ATI RN Paediatric Nursing 2023
Total Questions : 55
Showing 25 questions, Sign in for moreExhibit 1
Exhibit 2
Exhibit 3
History and Physical
School-age child admitted, diagnosed with cystic fibrosis at 3 months of age, has experienced failure to thrive, and has chronic obstructive pulmonary disease. The child presents with wheezing, rhonchi, paroxysmal cough, and dyspnea. The parent reports large, frothy, foul-smelling stools. The child has deficient levels of vitamin A, D, E, and K.
Barrel-shaped chest
Clubbing of the fingers bilaterally
Respiratory rate 40/min with wheezing and rhonchi noted bilaterally, dyspnea, and paroxysmal cough
Vital Signs
Temperature 38.4° C (101.1° F) Heart rate 100/min Respiratory rate 40/min
Blood pressure 100/57 mm Hg
Laboratory Results
Sputum culture positive for Pseudomonas aeruginosa Stool analysis positive for presence of fat and enzymes Chest x-ray indicates obstructive emphysema WBC count 20,000/mm3 (5,000 to 10,000/mm3)
A nurse is reviewing the child's medical record. Which of the following medications should the nurse expect the provider to prescribe or reconcile from the child's home medication list?
Select all that apply.
Explanation
Rationale:
A. Deficient levels of vitamins A, D, E, and K indicate malabsorption, necessitating supplementation with water-soluble vitamins to address nutritional deficiencies.
B. Acetaminophen is an analgesic and antipyretic that has no effect on the underlying cause of cystic fibrosis.
C. Dornase alfa (Pulmozyme) is a recombinant human deoxyribonuclease enzyme used in the management of cystic fibrosis to improve pulmonary function by reducing the viscosity of mucus in the airways.
D. Meperidine is an opioid analgesic that can cause respiratory depression and increase the risk of pulmonary complications.
E. Children with cystic fibrosis often have pancreatic insufficiency, leading to malabsorption of fats and fat-soluble vitamins. Pancreatic lipase supplements are necessary to aid in the digestion of fats.
Exhibit 1 Exhibit Exhibit 3
Exhibit 4
History and Physical
A 15-year-old adolescent is admitted for a vaso-occlusive crisis. The parent reports that the adolescent has a low-grade fever and has vomited for 3 days. The adolescent reports having right- sided and low back pain. They also report hands and right knee are painful and swollen. The client reports pain as 8 on a scale of 0 to 10.
Vital Signs
Temperature 37.8° C (100° F) Heart rate 100/min
Blood pressure 110/72 mm Hg Respiratory rate 20/min Oxygen saturation 95% on room air
Assessment
Awake, alert, and oriented x 3
Yellow sclera of eyes noted bilaterally
Right upper quadrant tender to palpation Hands painful to touch and swollen bilaterally
Right knee is swollen, warm to palpation, and the client reports pain as 8 on a scale of 0 to 10.
Client is tearful and grimacing during the examination.
The nurse is planning care for the adolescent. Select the 5 interventions the nurse should include.
Explanation
Rationale:
A. Instructing the parent to ensure the pneumococcal vaccine is current is not an immediate priority for the client's care and should be done as part of routine health maintenance.
B. Folic acid supplementation may be part of the overall management of sickle cell disease, but it is not a priority intervention during a vaso-occlusive crisis.
C. Vaso-occlusive crises can lead to tissue hypoxia due to impaired blood flow.
Continuous monitoring of oxygen saturation helps in assessing tissue perfusion and detecting hypoxemia early.
D. Placing the client on strict bed rest can increase the risk of thrombosis and impair circulation.
E. Applying cold compresses to the affected joints is a non-pharmacological intervention that can reduce inflammation and pain in the joints affected by vaso-occlusion. Cold compresses can also constrict blood vessels and reduce blood flow to the area, which can prevent further sickling and tissue damage.
F. Meperidine (Demerol) is a potent opioid analgesic that can help alleviate severe pain associated with vaso-occlusive crises.
G. The nurse should not restrict oral intake, as hydration is important to prevent dehydration and further sickling.
H. Hydroxyurea is used to prevent vaso-occlusive crises in patients with sickle cell disease but is not typically administered during an acute crisis. This is a medication that reduces the frequency and severity of vaso-occlusive crises by increasing the production of fetal hemoglobin, which prevents sickling.
A nurse is caring for a child who has disseminated intravascular coagulation. Which of the following laboratory findings should the nurse expect?
Explanation
Rationale:
A. Disseminated intravascular coagulation (DIC) is associated with consumption of clotting factors, leading to prolonged clotting times, such as increased prothrombin time (PT) and activated partial thromboplastin time (aPTT), rather than decreased.
B. DIC does not typically cause an increase in hemoglobin (Hgb) levels; in fact, it may lead to anemia due to blood loss and consumption of clotting factors.
C. DIC does not typically cause an increase in red blood cell (RBC) count; if anything, it can lead to anemia due to blood loss.
D. DIC is characterized by widespread activation of coagulation, leading to consumption of platelets and decreased platelet count, which can result in bleeding tendencies.
Explanation
Rationale:
A. A toddler who has a heart rate of 68/min is likely to have bradycardia, a slow heart rate that can affect oxygen delivery. Bradycardia could be caused by hypoxia, hypothermia, or cardiac problems. The nurse should report this finding to the provider immediately.
B. This temperature is within the normal range, so it does not require reporting.
C. This blood pressure is within the normal range for an adolescent, so it does not require reporting.
D. The normal respiratory rate for a 3-month-old infant is 25 to 40/min.
Explanation
Rationale:
A. While it's important to ensure that clothing doesn't have small parts that could pose a choking hazard, loose buttons are not typically a significant safety concern.
B. Water heater temperature should be set to around 120°F (approximately 49°C) to prevent scalding burns, so adjusting it to 54°C (129.2°F) would pose a safety risk rather than prevent injury.
C. This is an important safety measure to prevent falls from windows, which can be a significant risk for toddlers.
D. Balloons pose a choking hazard for young children due to the risk of ingestion or aspiration, so they should not be provided as toys for toddlers.
Explanation
Rationale:
A. Dark brown blood indicates old blood and is not a sign of active bleeding.
B. Drinking through a straw can increase the risk of bleeding after tonsillectomy, so it should be avoided.
C. Frequent swallowing may indicate discomfort or bleeding and should prompt notification of the healthcare provider.
D. Clearing the throat can also increase the risk of bleeding and should be discouraged after tonsillectomy.
Explanation
Rationale:
A. Allowing the child to sit on the parent's lap can provide comfort and support during the procedure.
B. While the electrocardiogram (ECG) machine may have alarms, they are not typically related to abnormal heart rhythms during the procedure.
C. ECG leads are typically placed on the chest, not the back.
D. The duration of an ECG is relatively short, usually only a few minutes, so stating that it will take at least 30 minutes may cause unnecessary concern for the parent.
Explanation
Rationale:
A. This is the priority action to confirm the correct placement of the NG tube in the stomach before administering the enteral feeding.
B. This should only be done after confirming proper tube placement.
C. Flushing the tube is necessary, but it should occur after confirming placement.
D. This should occur after confirming proper tube placement.
Explanation
Rationale:
A. Placing an infant who is 5 months old in a high chair to feed is unsafe because the infant might fall or choke.
B. Positioning a 1-month-old infant supine on a soft mattress increases the risk of sudden infant death syndrome (SIDS).
C. Providing a one-piece pacifier is a safe practice since it prevents the pacifier from breaking apart and causing a choking hazard.
D. Infants should be secured in car seats that are away from airbags. Securing the infant's car seat behind an airbag is dangerous because the airbag could injure or kill the infant in a crash.
Explanation
Rationale:
A. Obtaining an x-ray of the child's neck may be necessary for diagnosis, but ensuring immediate safety and infection control measures take precedence.
B. Administering intravenous antibiotics is important in the treatment of epiglottitis but is not the immediate priority.
C. Initiating droplet precautions is crucial in this case to prevent the spread of infection to others but is not as important as securing the airway.
D. Placing intubation equipment at the bedside is the first priority because epiglottitis can cause airway obstruction and respiratory distress.
Which of the following instructions should the nurse include in the teaching?
Explanation
Rationale:
A. Washing the child's hair with ketoconazole shampoo is not typically indicated for treating scabies, which is caused by mites.
B. Treating close contacts is essential to prevent the spread of scabies.
C. Applying petroleum jelly is not an effective treatment for scabies.
D. Soaking combs and brushes in boiling water may help to disinfect them but is not the primary treatment for scabies.
Explanation
Rationale:
A. Retesting in a week may be necessary, but notifying the public health department is a more immediate concern.
B. Notifying the public health department is essential for contact tracing and preventing the spread of syphilis.
C. Involving the patient's parents may not be appropriate for a 20-year-old patient.
D. Metronidazole is not typically used to treat syphilis; penicillin or other antibiotics are the standard treatment.
Explanation
Rationale:
A. This is a positive reinforcement strategy that can motivate the child to take the medication and reduce the unpleasant taste.
B. Giving milk with the medication may not be suitable for all medications, and some medications may interact with dairy products.
C. Mixing the medication with the child's favorite food is not advised because it can alter the taste and texture of the food and make the child dislike it in the future.
D. Diluting the medication with water may not be appropriate for all medications, and it could alter the effectiveness or stability of the medication.
Nurses' Notes
The child's guardian states the child has been unable to sleep recently and has been very irritable. Guardian expresses concern about the child's atopic dermatitis worsening and the child scratching excessively, which results in the areas bleeding. Guardian states the child has a history of allergic rhinitis.
Assessment
Child is alert and responsive
Respiratory rate even and nonlabored at rate of 24/min. No adventitious sounds auscultated.
Heart rate 108/min
Generalized small clusters of reddish, scaly patches with lichenifications and depigmentation on the child's bilateral upper and lower extremities.
Which of the following statements should the nurse plan to include in the discharge instructions for the child's guardian?
Select all that apply.
Explanation
Rationale:
A. Cutting and filing the child's fingernails frequently can help prevent further damage from scratching and reduce the risk of infection.
B. Using a mild detergent for the child's laundry can help minimize irritation to the skin.
C. Pimecrolimus cream is a topical immunomodulator that may be used for atopic dermatitis, but the thick layer application is not typically recommended for children due to safety concerns.
D. Informing the guardian that the child will experience occasional flare-ups of the condition helps manage expectations and prepares them for potential recurrence.
E. Atopic dermatitis is not typically contagious, so the statement that the child's condition is contagious when lesions are present is inaccurate.
F. Applying gloves to the child's hands can prevent scratching and further damage to the skin.
G. Applying emollients to the child's skin after bathing helps maintain skin hydration and barrier function, reducing the severity of atopic dermatitis symptoms.
Exhibit 3 Diagnostic Results Cerebrospinal fluid
Pressure: 22 cm H,O (less than 20 cm H2O) Color: Cloudy (clear or colorless)
Blood: None (none)
Cells
RBC: 0 (0)
WBC: 36 cells/mcL (0 to 30 cells/mcL) Protein: 92 mg/dL (up to 70 mg/dL) Glucose: 36 mg/dL (50 to 75 mg/dL)
Serum glucose: 64 mg/dL (60 to 100 mg/dL)
A nurse in an emergency department is caring for a 3-month-old infant. Which of the following actions should the nurse take? (Click on the "Exhibit" button for additional information about the client. There are three tabs that contain separate categories of data.)
Explanation
Rationale:
A. Given the cloudy appearance of the cerebrospinal fluid (CSF) and elevated white blood cell count (WBC) in the CSF, there may be an indication of meningitis.
Ceftriaxone is a broad-spectrum antibiotic commonly used to treat bacterial meningitis. Therefore, administering ceftriaxone would be an appropriate action.
B. While vaccines are important for preventing infections, administering the pneumococcal conjugate vaccine is not the immediate priority in this scenario. The patient is already exhibiting signs of a potential infection, and treatment should focus on addressing the current condition first.
C. The infant's serum glucose level is low at 64 mg/dL (normal range: 60 to 100 mg/dL).
However, the primary concern at this moment appears to be the potential bacterial meningitis indicated by the cloudy CSF, elevated WBC count, and abnormal CSF glucose level. While monitoring serum glucose is important, it is not the most critical action in this case.
D. Neutropenic precautions are typically implemented to protect patients with low neutrophil counts (neutropenia) from acquiring infections. However, there is no indication of neutropenia in the provided diagnostic results. Additionally, the cloudy CSF and elevated WBC count suggest a possible bacterial infection rather than a neutropenic condition.
Explanation
Rationale:
A. This amount of drainage may be expected postoperatively, and it is not indicative of a significant issue.
B. This is a concerning finding indicating possible inadequate renal perfusion, especially considering the postoperative status of the toddler.
C. While slightly lower than the typical body temperature, it is not necessarily abnormal, particularly in a postoperative setting.
D. Pulses of 2+ indicate adequate perfusion and are not concerning.
A nurse is assessing a school-age child who is receiving morphine. For which of the following adverse effects should the nurse monitor?
Explanation
Rationale:
A. This is not a common adverse effect associated with morphine.
B. Nausea is a common adverse effect of morphine and should be monitored for, particularly in pediatric patients.
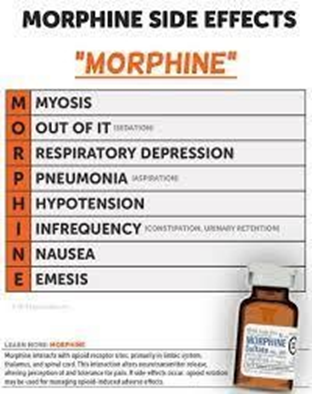
C. Stevens-Johnson syndrome is a severe allergic reaction and is not typically associated with morphine.
D. While morphine can cause urinary retention, it is not typically associated with renal failure.
Explanation
Rationale:
A. Cyanosis can occur in children with heart failure due to inadequate oxygenation of tissues.
B. Weight gain or fluid retention is more common in children with heart failure.
C. Bounding pulses are more commonly associated with conditions such as hypertension or hyperthyroidism, rather than heart failure.
D. Dyspnea, or difficulty breathing, is a common symptom of heart failure due to fluid buildup in the lungs.
E. Tachycardia, or a rapid heart rate, can occur as a compensatory mechanism in response to decreased cardiac output in heart failure.
Explanation
Rationale:
A. Mood swings are a common side effect of prednisone and indicate an understanding of the potential adverse effects.
B. Routine blood tests are not typically required for children on maintenance prednisone therapy for asthma.
C. Prednisone should not be withheld before physical activity, as it is a maintenance medication for asthma.
D. Decreased appetite is a common side effect of prednisone but is not the best indicator of understanding the teaching.
A nurse is caring for a child whose guardian requests information about essential oils to help their child relax. Which of the following oils should the nurse recommend?
Explanation
Rationale:
A. Lavender oil is commonly used for relaxation and calming effects.

B. Eucalyptus oil is more commonly used for respiratory issues and may not be as suitable for relaxation.
C. Jasmine oil is often used for its pleasant scent but may not have the same relaxation properties as lavender.
D. Tea tree oil is typically used for its antimicrobial properties and may not be as effective for relaxation purposes as lavender.
Explanation
Rationale:
A. The MMR vaccine is typically administered at 12 months of age as part of routine immunization schedules.
B. The varicella vaccine is typically administered at 12 months of age as part of routine immunization schedules.
C. Rotavirus (RV): The rotavirus vaccine is typically administered at 2, 4, and 6 months of age.
D. The herpes zoster vaccine is not routinely administered to infants at 12 months of age.
E. The HPV vaccine is typically administered starting at age 11 or 12 years, not at 12 months of age.
Explanation
Rationale:
A. Observing the child's throat with a flashlight is necessary to detect any bleeding.
B. Giving the child small sips of water helps soothe the throat and promote hydration but it does not address the risk of bleeding as a complication of tonsillectomy.
C. Administering an analgesic may be indicated if the child is experiencing pain, but the throat should be assessed for any bleeding first.
D. Offering the child an ice collar may provide comfort, but assessing the throat for any bleeding is more essential.
Explanation
Rationale:
A. Tachypnea (rapid breathing) is a common clinical manifestation of heart failure due to decreased cardiac output and inadequate tissue perfusion.
B. Tremors are not typically associated with heart failure.
C. Increased appetite is not typically associated with heart failure and may even be decreased due to symptoms such as fatigue and dyspnea.
D. Bradycardia (slow heart rate) is not typically associated with heart failure; instead, tachycardia (rapid heart rate) may occur as a compensatory mechanism.
A nurse is caring for a school-age child who has diabetes mellitus. Which of the following findings should the nurse recognize as being consistent with hyperglycemia?
Explanation
Rationale:
A. Sweating is more commonly associated with hypoglycemia (low blood sugar) rather than hyperglycemia (high blood sugar).
B. Tremors are more commonly associated with hypoglycemia.
C. Pallor is not typically associated with hyperglycemia.
D. Thirst (polydipsia) is a classic symptom of hyperglycemia in diabetes mellitus, as the body tries to dilute the excess sugar in the bloodstream by increasing fluid intake.
Explanation
Rationale:
A. This statement describes peritoneal dialysis, not hemodialysis.
B. Hemodialysis does not use an electrolyte solution to clean the blood.
C. Hemodialysis indeed involves circulating the blood outside the body through an artificial membrane in the dialysis machine to remove waste products and excess fluids.
D. Hemodialysis involves intermittent filtration of the blood, not continuous filtration.
Sign Up or Login to view all the 55 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

