Ati RN Pharmacology 2019 - Exam 3
Total Questions : 60
Showing 25 questions, Sign in for moreA nurse is teaching a client who has a prescription for ferrous gluconate. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A rationale:
Taking ferrous gluconate with milk can reduce its absorption due to the presence of calcium.
Choice B rationale:
Notifying the provider about black stools is important because it could indicate gastrointestinal bleeding, a potential side effect of iron supplementation.
Choice C rationale:
Taking an antacid with ferrous gluconate can reduce its absorption due to increased gastric pH.
Choice D rationale:
Staying upright after taking the medication helps prevent esophageal irritation, but it is not the most relevant response indicating understanding of the teaching.

A nurse is caring for a client who has tuberculosis and is taking isoniazid and rifampin. Which of the following outcomes indicates that the client is adhering to the medication regimen?
Explanation
Choice A rationale:
Testing negative for HIV does not mean that the client is taking the antibiotics as prescribed. HIV is a virus that weakens the immune system and makes people more susceptible to tuberculosis, but it is not related to the medication regimen for tuberculosis.
Choice B rationale:
having a positive purified protein derivative test does not mean that the client is taking the antibiotics as prescribed. A purified protein derivative test is a skin test that checks for exposure to tuberculosis bacteria, but it does not measure the effectiveness of the medication regimen. A positive test means that the client has been exposed to tuberculosis bacteria at some point in their life, but it does not mean that they have an active infection or that they are taking the antibiotics as prescribed.
Choice C rationale:
The client has a negative sputum culture. A sputum culture is a test that checks for the presence of tuberculosis bacteria in the mucus that is coughed up from the lungs. A negative sputum culture means that the bacteria are no longer detectable and that the medication regimen is effective. A positive sputum culture means that the bacteria are still present and that the medication regimen may need to be adjusted.
Choice D rationale:
Having normal liver function test results does not mean that the client is taking the antibiotics as prescribed. Liver function tests are blood tests that check for damage to the liver caused by medications or other factors. Isoniazid and rifampin can cause liver damage, so the nurse should monitor the client's liver function tests regularly to prevent or detect any problems. However, having normal liver function test results does not mean that the client is taking the antibiotics as prescribed or that the medication regimen is effective.
A nurse is caring for a client who has heart failure and monitor when administering lisinopril?
Explanation
Choice A rationale:
Bradycardia (slow heart rate) is not a primary concern when administering lisinopril.
Choice B rationale:
Hypokalemia (low potassium levels) can be a concern with certain medications, but it is not directly related to lisinopril administration.
Choice C rationale:
Lisinopril is an angiotensin-converting enzyme (ACE) inhibitor commonly used to treat heart failure. One of the potential side effects of ACE inhibitors is hypotension (low blood pressure), so the nurse should monitor the client's blood pressure closely during and after administration.
Choice D rationale:
Tinnitus (ringing in the ears) is not a common side effect of lisinopril.
A nurse is preparing to initiate IV therapy for a client. Which of the following sites should the nurse use to place the peripheral IV catheter?
Explanation
Choice A rationale:
The dorsal vein is not typically used for peripheral IV catheter placement due to its location and potential for complications.
Choice B rationale:
The nondominant forearm basilic vein is a common site for peripheral IV catheter placement due to its accessibility and stability.
Choice C rationale:
The distal dorsal vein is not a common site for peripheral IV catheter placement.
Choice D rationale:
The antecubital basilic vein can be used, but the nondominant forearm basilic vein is often preferred for peripheral IV catheter placement due to its accessibility and stability.
A nurse is reviewing the laboratory results of a client who is taking amitriptyline. Which of the following laboratory values should the nurse report to the provider?
Explanation
Choice A rationale:
A hematocrit (Hct) value of 44% is within the expected range and does not require immediate reporting.
Choice B rationale:
A white blood cell (WBC) count of 5,000/mm3 falls within the normal range and does not require immediate reporting.
Choice C rationale:
Elevated total bilirubin levels can indicate potential liver dysfunction, which can be a concern when a client is taking medications like amitriptyline. The nurse should report this value for further evaluation.
Choice D rationale:
A potassium level of 4.2 mEq/L is within the normal range and does not require immediate reporting.
A nurse is caring for a client who develops an anaphylactic reaction to IV antibiotic administration. After assessing the client's respiratory status and stopping the medication infusion, which of the following actions should the nurse take next?
Explanation
Choice A rationale:
While diphenhydramine is used to manage allergic reactions, epinephrine is the first-line treatment for severe anaphylactic reactions.
Choice B rationale:
In cases of anaphylactic reactions, epinephrine is the first-line treatment to reverse the severe allergic response. It helps to relieve bronchoconstriction, improve blood pressure, and counteract the symptoms of anaphylaxis.
Choice C rationale:
Elevating the client's legs and feet is not the appropriate intervention for anaphylactic reactions.
Choice D rationale:
Replacing the infusion with 0.9% sodium chloride is not the priority action in managing anaphylactic reactions. Administering epinephrine and managing the client's airway and circulation are more important.
A nurse is caring for a client who is taking lithium and reports starting a new exercise program. The nurse should assess the client for which of the following electrolyte imbalances?
Explanation
Choice A rationale:
Hypomagnesemia involves a deficiency of magnesium, and it's not directly related to starting an exercise program while taking lithium.
Choice B rationale:
Hypokalemia involves low levels of potassium, which might not be directly influenced by the client's exercise program.
Choice C rationale:
Hypocalcemia involves low levels of calcium, and exercise is not a primary factor affecting calcium balance.
Choice D rationale:
Hyponatremia involves low levels of sodium in the blood. Starting a new exercise program while taking lithium can lead to increased sweating, potentially causing a loss of sodium. Lithium itself can also impact sodium levels. Monitoring for hyponatremia is important due to its potential impact on lithium toxicity.
A nurse is caring for a client who is taking triamterene. For which of the following laboratory values should the nurse withhold the medication?
Explanation
Choice A rationale:
BUN (blood urea nitrogen) measures kidney function and hydration status but is not a specific indicator for withholding triamterene.
Choice B rationale:
Triamterene is a potassium-sparing diuretic. With a potassium level of 5.3 mEq/L, which is elevated, the nurse should withhold the medication to prevent further potassium retention.
Choice C rationale:
Sodium level of 142 mEq/L is within the normal range and does not indicate a need to withhold triamterene.
Choice D rationale:
Albumin level of 4 g/dL is within the normal range and does not directly impact the decision to withhold triamterene.
A nurse is assessing a client who is taking an osmotic laxative. Which of the following findings should the nurse identify as an indication of fluid volume deficit?
Explanation
Choice A rationale:
Weight gain is not typically associated with fluid volume deficit; it's more indicative of fluid retention.
Choice B rationale:
Oliguria refers to decreased urine output and can be a sign of fluid volume deficit.
Choice C rationale:
Nausea can be caused by various factors, including gastrointestinal issues, but it's not a specific indicator of fluid volume deficit.
Choice D rationale:
Headaches can have multiple causes and are not a direct sign of fluid volume deficit.
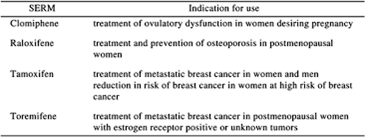
A nurse is consulting a formulary about a client's new prescription for raloxifene. The nurse should identify that this medication is used to treat which of the following conditions?
Explanation
Choice A rationale:
Raloxifene is not used to treat urinary tract infections.
Choice B rationale:
Raloxifene is not used to treat deep-vein thrombosis.
Choice C rationale:
Raloxifene is a medication used to treat and prevent osteoporosis in postmenopausal women. It helps to prevent bone loss and reduce the risk of fractures.
Choice D rationale:
Raloxifene is not used to treat hypothyroidism; it's primarily focused on bone health.
A nurse is planning care for a client who is receiving morphine via continuous epidural infusion. The nurse should monitor the client for which of the following adverse effects?
Explanation
Choice A rationale:
Pruritus, or itching, is a common adverse effect of opioid medications like morphine.
Choice B rationale:
Gastric bleeding is not a typical adverse effect of morphine administered via epidural infusion.
Choice C rationale:
Tachypnea, or rapid breathing, is not a common adverse effect of morphine. It's more commonly associated with opioid overdose.
Choice D rationale:
Cough is not a prominent adverse effect of morphine administered via epidural infusion.
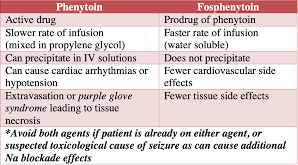
A nurse is assessing a client after administering phenytoin IV bolus for a seizure. Which of the following findings should the nurse identify as an adverse effect of this medication?
Explanation
Choice A rationale:
Red man syndrome is associated with vancomycin, not phenytoin.
Choice B rationale:
Hypotension, or low blood pressure, can be an adverse effect of phenytoin.
Choice C rationale:
Hypoglycemia is not a typical adverse effect of phenytoin.
Choice D rationale:
Bradycardia is not a common adverse effect of phenytoin.
A nurse is providing teaching to a client who has a new prescription for clozapine. Which of the following statements should the nurse include in the teaching?
Explanation
Choice A rationale:
Ringing in the ears is not typically associated with clozapine.
Choice B rationale:
Diarrhea is not a common adverse effect of clozapine.
Choice C rationale:
Clozapine can cause agranulocytosis, a serious condition involving a decrease in white blood cells. Fever can be a sign of infection, so clients taking clozapine should notify their provider if they develop a fever.
Choice D rationale:
Weight loss is not a common adverse effect of clozapine.
A nurse recently administered filgrastim intravenously to a client who has ccer and is receiving cytotoxic chemotherapy. For which of the following data, discovered after the medication was administered, should the nurse file an incident report?
Explanation
Choice A rationale:
Flushing the IV line is a routine action and not a reason for filing an incident report.
Choice B rationale:
An absolute neutrophil count of 2.500/mm3 is not an alarming finding and doesn't necessitate an incident report.
Choice C rationale:
Administering filgrastim within close proximity to cytotoxic chemotherapy can increase the risk of bone pain and other complications. This situation requires an incident report for further investigation.
Choice D rationale:
Allowing the medication vial to sit at room temperature for 2 hours before administration is not a critical error that warrants an incident report.
A nurse is reviewing the medical record of an adult client who has a fever and a prescription for acetaminophen. Which of the following findings should the nurse identify as a contraindication for receiving this medication?
Explanation
Choice A rationale:
Alcohol use disorder is not a contraindication for receiving acetaminophen.
Choice B rationale:
Chronic kidney disease may require dose adjustments but is not an absolute contraindication for acetaminophen.
Choice C rationale:
Receiving a hepatitis B vaccine within the last week can lead to potential interactions or adverse effects when taking acetaminophen. The body's immune response to the vaccine can be affected.
Choice D rationale:
Diabetes mellitus is not a contraindication for receiving acetaminophen.
A nurse is administering naloxone to a client who has developed an adverse action to morphine. The nurse should identify which of the following findings as a therapeutic effect of naloxone?
Explanation
Choice A rationale:
Naloxone is an opioid antagonist and does not increase pain relief.
Choice B rationale:
Naloxone is used to reverse opioid overdose, and an increased respiratory rate is a therapeutic effect, as it helps to counteract the respiratory depression caused by opioids.
Choice C rationale:
Decreased blood pressure is not a therapeutic effect of naloxone.
Choice D rationale:
Naloxone is not used to treat nausea directly.
A nurse is assessing for allergies with a client who is scheduled to receive the influenza vaccine. Which of the following allergies should the nurse report to the provider as a possible contraindication to receiving the vaccine?
Explanation
Choice A rationale:
Peanuts are not directly related to influenza vaccine contraindications.
Choice B rationale:
Shellfish allergies are not directly related to influenza vaccine contraindications.
Choice C rationale:
Milk allergies are not directly related to influenza vaccine contraindications.
Choice D rationale:
Influenza vaccines are typically grown in eggs and may contain trace amounts of egg protein. A severe egg allergy can be a contraindication for receiving the influenza vaccine due to the risk of an allergic reaction.
A nurse is caring for a client who is taking digoxin to treat heart failure. Which of the following factors predisposes this client to developing digoxin toxicity?
Explanation
Choice A rationale:
Taking an HMG-CoA reductase inhibitor (statin) is not directly related to digoxin toxicity.
Choice B rationale:
Having a prolapsed mitral valve is not a known risk factor for digoxin toxicity.
Choice C rationale:
Having a history of COPD is not directly associated with digoxin toxicity.
Choice D rationale:
High-ceiling diuretics (loop diuretics) can lead to electrolyte imbalances, such as hypokalemia, which can increase the risk of digoxin toxicity. Potassium plays a role in the effects of digoxin on the heart, and low levels can potentiate toxicity.
A nurse is reviewing the medical record of a client who has sinusitis and a nem prescription for cefuroxime. Which of the following client information is the priority for the nurse to report to the provider?
Explanation
Choice A rationale:
A history of nausea with cefuroxime is a common side effect and may not be the highest priority to report.
Choice B rationale:
A BUN level of 18 mg/dL is within the normal range and may not be an immediate concern.
Choice C rationale:
Taking aspirin daily may have some interactions with cefuroxime, but a history of a severe penicillin allergy is more critical to report.
Choice D rationale:
Cefuroxime is a cephalosporin antibiotic, and individuals with a severe penicillin allergy may have an increased risk of cross-reactivity with cephalosporins. This history should be reported to the provider for further assessment and consideration of alternative antibiotics.
A nurse is administering naloxone to a client who has developed an adverse action to morphine. The nurse should identify which of the following findings as a therapeutic effect of naloxone?
Explanation
Choice A rationale:
Increased pain relief is not a therapeutic effect of naloxone, but rather an adverse effect of morphine. Naloxone would reduce the analgesic effect of morphine and increase the pain sensation in the client.
Choice B rationale:
Naloxone is an opioid antagonist that reverses the effects of opioids, such as morphine, on the central nervous system. One of the main adverse effects of opioids is respiratory depression, which can lead to hypoxia and death. Naloxone restores normal breathing by blocking the opioid receptors in the brain and spinal cord. Therefore, a therapeutic effect of naloxone is increased respiratory rate.
Choice C rationale:
Decreased blood pressure is not a therapeutic effect of naloxone, but rather a possible side effect of morphine. Naloxone would not affect the blood pressure significantly, unless the client had severe hypotension due to opioid overdose.
Choice D rationale:
Decreased nausea is not a therapeutic effect of naloxone, but rather a possible side effect of morphine. Naloxone would not affect the gastrointestinal system, unless the client had severe nausea and vomiting due to opioid overdose.
A nurse is monitoring for an infusion reaction for a client who is receiving a dose of IV amphotericin B. Which of the following findings should indicate to the nurse that the client is experiencing an acute infusion reaction?
Explanation
Choice A rationale:
Hyperglycemia is not typically associated with an acute infusion reaction to amphotericin B.
Choice B rationale:
A dry cough is a common side effect of amphotericin B, but it is not an indicator of an acute infusion reaction.
Choice C rationale:
Pedal edema is not a typical sign of an acute infusion reaction to amphotericin B.
Choice D rationale:
Fever, along with other symptoms like chills, fever, nausea, and vomiting, can be indicative of an acute infusion reaction to amphotericin B. It may require stopping the infusion and providing appropriate treatment.
A client who has Graves' disease is prescribed methimazole. Which of the following effects should the nurse expect to see after the client has taken the medication for 2 months?
Explanation
Choice A rationale:
Methimazole does not typically affect skin temperature.
Choice B rationale:
Methimazole is used to treat hyperthyroidism, so a decrease in pulse rate would be expected, not an increase.
Choice C rationale:
Increased sleeping is not a typical effect of methimazole.
Choice D rationale:
Methimazole is used to treat hyperthyroidism by reducing thyroid hormone production. As a result, weight loss is a common effect due to the normalization of metabolic activity.
A nurse is reviewing the list of current medications for a client who is to start a new prescription for carbamazepine. The nurse should identify that which of the following medications interacts with carbamazepine?
Explanation
Choice A rationale:
Nicotine transdermal system is not known to have a significant interaction with carbamazepine.
Choice B rationale:
Beclomethasone is not known to have a significant interaction with carbamazepine.
Choice C rationale:
Carbamazepine can induce the metabolism of estrogen and progestin, potentially reducing their effectiveness in birth control. Women taking these combinations should use alternative contraceptive methods.
Choice D rationale:
Diphenhydramine is not known to have a significant interaction with carbamazepine.
A nurse is assessing a client who has hypermagnesemia. Which of the following medications should the nurse prepare to administer?
Explanation
Choice A rationale:
Calcium gluconate is used to treat hypermagnesemia by antagonizing the effects of excess magnesium and reducing its impact on cardiac function.
Choice B rationale:
Flumazenil is used to reverse the effects of benzodiazepine overdose, not to treat hypermagnesemia.
Choice C rationale:
Protamine sulfate is used to reverse the effects of heparin, not to treat hypermagnesemia.
Choice D rationale:
Acetylcysteine is used to treat acetaminophen overdose, not to treat hypermagnesemia.
A nurse is teaching a guardian of a school-age child who has a new prescription for a fluticasone metered-dose inhaler. Which of the following information should the nurse include in the teaching? (Select all that apply.)
Explanation
Choice A rationale:
The nurse should teach the guardian to shake the device prior to administration to ensure that the medication is well mixed and delivered in the right dose.
Choice B rationale:
Soaking the inhaler in water is not a recommended action as this can damage the device and affect its function.
Choice C rationale:
The nurse should also teach the guardian to use a spacer with the inhaler, which is a device that attaches to the mouthpiece and helps deliver the medication more effectively to the lungs.
Choice D rationale:
The nurse should also not teach the guardian to have the child take one inhalation as needed for shortness of breath, as fluticasone is a long-acting corticosteroid that is used for maintenance therapy and prevention of asthma symptoms, not for acute relief. The child should have a separate rescue inhaler, such as albuterol, for quick relief of bronchospasm.
Choice E rationale
The nurse should instruct the guardian to rinse the child's mouth with water after using the inhaler to prevent oral candidiasis, which is a fungal infection that can occur from the steroid medication.

Sign Up or Login to view all the 60 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

