ATI RN VATI Adult Medical Surgical S 2019
Total Questions : 89
Showing 25 questions, Sign in for moreA nurse is caring for a client who is hemorrhaging and hypotensive from esophageal variceal bleeding. Which of the following actions should the nurse take first?
Explanation
Verify that the client has adequate IV access.

Choice A rationale:
Administering vasopressin to the client might be necessary to manage the hemorrhage, but before any medication administration, it is crucial to ensure the client has adequate IV access. Vasopressin is a vasoconstrictor and can help control bleeding from esophageal varices, but its effectiveness relies on IV access to deliver the medication promptly.
Choice B rationale:
Requesting blood from the blood bank is essential for a client experiencing significant bleeding. However, the priority action is to verify IV access to administer any necessary blood products.
Choice C rationale:
This is the correct choice. Before initiating any interventions, ensuring the client has appropriate IV access is a priority. Adequate IV access is necessary to administer fluids, medications, or blood products promptly and effectively stabilize the client's blood pressure.
Choice D rationale:
Inserting an indwelling urinary catheter is not the priority action in this situation. While monitoring urine output is important, it should be secondary to addressing the client's hypotension and hemorrhage.
A nurse is providing teaching about dietary options for a client who has cholelithiasis. Which of the following statements should the nurse include in the teaching?
Explanation
Choice A rationale:
Cauliflower is not a good dietary choice for a client with cholelithiasis. Cholelithiasis refers to the presence of gallstones, and certain foods, including cauliflower, can exacerbate symptoms in some individuals.
Choice B rationale:
Increasing the amount of egg yolks in the diet is not advisable for a client with cholelithiasis. Egg yolks are high in cholesterol and can contribute to gallstone formation.
Choice C rationale:
This is the correct choice. Desserts like angel-food cake are a better dietary option for a client with cholelithiasis. Angel-food cake is typically low in fat and cholesterol, making it a more suitable choice for those with gallbladder issues.
Choice D rationale:
Eating choice or prime cuts of meat is not recommended for clients with cholelithiasis. These types of meat are often higher in fat, which can trigger gallbladder symptoms.
A nurse is planning care for a client who is receiving brachytherapy. Which of the following interventions should the nurse include in the plan of care?
Explanation
Dispose of the client's feces and urine in a special container.
Choice A rationale:
This is the correct choice. Brachytherapy involves the placement of a radiation source in or near the tumor. To minimize radiation exposure to others, the client's bodily fluids (feces and urine) should be considered radioactive and disposed of properly in a designated container.
Choice B rationale:
While limiting the time of visitors can be a good measure to reduce radiation exposure, it is not the priority intervention. The primary concern is proper handling and disposal of radioactive bodily fluids.
Choice C rationale:
Keeping the client's linens in the room until after removal of the radiation source is not the correct choice. Radioactive linens should be handled and laundered separately, following appropriate safety protocols.
Choice D rationale:
Providing one dosimeter badge for staff to share while caring for the client is not adequate. Each staff member involved in direct care should have their dosimeter badge to monitor their individual radiation exposure levels.
A nurse is caring for a client who is postoperative following a total left hip arthroplasty. Which of the following actions should the nurse take?
Explanation
Choice A rationale:
The nurse should not cross the client's legs when sitting in the recliner following a total left hip arthroplasty. Crossing the legs can put strain on the operative hip and may increase the risk of dislocation or other complications.
Choice B rationale:
Providing a heating pad to the operative hip is not recommended. Heat can increase blood flow to the area and may lead to increased swelling and potential complications in the postoperative period.
Choice C rationale:

Placing a pillow between the legs when turning the client to their side is the correct action. This technique is known as the "abduction pillow”. or "wedge pillow.”. It helps maintain proper hip alignment and prevents the operated leg from crossing the midline, reducing the risk of dislocation and promoting healing.
Choice D rationale:
Having the client lean forward when assisting them out of the bed is not appropriate after a total left hip arthroplasty. Leaning forward can put strain on the hip joint and increase the risk of injury.
A nurse is caring for a client who had moderate sedation during a procedure. The client's airway is obstructing, and they have an oxygen saturation of 90%. Which of the following interventions is the first action the nurse should take?
Explanation
Choice A rationale:
Preparing an endotracheal tube for intubation is not the first action the nurse should take in this situation. Intubation is an invasive procedure and should be reserved for cases where other, less invasive methods of airway management have failed.
Choice B rationale:
Inserting a plastic oral airway may help maintain the airway in some situations, but it is not the first action to take when the client's airway is obstructing and their oxygen saturation is low.
Choice C rationale:
Providing oxygen using a manual resuscitation bag (bag-valve-mask device) is the correct first action. This allows the nurse to manually assist the client's breathing and deliver oxygen more effectively than just providing supplemental oxygen through a nasal cannula or face mask.
Choice D rationale:
Performing a head tilt with a chin-lift is a basic airway maneuver, but it may not be sufficient in this situation, especially if the airway is completely obstructed. Providing oxygen with a manual resuscitation bag takes precedence.
A nurse is providing information about maintaining a special diet with a client who has irritable bowel syndrome. Which of the following information should the nurse include?
Explanation
Choice A rationale:
Increasing the intake of dairy products is not recommended for a client with irritable bowel syndrome (IBS) as dairy can exacerbate symptoms in some individuals, particularly if they are lactose intolerant.
Choice B rationale:
Drinking ten glasses of water each day is a helpful recommendation for clients with IBS. Staying hydrated can aid in digestion and help alleviate symptoms like constipation.
Choice C rationale:
Decreasing daily fiber intake to 20 grams is not advisable for IBS management. Adequate fiber intake is essential for maintaining bowel regularity and overall gut health. Instead, it is recommended to focus on soluble fiber and gradually increase fiber intake to avoid exacerbating symptoms.
Choice D rationale:
Encouraging the intake of clear carbonated fluids is not ideal for clients with IBS. Carbonated beverages can cause bloating and gas, potentially worsening symptoms in individuals with sensitive digestive systems. It is better to recommend non-carbonated, non-caffeinated fluids for hydration.
A nurse is planning care for a client who has disseminated herpes zoster (shingles). Which of the following interventions should the nurse include?
Explanation
Choice A rationale:
Placing the client in a room with negative airflow is not necessary for disseminated herpes zoster (shingles). Shingles are caused by the reactivation of the varicella-zoster virus and are not airborne. Standard precautions are sufficient for caring for clients with shingles.
Choice B rationale:
Removing the isolation gown after leaving the client's room is not a necessary intervention for disseminated herpes zoster. The nurse should remove the gown before leaving the client's room to prevent the spread of infectious particles.
Choice C rationale:
Applying ketoconazole to the lesions three times per day is not a recommended intervention for disseminated herpes zoster. Ketoconazole is an antifungal medication, and shingles are caused by a virus, not a fungus. Antiviral medications such as acyclovir or valacyclovir are used to treat shingles.
Choice D rationale:
This is the correct choice. Providing the client with eye protection for ultraviolet B (UVB) light therapy is an important intervention. Disseminated herpes zoster can affect the eyes, leading to serious complications, including vision loss. UVB light therapy can help manage the symptoms, but eye protection is necessary to prevent damage to the eyes during treatment.
A nurse in the emergency department is preparing to irrigate the eyes of a client who received a chemical splash on their face. Which of the following actions should the nurse take?
Explanation
Choice A rationale:
Completely irrigating one eye before irrigating the second eye is the correct action to take when a client receives a chemical splash on their face. This approach helps prevent the potential spread of the chemical from one eye to the other. Irrigation should be done immediately to flush out the chemical and minimize its harmful effects.
Choice B rationale:
Informing the client to blink their eyes rapidly during the irrigation process is not recommended. Blinking may exacerbate the dispersion of the chemical and could lead to further damage to the eyes. Instead, the client should keep their eyes open during irrigation.
Choice C rationale:
Delaying the irrigation process until the type of chemical in the eyes is identified is not appropriate. Time is critical in minimizing the impact of the chemical on the eyes. Immediate irrigation is essential, regardless of the type of chemical, to remove the substance from the eyes.
Choice D rationale:
Asking the client to count the number of fingers held up by the nurse before irrigating their eyes is not relevant in this situation. The priority is to initiate immediate irrigation to remove the chemical from the eyes. Assessing the client's visual acuity can be done later in the evaluation process after the eyes have been irrigated.
A nurse is caring for a client who has a pulmonary embolism and is receiving therapy with unfractionated heparin. Which of the following laboratory results indicates that the therapy is effective?
Explanation
Choice A rationale:
A PT (Prothrombin Time) of 12 seconds is not indicative of the effectiveness of heparin therapy for a pulmonary embolism. PT measures the extrinsic pathway of the coagulation cascade, and it is more relevant to monitor in patients on warfarin therapy.
Choice B rationale:
The aPTT (Activated Partial Thromboplastin Time) of 75 seconds is the correct choice as it reflects the effectiveness of unfractionated heparin therapy. Heparin works by inhibiting clotting factors in the intrinsic pathway, and the aPTT is used to monitor heparin's anticoagulant effect. The normal range for aPTT is typically 25-35 seconds.
Choice C rationale:
An INR (International Normalized Ratio) of 1.1 is not the appropriate parameter to assess the effectiveness of heparin therapy. INR is primarily used to monitor the effectiveness of oral anticoagulants like warfarin, not heparin.
Choice D rationale:
The platelet count of 200,000/mm² is not a suitable parameter to evaluate the effectiveness of heparin therapy. Platelet count is important for assessing the risk of bleeding or clotting disorders but does not directly measure the impact of heparin on clotting factors.
A nurse is planning care for a client who has long-term liver cirrhosis and a new diagnosis of abdominal ascites. Which of the following interventions should the nurse include in the plan of care to prevent complications?
Explanation
Choice A rationale:
Administering furosemide may be appropriate for managing ascites, but it is not directly related to preventing complications. Furosemide is a diuretic that helps reduce fluid retention but does not address other potential complications of liver cirrhosis.
Choice B rationale:
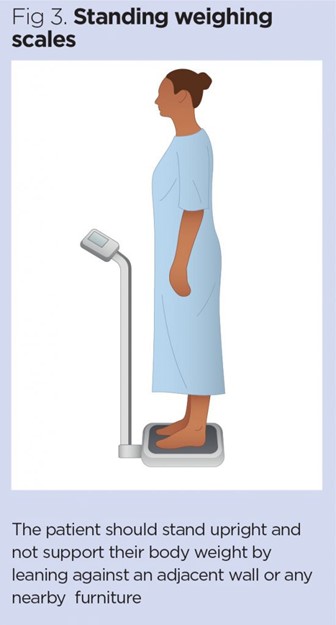
Weighing the client weekly is essential to monitor changes in body weight and fluid status, which is crucial in detecting worsening ascites or fluid retention. Sudden weight gain could indicate an exacerbation of ascites or other complications, warranting timely intervention.
Choice C rationale:
Offering the client a high-sodium diet is contraindicated in managing ascites. A high-sodium diet would lead to increased fluid retention and worsen the ascites, potentially exacerbating the client's condition and increasing the risk of complications.
Choice D rationale:
Administering heparin is not relevant to preventing complications in a client with liver cirrhosis and abdominal ascites. Heparin is an anticoagulant, and its use is not indicated for this particular condition.
A nurse is caring for a client who recently assumed the role of caregiver for their aging parents who have chronic illnesses. The nurse should identify that which of the following statements by the client indicates acceptance of the role change?
Explanation
"I changed the floor plan of our home to accommodate my father's wheelchair.”.
Choice A rationale:
This statement indicates acceptance of the role change as a caregiver for the aging parents. Making changes to the home to accommodate the father's wheelchair demonstrates the client's willingness to adapt and provide a suitable environment for caregiving.
Choice B rationale:
Feeling stressed out and overwhelmed does not necessarily indicate acceptance of the role change. It may reflect the challenges and emotional burden that come with caregiving but does not necessarily signify acceptance.
Choice C rationale:
Expressing frustration with caregiving does not necessarily indicate acceptance of the role change. It is normal to feel frustrated at times, especially when dealing with chronic illnesses, but acceptance involves embracing the responsibilities that come with the role.
Choice D rationale:
While the statement shows a willingness to learn and adapt to caregiving, it does not explicitly indicate acceptance of the role change. Acceptance involves acknowledging and embracing the new responsibilities and challenges fully.
A nurse is caring for a client who has an NG tube to suction and is receiving IV fluids to maintain fluid volume balance. Which of the following findings should indicate to the nurse that this therapy is effective?
Explanation
Choice A rationale:
A decrease in NG tube drainage indicates that the client's stomach contents are not being aspirated excessively, which suggests that the IV fluids are effectively maintaining fluid volume balance. This finding is positive because it shows that the client is retaining the fluids they need, and it may also indicate improved gastrointestinal function and decreased risk of dehydration.
Choice B rationale:
The potassium level of 3.3 mEq/L (milliequivalents per liter) is low. The normal range for potassium is typically between 3.5 to 5.0 mEq/L. Hypokalemia (low potassium) can result from various factors and may cause muscle weakness, cardiac arrhythmias, and other complications. It is not a finding that indicates the effectiveness of fluid volume balance therapy.
Choice C rationale:
An increased heart rate may suggest that the client is experiencing fluid volume deficit or other physiological stress. It is not a finding that indicates the effectiveness of fluid volume balance therapy.
Choice D rationale:
A hematocrit level of 46% is within the normal range for adult males (typically around 38.8% to 50%) and indicates the proportion of red blood cells in the blood. While it can provide information about blood viscosity and hydration status, it does not directly indicate the effectiveness of fluid volume balance therapy.
A nurse is planning care for a client who is scheduled for surgery and has a latex allergy. Which of the following actions should the nurse plan to take?
Explanation
Choice A rationale:
Scheduling the client for the last surgery of the day is not directly related to the client's latex allergy. Proper planning for surgery in a latex-allergic client involves addressing potential exposures to latex-containing products and minimizing the risk of allergic reactions.
Choice B rationale:
Placing monitoring cords and tubes in a stockinette can help create a barrier between the client's skin and the latex-containing products. This measure helps reduce the risk of direct contact with latex, which could trigger an allergic reaction in a latex-sensitive individual.
Choice C rationale:
Choosing rubber injection ports for fluid administration is not appropriate for a client with a latex allergy. Rubber products often contain latex, which can lead to an allergic reaction in susceptible individuals.
Choice D rationale:
Having phenytoin IV readily available is not directly relevant to a client with a latex allergy. Phenytoin is an antiepileptic medication and should be available for clients who require it, but it does not address the specific concern of latex exposure.
A nurse is caring for a client who is experiencing anxiety as well as numbness and tingling of the lips and fingers. The client's ABGs are pH 7.48, PCO2 30 mm Hg, HCO3 24 mEq/L, PaO2 85 mm Hg. Which of the following acid-base imbalances should the nurse identify that the client is experiencing?
Explanation
Choice A rationale:
The client's ABG values show a pH of 7.48, PCO2 of 30 mm Hg, HCO3 of 24 mEq/L, and PaO2 of 85 mm Hg. The elevated pH and decreased PCO2 (respiratory component) suggest respiratory alkalosis. Respiratory alkalosis occurs when there is excessive ventilation, leading to a decrease in carbon dioxide levels (hypocapnia) and subsequent alkalosis.
Choice B rationale:
Respiratory acidosis is characterized by an elevated PCO2 and decreased pH. In this case, the client's PCO2 is decreased, indicating respiratory alkalosis rather than respiratory acidosis.
Choice C rationale:
Metabolic alkalosis is characterized by an elevated HCO3 (bicarbonate) level and an increased pH. The client's HCO3 level is within the normal range, making metabolic alkalosis an incorrect identification.
Choice D rationale:
Metabolic acidosis is characterized by a decreased HCO3 level and a decreased pH. The client's HCO3 level is within the normal range, ruling out metabolic acidosis as the acid-base imbalance in this case.
A nurse is preparing to give a bed bath to a client who had a cerebrovascular accident (CVA). Which of the following actions should the nurse plan to take?
Explanation
Choice A rationale:
The nurse should wash the client in a distal to proximal direction during a bed bath after a cerebrovascular accident (CVA) to prevent the risk of clot dislodgement. This method ensures that any potential clots or debris are moved away from the central circulation, reducing the risk of harm.
Choice B rationale:
Using a circular motion with the washcloth can increase friction and potentially irritate the skin. Clients with a history of CVA might have reduced sensation or mobility, making them susceptible to skin breakdown. Hence, avoiding circular motions is important to prevent skin damage.
Choice C rationale:
Massaging the legs after completing the bath can also pose a risk of clot dislodgement. It is essential to avoid vigorous massage on areas affected by deep vein thrombosis (DVT) to prevent complications like pulmonary embolism.
Choice D rationale:
There is no need to disconnect the IV tubing before performing the bath unless specifically indicated by the healthcare provider. In general, clients receiving continuous IV infusions can continue the infusion while maintaining proper infection control measures during the bath.
A nurse is assessing a client who is receiving IV fat emulsion therapy. Which of the following findings should the nurse identify as a manifestation of fat overload syndrome?
Explanation
Choice A rationale:
Hypertension is not a manifestation of fat overload syndrome. Fat overload syndrome occurs when the body is unable to metabolize a large amount of fat delivered by IV fat emulsions, leading to fat accumulation in organs such as the lungs, liver, and bone marrow.
Choice B rationale:
Weight gain is a common manifestation of fat overload syndrome. The excess fat not metabolized accumulates in the body, leading to weight gain and potential complications.
Choice C rationale:
Fever is not directly related to fat overload syndrome. This condition primarily involves the accumulation of fat and its related complications rather than causing fever.
Choice D rationale:
Hypoglycemia is not associated with fat overload syndrome. This condition results from low blood sugar levels and is not directly related to the administration of IV fat emulsions.
A nurse is assessing a client who takes salmeterol to treat moderate asthma. Which of the following findings should indicate to the nurse that the medication has been effective?
Explanation
The client's daily peak expiratory flow (PEF) measures 85% above personal best.
Choice A rationale:
Salmeterol is a long-acting beta-agonist used to treat asthma. Improvement in the client's daily peak expiratory flow (PEF) of 85% above their personal best indicates effective bronchodilation and better asthma control.
Choice B rationale:
ABGs showing a pH level of 7.32 are not indicative of the effectiveness of salmeterol. ABG values assess the client's acid-base balance and gas exchange, but they do not directly reflect the action of the medication.
Choice C rationale:
A decrease in forced expiratory volume after treatment with medication indicates a lack of response to the therapy, not an effective outcome. It suggests the medication is not adequately controlling the client's asthma symptoms.
Choice D rationale:
Wheezing limited to expiration is not a clear indicator of medication effectiveness. Wheezing can be present in various respiratory conditions and is not solely associated with asthma control. Exhibit. The correct answer is choice B: Increase the rate of the infusion by 160 units/hr.
A nurse is inspecting the skin of a client who has basal cell carcinoma. The nurse should identify which of the following lesion characteristics on the client's skin?
Explanation
the correct answer is Choice A.
Choice A rationale: Basal cell carcinoma (BCC) is a type of skin cancer that develops in basal cells, a type of cell within the skin that produces new skin cells1.One of the common symptoms of BCC is a pearly white, skin-colored or pink bump1.This can also appear as a shiny or pearly nodule with a smooth surface2.Therefore, a pearly, waxy nodule is a characteristic lesion of basal cell carcinoma
Choice B rationale: An irregular border on a variegated-colored lesion is more commonly associated with melanoma, another type of skin cancer, rather than basal cell carcinoma1.While BCC can have a variety of appearances, an irregular border on a variegated-colored lesion is not typically characteristic of BCC
Choice C rationale: A firm, nodular, crusty, or ulcerated lesion can be a sign of several types of skin conditions, including squamous cell carcinoma, another type of skin cancer1.While BCC can sometimes appear as a firm nodule1, the description of a crusty or ulcerated lesion is not as characteristic of BCC as a pearly, waxy nodule
Choice D rationale: A weeping vesicle is not typically associated with basal cell carcinoma1.BCC lesions are more likely to appear as a shiny bump or nodule, or a flat, scaly patch1.A weeping vesicle could be indicative of a different skin condition
A nurse is caring for a group of clients. In which of the following scenarios is the nurse acting as a client advocate?
Explanation
Choice A rationale:
Filing an incident report regarding a medication error is part of a nurse's responsibility to ensure patient safety and quality care. While it demonstrates accountability, it is not necessarily acting as a client advocate.
Choice B rationale:
Providing wound care to a client at the promised time is an example of delivering timely and appropriate care, which is part of the nurse's role. It is not specifically acting as a client advocate, although it does promote the client's well-being.
Choice C rationale:
The nurse declines to inform a client's neighbor about the client's prognosis. This choice shows the nurse advocating for the client's right to privacy and confidentiality, which is a crucial aspect of being a client advocate.
Choice D rationale:
Referring a client with chronic obstructive pulmonary disease for palliative care services is an important action to ensure the client receives appropriate care and symptom management. While it is a valuable aspect of nursing care, it does not necessarily represent advocating for the client's rights or wishes.
A nurse is providing teaching to a female client who has herpes simplex virus type 2. Which of the following client statements indicates an understanding of the teaching?
Explanation
Choice A rationale:
Taking sitz baths can provide comfort but will not directly address the transmission of herpes simplex virus type 2 (HSV-2). It is essential to avoid sexual activity during outbreaks to prevent spreading the infection to a partner.
Choice B rationale:
Cleansing lesions with 1/2 strength peroxide may irritate the affected area and delay healing. The recommended approach is to use gentle soap and water to clean the lesions.
Choice C rationale:
"I will avoid sexual activity until my lesions are healed.”. This statement indicates an understanding of the teaching because HSV-2 is highly contagious during active outbreaks. Avoiding sexual activity during this time is essential to prevent transmitting the virus to a partner.
Choice D rationale:
"I am not contagious once I begin antiviral medication.”. This statement is incorrect as antiviral medications can help manage outbreaks but do not eliminate the risk of transmission entirely. The virus remains contagious until lesions are completely healed.
A nurse in an emergency department is caring for a client who has appendicitis. Which of the following actions should the nurse take?
Explanation
Choice A rationale:
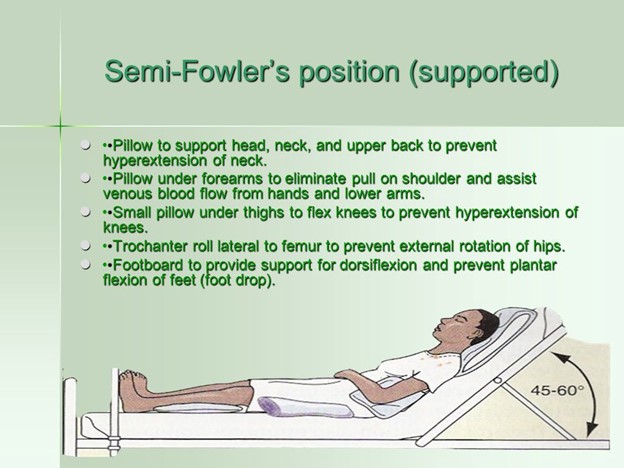
The nurse should maintain the client in a semi-Fowler's position to promote comfort and reduce the risk of complications related to appendicitis. This position helps to decrease pressure on the abdomen and may alleviate pain by reducing tension on the abdominal muscles.
Choice B rationale:
Administering an enema 1 hour prior to surgery is not indicated for a client with appendicitis. Enemas are generally not recommended for clients with suspected or confirmed appendicitis as they can potentially worsen inflammation and cause perforation of the inflamed appendix.
Choice C rationale:
Applying a warm pack to the client's lower abdomen is contraindicated in appendicitis. Heat can exacerbate inflammation and should be avoided in such cases.
Choice D rationale:
Placing the client on a clear liquid diet is not appropriate for appendicitis. Clients with appendicitis are typically NPO (nothing by mouth) to avoid stimulating the gastrointestinal tract and reduce the risk of rupture if surgery is needed.
A nurse is preparing to administer total parenteral nutrition (TPN) to a client. The nurse should notify the provider of which of the following findings?
Explanation
Choice A rationale:
A blood glucose level of 100 mg/dL is within the normal range, so there is no need to notify the provider of this finding.
Choice B rationale:
A client's temperature of 37.6°C (99.7°F) is slightly elevated but not considered a critical finding. It may be indicative of an infection or other mild inflammation, but it does not warrant immediate provider notification.
Choice C rationale:
A potassium level of 5.7 mEq/L is above the normal range (3.5-5.0 mEq/L). Hyperkalemia can lead to serious cardiac complications, such as arrhythmias, and requires immediate attention from the provider.
Choice D rationale:
Weight loss of 0.8 kg/day (1.8 lb/day) should be evaluated and monitored, but it is not an immediate concern that warrants urgent provider notification.
A nurse is providing teaching about health promotion activities for a client who has a new diagnosis of type 1 diabetes mellitus. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A rationale:
The statement "If I can keep my hemoglobin A1C less than 6.5%, I will be cured of diabetes.”. is incorrect. While maintaining an A1C level below 6.5% is a recommended target for some individuals with diabetes, achieving this level does not cure diabetes. Diabetes is a chronic condition that requires ongoing management and lifestyle modifications.
Choice B rationale:
Checking blood sugar levels before exercising is an important aspect of managing type 1 diabetes. Exercise can affect blood glucose levels, and knowing the current level helps the client determine whether it is safe to engage in physical activity or if adjustments to insulin or carbohydrate intake are needed.
Choice C rationale:
Having regular eye checks every 2 years is essential for clients with diabetes, but it is not the best statement that indicates an understanding of health promotion activities for a new diagnosis of type 1 diabetes mellitus.
Choice D rationale:
Soaking feet daily in warm, soapy water is not a recommended practice for clients with diabetes. It can lead to skin dryness and increase the risk of infection. Instead, clients with diabetes should practice daily foot inspections and keep their feet moisturized to prevent complications related to peripheral neuropathy.
A nurse is caring for a client who is receiving mechanical ventilation. Which of the following actions should the nurse implement to decrease the client's risk for ventilator-associated pneumonia (VAP)? (Select all that apply.).
Explanation
Choice A rationale:
The nurse should wear a protective gown when suctioning the client's airway to prevent the spread of infection. During suctioning, there is a risk of exposure to the client's respiratory secretions, which may contain infectious organisms. Wearing a gown will help protect the nurse from contact with these secretions.
Choice B rationale:
Monitoring for oral secretions every 2 hours is essential to prevent the accumulation of mucus or saliva in the client's mouth. Excessive secretions can increase the risk of aspiration, which may lead to ventilator-associated pneumonia (VAP).
Choice C rationale:
Providing oral care every 2 hours is crucial to maintain oral hygiene and reduce the growth of bacteria in the mouth. Oral bacteria can potentially enter the lungs during mechanical ventilation, contributing to the development of VAP.
Choice D rationale:
Maintaining the client in a supine position is not recommended as it can increase the risk of VAP. The supine position may cause secretions to pool in the back of the throat, making it more likely for the client to aspirate these secretions.
Choice E rationale:
Assessing the client daily for readiness for extubation is important but not directly related to decreasing the risk of VAP. Extubation refers to the removal of the endotracheal tube, which helps prevent complications associated with prolonged intubation but does not specifically address VAP prevention.
A nurse is caring for a client who had a fiberglass cast applied 30 min ago for a fractured tibia. Which of the following actions should the nurse take?
Explanation
Choice A rationale:
The nurse should maintain the affected leg elevated on several pillows to reduce swelling and promote venous return. Elevating the leg helps minimize edema, which can be beneficial for the healing process and overall comfort of the client.
Choice B rationale:
Instructing the client to wiggle the toes once every 4 hours is not necessary and may cause discomfort to the fractured tibia. Toe wiggling does not provide any significant benefit in this context and could potentially disrupt the healing process.
Choice C rationale:
Using a hair dryer to promote drying of the cast is not recommended. Applying heat to the fiberglass cast may alter its integrity and lead to uneven drying, potentially weakening the cast's support.
Choice D rationale:
Applying heat to the client's cast for pain relief is not advisable. Heat may also weaken the cast material and is unlikely to provide effective pain relief for a fractured tibia. Instead, the nurse should follow the prescribed pain management plan and use appropriate pain medications as ordered by the healthcare provider.
Sign Up or Login to view all the 89 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

