Dosage Calculation
Total Questions : 56
Showing 25 questions, Sign in for moreFosamax (alendronate sodium) 60 mg by mouth is ordered. Fosamax 70 mg/75 mL is available. How many milliliters should the nurse administer to the patient?
Round to the nearest whole number.
Explanation
The correct answer is choice B, 64 mL. To determine the amount of Fosamax the nurse should administer, we use the formula: (dose ordered ÷ dose available) x volume available. Substituting the given values, we get: (60 ÷ 70) x 75 = 64.28 mL, rounded to 64 mL.
A client diagnosed with tuberculosis is prescribed rifampin, 4 mg/kg. 8 hourly for 6 days. The client weighs 43 kg. How many 100 mg bottles of rifampin will be required for this client?
Round your answer to the nearest whole number.
Explanation
The correct answer is choice B. 31. To find the number of bottles required, use the formula: (dose x frequency x duration) / (bottle size x bottle concentration). In this case, (4 mg/kg x 43 kg x 3 times/day x 6 days) / (100 mg/bottle) = 30.96 bottles. Round up to the nearest whole number to get 31 bottles.
A client is prescribed a course of 600 mg/day of ciprofloxacin for 1 week to treat a throat infection. Each bottle contains 7 tablets that are 300 mg.
How many bottles would be required for the client's prescribed course of treatment throughout the week?
Explanation
The correct answer is choice B. 2 bottles. To find the number of bottles required, use the formula: (dose x duration) / (bottle size x tablet strength). In this case, (600 mg/day x 7 days) / (7 tablets/bottle x 300 mg/tablet) = 2 bottles.
A primary healthcare provider prescribes 15 g/day niacinamide to a client. Upon seeing the medication bottle, a nurse finds each tablet has a score mark.
What should the nurse do while administering this medication?
Explanation
The nurse should give two tablets of medication thrice daily. To find the number of tablets to administer, use the formula: (dose / tablet strength). In this case, (15 g/day / 0.5 g/tablet) = 30 tablets/day.
Divide by three to get the number of tablets per dose: 30 / 3 = 10 tablets/dose.
Each tablet has a score mark, which means it can be split in half.
Therefore, the nurse should give two tablets (or four halves) of medication thrice daily. Niacinamide is a form of vitamin B3 that is essential for many cellular functions and energy production. Niacinamide can be used to treat niacin deficiency, which can cause pellagra, a condition characterized by skin lesions, diarrhea, and mental confusion.
Niacinamide may also have anti-inflammatory and antioxidant effects and may benefit skin health and neurological function..
Robitussin DM contains 100 mg of guaifenesin per 1 teaspoon. How many milligrams of guaifenesin are in 10 mL?
Explanation
Robitussin DM contains 100 mg of guaifenesin per 1 teaspoon. One teaspoon is equivalent to 5 milliliters, so 100 mg is present in 5 mL. Therefore, 10 mL of Robitussin DM contains 2 times the amount of guaifenesin in 1 teaspoon or 200 mg.
A client is prescribed 250 mg of metformin. The pharmacy supplies 500 mg pre- scored tablets of metformin. How should the nurse administer the medication to the client?
Explanation
Administer one half tablet. To find the amount of tablets to administer, use the formula: (ordered dose / available dose). In this case, (250 mg / 500 mg) = 0.5 tablet. Since the tablet is pre-scored, it can be easily split in half.
Metformin is a medication that belongs to a class of drugs called biguanides. It is used to treat type 2 diabetes by lowering blood sugar levels and improving insulin sensitivity. Metformin works by reducing the amount of glucose produced by the liver and increasing the uptake of glucose by the muscles and other tissues.
Metformin can also help prevent or delay the onset of diabetes complications, such as heart disease and kidney damage.
A patient is ordered Amoxil (amoxicillin) 0.5 grams by mouth three times per day. The concentration is 125 mg/5 mL.
How many milliliters per dose should the nurse administer to the patient?
Explanation
The patient is ordered to receive 0.5 grams of amoxicillin three times per day, which is equivalent to 500 mg per dose.
The concentration of amoxicillin is 125 mg/5 mL, which means there is 125 mg of amoxicillin in 5 mL of solution. To calculate how many milliliters per dose the nurse should administer, we can use the following formula:
500 mg / 125 mg per 5 mL = X mL X = 20 mL per dose
Amoxicillin is a type of antibiotic that belongs to the penicillin group of drugs. It is used to treat various bacterial infections, such as ear infections, sinus infections, throat infections, urinary tract infections, and skin infections. Amoxicillin works by interfering with the cell wall synthesis of bacteria, causing them to die or stop growing. Amoxicillin can also be used in combination with other drugs to treat stomach ulcers caused by Helicobacter pylori bacteria.
A client is ordered Mylanta 1 tablespoon by mouth after meals and at bedtime. How many milliliters should the client take with each dose?
Explanation
The correct answer is choice D. 30 mL. To convert a tablespoon measurement to a milliliter measurement, multiply the volume by the conversion ratio of 14.786765 milliliters per tablespoon. In this case, 1 tablespoon x 14.786765 mL/tbsp = 14.786765 mL.
Round up to the nearest whole number to get 15 mL.
However, the ordered dose is 1 tablespoon, not 0.5 tablespoon, so multiply by 2 to get 30 mL. Mylanta is a brand name of an antacid that contains aluminum hydroxide, magnesium hydroxide, and simethicone. It is used to treat symptoms of indigestion, heartburn, gas, and sour stomach.
Mylanta works by neutralizing stomach acid and reducing gas bubbles in the stomach and intestines. Mylanta can also be used to prevent ulcers or bleeding from ulcers in some cases.
A client is prescribed 500 mL of a medication that is available in 2 mg/mL vials. How many mg of the medication should the client receive?
Explanation
To calculate the total amount of medication the client should receive, multiply the volume of the medication by its concentration:
500 mL x 2 mg/mL = 1000 mg
Therefore, the client should receive 1000 mg of the medication.
A physician ordered 5 mL 10% dextrose stat. The only dextrose available is a vial of 5 mL 50% dextrose.
How can the nurse provide the appropriate dose?
Explanation
Dextrose 50%, add 1 mL to 4 mL injectable saline. To obtain 5 mL of 10% dextrose, 0.5 mL of the 50% dextrose should be diluted with 4.5 mL of sterile water or normal saline. Therefore, the nurse should add 1 mL of the 50% dextrose to 4 mL of injectable saline to get a final concentration of 10% dextrose in 5 mL. This will give the client the appropriate dose.
Choice B is incorrect because adding 2 mL of the 50% dextrose to 3 mL of saline would give a final concentration of 20%, which is higher than the prescribed concentration of 10%.
Choice C is incorrect because adding 3 mL of the 50% dextrose to 2 mL of saline would give a final concentration of 30%, which is significantly higher than the prescribed concentration of 10%.
Choice D is incorrect because adding 4 mL of the 50% dextrose to 1 mL of saline would give a final concentration of 40%, which is much higher than the prescribed concentration of 10%.

A patient is ordered 5 mg of IV Lopressor (metoprolol tartrate) to be administered over 60 seconds. The concentration is 1 mg/1 mL.
How many milliliters per minute should the nurse administer to the patient? A. 0.008 mL
Explanation
The patient is ordered to receive 5 mg of Lopressor over 60 seconds, which is equivalent to 1 minute. The concentration of Lopressor is 1 mg/1 mL, which means there is 1 mg of Lopressor in 1 mL of solution. To calculate how many milliliters per minute the nurse should administer, we can use the following formula:
5 mg / 1 mg per 1 mL = X mL X = 5 mL per minute.
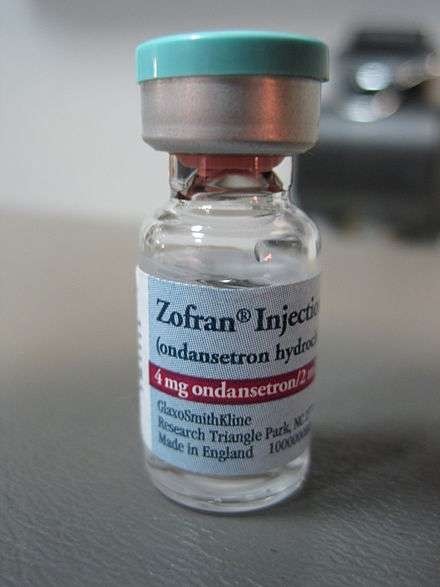
A nurse will administer Zofran (ondansetron) 0.15 mg/kg over 15 minutes. The patient weighs 176 lb. The nurse receives the medication from the pharmacy mixed in 50 mL normal saline...
How should the nurse set the IV pump to deliver the correct dose?
Explanation
The patient is ordered to receive 0.15 mg/kg of Zofran over 15 minutes. The patient weighs 176 lb, which is equivalent to 80 kg. To calculate the total amount of Zofran the patient should receive, multiply the weight by the dosage:
80 kg x 0.15 mg/kg = 12 mg
The Zofran arrives from the pharmacy mixed in 50 mL of normal saline, which means there is 12 mg of Zofran in 50 mL of solution. To calculate how many milliliters per hour the nurse should set the IV pump, we can use the following formula:
50 mL / 0.25 hour = X mL per hour X = 200 mL per hour
Therefore, the nurse should set the IV pump to deliver 200 mL of Zofran per hour to the patient.
A nurse will administer Nubain (nalbuphine) 0.3 mg/kg IV over 10 minutes. The Nubain is available in 10 mg/mL. The patient weighs 148 lb.
How many milliliters per minute of Nubain should the nurse administer?
Explanation
The patient is ordered to receive 0.3 mg/kg of Nubain IV over 10 minutes. The patient weighs 148 lb, which is equivalent to 67.3 kg. To calculate the total amount of Nubain the patient should receive, multiply the weight by the dosage:
67.3 kg x 0.3 mg/kg = 20.19 mg
The Nubain is available in 10 mg/mL, which means there is 10 mg of Nubain in 1 mL of solution. To calculate how many milliliters of Nubain the patient should receive, divide the total amount of Nubain by the concentration:
20.19 mg / 10 mg per mL = 2.019 mL
To calculate how many milliliters per minute the nurse should administer, divide the total volume of Nubain by the infusion time:
2.019 mL / 10 minutes = 0.2019 mL per minute
Rounding to one decimal place, the nurse should administer 0.2 mL of Nubain per minute to the patient.
A physician orders fosphenytoin 0.5 mg/kg IV once daily for a client. The client weighs 57 kg. What is the drug dosage that needs to be administered to the client?
Explanation
To calculate the drug dosage, multiply the prescribed dose per kilogram by the client’s weight in kilograms:
0.5 mg/kg x 57 kg = 28.5 mg

Coumadin 75 mg is ordered for a patient with deep vein thrombosis. Coumadin 25 mg oral tablets are available in the electronic medication administration record.
How many tablets should the nurse administer to the patient?
Explanation
The correct answer is choice C, 3 tablets. To calculate the number of tablets, divide the ordered dose by the available dose:
75 mg ÷ 25 mg = 3
The nurse should administer 3 tablets of Coumadin 25 mg to the patient to give a total dose of 75 mg.
Why is subcutaneous (SC) insulin usually administered into the abdomen as the preferred site?
Explanation
According to the web, the abdomen is the preferred site for insulin injection because insulin is absorbed more quickly and predictably there.
This helps to maintain a stable blood glucose level and avoid hypoglycemia or hyperglycemia.
The other choices are not answers because:
Choice A (it is the least painful location for this injection) is incorrect because pain depends on various factors, such as needle size, injection technique, and individual sensitivity. The abdomen may not be the least painful location for everyone.
Choice B (it causes less bruising at the site) is incorrect because bruising can occur at any injection site if the needle damages a blood vessel. The abdomen does not have less blood vessels than other sites.
Choice C (there are fewer insulin side effects when given in this site) is incorrect because insulin side effects are not related to the injection site, but to the dose, type, and quality of insulin. The abdomen does not reduce the risk of side effects such as allergic reactions, weight gain, or low blood sugar.
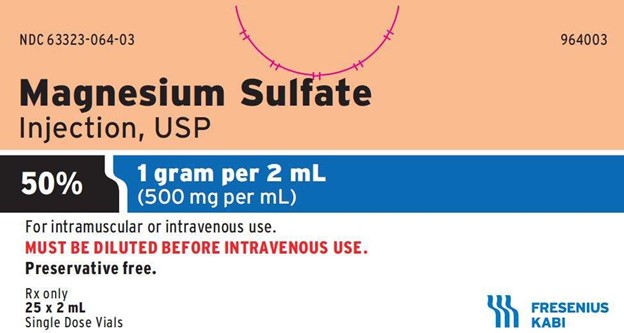
A physician orders magnesium sulfate, 6 grams loading dose to be administered over 30 minutes. There are 40 grams of magnesium sulfate in the IV bag. What is the rate per hour to administer the loading dose?
Explanation
To calculate the rate per hour, divide the amount of magnesium sulfate to be administered by the concentration of magnesium sulfate in the IV bag:
6 grams ÷ 40 grams = 0.15
Then, multiply the result by the volume of the IV bag, which is usually 1000 mL: 0.15 x 1000 mL = 150 mL
This is the amount of fluid that contains 6 grams of magnesium sulfate. To administer this amount over 30 minutes, multiply by 2 to get the rate per hour:
150 mL x 2 = 300 mL/hr.
Morphine sulfate 10 mg IM is ordered. Morphine sulfate 5 mg/mL is available. What volume (mL) should be administered?
Explanation
To calculate the volume to be administered, divide the ordered dose by the available concentration:
10 mg ÷ 5 mg/mL = 2 mL
The nurse should administer 2 mL of morphine sulfate 5 mg/mL to give a total dose of 10 mg.

A patient is ordered 5 mg of IV Lopressor (metoprolol tartrate) to be administered over 2 minutes. The concentration is 1 mg/mL.
How many milligrams per minute should the patient receive?
Explanation
To calculate the amount of drug per minute, divide the total dose by the infusion time in minutes:
5 mg ÷ 2 minutes = 2.5 mg/minute
The patient should receive 2.5 mg of Lopressor per minute for 2 minutes to get a total dose of 5 mg.
A patient with deep vein thrombosis has heparin ordered. Heparin 25,000 units in 250 mL D5W infuses at a rate of 12 mL/hr from 9:00 a.m. to 11:00 a.m. and 10 mL/hr from 11:00 a.m. to 2:00 p.m.
What is the total amount of heparin, in units, that the patient received from 9:00 a.m. to 2:00 p.m.?
Explanation
To calculate the total amount of heparin, we need to multiply the infusion rate by the time and then by the concentration of heparin in the IV bag. From 9:00 a.m. to 11:00 a.m., the infusion rate was 12 mL/hr, so the amount of heparin infused in this period was 12 mL/hr x 2 hours x 100 units/mL = 2400 units.
From 11:00 a.m. to 2:00 p.m., the infusion rate was 10 mL/hr, so the amount of heparin infused in this period was 10 mL/hr x 3 hours x 100 units/mL = 3000 units. The total amount of heparin infused from 9:00 a.m. to 2:00 p.m. was 2400 units + 3000 units = 5400 units.

A client is receiving intravenous infusion of 1.5 L saline solution at a rate of 75 mL/hr.
How many hours will it take to finish the infusion at the current rate?
Explanation
To calculate the time it will take to finish the infusion, we can use the formula:
Time = Volume / Rate
Plugging in the given values, we get:
Time = 1.5 L / 75 mL/hr Converting 1.5 L to mL, we get:
Time = 1500 mL / 75 mL/hr Simplifying, we get:
Time = 20 hours
Therefore, it will take 20 hours to finish the infusion at the current rate.
A client is receiving intravenous infusion of 1.5 L saline solution at a rate of 75 mL/hr.
How many hours will it take to finish the infusion at the current rate?
Explanation
To calculate the time it will take to finish the infusion, we can use the formula:
Time = Volume / Rate
Plugging in the given values, we get: Time = 1.5 L / 75 mL/hr
Converting 1.5 L to mL, we get:
Time = 1500 mL / 75 mL/hr Simplifying, we get:
Time = 20 hours
Therefore, it will take 20 hours to finish the infusion at the current rate.
What is the correct angle for giving an intradermal injection?
Explanation
According to the web, intradermal injections are administered into the dermis just below the epidermis at a 5 to 15 degree angle12 This angle allows for smooth piercing of the skin and induction of the medication into the dermis.
Option B (20 to 35 degrees) is incorrect because it is too steep for an intradermal injection and may cause the medication to enter the subcutaneous layer instead of the dermis.
Option C (45 to 70 degrees) is incorrect because it is too steep for an intradermal injection and may cause the medication to enter the subcutaneous layer instead of the dermis.
Option D (90 degrees) is incorrect because it is too steep for an intradermal injection and may cause the medication to enter the muscle layer instead of the dermis.
A patient is to receive magnesium sulfate 2 grams per hour at 50 mL/hour rate of infusion.
How much magnesium sulfate must be added to 1000 mL normal saline to provide the ordered infusion?
Explanation
To calculate the amount of magnesium sulfate to be added to the normal saline, we can use the formula:
Concentration = Dose / Volume Plugging in the given values, we get:
Concentration = 2 g / 50 mL Simplifying, we get:
Concentration = 0.04 g/mL
To find the amount of magnesium sulfate needed for 1000 mL of normal saline, we can multiply the concentration by the volume:
Amount = Concentration × Volume Amount = 0.04 g/mL × 1000 mL Amount = 40 g
Therefore, 40 g of magnesium sulfate must be added to 1000 mL of normal saline to provide the ordered infusion.
Cefuroxime is available as a suspension of 25 mg in 2 mL. A mother informs a nurse that she gives her child 2 tsp of the suspension once a day orally.
What is the dose that the child receives?
Explanation
To calculate the dose that the child receives, we need to first convert the volume of the suspension from teaspoons to milliliters. One teaspoon is equal to 5 milliliters, so 2 teaspoons is equal to 10 milliliters. Then, we can use the concentration of the suspension to find the amount of cefuroxime in 10 milliliters. The concentration is 25 mg in 2 mL, or 12.5 mg in 1 mL. Therefore, the amount of cefuroxime in 10 mL is:
10 mL × 12.5 mg/mL = 125 mg
Therefore, the child receives 125 mg of cefuroxime once a day orally.
Sign Up or Login to view all the 56 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

