Ati RN Psychtriac Nursing
Total Questions : 49
Showing 25 questions, Sign in for moreA nurse is caring for a client who has major depressive disorder (MDD). Which of the following findings should the nurse expect?
Explanation
A. Clients with major depressive disorder often exhibit decreased response to stimuli rather than an exaggerated response.
B. Weight changes, either a significant gain or loss, are common in individuals with major depressive disorder due to changes in appetite.
C. Hyperexcitability is not typically associated with major depressive disorder. Instead, individuals with depression often exhibit decreased energy and enthusiasm.
D. While seeking attention can manifest in some individuals with mental health conditions, it's not a defining characteristic of major depressive disorder.

A nurse in an acute care mental health facility is caring for a client who has depression. After 3 days of treatment, the nurse notices that the client suddenly seems cheerful and relaxed and there are no longer signs of a depressive state. Which of the following interventions is appropriate to include in the plan of care?
Explanation
A. While social support is essential, sudden changes in behavior warrant assessment and understanding before taking the client outside the facility.
B. Monitoring might be necessary but does not directly address the reason behind the sudden change in behavior.
C. This approach may reinforce the behavior without addressing the underlying cause.
D. This intervention is crucial for assessment and understanding the sudden shift in the client's mood, which could provide insight into the effectiveness of the treatment or other factors contributing to the change.
A nurse is discussing legal exceptions to client confidentiality with nursing staff. Which of the following statements by a staff member indicates an understanding of the teaching?
Explanation
A. This statement refers to the "duty to warn," a legal obligation to protect third parties if a client expresses a serious threat of harm to others. It's a crucial exception to confidentiality.
B. This statement is inaccurate as there are scenarios where healthcare workers are legally required to provide information to the court.
C. This statement is not entirely accurate; there are legal boundaries and requirements for disclosing client information to attorneys.
D. Confidentiality extends even after a client's death in many situations, but there are exceptions based on state laws and ethical guidelines.
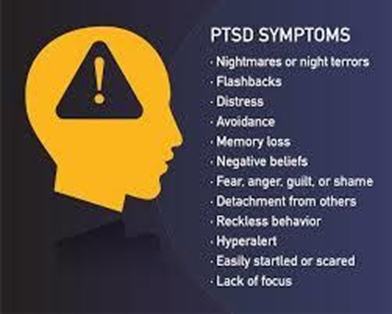
Which experiences are most likely to precipitate posttraumatic stress disorder (PTSD)? (Select all that apply.)
Explanation
A. Experiencing a life-threatening event such as being trapped can precipitate PTSD.
B. Exposure to an R-rated movie, while potentially distressing, is not typically considered a traumatic event that leads to PTSD.
C. Prolonged exposure to traumatic events like abduction and captivity often leads to PTSD due to the severe and chronic trauma experienced.
D. This is not typically considered a traumatic event leading to PTSD as it's a voluntary, recreational activity that involves perceived safety measures.
A nurse is caring for a client following a suicide attempt. The client has a history of depression, substance abuse, and anorexia nervosa. Which of the following actions is the nurse's priority?
Explanation
A. While assessing depression is crucial, in a situation following a suicide attempt, the immediate safety of the client takes precedence.
B. While ensuring the client's nutrition is important, safety regarding the recent suicide attempt is the priority.
C. This is relevant to the situation but doesn't directly address the immediate risk of self-harm or suicide.
D. Given the client's history of a suicide attempt and the present situation, initiating measures to ensure the client's safety and prevent any further harm, such as suicide precautions, is the priority.
A nurse is caring for a client who was admitted for suspected abuse. The client is quiet and withdrawn. Which of the following actions should the nurse take to promote client communication?
Explanation
A. While family involvement can be beneficial, it might not directly promote communication with the client who may feel more comfortable without others present initially.
B. While important, addressing physical injuries doesn't directly address the need for communication.
C. Creating an environment of trust and honesty encourages communication and may help the client feel comfortable to share information.
D. While gathering information is important, pressuring the client with probing questions might be counterproductive, causing the client to withdraw further.
A nurse is caring for a client who was involved in heavy combat and observed war casualties. The nurse should suspect that the client is suffering from posttraumatic stress disorder (PTSD) if the client makes which of the following statements?
Explanation
A. This statement reflects concern about a potential cause of a birth defect, not necessarily PTSD symptoms.
B. This statement indicates recurrent nightmares, a potential symptom of PTSD, but it doesn't involve the persistent feeling of threat.
C. This statement reflects hypervigilance and persistent feelings of threat, a common symptom of PTSD.
D. While this statement might be related to combat experience, it doesn't necessarily indicate PTSD.
A patient with suicidal impulses is on the highest level of suicide precautions. Which measures should the nurse incorporate into the patient's plan of care? (Select all that apply.)
Explanation
A. This precaution helps eliminate potential means for self-harm.
B. Regular checks and verbal contact are essential to monitor the patient's safety and provide support.
C. Removing objects that could be used for self-harm is a key part of suicide precautions.
D. While this is an intensive level of observation, it might not be feasible at all times due to staffing limitations, making this choice less practical than the others.
A nurse interacts with a newly hospitalized patient. Which nursing statement reflects the communication technique of "offering self"?
Explanation
A. This statement demonstrates the nurse's willingness to spend time with the patient to build rapport and trust, offering the nurse's presence and support.
B. This statement expresses hope but doesn't directly offer the nurse's presence or support.
C. This question encourages exploration of the patient's feelings but doesn't directly offer the nurse's presence.
D. This statement shares personal experiences but doesn't directly offer the nurse's presence or support.
A nurse is caring for a client who has delusional behavior and states, "I can't go to group therapy today. I am expecting a high-level official to visit me!" The nurse responds, "I understand, but it is time for group therapy and we expect everyone to attend. Let's walk over together." For which of the following reasons is the nurse's response considered therapeutic?
Explanation
A. While the nurse's response is supportive, it primarily focuses on setting boundaries rather than solely displaying empathy.
B. This response does communicate expectations, but the therapeutic value primarily lies in setting boundaries.
C. The nurse's response acknowledges the client's delusional belief while gently setting limits by encouraging attendance at group therapy, a structured therapeutic activity.
D. Reflection involves restating or exploring the client's feelings or statements. In this scenario, the nurse is redirecting the client to attend group therapy rather than reflecting the delusional belief.
A nurse in a psychiatric unit is admitting a client who attacked a neighbor. The nurse should know that the client can be kept in the hospital after the 72-hr hold is over for which of the following conditions?
Explanation
A. This alone might not be a sufficient reason for involuntary commitment. The key factor for extended hospitalization is a threat to safety.
B. Moving out of the state might not justify extended hospitalization if there's no indication of imminent danger.
C. Personal dislike, without posing an immediate danger, might not be sufficient for extended hospitalization.
D. If the client continues to pose a risk of harm to herself or others, involuntary hospitalization beyond the initial hold might be warranted.
A nurse caring for a patient prescribed a selective serotonin reuptake inhibitor (SSRI) will develop outcome criteria related to what outcome?
Explanation
A. Extrapyramidal symptoms are more commonly associated with antipsychotic medications rather than SSRIs.
B. SSRIs might have varying effects on motor activity, but this is not a primary outcome for their use.
C. While SSRIs may indirectly contribute to cognitive improvements, the primary expected outcome revolves around mood changes rather than thought processes.
D. SSRIs are primarily used to treat mood disorders like depression and anxiety, and the main goal of their use is to improve mood and emotional symptoms. Therefore, the expected outcome criteria often relate to mood improvement.
A soldier returns to the United States from active duty in a combat zone. The soldier is diagnosed with posttraumatic stress disorder (PTSD). The nurse's highest priority is to screen this soldier for which problem?
Explanation
A. While both schizophrenia and PTSD are mental health disorders, the priority in this context for a soldier with a history of combat exposure is to screen for conditions that commonly arise from traumatic experiences, such as PTSD and major depressive disorder.
B. PTSD and major depressive disorder can often co-occur, especially in individuals exposed to trauma. Given the soldier's history of combat exposure and PTSD diagnosis, screening for major depressive disorder is crucial due to its frequent association with PTSD and its potential severity.
C. Bipolar disorder may share some symptoms with PTSD, but given the context of returning from combat and the diagnosis of PTSD, the priority would be to focus on screening for
conditions more directly linked to trauma.
D. Dementia is less likely to be directly related to combat exposure in a returning soldier. While it's essential to assess the soldier's overall mental health, the immediate concern in this scenario would be mental health conditions more commonly associated with trauma.

A client has made a successful suicide attempt while hospitalized on a unit that specializes in the treatment of depression. When considering both milieu control and crisis management, which intervention will the nursing staff implement?
Explanation
A. While assessing the impact of a suicide attempt on others is important, the immediate focus following a successful suicide attempt in a mental health unit is to ensure the safety of all clients.
B. Restricting group therapy for 72 hours might impede the therapeutic process and does not directly address the safety of clients after a suicide attempt.
C. Following a suicide attempt, it's standard practice to heighten monitoring and implement suicide precautions for all clients to ensure their safety.
D. While assessing the situation is important, immediate intervention to prevent further harm to other clients is a priority following a suicide attempt. The psychological assessment might occur but would not be the primary intervention in this immediate crisis situation.
A patient diagnosed with major depressive disorder was hospitalized for 8 days. Treatment included six electroconvulsive therapy sessions and aggressive dose adjustments of antidepressant medications. The patient owns a small business and was counseled not to make major decisions for a month. Select the correct rationale for this counseling.
Explanation
A. This is not the primary reason for the counseling. The decision-making recommendation is
more related to the effects of the electroconvulsive therapy and the need for the patient to recover from its associated side effects.
B. While readjustment to a work schedule might be a consideration, the primary reason for counseling against major decisions for a month is related to the potential side effects of
electroconvulsive therapy.
C. Temporary memory impairments and confusion are potential side effects of electroconvulsive therapy, which might interfere with decision-making abilities, hence the advice to refrain from major decisions.
D. Antidepressant medications causing confusion related to dietary limitations with tyramine is not directly relevant to the counseling against making major decisions after electroconvulsive therapy.
A nurse in a mental health facility is caring for a client who has major depressive disorder.
Progress Notes
Week 1
Client is experiencing major depressive disorder following the unexpected death of their partner 6 months ago. Has been unable to proceed through stages of grief. Has been on anti-depressant therapy for 5 months.
Admits to having thoughts of self-harm. Reports increasing anxiety levels. Loss of 15 lb over past months due to anorexia and anxiety. Reports insomnia, sleeping only 4 to 5 hr/night with frequent nightmares. Reports feelings of extreme fatigue.
Plan: Admit for group and individual therapy. Suicide precautions. Will add alprazolam to medication regimen.
Week 2
Client remains depressed, continues to have thoughts of self-harm. Not responding to group or individual therapy. States no improvement in mood or energy level. Admits to less anxiety and increased hours and quality of nightly sleep with addition of alprazolam. Anorexia still present.
Plan: Due to ineffectiveness of antidepressant regimen and psychotherapy, suggest addition of electroconvulsive therapy (ECT).
Medication Administration Record
Bupropion 100 mg PO TID
Escitalopram 20 mg PO daily
Alprazolam 0.25 PO BID PRN anxiety
Which of the following items in the client's medical record indicate that they are a candidate for electroconvulsive therapy (ECT)?
(Select all that apply.)
Explanation
A. Indication for ECT. The client reports extreme fatigue despite treatment, suggesting a lack of improvement in energy levels with medication and therapy.
B. Indication for ECT. The client has not shown significant improvement in response to antidepressant therapy, as stated in the progress notes.
C. Not an indication since the client reports increased hours and better quality of sleep.
D. Potential indication for ECT. The client has anorexia, which indicates a persistent lack of appetite despite the treatment received.
E. Mixed indication. While alprazolam has helped with anxiety and improved sleep, it hasn't resolved the underlying depressive symptoms or suicidal thoughts. Therefore, it might contribute to considering ECT as an alternative or additional therapy option.
A nurse in an acute mental health facility is caring for a client who jumps out of her chair and begins to shout angrily at the clients around her. Which of the following actions should the nurse take first?
Explanation
A. Restraining the client should be a last resort and is not the initial action to take when managing an agitated client.
B. Seclusion should also be considered as a last resort, and de-escalation techniques should be attempted before secluding the client.
C. Speaking calmly and providing simple directions can help de-escalate the situation by promoting a calm environment and reducing stimuli that may exacerbate the client's agitation.
D. While medication might be necessary in some cases, it's not the first action to take when a client becomes agitated.
A charge nurse is conducting a staff education in-service about depressive disorders. Which of the following should the nurse identify as a risk factor for depression?
Explanation
A. Being married might have protective factors against depression for some individuals due to social support; however, it's not universally a risk factor.
B. Chronic illness, due to its impact on quality of life, pain, and coping mechanisms, is a well-known risk factor for developing depression.
C. While depression can affect anyone regardless of gender, it's not accurate to label male gender as a risk factor in itself.
D. Pregnancy can be associated with perinatal mood disorders like postpartum depression, but it's not a universal risk factor for depression in all cases.

A patient cries as the nurse explores the patient's relationship with a deceased parent. The patient says, "I shouldn't be crying like this. It happened a long time ago." Which responses by the nurse will facilitate communication? (Select all that apply.)
Explanation
A. This response invalidates the patient's feelings and avoids addressing the emotion, hindering communication.
B. Acknowledging the patient's emotion validates their feelings and encourages further discussion.
C. Validates the patient's emotional expression and offers understanding.
D. Acknowledges the depth of the patient's pain and encourages expression without judgment.
An individual has been diagnosed with a dissociative disorder. Which comorbid psychiatric disorders are most likely to accompany this type of mental illness? (Select all that apply.)
Explanation
A. Dissociative disorders can coexist with personality disorders, as both involve disruptions in self-identity and behavior.
B. Individuals with dissociative disorders may use substances to cope with symptoms or distress.
C. While dissociative disorders and eating disorders share some symptoms, they are not commonly identified as comorbid conditions.
D. It is common for dissociative disorders to co-occur with depressive disorders due to shared symptoms and overlapping psychological factors.
A nurse is providing teaching for a client who has major depressive disorder and is seeking voluntary admission to an acute mental health facility. Which of the following statements should the nurse include?
Explanation
A. This statement is not necessarily accurate and could cause undue concern. Providers are not typically required to notify employers of a patient's admission to a mental health facility due to confidentiality regulations.
B. Informed consent for treatments, interventions, or medications is an ongoing process, and the client maintains this right even after admission to the facility. It's crucial to ensure the client
understands this.
C. While there are restrictions on leaving against medical advice (AMA) in some situations, the statement is too absolute. The client's ability to leave might depend on specific circumstances.
D. This statement is not entirely true. Even in an inpatient setting, patients generally have the right to refuse medications, although there might be discussions about treatment plans.
A nurse is performing an admission assessment for a client who is receiving treatment following a situational crisis. Which of the following assessments by the nurse is the highest priority?
Explanation
A. While assessing coping skills is essential, in a crisis situation, determining immediate risks to the client's safety takes precedence.
B. Assessing for psychotic thinking is crucial to address immediate safety concerns. Psychosis can present significant risks and requires immediate attention.
C. While support systems are important for long-term recovery, determining immediate safety concerns is a priority.
D. Identifying the cause of the crisis is relevant but may not be the immediate priority when the client's safety is at risk due to potential psychotic thinking.
In a team meeting, a nurse says, "I'm concerned whether we are behaving ethically by using restraint to prevent one patient from self-mutilation while the care plan for another patient who has also self-mutilated calls for one-on-one supervision." Which ethical principle most clearly applies to this situation?
Explanation
A. Fidelity pertains to faithfulness, loyalty, and keeping promises, which may not directly address the fairness of resource allocation or treatment.
B. Beneficence refers to doing good and promoting the patient's well-being. While it's relevant to patient care, it might not specifically address the fair distribution of resources or actions among different patients.
C. Autonomy emphasizes a patient's right to make decisions about their care and treatment, which doesn't directly address the fairness or justice in the scenario described.
D. Justice concerns the fair and equitable distribution of resources, treatment, and decisions among individuals. In this case, it's about ensuring fairness in the application of care plans and resources for patients who self-mutilate.

Nursing behaviors associated with the implementation phase of the nursing process are concerned with the responsibilities of the psychiatric mental health nurse?
Explanation
A. This is more aligned with the evaluation phase of the nursing process, ensuring that interventions are achieving the intended results.
B. During implementation, nurses execute the care plan, carry out interventions, and coordinate care with other healthcare team members to meet the patient's needs.
C. This is primarily part of the assessment phase, ensuring a thorough understanding of the patient's situation.
D. This involves collaborative goal-setting and is more aligned with the planning phase, ensuring that patient goals are agreed upon and relevant.
A nurse in an acute mental health facility is caring for a client who has major depressive disorder. Since her admission 3 days ago, she has not put on clean clothes, washed her hair, or participated in any of the unit activities. On this day, the nurse observes that she is wearing clean clothes and has combed her hair. Which of the following responses should the nurse make?
Explanation
A. This response may convey a sense of judgment or imply the client's previous state was unacceptable, potentially making the client feel criticized.
B. This question might inadvertently put the client on the defensive and seems intrusive, possibly making the client uncomfortable.
C. This response is observational and nonjudgmental, acknowledging the change without implying any criticism.
D. This response assumes the reason for the change without allowing the client to express herself and might not accurately reflect the client's emotional state or motivation.
Sign Up or Login to view all the 49 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

