Endocrinology Midterm Exam
Total Questions : 42
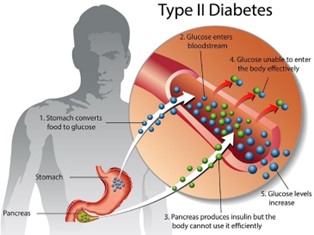
Showing 25 questions, Sign in for moreMary, a 63-year-old patient is newly diagnosed with type 2 diabetes. When determining an education plan, the nurse’s first action should be to?
Explanation
The first step in the education plan should be to assess their understanding and perception of the disease. This will help the nurse to identify any misconceptions or knowledge gaps that the patient may have and tailor the education plan accordingly. Understanding the patient's perceptions will also help the nurse to establish a trusting relationship with the patient and increase their engagement in diabetes self-management.
Options b, c, and d are important components of the diabetes education plan, but they should be implemented after the initial assessment of the patient's perception and understanding of their diagnosis.
A client has been taught to restrict dietary sodium. Which food selection by the client indicates to the nurse that teaching has been effective?
Explanation
This meal choice is low in sodium as it contains fresh ingredients and does not include processed or pre-packaged foods that are typically high in sodium. Chicken, bread, and carrots are naturally low in sodium, and the client can control the amount of added salt or seasoning. In contrast, the other food choices are likely to be high in sodium due to added salt, cheese, or processed ingredients.
Therefore, the nurse should encourage the client to choose fresh, low-sodium foods and avoid processed or pre-packaged meals.

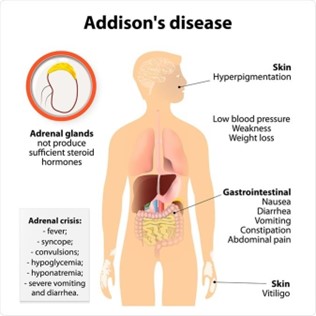
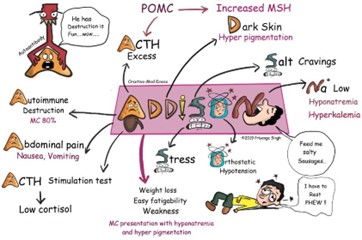
A patient is admitted to the hospital in Addisonian Crisis a month after a diagnosis of Addison’s disease. The nurse identifies the nursing diagnosis of ineffective therapeutic regimen management related to lack of knowledge of management of the condition when the patient says:
Explanation
The statement "I had the stomach flu earlier this week and couldn't take the hydrocortisone" indicates that the patient may not be adhering to their prescribed medication regimen, which can lead to an Addisonian crisis. Therefore, the nursing diagnosis of ineffective therapeutic regimen management related to lack of knowledge of management of the condition is appropriate.
Addison’s disease is a condition in which the adrenal glands do not produce enough cortisol and aldosterone. Hydrocortisone is a glucocorticoid medication that is often used to replace the cortisol that the adrenal glands are not producing. In the Addisonian crisis, the body is unable to produce the necessary levels of cortisol and aldosterone, which can lead to potentially life-threatening complications such as hypotension, dehydration, and electrolyte imbalances.
The other statements may indicate areas where patient education is needed, but they do not directly relate to the immediate risk of an Addisonian crisis.
When admitting a patient with a stroke who is unconscious and unresponsive to stimuli. The nurse learns from the patient’s family that the patient has a history of GERD, the nurse will plan to do frequent assessment of the patient’s:
Explanation
GERD can increase the risk of aspiration (inhalation of stomach contents into the lungs), which can cause respiratory issues, including abnormal breath sounds. In these cases, monitoring of breath sounds may be more appropriate than monitoring of bowel sounds.
Bowel sounds are not typically monitored for GERD patients as GERD is a condition that affects the esophagus and the stomach, not the intestines. GERD is caused by the reflux of stomach contents into the esophagus, which can cause symptoms such as heartburn and regurgitation.
Abdominal girth is not routinely monitored for GERD patients as it is not typically related to the condition. GERD is a disorder that affects the esophagus and stomach and does not typically cause significant changes in abdominal size or girth. In rare cases, GERD can be complicated by a condition known as a para oesophageal hernia, which can cause a visible bulge in the abdomen. In these cases, monitoring of abdominal size and shape may be necessary.
The apical pulse is not routinely monitored for GERD patients as it is not directly related to the condition. GERD is a disorder that affects the digestive system, specifically the esophagus and stomach and does not typically have an impact on heart rate or rhythm.
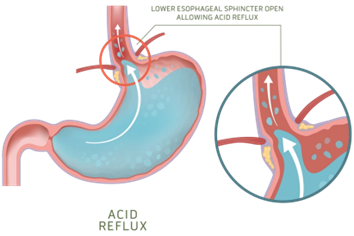
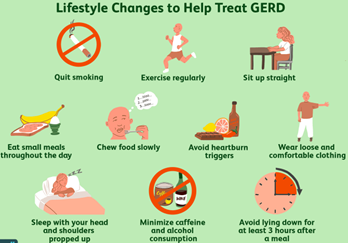
Which information will the nurse include when teaching a patient with newly diagnosed GERD?
Explanation
When teaching a patient with newly diagnosed GERD, the nurse will include that they will need to keep the head of their bed elevated on blocks. This helps prevent stomach acid from flowing back into the esophagus while sleeping.
Peppermint tea might not be helpful in reducing GERD symptoms as it can relax the lower esophageal sphincter and worsen reflux.
Eating between meals is not recommended as it can increase acid secretion. Vigorous physical activities may increase the incidence of reflux.
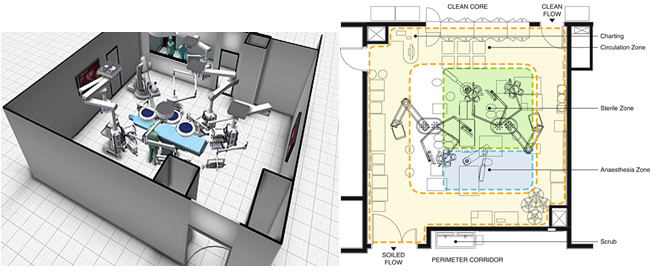
The physical environment and traffic control measures of the operating room are designed primarily to:
Explanation
The operating room is a sterile environment, and it is critical to maintain a clean and controlled environment to reduce the risk of infection to the patient. The measures taken include maintaining positive air pressure, controlling temperature and humidity, filtering the air, using sterile surgical instruments, and limiting traffic in and out of the operating room. These measures help to prevent the spread of infectious agents that may be present in the operating room. While the other options (a, b, and d) may also be important considerations in the design of the operating room, preventing transmission of infection is the primary goal.
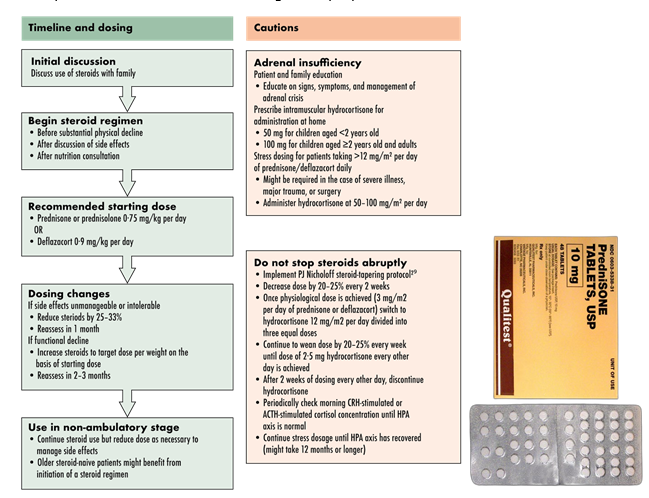
A patient is taking high doses of prednisone to control the symptoms of acute exacerbation of systemic lupus erythematosus. When teaching the patient about the use of prednisone, which information is important for the nurse to include?
Explanation
Sudden discontinuation of prednisone can result in adrenal insufficiency and can lead to life-threatening complications. The nurse should also instruct the patient to report any symptoms of an infection, such as fever, to the doctor promptly, as prednisone can mask signs of an infection.
Monitoring for mood alterations and daily weight measurement are also important aspects of care, but they are not as crucial as the need to gradually taper off the medication.
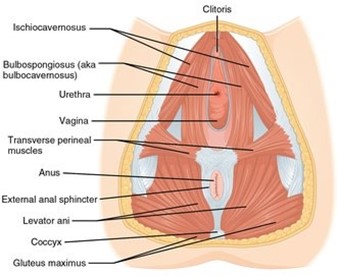
After her bath, a 62-year-old patient asks the nurse for a perineal pad saying that she uses them because sometimes she leaks urine when she laughs or coughs. Which intervention is most appropriate to include in the care plan for the patient?
Explanation
Kegel exercises are designed to strengthen the pelvic floor muscles, which can help improve urinary incontinence. By teaching the patient how to perform Kegel exercises, the nurse can provide a non-invasive, effective intervention that the patient can perform on her own to help manage her urinary incontinence.
Assisting the patient to the bathroom q3hr (b) may help reduce the frequency of incontinence episodes but it does not address the underlying issue of weakened pelvic floor muscles.
Demonstrating how to perform Crede’s maneuver (c) involves applying manual pressure to the bladder to assist with urination and is not appropriate for managing urinary incontinence related to laughing or coughing.
Placing a commode at the patient’s bedside (d) may be appropriate for patients who have difficulty with mobility or accessing the bathroom, but it does not address the underlying issue of weakened pelvic floor muscles causing urinary incontinence.

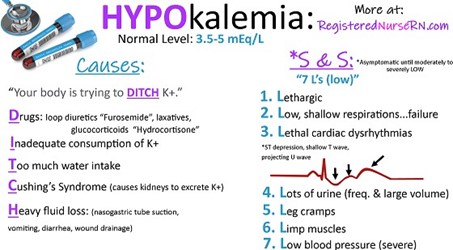
A client is taking furosemide (Lasix), a diuretic. and becomes confused. Which potassium level does the nurse correlate with this condition?
Explanation
Furosemide is a loop diuretic that works by blocking the reabsorption of sodium and chloride in the ascending loop of Henle in the kidney, leading to increased urine output. However, this medication can also cause potassium loss through increased urinary excretion, which can lead to hypokalemia (low potassium level). Hypokalemia can cause confusion, weakness, and other neurological symptoms.
The normal range for serum potassium is 3.5 to 5.0 mEq/L. A potassium level of 2.9 mEq/L is below the normal range and is considered hypokalemic. Therefore, the nurse should correlate the client's confusion with the low potassium level and notify the healthcare provider to adjust the medication or provide potassium supplements if indicated.

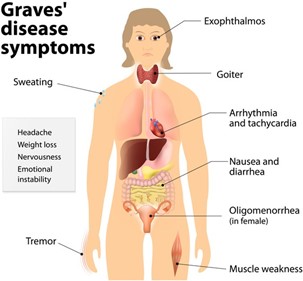
During the nursing assessment of a patient with Graves' disease. The nurse notes a bounding, rapid pulse and systolic hypertension. Based on these assessment data, which question is important for the nurse to ask the patient?
Explanation
The patient's bounding, rapid pulse and systolic hypertension may indicate cardiovascular complications associated with Graves' disease, such as tachycardia, atrial fibrillation, or congestive heart failure, which can cause chest pain. It is important for the nurse to assess for any symptoms of cardiovascular distress and report any abnormal findings to the healthcare provider for prompt intervention. Questions about appetite and constipation may be relevant to the patient's overall health status, but they are not the most important concern in this situation.
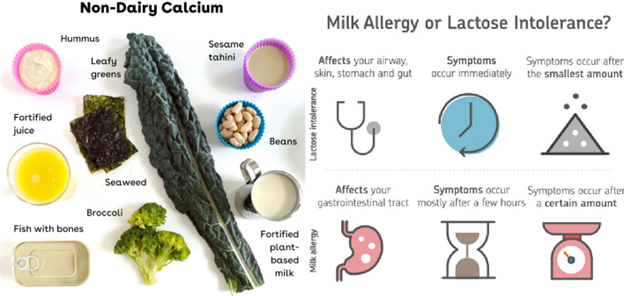
A nurse is teaching nutritional strategies to a client who has a low calcium level and an allergy to milk. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Broccoli and kale are good sources of calcium, and by adding them to their diet, the client can increase their calcium intake without consuming milk. It is important to note that some calcium supplements may irritate the stomach but stopping them altogether is not advisable without consulting a healthcare provider. Vitamin D is not a milk product, and it is essential for calcium absorption. Avoiding foods with vitamin D can worsen the low calcium levels. Cheese is a milk product and may not be suitable for someone with a milk allergy.
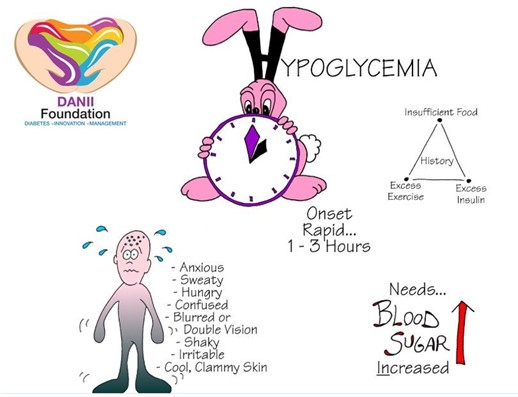
Mr. D receives a daily injection of 70/30 NPH/regular insulin premix at 7:00 AM. The nurse expects that a hypoglycemic reaction is most likely to occur between:
Explanation
The peak time of 70/30 NPH/regular insulin premix is usually 2 to 12 hours after injection, with an average peak time of 4 to 6 hours. This means that the highest risk of hypoglycemia is typically 4 to 6 hours after the injection, which would fall between 11:00 AM and 1:00 PM. However, it's important to note that hypoglycemic reactions can occur at any time, so the client should be monitored closely throughout the day for any signs or symptoms of low blood sugar.
A nurse is planning care for a client who has acute gastritis. Which of the following nursing interventions should NOT be included in the plan of care?
Explanation
Clients with acute gastritis are recommended to eat smaller, frequent meals instead of three large meals. This helps to reduce the workload on the digestive system and allows the stomach to heal. Therefore, option A is not a suitable nursing intervention for a client with acute gastritis.
Options b, c, and d are all appropriate nursing interventions for a client with acute gastritis. Observing stool characteristics can help to identify any bleeding or inflammation in the gastrointestinal tract, evaluating intake and output can help to identify any fluid imbalances, and monitoring laboratory reports of electrolytes can help to identify any imbalances that may occur because of vomiting or diarrhea.
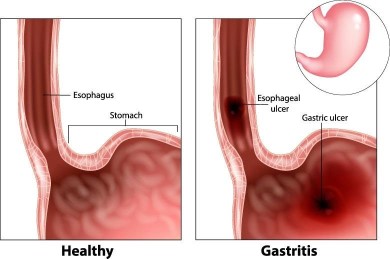
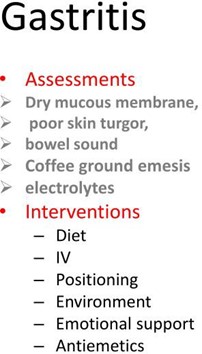
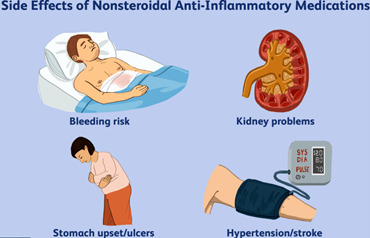
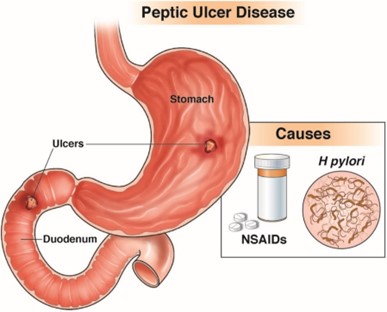
The nurse is admitting a patient who is nauseated and vomiting up blood-streaked fluid with diagnosis of acute gastritis. When obtaining the admission health history, it will be most important for the nurse to ask the patient about:
Explanation
NSAIDs are known to be a common cause of acute gastritis. Therefore, it is essential for the nurse to ask the patient about their frequency of NSAID use to determine if this may have caused their current symptoms. Other options such as family history of gastric problems, recent weight gain or loss, and amount of fat in the diet, may also be relevant to the patient's overall health status, but they are not as important as the potential cause of their current condition.
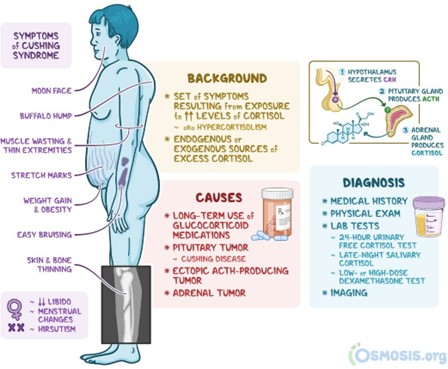
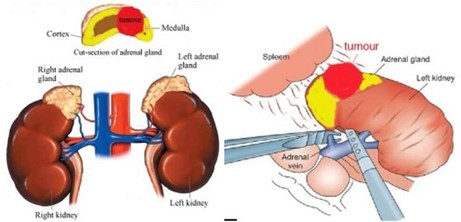
A patient with crushing syndrome is admited to the hospital to have laparoscopic adrenalectomy. During the admission assessment, the patient tells the nurse "The worst thing about this disease is how terrible I look; I feel awful about it.' The best response by the nurse is:
Explanation
This response acknowledges the patient's concerns and provides reassurance that the changes are temporary and will improve after surgery. Response is dismissive of the patient's concerns and may make the patient feel unheard. Response c may be helpful, but it does not address the patient's emotional concerns. Response d is not accurate because the patient has expressed feeling awful about their appearance.
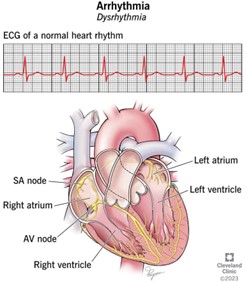
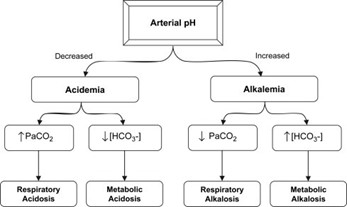
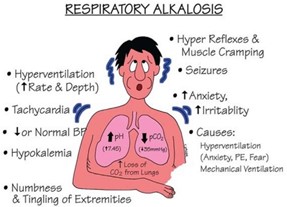
A client comes to the emergency department with Asthma. Based on the documentation noted below, the nurse suspects that the client has what abnormality?
10/1/2022 at 18:30
Client wheezing, RR44, BP 140/90, HR 104, T 98.4 F, ABG results show pH 7.52 mmHg, HCO3-26, PaO2 90 mmHg C. Wynn RN
Explanation
Based on the given documentation, the nurse suspects that the client has respiratory alkalosis. The client's ABG results show a pH of 7.52, which indicates alkalosis and the PaO2 level is slightly low, suggesting respiratory involvement. Rapid breathing (RR44) and wheezing also support the possibility of respiratory alkalosis.
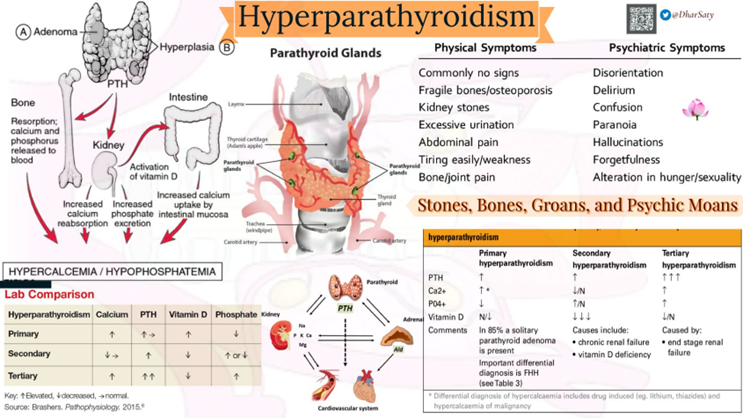
A patient with primary hyperparathyroidism has a serum calcium level of 14 mg/dl (3.5 mmol/L), phosphorus of 1.7 mg/dl (55 mmol/L), serum creatinine of 2.2 mg/dl (194 mmol/L). and high urine calcium. While the patient awaits surgery, the nurse should:
Explanation
The patient with primary hyperparathyroidism has high levels of calcium in the blood (hypercalcemia) which can lead to symptoms such as kidney stones, bone pain, and weakness. High urine calcium levels may also be present due to the increased calcium in the blood.
One important intervention for managing hypercalcemia is to encourage fluid intake to promote increased urine output and prevent the formation of kidney stones. Therefore, the nurse should encourage the patient to drink at least 4000 ml of fluids per day.
Seizure precautions (a), range-of-motion exercises (b), and monitoring for positive Chvostek’s or Trousseaus sign (d) are not directly related to managing hypercalcemia and are not necessary in this case.
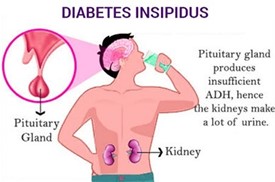
Which of the information below obtained when caring for a patient who has been admited for evaluation of diabetes insipidus will be of greatest concern to the nurse?
Explanation
Diabetes insipidus is a condition where the body is not able to regulate water balance properly, leading to excessive urine output and dehydration. The patient's urine output of 800 ml/hr (option A) and low urine specific gravity of 1.003 (option C) is consistent with diabetes insipidus and requires monitoring, but they are not as immediately concerning as the patient's confusion and lethargy.
Confusion and lethargy may indicate severe dehydration, electrolyte imbalances, or even brain swelling (if the patient had a recent head injury, as mentioned in option D). These symptoms require immediate attention to prevent further complications and ensure the patient's safety.
A patient is hospitalized with acute adrenal insufficiency. The nurse determines that the patient is responding favorably to treatment on finding:
Explanation
One of the hallmarks of adrenal insufficiency is dehydration and decreased urinary output, which can lead to electrolyte imbalances such as hyperkalemia and hyponatremia. As treatment begins to take effect, the patient's fluid and electrolyte balance should improve, leading to an increase in urinary output. Acute adrenal insufficiency, also known as the Addisonian crisis, is a life-threatening condition caused by a sudden decrease in cortisol and aldosterone hormones. Treatment usually involves the administration of intravenous glucocorticoids and mineralocorticoids to replace the deficient hormones.
Decreasing serum sodium (a) and decreasing blood glucose (b) are not signs of improvement but rather indicative of continued adrenal insufficiency. Decreasing serum potassium (c) is also not a sign of improvement as it could indicate that the patient is developing hyperkalemia, which is a potential complication of adrenal crisis.
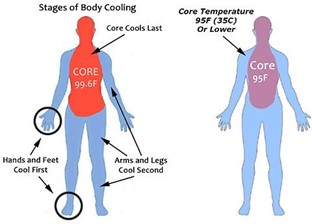
The nurse is caring for a patient with hypothermia and fluid volume excess. Which of the following would be included in the plan of care?
Explanation
The plan of care for a patient with hypothermia and fluid volume excess would typically include measures to increase the patient's body temperature and decrease their fluid volume. Therefore, option a (fluid restriction) would be appropriate for this patient.
Options b (administration of hypotonic IV fluids) and d (administration of ion-exchange resin) would not be appropriate because they would increase the patient's fluid volume rather than decrease it.
Option c (placement of an indwelling urinary catheter) may be appropriate to closely monitor the patient's urine output, which is an important indicator of their fluid status. However, this alone would not be sufficient to manage the patient's hypothermia and fluid volume excess.
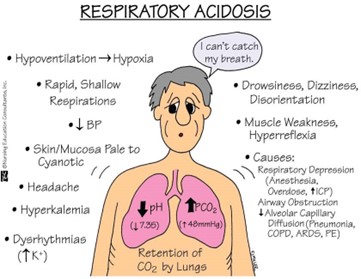
A nurse is admitting a client who has status asthmaticus. The client's ABG results are Ph:7.31, Pa02:74mm Hg, PaC02: 56 mmHg and HCO-3: 26mEq/L The nurse should interpret these laboratory values as which of the following imbalances?
Explanation
The pH value is less than the normal range of 7.35-7.45, indicating acidosis. The PaCO2 value is elevated above the normal range of 35-45 mmHg, indicating respiratory acidosis. The PaO2 value is lower than normal, but not significantly low enough to indicate hypoxemia. The HCO3- level is within the normal range, but not significantly high enough to indicate metabolic compensation for respiratory acidosis.
A nurse is preparing to administer oral potassium to a client who has a potassium level of 5.5 mEq/L. Which of the following actions should the nurse take first?
Explanation
Before administering any medication, the nurse should confirm the potassium level to ensure that it is still elevated and needs to be treated. Potassium levels can fluctuate, so repeating the test will ensure that the client receives the appropriate treatment.
Options (a) Withhold the medication and (b) Administering a hypertonic solution may be appropriate interventions depending on the client's condition, but confirming the potassium level is the first step.
Option (d) Monitoring for paresthesia is important but not the first action that the nurse should take.
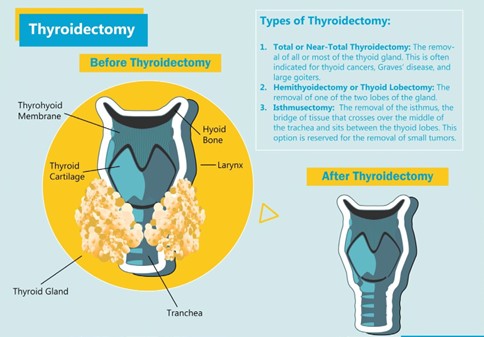
While assessing a patient who has just arrived in the post-anesthesia recovery unit (PACU) after a thyroidectomy, the nurse obtains this data. Which is the most important to communicate to the surgeon?
Explanation
This is a critical finding that could indicate bleeding or compromised airway, both of which are potentially life-threatening complications following a thyroidectomy. Immediate intervention may be necessary to prevent further harm to the patient. The other options are important to note and should be addressed, but they do not require immediate intervention as the swelling in the neck does.
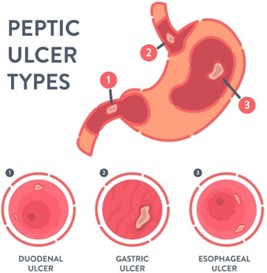
The nurse is caring for a client with diagnosis of peptic ulcer disease. Which assessment finding indicates to the nurse that the client most likely has an ulcer in the stomach rather than the duodenum?
Explanation
Abdominal discomfort an hour after a meal is a common symptom of a gastric ulcer because the stomach is where food is initially processed, and stomach acid is most concentrated. In contrast, duodenal ulcers typically cause pain 2-3 hours after meals, as food moves out of the stomach and into the duodenum, where it encounters duodenal acid.
A positive stool occult blood test is a non-specific finding that can be caused by many gastrointestinal conditions, including peptic ulcers. It does not indicate the location of the ulcer.
The number of ulcers the client has had in the past does not indicate the location of the current ulcer.
Normal hemoglobin and hematocrit levels do not provide information about the location of the ulcer.
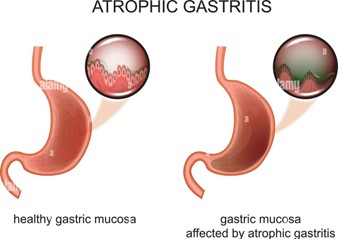
A patient with chronic atrophic gastritis was prescribed monthly Cobalamin (B12) injections The determines that teaching regarding the injections has been effective when the patient States:
Explanation
Chronic atrophic gastritis can lead to a deficiency in vitamin B12, which is needed to produce red blood cells. Without adequate B12, anemia can develop. Cobalamin injections are prescribed to correct the B12 deficiency and prevent anemia. The injections do not increase hydrochloric acid in the stomach, heal the inflamed stomach, or decrease the risk for developing stomach cancer.
Sign Up or Login to view all the 42 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now