CTO1 Dosage Calculations
Total Questions : 66
Showing 25 questions, Sign in for moreA physician gives the following order: "Infuse LR, 500 ml over 2 hours."
At what rate should the nurse set the IV pump to deliver this infusion (mL/hr)?
Explanation
To calculate the rate at which the nurse should set the IV pump to deliver the LR infusion, we need to divide
the total volume (500 ml) by the total time (2 hours).
500 ml / 2 hours = 250 ml/hr
Therefore, the nurse should set the IV pump to deliver the LR infusion at a rate of b. 250 mL/hr.
a. 100 mL/hr: This rate is too low and would result in the infusion taking longer than the prescribed 2 hours.
c. 500 mL/hr: This rate is too high and would result in the infusion being delivered faster than the prescribed 2 hours.
d. 1000 mL/hr: This rate is even higher than the total volume of the infusion divided by the total time. It
would deliver the infusion at a significantly faster rate than intended.
Therefore, the correct rate at which the nurse should set the IV pump to deliver the LR infusion is b. 250 mL/hr, as it ensures that the infusion is delivered over the prescribed 2-hour timeframe
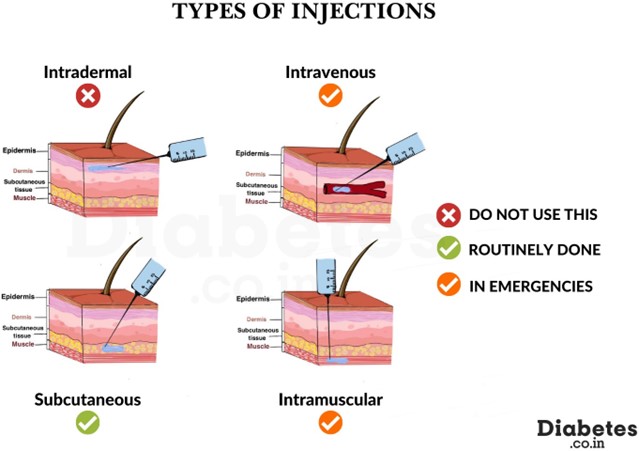
Why is subcutaneous (SC) insulin usually administered into the abdomen as the preferred site?
Explanation
Subcutaneous (SC) insulin is usually administered into the abdomen as the preferred site because there is
steady absorption of insulin from this area.
The abdomen has a rich blood supply and a relatively higher number of capillaries compared to other subcutaneous sites. As a result, insulin injected into the abdominal subcutaneous tissue is absorbed more consistently and predictably. This allows for better control of blood glucose levels.
A. There are fewer insulin side effects when given at this site: The site of injection does not directly affect the side effects of insulin. Side effects can occur regardless of the injection site and are more related to the medication itself and individual patient factors.
B. It is the least painful location for this injection: The perception of pain can vary among individuals, and the least painful location for an injection may differ from person to person. While some individuals may find the abdomen to be less painful, others may have different preferences or experiences.
D. . It causes less bruising at the site: Bruising at the injection site can occur regardless of the location due to various factors such as needle size, technique, and individual patient characteristics. The choice of injection site does not specifically prevent bruising.
Therefore, the main reason why subcutaneous insulin is usually administered into the abdomen as the preferred site is c. There is steady absorption of insulin from this site, ensuring consistent and predictable insulin delivery for better blood glucose control.
A primary healthcare provider prescribes 1.5 L of normal saline (NS) to be given over 24 hours for
continuous intravenous (IV) infusion to a client who has diarrhea.
What should be the rate of infusion that is required to be set in the infusion pump?
Explanation
To calculate the rate of infusion required for the continuous intravenous (IV) infusion of 1.5 L of normal saline (NS) over 24 hours, we need to divide the total volume (1500 ml) by the total time (24 hours).
1500 ml / 24 hours = 62.5 ml/hr
Therefore, the rate of infusion that should be set in the infusion pump is a. 62.5 mL/hr.
B. 41.7 mL/hr: This rate is too low and would result in the infusion taking longer than the prescribed 24 hours.
C. 20.8 mL/hr: This rate is even lower and would result in an even longer infusion time, which is not consistent with the prescribed 24 hours.
D. 83.3 mL/hr: This rate is too high and would result in the infusion being delivered faster than the prescribed 24 hours.
Therefore, the correct rate of infusion to be set in the infusion pump for the continuous IV infusion of 1.5 L of normal saline over 24 hours is a. 62.5 mL/hr, as it ensures the prescribed volume is infused within the specified time frame.

A nurse, via an infusion pump, sets up an infusion rate ratio of 2.75 mL/min for a continuous intravenous
(IV) fluid for 7 hours.
What is the total volume of IV fluid being infused, in liters?
Explanation
To calculate the total volume of IV fluid being infused, we need to multiply the infusion rate ratio (2.75 mL/min) by the total time (7 hours) and then convert the result to liters.
2.75 mL/min * 60 min/hour * 7 hours = 1155 mL
To convert mL to liters, we divide by 1000:
1155 mL / 1000 = 1.155 L
Therefore, the total volume of IV fluid being infused is d. 1.155 L.
A. 1.161 L: This value is slightly higher and does not match the calculated result.
B. 1.25 L: This value is significantly higher and does not match the calculated result.
C. 1.15 L: This value is slightly lower and does not match the calculated result.
Therefore, the correct total volume of IV fluid being infused is d. 1.155 L, as calculated based on the given infusion rate ratio and total time.

A physician gives the following order: "Infuse 0.9% sodium chloride solution, 2.5L over 15 hours."
What is the mL/hr flow rate for continuous infusion?
Explanation
To calculate the mL/hr flow rate for the continuous infusion of 0.9% sodium chloride solution over 15 hours, we need to divide the total volume (2.5 L) by the total time (15 hours) and then convert the result to mL/hr.
2.5 L / 15 hours = 166.67 mL/hr
Therefore, the mL/hr flow rate for continuous infusion is a. 166.67 mL/hr.
B. 41.67 mL/hr: This rate is too low and does not match the calculated result.
C. 250 mL/hr: This rate is significantly higher and does not match the calculated result.
D. 1000 mL/hr: This rate is even higher and does not match the calculated result.
Therefore, the correct mL/hr flow rate for the continuous infusion of 0.9% sodium chloride solution over 15 hours is a. 166.67 mL/hr, as calculated based on the given order and total time.
A nurse needs to infuse esmolol into a client weighing 65 kg. The dose on hand is 2,500 mg esmolol in 250 mL of fluid. The client requires a dose of 200 mcg/kg/min to control a hypertensive crisis. Which rate should the nurse calculate to infuse this medication?
Round to the nearest whole number
Explanation
To calculate the rate at which the nurse should infuse esmolol to the client, we need to determine the total amount of medication (in mg) required per minute and then convert it to mL/hr based on the concentration of the medication.
First, we need to calculate the total amount of esmolol required per minute:
Dose per minute = dose/kg/min x weight Dose per minute = 200 mcg/kg/min x 65 kg
To convert mcg to mg, divide by 1000:
Dose per minute = (200 mcg/kg/min x 65 kg) / 1000
Now, let's calculate the rate of infusion based on the concentration of the medication:
Rate of infusion (mL/hr) = (Dose per minute (mg/min) / Concentration (mg/mL)) x 60 min/hr
Given that the dose on hand is 2,500 mg esmolol in 250 mL of fluid:
Rate of infusion (mL/hr) = ((200 mcg/kg/min x 65 kg) / 1000 mg/mg) / (250 mL/2500 mg) x 60 min/hr
Simplifying the equation:
Rate of infusion (mL/hr) = (13 mg/min) / (1 mL/min) x 60 min/hr
Rate of infusion (mL/hr) = 13 mL/hr
Therefore, the rate at which the nurse should calculate to infuse esmolol is b. 13 mL/hr, rounded to the nearest whole number.

A physician orders Dobutamine 10 mcg/kg/min for a patient. The patient is 110 lb.
How many milligrams per hour should the patient receive?
Explanation
To calculate the dosage of Dobutamine in milligrams per hour (mg/hr), we need to convert the patient's
weight from pounds to kilograms and then multiply it by the ordered dose.
First, let's convert the patient's weight from pounds to kilograms:
110 lb / 2.2046 = 49.9 kg (rounded to the nearest tenth)
Now, we can calculate the dosage in milligrams per hour: Dosage = dose per kg/min x weight in kg x 60 min/hr Dosage = 10 mcg/kg/min x 49.9 kg x 60 min/hr
To convert mcg to mg, divide by 1000:
Dosage = (10 mcg/kg/min x 49.9 kg x 60 min/hr) / 1000
Calculating the dosage:
Dosage = 29.94 mg/hr (rounded to the nearest hundredth)
Therefore, the patient should receive approximately 30 mg/hr of Dobutamine, which corresponds to the option.
A nurse is preparing to administer 1 L of 0.9% sodium chloride solution to a client over 6 hours. The intravenous (IV) fluid has a drop factor of 15 gt/mL.
What will be the gt/min flow rate?
Explanation
To calculate the gt/min flow rate for administering 1 L of 0.9% sodium chloride solution over 6 hours, we need to determine the total number of drops required and then divide it by the total time in minutes.
First, let's calculate the total volume of the solution in mL:
1 L = 1000 mL
Next, we need to calculate the total number of drops based on the drop factor:
Total drops = total volume (mL) x drop factor (gt/mL) Total drops = 1000 mL x 15 gt/mL
Now, let's calculate the flow rate in gt/min:
Flow rate (gt/min) = total drops / total time (min)
Flow rate (gt/min) = (1000 mL x 15 gt/mL) / (6 hours x 60 min/hour)
Simplifying the equation:
Flow rate (gt/min) = (15000 gt) / (360 min)
Calculating the flow rate:
Flow rate (gt/min) = 41.67 gt/min (rounded to the nearest hundredth)
Therefore, the gt/min flow rate for administering 1 L of 0.9% sodium chloride solution over 6 hours is approximately 41.67 gt/min, which corresponds to option a. 41.6 gt/min.
A healthcare provider orders nitroprusside (100 mcg/1 mL) 3 mcg/kg/minute for a patient weighing 154 lb.
What rate (mL/hr) should the nurse program into the IV pump?
Explanation
To calculate the rate in mL/hr that the nurse should program into the IV pump for administering nitroprusside to the patient, we need to convert the patient's weight from pounds to kilograms and then calculate the dosage based on the weight and ordered dose.
First, let's convert the patient's weight from pounds to kilograms: 154 lb / 2.2046 = 69.85 kg (rounded to the nearest hundredth)
Now, we can calculate the dosage in mcg/min:
Dosage = dose per kg/min x weight in kg Dosage = 3 mcg/kg/min x 69.85 kg
To convert mcg to mg, divide by 1000:
Dosage = (3 mcg/kg/min x 69.85 kg) / 1000
Now, let's calculate the rate in mL/hr:
Rate (mL/hr) = (Dosage (mg/min) / Concentration (mg/mL)) x 60 min/hr
Rate (mL/hr) = ((3 mcg/kg/min x 69.85 kg) / 1000) / (100 mcg/mL) x 60 min/hr
Simplifying the equation:
Rate (mL/hr) = (0.20955 mg/min) / (0.1 mL/min) x 60 min/hr
Rate (mL/hr) = 1257.3 mL/hr
Therefore, the nurse should program the IV pump to deliver nitroprusside at a rate of approximately 1257.3 mL/hr, which corresponds to option a. 1260 mL/hr.

Under which circumstance should a pediatric medication dose calculated from an adult dose be avoided?
Explanation
A pediatric medication dose calculated from an adult dose should be avoided if the drug insert specifically states that the medication is not intended for pediatric use.
The drug insert or package labeling provides important information about the medication, including indications, dosage, contraindications, and safety considerations for different patient populations. If the drug insert explicitly mentions that the medication is not suitable for use in pediatric patients, it means that the medication has not been adequately studied or approved for use in children. In such cases, it is essential to follow the prescribing guidelines and seek alternative medications or dosage forms that are specifically approved for pediatric use.
A. If the drug insert does not specify a pediatric dose: In some cases, the drug insert may not provide a specific pediatric dose but still indicates that the medication is safe and effective for use in children. In such situations, a pediatric dose can be calculated based on appropriate dosage guidelines or established pediatric dosing principles.
B. If the child has gained or lost weight in the past month: Changes in a child's weight can affect medication dosing, especially if the medication dosage is weight-dependent. In such cases, the dose calculation should be adjusted based on the current weight of the child to ensure accurate and safe administration.
D. If the child has an elevated temperature that has not responded to treatment: The child's elevated temperature or lack of response to treatment does not directly impact the calculation of a pediatric medication dose based on an adult dose. However, the underlying condition causing the elevated temperature may influence the choice of medication or dosing considerations. It is important to consider the child's overall clinical condition, including the underlying illness, in determining the appropriate medication and dosage.
Therefore, the circumstance in which a pediatric medication dose calculated from an adult dose should be avoided is when the drug insert explicitly states that the medication is not intended for pediatric use (option c).
A physician orders a medication of 140 mcg/kg/min for a patient weighing 176 lb. The infusion will last 6 min.
How many milligrams should the nurse administer to the patient?
Explanation
To calculate the total amount of medication in milligrams that the nurse should administer to the patient, we need to determine the dosage per minute based on the patient's weight and the ordered dose, and then multiply it by the total infusion time.
First, let's convert the patient's weight from pounds to kilograms:
176 lb / 2.2046 = 79.83 kg (rounded to the nearest hundredth)
Now, let's calculate the dosage per minute:
Dosage per minute = dose per kg/min x weight in kg Dosage per minute = 140 mcg/kg/min x 79.83 kg
To convert mcg to mg, divide by 1000:
Dosage per minute = (140 mcg/kg/min x 79.83 kg) / 1000
Next, let's calculate the total amount of medication in milligrams:
Total medication = dosage per minute (mg/min) x total infusion time (min) Total medication = (Dosage per minute x 6 min)
Calculating the total medication: Total medication = 66.3 mg
Therefore, the nurse should administer approximately 66.3 mg of medication to the patient, which corresponds to option c. 67.2 mg.
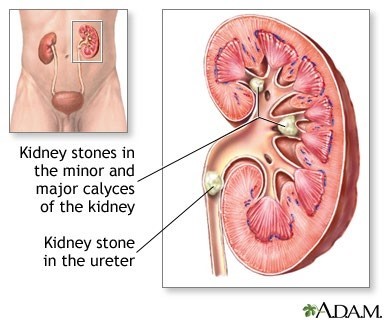
A primary healthcare provider has instructed a nurse to give 100 fl oz of fluids to a client with renal calculi. What should the nurse do while caring for this client?
Explanation
When caring for a client with renal calculi (kidney stones), it is important to maintain adequate hydration to help flush out the stones and prevent further formation. Providing an appropriate amount of fluids is crucial in this situation.
The primary healthcare provider has instructed the nurse to give 100 fl oz of fluids to the client. To convert fluid ounces to liters, we can use the conversion factor 1 fl oz = 0.0296 L.
100 fl oz x 0.0296 L/fl oz ≈ 2.96 L
Therefore, the nurse should provide approximately 3 liters of fluids daily to the client. This corresponds to option a. Provide 3 L of fluids daily.
B. Provide 2400 mL of fluids daily: 2400 mL is equal to 2.4 liters, which is slightly less than the recommended 3 liters.
C. Instruct the client to drink 250 mL of water daily: 250 mL is far below the necessary fluid intake for a client with renal calculi. It is important to provide sufficient fluids to promote hydration.
D. Instruct the client to drink 6 cups of fluids: Cups can vary in size, so this measurement is not precise enough to ensure the appropriate fluid intake. It is best to provide fluid amounts in liters or milliliters for accurate hydration management.
A mother calls a nurse to say that she lost the measuring cup that comes with the cough syrup bottle.
How many teaspoons should the nurse recommend for the child if the dose is 10 mL?
Explanation
To convert milliliters (mL) to teaspoons (tsp), we can use the conversion factor 1 tsp = 5 mL.
Given that the dose is 10 mL, we can calculate the equivalent amount in teaspoons:
10 mL / 5 mL/tsp = 2 tsp
Therefore, the nurse should recommend 2 teaspoons for the child if the dose is 10 mL, which corresponds to option B. 1 teaspoon is not the correct answer, as it does not accurately represent the dose of 10 mL. Option C, 4 teaspoons, is also incorrect. The correct answer is 2 teaspoons.
How many milliliters of mouthwash does a patient use in 1 tablespoon?
Explanation
One tablespoon is equivalent to 15 milliliters (mL). Therefore, the correct answer is a. 15 mL.
Which abbreviation is on the official "Do Not Use" list of the Joint Commission?
Explanation
According to the Joint Commission's official "Do Not Use" list, QD (daily) is on the list because it can be mistaken for other abbreviations such as QOD (every other day). The period after the Q can be mistaken for "I" and the "O" can be mistaken for "I". Instead of using QD, it is recommended to write out "daily"¹.
Which numeric form is appropriate, according to the Joint Commission?
Explanation
According to the Joint Commission's official "Do Not Use" list, trailing zeros (X.0 mg) should not be used because the decimal point can be missed. Instead of using a trailing zero, it is recommended to write X mg. Lack of leading zero (.X mg) should also be avoided because the decimal point can be missed. Instead of using a lack of leading zero, it is recommended to write 0.X mg.
A client weighing 60 kg reports shortness of breath, wheezing, and chest discomfort. The client is prescribed 5 mg/kg ipratropium every 12 hours. In a recall visit, the client reports taking 300 mg/day ipratropium.
What instruction should be given to the client for the effective management of asthma?
Explanation
The client is prescribed a dosage of 5 mg/kg of ipratropium every 12 hours. To calculate the appropriate daily dose for a 60 kg client, we can multiply the weight (60 kg) by the prescribed dosage (5 mg/kg):
60 kg * 5 mg/kg = 300 mg/day
The client reports taking 300 mg/day, which matches the prescribed dose. Therefore, the client is already taking the correct dose of ipratropium.
Based on this information, there is no need to double the dose (option a) or halve the dose (option b) because the client is already taking the prescribed amount.
Changing to an alternative medication (option c) would not be necessary as the client is effectively managing their asthma symptoms with the currently prescribed medication.
Thus, the appropriate instruction for the client is to continue the same dose of medication (option d) as prescribed.
Which actions should a nurse take to prevent medication errors?
Select all that apply.
Explanation
Preventing medication errors is a crucial aspect of nursing practice to ensure patient safety. Here are the explanations for the correct options:
b. Know the recommended dose range for the drug: It is essential for nurses to be knowledgeable about the recommended dose range for the medications they administer. Understanding the appropriate dosages helps in identifying any potential errors or discrepancies.
d. Question a drug dose that appears incorrect: If a nurse comes across a drug dose that seems incorrect or questionable, it is important to clarify and verify the dosage with the prescribing healthcare provider or pharmacist. This helps to prevent the administration of potentially harmful doses.
e. Recalculate the drug dosage if in doubt: If a nurse has doubts or uncertainties about the calculated drug dosage, it is crucial to double-check the calculations and recalculate to ensure accuracy. Being cautious and thorough in dosage calculations reduces the risk of medication errors.
a. Ask the charge nurse to administer the medication: While it is always advisable to seek guidance or clarification from senior nurses or charge nurses, the responsibility of administering medications lies with the nurse who has the knowledge and training to do so. Depending solely on the charge nurse to administer medications may not be practical or feasible in all situations.
c. Calculate all drug dosages by body surface area: Calculating drug dosages based on body surface area is necessary for certain medications, especially those with narrow therapeutic ranges or when administering chemotherapy drugs. However, it is not applicable to all medications. The method of dosage calculation varies depending on the medication and prescribed dosage regimen.
Therefore, the correct actions a nurse should take to prevent medication errors are knowing the recommended dose range for the drug, questioning a drug dose that appears incorrect, and recalculating the drug dosage if in doubt.
A physician orders Garamycin (gentamicin) 4 mg/kg/dose IV piggyback every 12 hours for a newborn
weighing 7 lb, 11.2 oz. After reconstitution, the dosage is 20 mg/10 mL.
How many milliliters should the nurse administer to the patient?
Explanation
To determine the correct dose of Garamycin (gentamicin) to administer, we need to calculate the weight of the newborn in kilograms.
7 lb, 11.2 oz can be converted to kilograms using the following conversions: 1 lb = 0.4536 kg
1 oz = 0.02835 kg
Weight in kilograms:
7 lb * 0.4536 kg/lb = 3.1752 kg
11.2 oz * 0.02835 kg/oz = 0.31752 kg
Total weight in kilograms:
3.1752 kg + 0.31752 kg = 3.49272 kg
Now, we can calculate the dose of gentamicin based on the weight:
Dose = 4 mg/kg * 3.49272 kg = 13.97088 mg
The reconstituted dosage of Garamycin is 20 mg/10 mL. To calculate the volume (in mL) to administer, we set up a proportion:
20 mg / 10 mL = 13.97088 mg / x
Cross-multiplying:
20x = 13.97088 * 10
20x = 139.7088
x = 139.7088 / 20 x ≈ 6.9854 mL
Rounding to the nearest tenth, the nurse should administer approximately 7 mL of Garamycin to the patient. Therefore, the correct answer is c. 7 mL.

Haldol (haloperidol) 5.0 mg po tid was ordered for a patient who is agitated. Which action should a nurse take before administering the medication?
Explanation
Before administering Haldol (haloperidol) or any medication, it is important for the nurse to communicate with the healthcare provider to clarify and understand the rationale for the medication order. This ensures patient safety and promotes informed decision-making.
In this scenario, the nurse should discuss the use of Haldol with the healthcare provider. This discussion allows the nurse to obtain additional information about the medication, including its purpose, potential side effects, and any specific considerations or precautions related to the patient's condition. It also provides an opportunity to confirm the appropriateness of the medication choice for managing the patient's agitation.
While options b, c, and d involve discussing specific aspects of the medication order (tid, po, trailing zero) with the healthcare provider, the most comprehensive and necessary action is to discuss the use of Haldol itself. This discussion encompasses all aspects of the medication order and ensures a clear understanding of the prescribed treatment.
Therefore, the correct action for the nurse to take before administering the medication is to discuss the use of Haldol with the healthcare provider.

The nurse is confirming a pediatric dose from an adult dose sent from the pharmacy. What is an accurate
method for calculating the child's dose?
Explanation
When calculating a pediatric dose from an adult dose, using the child's body surface area (BSA) is a more accurate method. BSA takes into account both the child's weight and height, which are important factors in determining the appropriate dose.
Body surface area can be calculated using various formulas, such as the Mosteller formula (BSA = √[height (cm) x weight (kg) / 3600]) or the Du Bois formula (BSA = 0.007184 x [height (cm)]^0.725 x [weight (kg)]^0.425).
By considering the child's BSA, the dose can be adjusted more precisely to account for differences in body composition and metabolic rate compared to adults. This helps to ensure that the child receives an appropriate and safe dosage.
Options b, c, and d (ideal body weight, actual body weight, actual body height) alone may not provide an accurate calculation for pediatric dosing, as they do not account for variations in body size and composition among children of different ages and developmental stages. BSA takes into consideration both weight and height, providing a more reliable basis for dose calculation in pediatrics.
Therefore, the accurate method for calculating the child's dose when confirming a pediatric dose from an
adult dose is to use body surface area (BSA).

A nurse documenting a wound assessment in a computer notices a client's wound measurement must be entered in inches instead of centimeters. How many inches (in.) is equal to 2.54 centimeters?
Explanation
One inch (in.) is equal to 2.54 centimeters (cm). This conversion factor is commonly used to convert measurements between inches and centimeters. Therefore, when converting from centimeters to inches, we divide the centimeter measurement by 2.54.
In this case, to convert 2.54 centimeters to inches, we divide 2.54 by 2.54:
2.54 cm / 2.54 = 1 in.
So, 2.54 centimeters is equal to 1 inch. Therefore, the correct answer is d. 1 in.
Which number should be multiplied by inches in order to convert a patient's height measurement from inches to centimeters?
Explanation
To convert a measurement from inches to centimeters, we need to multiply the measurement by the conversion factor of 2.54. This conversion factor represents the number of centimeters in one inch.
So, to convert a patient's height measurement from inches to centimeters, we would multiply the
measurement by 2.54.
Therefore, the correct answer is d. 2.54.
Amoxicillin 500 mg is ordered for a patient with a sinus infection. Amoxicillin oral suspension 200 mg per 5
mL is available. How many mL should the nurse administer?
Explanation
To determine the correct answer, we can use a proportion to find the equivalent amount of oral suspension
based on the given dosage.
The ratio of amoxicillin in the oral suspension is 200 mg per 5 mL. We need to find how many milliliters (mL) of the oral suspension contain 500 mg of amoxicillin.
Setting up the proportion, we have:
200 mg / 5 mL = 500 mg / x mL
Cross-multiplying, we get:
200 mg * x mL = 5 mL * 500 mg
Simplifying, we have:
200x = 2500
Dividing both sides by 200, we find:
x = 2500 / 200
x ≈ 12.5 mL
Therefore, the correct answer is c. 12.5 mL. The nurse should administer 12.5 mL of the amoxicillin oral suspension to deliver a dose of 500 mg of amoxicillin to the patient with a sinus infection.

A nurse-midwife orders Stadol (butorphanol) 1 mg IV push every 3-4 hours as needed for pain. The nurse
has Stadol available as 2 mg/mL injection. How many milliliters should the nurse administer to the patient?
Explanation
To determine the correct answer, we can use a calculation based on the desired dose and the concentration of the medication.
The nurse-midwife orders Stadol 1 mg IV push, and the available concentration is 2 mg/mL. We need to calculate the volume of Stadol injection required to administer 1 mg.
Using the formula:
Volume (mL) = Desired dose (mg) / Concentration (mg/mL
Plugging in the values:
Volume (mL) = 1 mg / 2 mg/mL Volume (mL) = 0.5 mL
Therefore, the correct answer is c. 0.5 mL. The nurse should administer 0.5 mL of the Stadol injection to deliver a dose of 1 mg to the patient.

Sign Up or Login to view all the 66 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

