ATI Rn Nursing Care of Children 2020
Total Questions : 58
Showing 25 questions, Sign in for moreA nurse is assessing an older adult client. Which of the following findings should the nurse expect?
Explanation
A decreased sense of balance is a normal age-related change that occurs in older adults due to changes in the vestibular system, vision, and proprioception. Nighttime urinary incontinence, increased nighttime sleeping, and heightened sense of pain are not normal findings and may indicate underlying health problems.
A nurse is caring for a client who has a chest tube following thoracic surgery. Which of the following tasks should the nurse delegate to assistive personnel?
Explanation
The nurse can delegate tasks that are routine, unskilled, and do not require nursing judgment to assistive personnel. Assisting the client to select food choices from the menu is an example of such a task. Evaluating the client's response to pain medication, monitoring the characteristics of the client's chest tube drainage, and teaching deepbreathing and coughing to the client are tasks that require nursing judgment and skill and should not be delegated.
A nurse is caring for a client who has restraints to each extremity. Which of the following assessments should the nurse perform first?
Explanation
When caring for a client who has restraints, the nurse should follow the ABCDE priority-setting framework and assess airway, breathing, circulation, disability, and exposure first. Peripheral pulses are an indicator of circulation and should be assessed first to ensure adequate blood flow to the extremities. Comfort level, skin integrity, and elimination needs are also important assessments but are not as high priority as circulation.

A nurse is providing preoperative teaching to a client over the phone in preparation for outpatient surgery. Which of the following information should the nurse include in the teaching?
Explanation
The nurse should explain the need to have another adult drive the client home following surgery, as this is a safety measure to prevent complications such as bleeding, infection, or injury due to impaired cognition or mobility after anesthesia or sedation. The nurse should ask the client to shower once with an antiseptic soap on either the night before or morning of surgery, not 3 times the day before surgery, as this can reduce the risk of surgical site infection. The nurse should inform the client that they cannot wear makeup during surgery, as this can interfere with the monitoring of skin color and oxygen saturation. The nurse should instruct the client to stop drinking clear liquids at least 2 hours before surgery, not 1 hour before surgery, as this can reduce the risk of aspiration and gastric distension.
A nurse is providing teaching to a client about the administration of clotrimazole vaginal suppositories. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Clotrimazole vaginal suppositories are antifungal medications that treat yeast infections in the vagina. They should be inserted as far inside the vagina as possible to reach the site of infection.

A nurse is caring for a client who is scheduled to have his alanine aminotransferase (ALT) level checked. The client asks the nurse to explain the laboratory test. Which of the following is an appropriate response by the nurse?
Explanation
A tracheostomy is a surgical opening in the neck that allows air to enter the lungs through a tube called a tracheostomy tube. The tube has two parts: an outer cannula that stays in place and an inner cannula that can be removed for cleaning. The tracheostomy ties are used to secure the tube to the neck and prevent it from falling out. They should be adjusted to allow one finger to fit snugly underneath so that they are not too tight or too loose.

A nurse is planning to provide discharge instructions to a client who does not speak the same language as the nurse. Which of the following actions should the nurse take?
Explanation
A nurse should use an interpreter who speaks the client's language when providing discharge instructions to ensure effective communication and understanding of the information. The interpreter should be a trained professional who can convey the message accurately and respect confidentiality.
A nurse is preparing to administer a controlled substance to a client for pain management. Which of the following actions should the nurse take?
Explanation
The nurse should ask a second nurse to record her signature when wasting any unused portion of the controlled substance. This is to ensure accountability and prevent diversion of narcotics. The nurse and the witness should document the amount wasted and the reason for wasting in the log book or electronic system.
A visitor reports to a nurse that she slipped and fell in a client's room. The visitor denies any injury, but is walking with a slight limp. Which of the following actions should the nurse take?
Explanation
A nursing incident report is a document that provides detailed information and account of the chain of events leading up to and following an unforeseen circumstance in a healthcare setting or facility especially in the nursing side. An incident report is used to communicate important safety information to hospital administrators and keep them updated on aspects of patient care for risk management, quality assurance, educational, and legal purposes. An incident report should be completed within 24 hours by whomever witnessed the incident or was notified first. In this case, the nurse should complete an incident report because the visitor's fall is an unforeseen circumstance that threatens patient safety and could have legal implications.
A nurse is assessing a client who is receiving continuous IV fluids through a peripheral IV. Which of the following findings indicates to the nurse that the client is experiencing fluid overload?
Explanation
This is because crackles are a sign of fluid overload in the lungs, which can occur when a client receives too much IV fluid. Fluid overload can cause pulmonary edema, which is a life threatening condition that reduces oxygen exchange in the lungs. Some other signs and symptoms of fluid overload include rapid weight gain, swelling in the arms, legs and face, high blood pressure and shortness of breath.
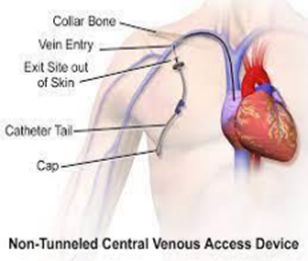
A nurse is planning care for a client who has a new prescription for parenteral nutrition (PN) in 20% dextrose and fat emulsions. Which of the following is an appropriate action to include in the plan of care?
Explanation
Rationale: Parenteral nutrition (PN) is a method of providing essential nutrients to the body through a central vein. PN is indicated for clients who cannot take oral or enteral nutrition due to intestinal failure or other conditions. PN requires a central venous line because the solution is hypertonic and can cause thrombophlebitis or damage to peripheral veins. A central venous line also allows for better monitoring of fluid balance and electrolyte levels.
A nurse is providing end-of-life care for a client. Which of the following actions should the nurse take?
Explanation
The nurse should encourage the client to make choices regarding hygiene, as this respects the client's autonomy and dignity. Suctioning the client's airway every hour is incorrect because it may cause discomfort and distress to the dying client. Offering the client sips of a citrus flavored soda is incorrect because it may irritate the client's mouth and throat, which are often dry and sensitive at the end of life. Positioning the client supine in bed is incorrect because it may increase the risk of aspiration and airway obstruction, as well as pressure ulcers.
A nurse is caring for a client who is dying and having Cheyne-Stokes respirations. Which of the following respiratory findings should the nurse expect?
Explanation
Cheyne-Stokes respirations are an abnormal pattern of breathing characterized by progressively deeper, and sometimes faster, breathing followed by a gradual decrease that results in a temporary stop in breathing called an apnea. The pattern repeats, with each cycle usually taking 30 seconds to 2 minutes. This type of breathing may occur in people who are dying due to heart failure, stroke, brain injury or other causes. The nurse should expect to observe irregular respirations with frequent periods of apnea in the client who is dying and having Cheyne-Stokes respirations.
A nurse is providing care for a client who is to undergo a total laryngectomy. Which of the following interventions is the nurse's priority?
Explanation
A total laryngectomy is a surgical procedure that removes the entire larynx (voice box) and separates the airway from the mouth, nose and esophagus. The client will have a permanent tracheostomy (an opening in the neck) and will not be able to speak normally. An artificial larynx is a device that produces sound by vibrating against the neck or cheek and allows the client to communicate orally. The nurse's priority intervention is to review the use of an artificial larynx with the client before surgery to facilitate postoperative communication and reduce anxiety.
A nurse in an acute care facility is preparing to transfer a client to a long-term care facility. Which of the following information should the nurse include in the hand-off report?
Explanation
The hand-off report is a verbal or written communication that provides essential information about the client's care, treatment, current condition and anticipated needs during a transition of care. The hand-off report should include information that is relevant, accurate, concise and timely. The effectiveness of the last dose of pain medication is an important information that should be included in the hand-off report, as it reflects the client's current pain level, response to treatment and need for further intervention.
A nurse is caring for a client who reports a pain level of 5 on a scale from 0 to 10. The client informs the nurse that pain medications are not an option for managing pain. Which of the following is an appropriate response by the nurse?
Explanation
The rationale for this answer is that a back massage is a non-pharmacological intervention that can help reduce pain by promoting relaxation and increasing blood circulation. It also shows respect for the client's preference and offers a choice of alternative therapy.
A nurse is conducting the Weber's test on a client. Which of the following is an appropriate action for the nurse to take?
Explanation
Place an activated tuning fork in the middle of the client's forehead. The rationale for this answer is that Weber's test is used to assess for conductive or sensorineural hearing loss by comparing bone conduction in both ears. The nurse places an activated tuning fork in the middle of the client's forehead and asks if the sound is heard equally in both ears or louder in one ear.
A nurse is monitoring a client who is receiving continuous IV fluid therapy via a peripheral vein in the left forearm. Which of the following findings indicates that the client has developed phlebitis at the IV site?
Explanation
The rationale for this answer is that phlebitis is inflammation of a vein caused by mechanical, chemical, or bacterial irritation from an IV catheter or fluid. It manifests as redness, warmth, tenderness, and swelling along the path of the vein.
A nurse receives a new prescription over the telephone from a client's provider. Which of the following actions should the nurse take first?
Explanation
The rationale for this answer is that reading back the prescription to the provider is a safety measure that helps prevent medication errors and ensures accuracy and clarity of communication. It also allows for confirmation and verification of any unclear or incomplete information.
A nurse is preparing to bathe a client who has dementia. Which of the following actions should the nurse take?
Explanation
The rationale for this answer is that using distractions such as music, conversation, or toys can help reduce anxiety and agitation in clients with dementia who may resist bathing. It also helps create a positive and comfortable environment for the client.
A nurse is planning an educational conference about informed consent. Which of the following information should the nurse include?
Explanation
Informed consent is the process in which a health care provider educates a patient about the risks, benefits, and alternatives of a given procedure or intervention. The patient must be competent to make a voluntary decision about whether to undergo the procedure or intervention. Informed consent is both an ethical and legal obligation of medical practitioners in the US and originates from the patient's right to direct what happens to their body. The nurse should include this information in the educational conference to inform the participants about the importance and components of informed consent.
A nurse on a medical-surgical unit is caring for a client who reports difficulty sleeping at night. Which of the following findings should indicate to the nurse that the client has sleep deprivation?
Explanation
Sleep deprivation is a condition that occurs when a person does not get enough quality sleep or has a disrupted sleep pattern. Sleep deprivation can affect a person's physical, mental, and emotional health. One of the effects of sleep deprivation is decreased judgment, which means that a person may have difficulty making decisions, solving problems, and concentrating. The nurse should recognize this finding as an indication that the client has sleep deprivation and intervene accordingly.
A nurse is preparing to administer a medication to a client. Which of the following should the nurse use as a client identifier?
Explanation
A client identifier is a unique piece of information that can be used to verify the identity of a client before providing care or services. Using client identifiers helps to prevent errors and ensure patient safety. A photograph is an example of a client identifier that can be used by the nurse to confirm that they are administering the medication to the right person.
A nurse is providing teaching about health promotion guidelines to a group of young adult male clients. Which of the following guidelines should the nurse include?
Explanation
Health promotion is the process of enabling people to increase control over their health and its determinants, and thereby improve their health. Health promotion guidelines are recommendations that help people prevent diseases and maintain optimal health status. One of the guidelines that the nurse should include in the teaching for young adult male clients is to have a dental examination every 6 months, as this can help prevent oral diseases and detect any problems early.
A nurse is speaking with the partner of a client who is unconscious and has a do-not resuscitate (DNR) order in place. The partner requests that CPR be performed if necessary. Which of the following responses should the nurse make?
Explanation
The nurse should acknowledge the partner's feelings and provide emotional support without judging or imposing personal values. The nurse should not suggest changing the DNR order.
Sign Up or Login to view all the 58 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

