ATI RN Nutrition 2019 Updated 2024
Total Questions : 59
Showing 25 questions, Sign in for moreA nurse is planning care for a client who has a new prescription for total parenteral nutrition (TPN). Which of the following actions should the nurse plan to take?
Explanation
The nurse should plan to change the IV tubing for the TPN solution every 72 hours. This is necessary to maintain the sterility of the system and minimize the risk of infection. TPN solutions are prone to bacterial growth, and changing the tubing regularly helps prevent contamination.
Removing TPN from the refrigerator 5 minutes before infusing it is not necessary. TPN solutions are typically stored in the refrigerator to maintain their stability and prevent spoilage. It should be brought to room temperature over a longer period of time, usually 30-60 minutes, before administration.
Discarding the remaining TPN solution that is still infusing after 24 hours is unnecessary. TPN solutions can typically be infused for up to 24 hours without compromising their safety and efficacy. However, it is important to monitor the solution closely for any signs of contamination or degradation, and if any concerns arise, the nurse should consult with the healthcare provider.
Changing the dressing around the IV site weekly is not specific to TPN administration. Dressing changes for peripheral IV sites are typically performed according to facility protocols and the condition of the site, but they are not necessarily done on a weekly basis. The frequency of dressing changes depends on factors such as the type of dressing used, the patient's condition, and any signs of infection or dislodgement.
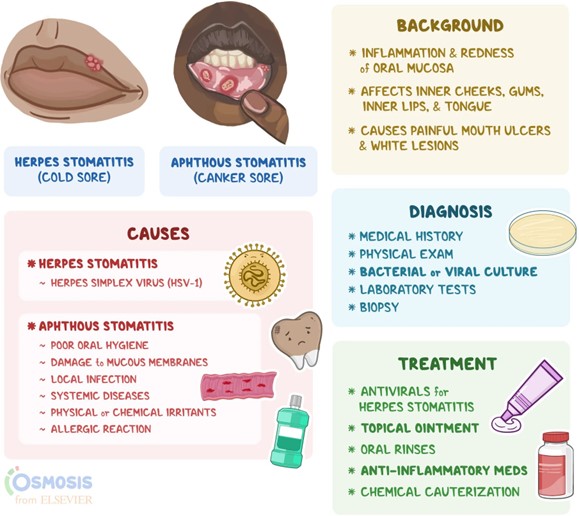
A nurse is caring for a client who has stomatitis following radiation therapy. Which of the following is an appropriate intervention for the nurse to take?
Explanation
An appropriate intervention for a nurse caring for a client with stomatitis following radiation therapy would be to serve foods without sauces or gravies. Stomatitis is the inflammation of the mucous membranes in the mouth, which can cause pain and discomfort. Foods with sauces or gravies can irritate the affected areas and exacerbate the symptoms. Serving plain or bland foods can help alleviate discomfort and promote healing.
Instructing the client to drink liquids without a straw is not specifically related to stomatitis. The use of a straw may not have a direct impact on the condition. However, it is generally recommended to avoid using a straw when there are mouth sores or ulcers to prevent further irritation.
Serving foods while still at a hot temperature is not appropriate for a client with stomatitis. Hot foods can cause additional discomfort and may further irritate the inflamed tissues. It is advisable to serve foods at a cooler or lukewarm temperature to provide relief.
Offering mouth rinses with normal saline and water is not specifically related to stomatitis following radiation therapy. While mouth rinses can be helpful in maintaining oral hygiene and soothing oral tissues, the choice of rinse solution may vary depending on the client's condition and healthcare provider's recommendations. In some cases, a healthcare provider may prescribe a specific mouth rinse or provide instructions on the appropriate solution to use.
A nurse is developing a plan of care for a client who is receiving radiation therapy and is experiencing nausea. Which of the following interventions should the nurse include in the plan?
Explanation
Administer antiemetics on a schedule. Antiemetics are medications used to prevent or relieve nausea and vomiting. By administering them on a schedule, the nurse can help manage and control the client's nausea more effectively.
Providing a snack 30 minutes before treatments is not an appropriate intervention for nausea associated with radiation therapy. In fact, eating before radiation therapy may worsen nausea in some individuals. It is generally recommended to have a light meal or snack a few hours before the treatment to avoid an empty stomach but also prevent overeating that can trigger nausea.
Ensuring foods are served hot is not a recommended intervention for nausea. In fact, hot foods may exacerbate nausea in some individuals. It is advisable to serve foods at a cooler or room temperature, as cooler foods may be better tolerated.
Serving low carbohydrate meals is not specific to managing nausea associated with radiation therapy. While some individuals may find low carbohydrate meals easier to digest, there is no strong evidence suggesting that they alleviate nausea specifically. The choice of meals should be based on the client's preferences, tolerance, and any dietary restrictions they may have.
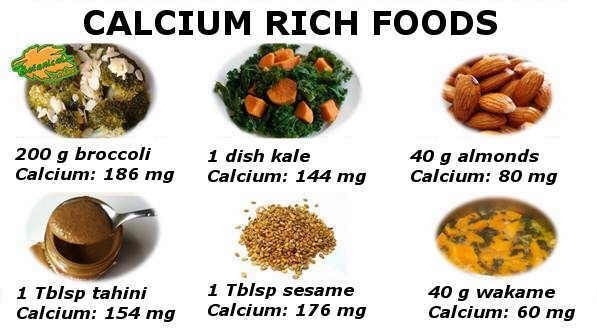
A nurse is teaching a group of clients about dietary needs to prevent osteoporosis. Which of the following dietary choices should the nurse recommend as having the highest calcium content?
Explanation
The dietary choice with the highest calcium content among the options provided would be 1 cup of broccoli. Broccoli is a good source of calcium and can contribute to meeting the body's calcium needs.
While tomatoes, bananas, and grapes are healthy fruits, they are not significant sources of calcium. They are lower in calcium content compared to broccoli. However, these fruits do offer other nutritional benefits such as vitamins and antioxidants.
To promote bone health and prevent osteoporosis, it is important to include calcium-rich foods in the diet, such as dairy products (milk, yogurt, cheese), fortified plant-based milk, leafy green vegetables (like broccoli), tofu, and certain fish (like salmon and sardines). Additionally, adequate vitamin D intake and regular weight-bearing exercise are also important for maintaining strong bones.
A nurse is teaching a class about dietary guidelines to promote cardiovascular health. Which of the following recommendations should the nurse include in the teaching?
Explanation
In teaching about dietary guidelines to promote cardiovascular health, the nurse should include the recommendation to increase the intake of whole grains. Whole grains, such as whole wheat, brown rice, oats, and quinoa, are rich in fiber, vitamins, minerals, and phytochemicals that are beneficial for cardiovascular health. They can help lower cholesterol levels, improve blood sugar control, and reduce the risk of heart disease.
The other choices are incorrect:
Increasing the intake of refined carbohydrates is not a recommended recommendation for promoting cardiovascular health. Refined carbohydrates, such as white bread, white rice, and sugary snacks, have been associated with an increased risk of heart disease. They are often low in fiber and can cause spikes in blood sugar levels, leading to poor cardiovascular health outcomes.
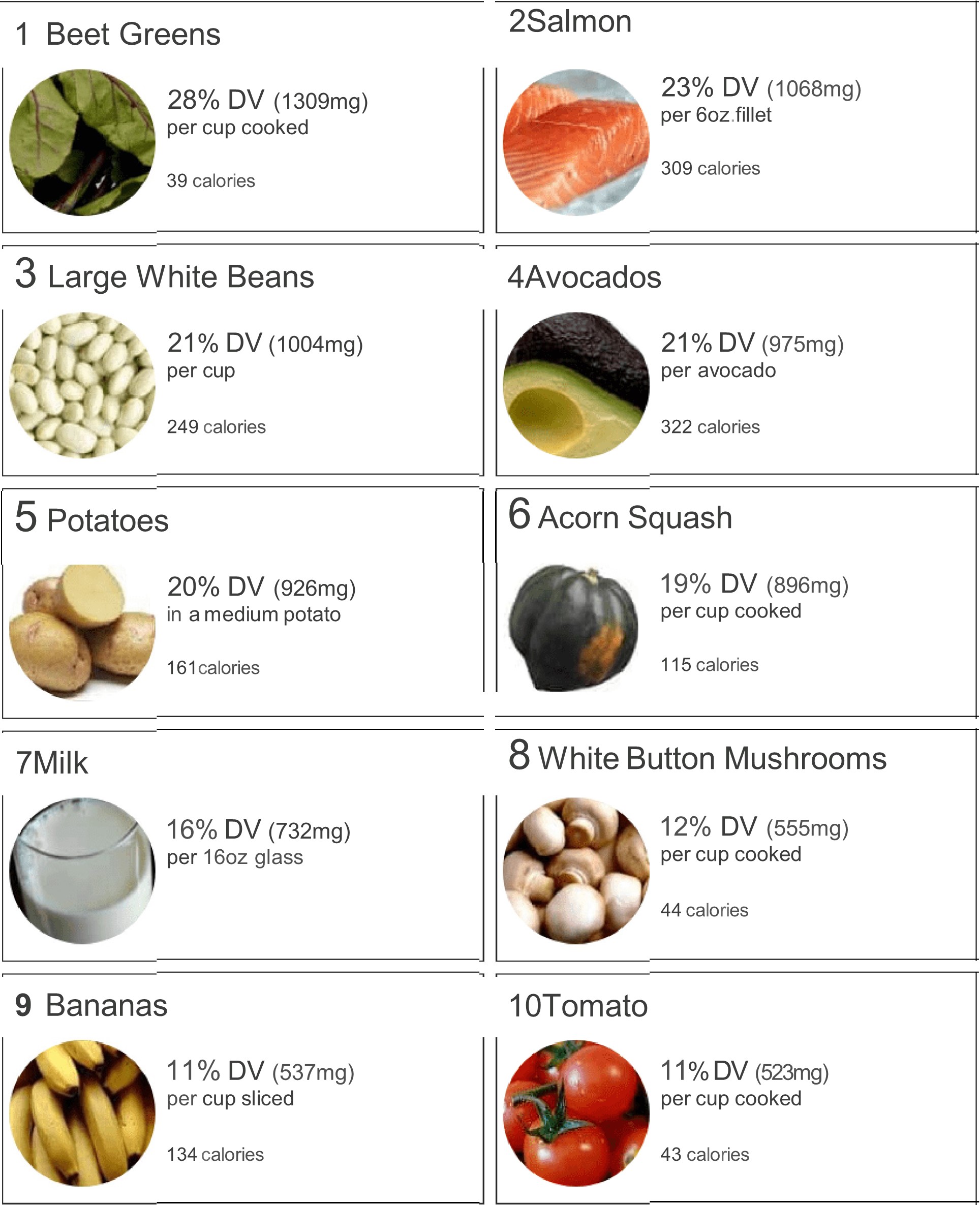
Decreasing the intake of potassium is also not a recommended recommendation. Potassium is an essential mineral that plays a vital role in maintaining heart health and blood pressure regulation. Adequate intake of potassium-rich foods, such as bananas, avocados, spinach, and sweet potatoes, can help lower blood pressure and reduce the risk of cardiovascular diseases.
Decreasing intake of omega-3 fatty acids is incorrect as well. Omega-3 fatty acids, found in fatty fish (such as salmon, mackerel, and sardines), flaxseeds, chia seeds, and walnuts, have been shown to have numerous cardiovascular benefits. They can help reduce inflammation, lower triglyceride levels, improve heart rhythm, and decrease the risk of heart disease. Therefore, it is important to include omega-3 fatty acids in the diet for optimal cardiovascular health.
A nurse is caring for a client who has dysphagia. Which of the following actions should the nurse take?
Explanation
Place the client in a semi-Fowler's position when eating. The semi-Fowler's position involves elevating the head of the bed to an angle of 30 to 45 degrees. This position helps prevent aspiration by facilitating proper swallowing and reducing the risk of food or liquid entering the airway.

Initiating a calorie count of daily food intake is not a specific action for dysphagia. Calorie counting is generally used for monitoring caloric intake in clients with specific dietary needs or conditions, but it is not directly related to dysphagia management. The focus for dysphagia management is on ensuring safe swallowing and preventing complications such as aspiration.
Instructing the client to keep their chin up when swallowing is not appropriate for dysphagia management. This action can actually increase the risk of aspiration. The proper technique for swallowing with dysphagia typically involves tucking the chin slightly down towards the chest to help close off the airway and direct the food or liquid down the esophagus.
Providing food in a thin liquid consistency is not appropriate for dysphagia unless specifically recommended by a healthcare professional. Dysphagia diets typically involve modifying the consistency of food and liquids based on the client's swallowing abilities and recommendations from a speech-language pathologist or dietitian. Different levels of texture modifications (such as pureed, minced, or mechanically soft) may be prescribed to ensure safe swallowing and reduce the risk of aspiration.
A nurse is teaching a client who has Parkinson's disease and is prescribed a monoamine oxidase inhibitor. Which of the following instructions should the nurse include?
Explanation
The instruction that the nurse should include for a client with Parkinson's disease prescribed a monoamine oxidase inhibitor (MAOI) is as follows: "Avoid aged cheeses while taking this medication."
MAOIs are a class of medications used to treat Parkinson's disease by increasing the levels of certain neurotransmitters in the brain. However, they can interact with certain foods and beverages, leading to potentially dangerous side effects.
The interaction between MAOIs and aged cheeses is due to the presence of tyramine, a substance that can cause a sudden and dangerous increase in blood pressure known as a hypertensive crisis. Aged cheeses, such as cheddar, blue cheese, and feta, contain high levels of tyramine, and consuming them while taking an MAOI can lead to this hypertensive crisis.
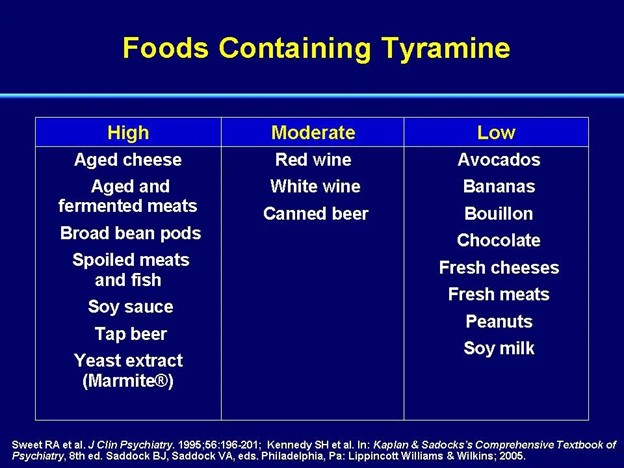
The other options listed in the question are not directly related to the use of MAOIs in Parkinson's disease:
Eating grapefruit is typically contraindicated with certain medications, but it is not specifically relevant to MAOIs or Parkinson's disease.
Maintaining a low-protein diet is not a standard recommendation for individuals taking MAOIs or Parkinson's disease unless specifically advised by the healthcare provider.
Reducing the intake of high-calorie foods is a general recommendation for overall health and weight management but is not specifically related to the use of MAOIs or Parkinson's disease.
A nurse is initiating continuous enteral feedings for a client who has a new gastrostomy tube. Which of the following actions should the nurse take?
Explanation
Keep the client's head elevated at 15° during feedings. Keeping the head elevated helps prevent reflux and aspiration during the feeding process. It promotes the downward movement of the food into the gastrointestinal tract, reducing the risk of complications.
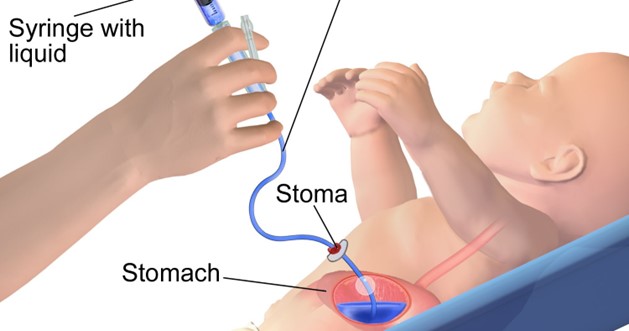
Obtaining the client's electrolyte levels every 4 hours is not necessary when initiating continuous enteral feedings unless specifically indicated by the healthcare provider. Frequent monitoring of electrolyte levels may be needed in certain situations, such as when there is a known electrolyte imbalance or the client is at high risk for such imbalances, but it is not a routine action during the initiation of enteral feedings.
Flushing the client's tube with 30 mL of water every 4 hours is not necessary when initiating continuous enteral feedings. Flushing the tube with water is typically performed before and after medication administration or as recommended by the healthcare provider. Routine flushing every 4 hours is not standard practice unless specifically ordered.
Measuring the client's gastric residual every 12 hours is not appropriate when initiating continuous enteral feedings. Gastric residual measurement is performed to assess the amount of feed remaining in the stomach and to monitor for feeding intolerance. However, the frequency of gastric residual measurement depends on factors such as the client's condition, risk for aspiration, and institutional protocols. Initially, more frequent measurements may be necessary to establish baseline data and ensure tolerance, but the specific frequency should be determined by the healthcare provider based on the client's individual needs.
A nurse is planning dietary teaching for a client who adheres to a vegan diet. The nurse should identify that the client is at greatest risk for which of the following nutrient deficiencies?
Explanation
Omega-3 fatty acids, specifically eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), are mainly found in fatty fish. Since vegans avoid animal products, they may not consume adequate amounts of EPA and DHA. Plant-based sources of omega-3 fatty acids, such as flaxseeds, chia seeds, and walnuts, provide a different type of omega-3 called
alpha-linolenic acid (ALA), which can be converted to EPA and DHA in the body to some extent. However, this conversion is not very efficient, and the amount of EPA and DHA obtained from plant-based sources may be insufficient to meet the body's needs. Therefore, vegan individuals are at greater risk of omega-3 fatty acid deficiency.
Magnesium, potassium, and vitamin A deficiencies are not specifically associated with a vegan diet. These nutrients can be obtained from various plant-based sources. Magnesium can be found in foods such as legumes, nuts, seeds, whole grains, and leafy green vegetables.
Potassium is abundant in fruits, vegetables, legumes, and whole grains.
Vitamin A can be obtained from plant-based sources like carrots, sweet potatoes, spinach, and other dark leafy greens. However, it is important for individuals following a vegan diet to ensure they consume a varied and balanced diet to meet their nutritional needs for these and other essential nutrients.
A nurse is assessing a client who is recovering from a stroke. Which of the following findings is a manifestation of dysphagia?
Explanation
Dysphagia refers to difficulty or discomfort in swallowing. It can occur as a result of weakened or impaired muscles involved in swallowing, which is common after a stroke. When dysphagia is present, it can affect the function of the vocal cords and lead to changes in voice quality, including hoarseness. The hoarseness may be due to the entry of food or liquid into the airway during swallowing, causing irritation to the vocal cords.
Weight gain is not a typical manifestation of dysphagia. If dysphagia is severe and leads to food avoidance or restricted intake, weight loss may occur instead.
Continuous smiling is not a specific manifestation of dysphagia. It may be seen in some stroke survivors as a result of changes in facial muscle control, such as facial weakness or spasticity. However, it is not directly related to dysphagia.
Expressive aphasia refers to difficulty expressing thoughts or using language effectively. It is a common language impairment that can occur after a stroke, specifically affecting the ability to produce or articulate words and sentences. While it is a communication difficulty, it is not directly related to dysphagia, which specifically refers to difficulty swallowing.
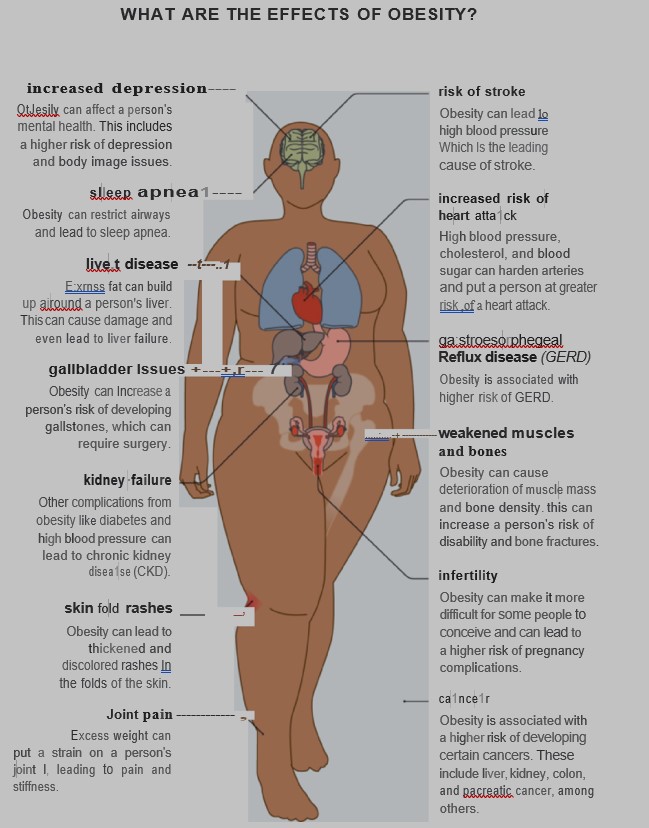
A nurse is teaching the family of a school-age child who is obese about complications of childhood obesity. Which of the following complications should the nurse include in the teaching?
Explanation
Childhood obesity is associated with an increased risk of developing various health problems, and hypertension is one of the most common complications. Excess weight and adiposity can lead to increased blood volume and systemic inflammation, which can contribute to the development of hypertension. Long-standing hypertension in childhood can increase the risk of cardiovascular disease and other health issues later in life.
The other options are incorrect:
Juvenile rheumatoid arthritis is an autoimmune condition characterized by joint inflammation in children. While obesity can place additional stress on joints, it is not directly linked to the development of juvenile rheumatoid arthritis.
Type 1 diabetes mellitus is an autoimmune condition where the body's immune system mistakenly attacks and destroys insulin-producing cells in the pancreas. Obesity is not a known cause of type 1 diabetes.
Hypothyroidism is a condition where the thyroid gland does not produce enough thyroid hormone. While obesity can be associated with thyroid disorders, such as hypothyroidism, it is not a direct complication of childhood obesity.
A nurse is caring for a client who follows a vegan diet. The nurse should identify that the client is at risk for which of the following deficiencies?
Explanation
The nurse should identify that the client who follows a vegan diet is at risk for deficiencies in Vitamin D, Vitamin B12, and potentially Calcium.
1. Vitamin D: Vitamin D is primarily obtained from sunlight exposure and is also found in animal-based foods such as fatty fish, liver, and egg yolks. Since a vegan diet excludes animal products, it can be challenging to obtain sufficient Vitamin D. Vegans should consider fortified foods (e.g., plant-based milk, breakfast cereals) and may require Vitamin D supplements.
2. Vitamin B12: Vitamin B12 is naturally found only in animal products, such as meat, fish, dairy, and eggs. Vegans are at a high risk of Vitamin B12 deficiency because
plant-based foods do not provide adequate amounts. Vegans should consider taking Vitamin B12 supplements or consuming foods fortified with Vitamin B12, such as certain plant-based milk, meat substitutes, and breakfast cereals.
3. Calcium: Calcium is essential for bone health. While it is possible to obtain calcium from plant-based sources such as fortified plant milk, tofu, leafy green vegetables, and fortified juices, vegan diets may be lower in calcium compared to diets that include dairy products. Vegans should pay attention to their calcium intake and consider supplements if needed.
Regarding the options listed in the question, Vitamin C, Magnesium, and Folic Acid deficiencies are not directly associated with a vegan diet. These nutrients can be adequately obtained from a well-planned vegan diet that includes a variety of fruits, vegetables, whole grains, legumes, nuts, and seeds.
A nurse is providing nutritional education to a client who is obese. The nurse should include in the information that which of the following gastrointestinal disorders is commonly associated with obesity?
Explanation
GERD is a chronic condition in which stomach acid and contents flow back into the esophagus, leading to symptoms such as heartburn, regurgitation, and chest pain. Obesity is a significant risk factor for developing GERD. The excess weight can put pressure on the stomach, causing the contents to reflux into the esophagus more easily. Additionally, obesity is associated with a higher prevalence of hiatal hernia, which can further contribute to the development of GERD
Crohn's disease, Peptic ulcer disease, and Celiac disease are not commonly associated with obesity:
Crohn's disease is a type of inflammatory bowel disease that can affect any part of the gastrointestinal tract. It is not specifically associated with obesity but rather has complex genetic and environmental factors as its causes.
Peptic ulcer disease refers to the presence of open sores in the lining of the stomach or small intestine. While obesity may be a risk factor for gastric ulcers, the association is not as strong as with GERD.
Celiac disease is an autoimmune disorder triggered by the ingestion of gluten, a protein found in wheat, barley, and rye. It is not directly related to obesity but is associated with a specific immune response to gluten in genetically susceptible individuals.
A nurse is reviewing the medication administration record for a client who is 2 days postoperative following abdominal surgery. The nurse should recognize which of the following medications places the client at risk for wound dehiscence?
Explanation
Prednisone is a corticosteroid medication that is commonly prescribed for various conditions due to its anti-inflammatory and immunosuppressive effects. However, corticosteroids can impair wound healing by reducing the body's inflammatory response, delaying collagen synthesis, and weakening the tensile strength of the wound. This increases the risk of wound dehiscence, which is the separation or opening of surgical incisions.
Omeprazole is a proton pump inhibitor used to reduce stomach acid production and prevent gastric ulcers but does not directly affect wound healing or increase the risk of wound dehiscence.
Zolmitriptan is a medication used for the acute treatment of migraines and does not directly affect wound healing or increase the risk of wound dehiscence.
Verapamil is a calcium channel blocker used to treat high blood pressure and certain heart conditions. It does not directly affect wound healing or increase the risk of wound dehiscence.
A nurse is providing teaching to a client who has a prescription for a low-saturated fat diet. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Avocado is a healthy source of unsaturated fats, which are beneficial for cardiovascular health. Choosing an avocado dip instead of salsa, which is typically low in fat, aligns with the goal of reducing saturated fat intake.
The other statements are incorrect:
Eating the skin on poultry, even if it is broiled, is not recommended for a low-saturated fat diet. Poultry skin contains significant amounts of saturated fat, so it is advisable to remove the skin before consumption to reduce saturated fat intake.
Including 7 ounces of fish in the diet weekly is not specific to a low-saturated fat diet. While fish is a healthy protein source, the recommendation to consume 7 ounces of fish per week is related to the intake of omega-3 fatty acids, which have cardiovascular benefits. However, the specific type of fish and preparation methods should be considered to ensure a low-saturated fat content.
Using margarine on waffles is not advisable for a low-saturated fat diet. Most margarines contain trans fats or hydrogenated oils, which are unhealthy and contribute to an increase in saturated fat intake. It is better to choose healthier alternatives such as spreads made from nuts, seeds, or avocado, or to use a small amount of healthier oils like olive oil or canola oil.
A nurse is assessing an older adult client who has dysphagia and is experiencing dehydration. Which of the following findings should the nurse expect?
Explanation
The expected finding in an older adult client with dysphagia and dehydration is tachycardia. Tachycardia, an increased heart rate, is a common finding in dehydration as the body tries to compensate for the decreased fluid volume.
The other choices (hypertension, distended neck veins, and decreased respiratory rate) are not typically associated with dehydration in this context.
here's an explanation of why these choices are incorrect:
1. Hypertension: Dehydration usually leads to a decrease in blood volume, resulting in low blood pressure rather than hypertension. Hypertension is not a typical finding in dehydration.
2. Distended neck veins: Dehydration causes a decrease in blood volume, which results in decreased venous return to the heart. Consequently, distended neck veins would not be an expected finding.
3. Decreased respiratory rate: Dehydration itself does not directly affect respiratory rate. However, severe dehydration can lead to electrolyte imbalances, such as hyponatremia (low sodium levels), which can affect brain function and potentially lead to changes in respiratory rate. However, decreased respiratory rate is not a common finding in dehydration alone.
It's important to remember that dehydration can have various signs and symptoms, including dry mucous membranes, decreased urine output, increased thirst, dry skin, dizziness, and confusion.
A nurse is providing discharge teaching to the mother of a newborn about breastfeeding. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
"I should feed my baby on demand at least eight times each day": This statement is correct. Breastfed newborns should be fed on demand, following their cues of hunger. Newborns typically need to breastfeed at least eight times per day to ensure they receive enough nutrition and to establish and maintain a healthy milk supply for the mother.
"I will dilute juice with 50 percent water to supplement between feedings": This statement is incorrect. Breast milk or formula should be the sole source of nutrition for a newborn. Diluting juice with water is not recommended for newborns, as it does not provide the necessary nutrients and may fill the baby's stomach without providing adequate nutrition.
"I should use pumped breast milk within 72 hours of refrigeration": This statement is incorrect. Pumped breast milk can typically be stored in the refrigerator for up to 4-5 days, not just 72 hours. It is important for the mother to follow proper storage guidelines to ensure the safety and freshness of the breast milk.
"I will begin and end with the same breast when I feed my baby": This statement is incorrect. The breastfeeding technique known as "switch nursing" is often recommended, especially for newborns. Switch nursing involves offering both breasts during a feeding session to ensure the baby receives hindmilk, which is richer in fat and provides essential nutrients for growth.
A nurse is assisting in the selection of food for a client who has hypokalemia. Which of the following foods should the nurse select that contains the greatest amount of potassium?
Explanation
According to some sources, the food that contains the greatest amount of potassium among the four options is one small baked potato, with about 925 mg of potassium per serving1.
The other foods have much lower amounts of potassium: 1 oz of cheddar cheese has about 28 mg, 1 cup of brown rice has about 84 mg, and one medium raw tomato has about 290 mg.
A nurse is selecting food items for a client who follows a lacto-vegetarian diet. Which of the following foods should the nurse include in the meals?
Explanation
A lacto-vegetarian diet is a type of vegetarianism that excludes meat, poultry, seafood, and eggs, but includes dairy products, such as milk, cheese, and yogurt. Therefore, the foods that the nurse should include in the meals for a client who follows a lacto-vegetarian diet are cheese and yogurt.
Shrimp and hamburger are not suitable for a lacto-vegetarian diet because they are animal flesh.
Eggs are also not allowed because they are animal products.
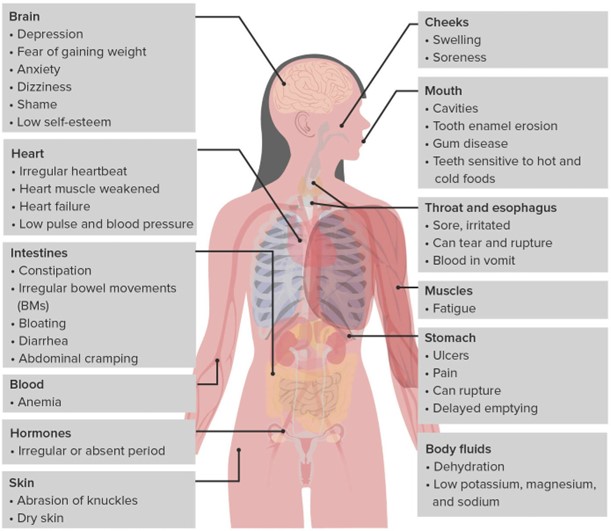
A nurse is reviewing the laboratory results of a client who has bulimia nervosa. The nurse should notify the provider of which of the following results?
Explanation
Low potassium levels, known as hypokalemia, can be a significant concern in individuals with bulimia nervosa due to the frequent purging behaviors associated with the condition. Purging, such as self-induced vomiting or misuse of laxatives or diuretics, can lead to excessive loss of potassium from the body. Hypokalemia can have serious consequences, including cardiac arrhythmias, muscle weakness, fatigue, and even life-threatening complications.
The normal range for potassium is typically around 3.5-5.0 mEq/L. With a potassium level of 3.2 mEq/L falling below the normal range, it indicates a low potassium level and requires prompt attention.
The other laboratory results mentioned in the question are within normal ranges:
● A WBC (white blood cell) count of 5,200/mm3 falls within the normal range (typically between 4,500 and 11,000/mm3) and indicates a normal white blood cell count.
● An Hgb (hemoglobin) level of 14 g/dL falls within the normal range (typically between 12 and 16 g/dL) and indicates a normal hemoglobin level.
● A magnesium level of 1.6 mEq/L, although slightly low, is still within the normal range (typically between 1.5 and 2.5 mEq/L). The nurse should monitor it closely and assess for symptoms associated with hypomagnesemia. If the client's symptoms or other clinical indications suggest a significant magnesium imbalance, the healthcare provider should be notified.
A nurse is providing teaching to a client who has type 1 diabetes mellitus. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
In type 1 diabetes mellitus, when blood glucose levels are consistently high, the body may start breaking down fat for energy, leading to the production of ketones. Ketones can be detected in urine as a result. A blood glucose level of 190 milligrams per deciliter is elevated and can potentially trigger the production of ketones. Monitoring urine for ketones can be an important indicator of diabetes management and helps identify potential complications.
The other statements by the client indicate a lack of understanding or potential misconceptions:
● "I will keep my blood glucose levels between 200 and 212 milligrams per deciliter": This statement suggests a target range that is higher than the recommended target blood glucose levels for individuals with diabetes. Generally, the target range for blood glucose levels in individuals with diabetes is lower, typically between 80-130 mg/dL before meals and below 180 mg/dL after meals.
● "Albumin in my urine is an indication of normal kidney function": This statement is incorrect. The presence of albumin in the urine, called albuminuria, is an indication of kidney damage or dysfunction. It is a common sign of kidney disease, including diabetic nephropathy, which is a complication of diabetes affecting the kidneys.
● "I will keep my HbA1c at five percent": While maintaining a lower HbA1c level is generally desirable for individuals with diabetes, a target of five percent is too low. HbA1c is a measure of average blood glucose levels over the past two to three months. The American Diabetes Association (ADA) recommends an HbA1c target of less than 7 percent for most adults with diabetes, although individualized targets may vary based on factors such as age and other health conditions.
A nurse is teaching a client who reports wanting to lose weight about behavioral modifications. Which of the following statements should the nurse include in the teaching?
Explanation
According to some sources, behavioral modifications for weight loss include:
● Keeping a food journal to track your intake and identify patterns
● Eating smaller portions and using smaller plates
● Filling half of your plate with fruits and vegetables
● Getting plenty of sleep and drinking fluids
● Eating slowly and consciously
● Eating breakfast every day
● Avoiding high-calorie add-ons such as cream, butter, mayonnaise and salad dressings
● Not eating while watching television, reading, working or doing other activities
● Planning healthy snacks and meals in advance and bringing them to work
● Replacing eating with another activity that you will not associate with food
Based on these suggestions, the statement that the nurse should include in the teaching is “Make sure to drink water with your meals.” This can help you feel full and hydrated, and reduce your calorie intake from other beverages.
The other statements are either false or not related to behavioral modifications. For example:
● Your biggest meal of the day should be breakfast. This is not a behavioral modification, but a dietary recommendation that may vary depending on your preferences and needs.
● Meal replacement shakes can cause weight gain. This is not a behavioral modification, but a claim that is not supported by evidence. Meal replacement shakes can be part of a weight loss plan if they are used appropriately and provide adequate nutrition.
● Set your weight loss goal to 2.5 pounds per week. This is not a behavioral modification, but a goal that may be unrealistic or unhealthy for some people. A more reasonable goal is to lose 1 to 2 pounds per week.
A nurse in a long-term care facility is implementing a nutrition plan for a client who is at risk for malnutrition. Which of the following actions should the nurse include in the plan? (Select all that apply.)
Explanation
In a nutrition plan for a client at risk for malnutrition, the nurse should include the following actions:
Assess for pain prior to mealtime: Pain can significantly impact a person's appetite and ability to eat. Assessing for pain before mealtime can help identify any discomfort that may hinder the client's ability to eat.
Provide mouth care before feeding: Proper oral hygiene is essential for maintaining a healthy appetite and preventing oral health issues that can affect eating. Providing mouth care before feeding helps ensure a clean and comfortable oral environment.
Remove the bedpan from the client's sight: Sight and smell can have a significant impact on a person's appetite. Removing the bedpan from the client's sight can help create a more pleasant dining environment and promote a better appetite.
However, the following actions should not be included in the plan:
Discourage snacks between meals: For clients at risk for malnutrition, it may be necessary to encourage nutrient-dense snacks between meals to increase caloric intake. Discouraging snacks may further contribute to malnutrition.
Administer antiemetics following the meal: Administering antiemetics following a meal is not a routine action in a nutrition plan. Antiemetics are typically used to treat nausea and vomiting, which may interfere with a person's ability to eat, but their administration should be based on specific symptoms and prescribed by a healthcare provider.
A nurse is teaching about denture care to the partner of a client who is unable to perform oral hygiene. Which of the following should the nurse include in the teaching?
Explanation
Wipe dentures before storing them in a dry container at night: This is a correct instruction. Before storing dentures overnight, it is important to remove debris and rinse them with water. Wiping the dentures helps to remove any remaining residue or particles and keeps them relatively clean until the next use. Storing dentures in a dry container helps prevent the growth of microorganisms and maintains the shape of the dentures.
Wrap gloved fingers with gauze to remove dentures: This is not the recommended technique for removing dentures. Instead, it is recommended to use a denture brush or a soft-bristled toothbrush with a non-abrasive denture cleaner or mild soap to clean the dentures. The use of gauze may not provide adequate cleaning and may cause damage to the denture surface.
Use a washcloth to clean the denture surfaces: A washcloth is not the ideal tool for cleaning dentures. Instead, a denture brush or a soft-bristled toothbrush should be used. These tools are specifically designed to clean denture surfaces effectively without causing damage.
Floss dentures as part of daily cleaning: Flossing is not necessary for denture cleaning since dentures do not have natural teeth or spaces between them. However, it is important to clean all surfaces of the dentures using a denture brush or a soft-bristled toothbrush to remove plaque, debris, and stains.
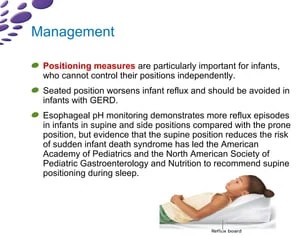
A nurse is providing teaching to the parent of a newborn who has gastroesophageal reflux. Which of the following instructions should the nurse include?
Explanation
"Position the newborn at a 20-degree angle after feeding": This is the correct instruction. After feeding, it is beneficial to position the newborn at a slight angle, usually around 20 degrees, to help reduce gastroesophageal reflux. This position helps gravity keep the stomach contents down and prevents them from regurgitating back into the esophagus.
"Provide a small feeding just before bedtime": This instruction is not recommended for a newborn with gastroesophageal reflux. It is advisable to avoid feeding the baby just before bedtime as lying down can worsen the reflux symptoms. Instead, it is generally recommended to keep the baby upright for some time after feeding to allow for proper digestion and minimize reflux.
"Place the newborn in a side-lying position if vomiting": Placing the newborn in a side-lying position after vomiting is not recommended. This position does not provide adequate support to prevent choking or aspiration in case of vomiting. Instead, it is recommended to keep the newborn in an upright or slightly elevated position after feeding to minimize reflux.
"Dilute formula with 1 tablespoon of water": Diluting formula with water is not a recommended practice unless specifically advised by a healthcare provider. It is important to follow the instructions on the formula packaging or the healthcare provider's guidance regarding formula preparation to ensure appropriate nutrition and hydration for the newborn.
Sign Up or Login to view all the 59 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

