hindmilk that is richer in fat and calories. It may also prevent proper drainage of the breast and lead to engorgement or mastitis. The nurse should advise the client to let the newborn feed until they are satisfied and release the breast on their own, which may take 10 to 20 minutes per breast on average.

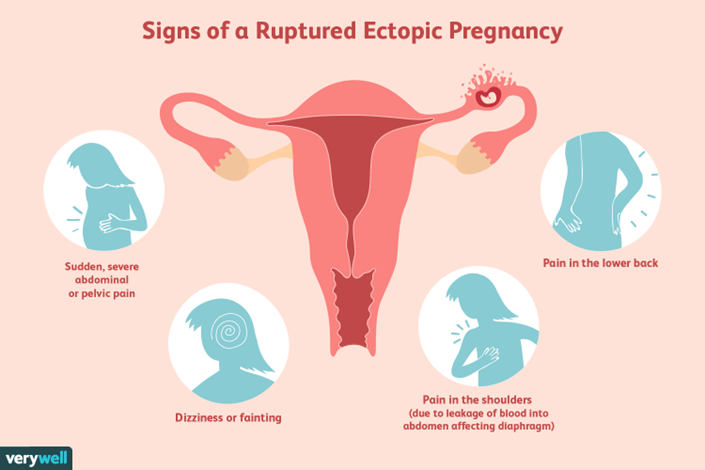
A nurse is caring for a client who is at 8 weeks of gestation and has an ectopic pregnancy. Which of the following manifestations should the nurse expect?
Explanation
An ectopic pregnancy is a pregnancy that occurs outside the uterus, usually in the fallopian tube. The most common manifestation of an ectopic pregnancy is sharp pelvic pain, typically on one side. This pain is often described as severe and may be accompanied by shoulder pain or dizziness. The pain occurs because the fallopian tube is not designed to accommodate a growing embryo, leading to stretching and possible rupture of the tube.
Elevated blood pressure is not typically associated with an ectopic pregnancy. Blood pressure changes may occur in other conditions, such as preeclampsia, but it is not a characteristic manifestation of an ectopic pregnancy.
Bright red vaginal discharge is not a typical manifestation of an ectopic pregnancy. Vaginal bleeding may occur, but it is usually darker and more like a menstrual flow. Bright red vaginal discharge may indicate other conditions, such as a threatened miscarriage or a vaginal infection.
A scaphoid abdomen (a concave or sunken appearance of the abdomen) is not a specific manifestation of an ectopic pregnancy. It may be seen in conditions like malnutrition or dehydration, but it is not directly related to an ectopic pregnancy.
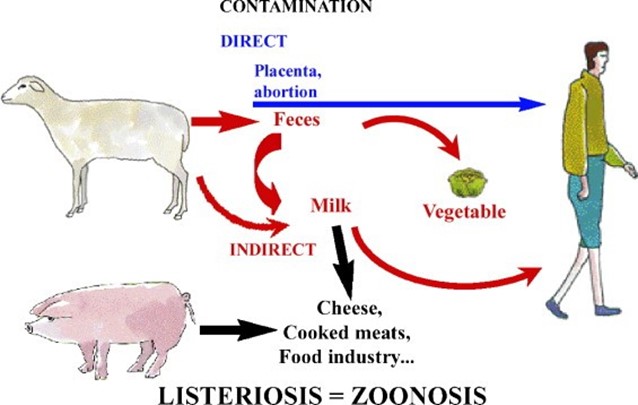
A nurse is teaching a prenatal client about listeriosis and dietary modifications during pregnancy. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Listeriosis is a foodborne illness that can be very dangerous during pregnancy. It is caused by eating foods contaminated with the bacterium Listeria monocytogenes, which can grow well at refrigerator temperatures. Listeriosis can cause miscarriage, stillbirth, preterm labor, and serious illness or death in newborns. Pregnant women are 10 times more likely than other people to get Listeria infection¹.
To prevent listeriosis, pregnant women should avoid certain types of food that are more likely to be contaminated with Listeria, such as:
- Hot dogs and deli meats, unless they are reheated until steaming hot
- Soft cheeses made from unpasteurized milk, such as feta, brie, camembert, blue-veined cheeses, and
queso fresco
- Refrigerated pâtés or meat spreads
- Refrigerated smoked seafood, such as salmon, trout, whitefish, cod, tuna, or mackerel
- Raw or undercooked meat, poultry, seafood, or eggs
- Unpasteurized milk or dairy products
- Unwashed fruits and vegetables
Grilled chicken on a bun is a safe choice for lunchtime because the chicken is cooked and the bun is not likely to be contaminated with Listeria. However, the other options are not safe for pregnant women because they may contain Listeria or other harmful bacteria. A hot dog at the ballpark may not be reheated enough to kill Listeria. A seafood salad from the grocery store may contain refrigerated smoked seafood or mayonnaise made from raw eggs. Soft cheese is often made from unpasteurized milk and can harbor Listeria.
The other options are incorrect because they may expose the client to Listeria or other harmful bacteria, as I explained in my previous response. Let me summarize the reasons for you:
b) "I can still have a hot dog at the ballpark. This is incorrect because hot dogs and deli meats may contain Listeria unless they are reheated until steaming hot. A hot dog at the ballpark may not be hot enough to kill the bacteria.
c) "I can purchase a seafood salad from the grocery store." This is incorrect because seafood salad may contain refrigerated smoked seafood or mayonnaise made from raw eggs. Refrigerated smoked seafood can harbor Listeria and raw eggs can contain Salmonella or other bacteria that can cause food poisoning.
d) "I can have a mid-day snack with soft cheese.” This is incorrect because soft cheese made from unpasteurized milk can be contaminated with Listeria. Examples of soft cheese are feta, brie, camembert, blue-veined cheeses, and queso fresco.
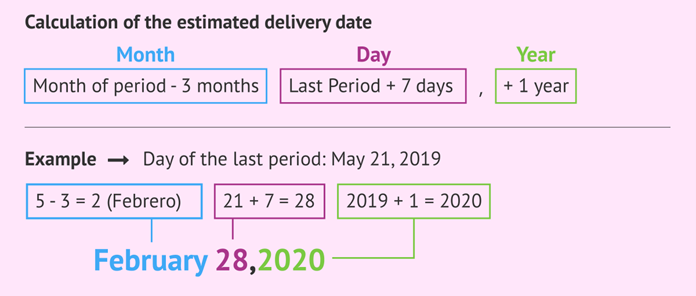
A nurse is calculating the estimated date of delivery for a client who reports that the first day of her last menstrual period was August 10. Using Nägele's Rule, which of the following is the client's estimated date of delivery?
Explanation
Nägele's Rule is a common method used to estimate the expected date of delivery (EDD) based on the first day of the client's last menstrual period (LMP). According to Nägele's Rule, you subtract 3 months from the LMP date and add 7 days, then adjust the year if necessary.
In this case, the first day of the client's last menstrual period was August 10. Subtracting 3 months gives us May 10. Adding 7 days gives us May 17. Therefore, the estimated date of delivery for this client is May 17.
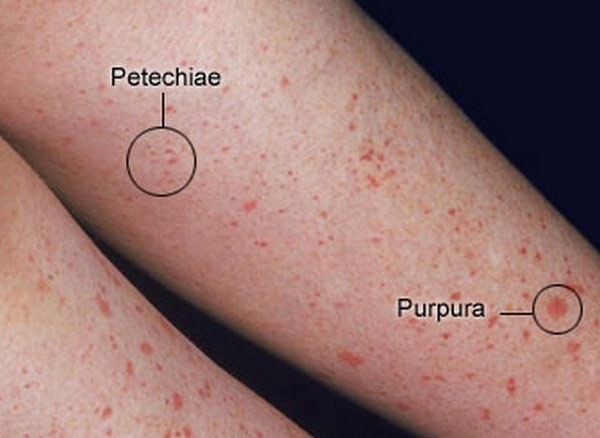
A nurse is performing an initial assessment of a newborn who was delivered with a nuchal cord. Which of the following clinical findings should the nurse expect?
Explanation
Facial petechiae are small, red or purple spots of bleeding under the skin or mucous membranes of the face. They are caused by the rupture of tiny blood vessels called capillaries. Facial petechiae can occur as a result of prolonged straining, such as during childbirth, vomiting, coughing, or crying¹. The increased pressure in the veins of the head and neck can cause the capillaries to burst, resulting in petechiae. Facial petechiae are usually harmless and resolve on their own without treatment.
The other options are not related to prolonged straining and have different causes and appearances:
a) Periauricular papillomas are benign, wart-like growths that occur near the ear. They are caused by human papillomavirus (HPV) infection and may be present at birth or develop later in life. They are usually painless and do not bleed⁴.
b) Erythema toxicum is a common skin condition in newborn babies. It causes a rash and small, fluid-filled bumps that may appear on the face, limbs, or chest. It is not caused by bleeding, infection, or allergy, but by an unknown mechanism. It does not cause discomfort to the baby and clears up without treatment within one to two weeks⁵.
d) Telangiectatic nevi are birthmarks that are caused by dilated blood vessels near the surface of the skin. They appear as red or purple patches or patterns on the skin that do not fade with pressure. They are present at birth and may grow in proportion to the child's growth. They are not associated with bleeding or infection and do not require treatment unless they cause cosmetic concerns⁶.
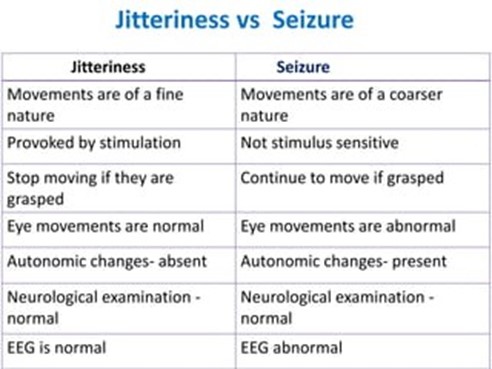
A nurse is assessing a newborn whose mother had gestational diabetes mellitus. The nurse should monitor for which of the following findings as a manifestation of hypoglycemia?
Explanation
Hypoglycemia is a condition in which the blood sugar (glucose) level is too low. Glucose is the main source
of energy for the brain and the body. Newborns need a steady supply of glucose to maintain normal body
functions and growth. Hypoglycemia can occur in newborns for various reasons, such as prematurity, infection, birth asphyxia, maternal diabetes, or inadequate feeding¹.
Hypoglycemia can cause various symptoms in newborns, depending on the severity and duration of the low blood sugar level. Some of the common symptoms include:
- Jitteriness or tremors
- Irritability or crying
- Lethargy or sleepiness
- Poor feeding or sucking
- Low body temperature
- Pale or blue skin color
- Sweating
- Rapid breathing or heart rate
- Seizures or coma
Jitteriness is one of the earliest and most frequent signs of hypoglycemia in newborns². It is caused by the stimulation of the nervous system by low blood sugar levels. Jitteriness can be distinguished from seizures by several features, such as:
- Jitteriness is provoked by stimuli, such as noise or touch, while seizures occur spontaneously
- Jitteriness stops when the stimulus is removed or when the baby is held, while seizures persist
- Jitteriness involves rapid movements of the limbs, chin, or trunk, while seizures involve rhythmic jerking of
the limbs or eyes
- Jitteriness does not affect the level of consciousness, while seizures may cause the baby to be unresponsive
The other options are not typical signs of hypoglycemia in newborns and have different causes:
a) Petechiae are small red or purple spots on the skin caused by bleeding under the skin. They can occur due to trauma during delivery, infection, clotting disorders, or low platelet count.
b) Increased muscle tone is a state of increased tension or stiffness in the muscles. It can occur due to neurological disorders, such as cerebral palsy, spinal cord injury, or brain damage.
d) Abdominal distention is a condition in which the abdomen becomes swollen or enlarged. It can occur due to various causes, such as intestinal obstruction, gas accumulation, organ enlargement, fluid accumulation, or tumor.
A nurse in a clinic is caring for a client who is in her second trimester of pregnancy. The client expresses concern about preparing her 2-year-old child for a new sibling. Which of the following is an appropriate response by the nurse?
Explanation
Preparing a toddler for a new sibling can be challenging, but there are some strategies that can help ease the transition and reduce the risk of jealousy or resentment. One of these strategies is to make any major changes in the toddler's routine or environment well before the baby arrives, such as moving to a new bed, starting preschool, or toilet training. This can help the toddler adjust to the change without feeling displaced or threatened by the baby. It can also prevent the toddler from associating the change with the baby and blaming the baby for it¹².
Moving a toddler to a new bed 2 months before the baby comes home is a good example of this strategy. It gives the toddler enough time to get used to sleeping in a different place and feeling comfortable and secure in it. It also avoids making the toddler feel like they are being kicked out of their bed to make room for the baby. The toddler may even feel proud of having a big-kid bed and being more independent¹².
The other options are not appropriate responses by the nurse because they may have negative effects on the toddler's adjustment to the new sibling:
a) "Let your toddler see you carrying the baby into the home for the first time." This is not a good idea because it may make the toddler feel left out or replaced by the baby. The toddler may not understand why they were not with you when you brought the baby home and may feel hurt or angry. A better option is to have someone else carry the baby into the home while you greet your toddler with a hug and a smile. Then, you can introduce your toddler to their new sibling and involve them in welcoming and caring for the baby¹³.
b) "Avoid bringing your toddler to prenatal visits." This is not a good idea because it may make the toddler feel excluded or curious about what is going on. Bringing your toddler to some of your prenatal visits can help them learn more about the baby and feel more connected to them. You can show your toddler pictures of the baby's development, let them hear the baby's heartbeat, or ask them to help you choose clothes or toys for the baby. However, you should also be prepared for your toddler's possible boredom or impatience during long or boring appointments and bring some snacks or activities to keep them entertained¹⁴.
c) "Require scheduled interactions between the toddler and the baby." This is not a good idea because it may make the toddler feel pressured or resentful toward the baby. Forcing your toddler to interact with the baby when they are not ready or interested can backfire and cause more conflict or distance between them. A better option is to follow your toddler's cues and let them decide how much and when they want to interact with the baby. You can also praise your toddler for any positive interactions they have with the baby, such as giving them a gentle kiss, sharing a toy, or singing a song¹³.
A nurse is assessing a newborn whose mother had a primary cytomegalovirus (CMV) infection during pregnancy. The newborn acquired CMV transplacentally. Which of the following findings should the nurse expect the newborn to exhibit?
Explanation
Cytomegalovirus (CMV) is a common virus that belongs to the herpes family. Most people who get infected with CMV have no symptoms or only mild symptoms, such as fever, fatigue, or sore throat. However, CMV can cause serious problems in newborns who are infected before birth or around the time of birth. This is called congenital CMV infection¹.
Congenital CMV infection can affect various organs and systems in the newborn, such as the brain, eyes, liver, spleen, lungs, and blood. Some of the possible signs and symptoms of congenital CMV infection are:
- Low birth weight
- Small head size (microcephaly)
- Enlarged liver and spleen (hepatosplenomegaly)
- Yellow skin and eyes (jaundice)
- Purple skin patches or bleeding spots (petechiae or purpura)
- Pneumonia
- Seizures
- Inflammation of the brain (encephalitis) or eye (retinitis)
One of the most common and serious complications of congenital CMV infection is hearing loss. Hearing loss can affect one or both ears and can range from mild to profound. Hearing loss can be present at birth or develop later in childhood. Hearing loss can affect the child's speech, language, and cognitive development².
Hearing loss due to congenital CMV infection is often progressive, meaning that it can worsen over time. Therefore, newborns who are diagnosed with congenital CMV infection should have regular hearing tests to monitor their hearing status and receive early intervention if needed. Early intervention may include hearing aids, cochlear implants, speech therapy, or sign language².
The other options are not typical signs of congenital CMV infection and have different causes:
a) Macrosomia is a condition in which a newborn has a birth weight above the 90th percentile for their gestational age. It can be caused by maternal diabetes, obesity, genetics, or prolonged pregnancy.
b) Cataracts are cloudy areas in the lens of the eye that impair vision. They can be caused by genetic disorders, infections, trauma, or exposure to certain drugs or radiation.
d) Urinary tract infection is an infection of the bladder, urethra, kidneys, or ureters. It can be caused by
bacteria, viruses, fungi, or parasites.
Sign Up or Login to view all the 62 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

