Exam 4: Gastrointestinal System
Total Questions : 21
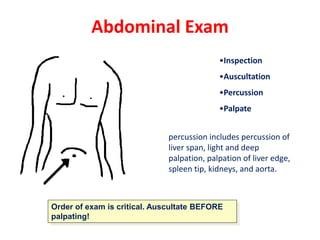
Showing 21 questions, Sign in for moreA nurse performs an abdominal assessment on 4 patients. Which of the following would be considered a normal abdominal assessment?
Explanation
A. abdomen nondistended, soft, with active bowel sounds in all four quadrants.
A normal abdominal assessment would involve an abdomen that is not distended (not bloated or swollen), it feels soft to the touch, and there are active bowel sounds heard in all four quadrants. Bowel sounds refer to the sounds produced by the movement of the intestines and are typically described as gurgling or rumbling noises.
Option A describes a normal assessment because the abdomen is not distended, it feels soft, and there are active bowel sounds in all four quadrants.
Option B is incorrect because a distended abdomen and hypoactive bowel sounds (decreased or absent bowel sounds) are not normal findings.
Option C is also incorrect because a distended abdomen with hyperactive bowel sounds (increased and loud bowel sounds) is not normal.
Option D is incorrect because a nondistended abdomen that feels firm and has hypoactive bowel sounds is also not a normal finding.
A nurse is monitoring bowel elimination of a patient who has a history of constipation. The nurse implements measures to assist with bowel elimination if the patient has not had a bowel movement - what would be the BEST option to try first?
Explanation
Stool softeners, also known as emollient laxatives, work by helping to moisten and soften the stool, making it easier to pass. They are typically taken orally and act by promoting water absorption into the stool, thereby making it softer and easier to pass. This option is often recommended as a first-line treatment for constipation, especially for patients with a history of constipation.
Soap suds enema (option B) is not recommendable as the best option to try first because it involves introducing a solution of soap and water into the rectum to stimulate bowel movement. It is usually used for immediate relief of constipation and is not recommended as the first option.
Suppositories (option C) is not recommendable as the best option to try first because they are medications that are inserted into the rectum to stimulate bowel movement. They work by irritating the lining of the rectum and promoting peristalsis. Suppositories are generally considered to be more invasive than stool softeners and are typically used if other methods have not been successful.
Mineral oil enema (option D) is not recommendable as the best option to try first because it involves introducing mineral oil into the rectum to lubricate the stool and facilitate its passage. This option is also considered more aggressive and is usually used when other methods have failed.
A nurse is preparing a cleansing enema for an adult patient who is constipated and has not responded to laxative use. Before giving the enema, the nurse should
Explanation
The nurse should warm the solution to body temperature before giving the enema to the adult patient. It is important for the solution to be at a comfortable and safe temperature for the patient to avoid any discomfort or injury. This can be achieved by using a thermometer to ensure the solution is warmed to approximately body temperature, which is around 98.6 degrees Fahrenheit (37 degrees Celsius). Microwaving the solution or using boiling water can lead to temperature extremes that could harm the patient. Cooling the solution to 65 degrees Fahrenheit may be too cool and uncomfortable for the patient. Therefore, warming the solution to body temperature is the most appropriate choice.
In option A, cooling the solution to 65 degrees F (option A) may be too cold and uncomfortable for the patient.
In option B, boiling the solution and letting it cool down (option B) is not necessary and may result in a solution that is too hot and potentially harmful to the patient. Boiling the solution is not recommended, as it can alter the composition of the enema and make it less effective.
In option D, warming the solution in the microwave (option D) is not recommended, as it can lead to uneven heating and potentially create hot spots in the solution. Microwaving enema solutions can also cause the solution to become too hot and pose a risk of injury to the patient.
It is important for the nurse to follow the manufacturer's instructions for preparing the cleansing enema solution, ensuring it is warmed to body temperature to provide optimal patient comfort and safety during the procedure.

There is an order to administer a large volume, cleansing enema to an adult patient. The enema bag is filled with how many milliliters of fluid for this procedure?
Explanation
A large volume enema is usually administered with 500 to 1000 mL of fluid. This amount of fluid helps to promote a thorough cleansing of the colon and facilitate the removal of fecal material. However, it's important to note that the specific volume may vary depending on the patient's individual needs, clinical situation, and healthcare provider's instructions.
300 to 500 mL in option (A) is incorrect because its wont help to promote a thorough cleansing of the colon.
200 to 100 mL in option (C) is incorrect because it will not facilitate the removal of fecal material.
50 to 150 ml in option (D) is incorrect because it describes smaller volumes of fluid that would be more suitable for other types of enemas, such as small volume enemas or retention enemas, which have different purposes and indications.
A patient who is constipated has just received a mineral oil-retention enema. The nurse encourages this patient to hold this enema for a minimum of how long?
Explanation
When a patient receives a mineral oil-retention enema for constipation, it is important for them to hold the enema for at least 15 minutes to allow the mineral oil to soften the stool and facilitate its passage. During this time, the patient should try to resist the urge to defecate and retain the enema solution in the rectum for the desired effect.
Holding the enema for just 5 minutes (option A) may not provide sufficient time for the mineral oil to have an optimal effect on softening the stool.
Holding the enema for 60 minutes (option B) is incorrect because is not typically necessary and may cause discomfort or inconvenience to the patient. Most mineral oil-retention enemas do not require such a long duration of retention.
Holding the enema for just 1 minute (option C) is incorrect because is too short a duration for the mineral oil to have any significant effect on softening the stool.
It is important for the nurse to provide specific instructions to the patient regarding the duration of enema retention and ensure the patient understands the importance of following these instructions.
A nurse is digitally removing stool that is impacted from a patient. The nurse should stop the procedure immediately and take corrective action if the patient's
Explanation
During the digital removal of impacted stool, if the patient's pulse rate decreases significantly, it is an indication of a potentially serious condition and the nurse should stop the procedure immediately. A sudden decrease in pulse rate may indicate vagal stimulation, which can lead to a vasovagal response or a more severe cardiovascular event. The nurse should assess the patient's condition, provide appropriate interventions, and notify the healthcare provider as necessary. The other options presented in the question are within normal ranges or do not indicate an immediate need for corrective action.
An increase in blood pressure from 110/84 to 118/88 mm Hg (option A) may not necessarily require immediate action, as it falls within a normal range and may be attributed to factors such as anxiety or pain.
A small increase in temperature from 98.8°F to 99.0°F (option B) may not be alarming on its own and may be within normal fluctuations.
An increase in respiratory rate from 16 to 24 breaths/min (option D) may indicate increased effort or anxiety during the procedure but is not typically a cause for immediate concern unless accompanied by other significant symptoms.

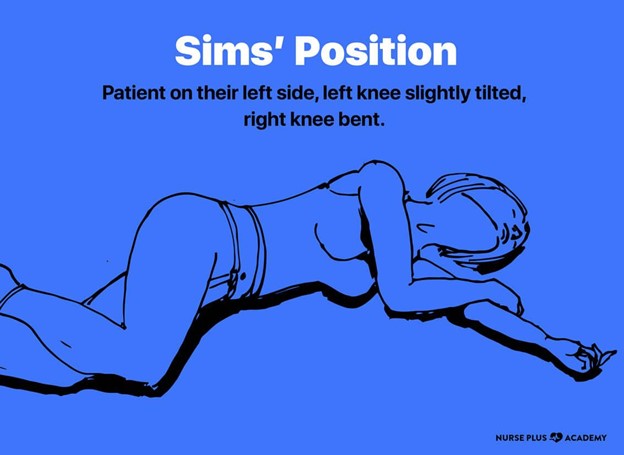
A nurse is preparing her patient to receive a Fleet enema. What position is best for the procedure?
Explanation
When preparing a patient to receive a Fleet enema, the left, lateral side-lying position (also known as the Sims position) is typically the most suitable. This position allows for better access to the rectum, making the administration of the enema easier and more effective. In the Sims position, the patient lies on their left side with the upper knee flexed, which helps to expose the rectal area for the enema administration. It also facilitates the retention of the enema solution, allowing it to flow toward the descending colon.
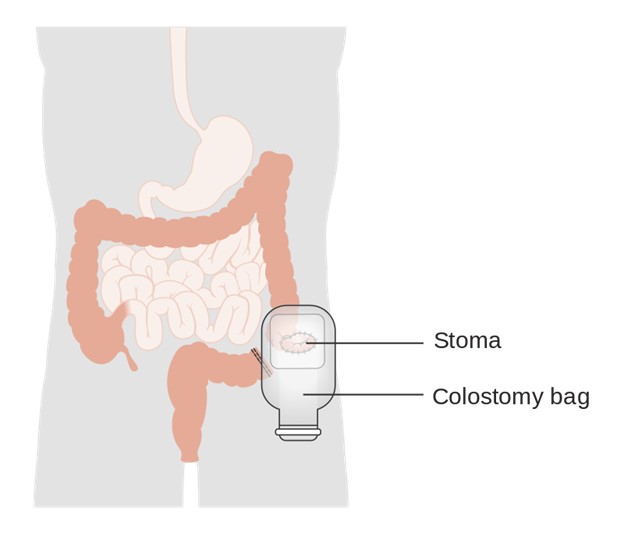
A patient with a colostomy asks how often the faceplate (wafer) of the ostomy appliance should be changed. The most appropriate response by the nurse is that it is usually changed every
Explanation
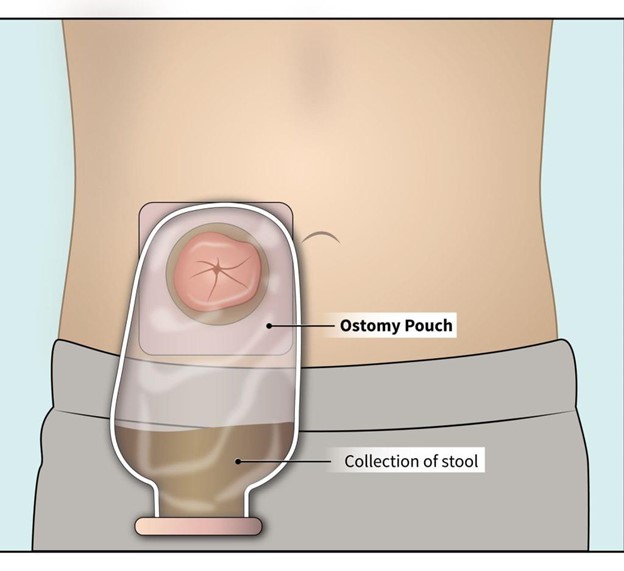
The faceplate, also known as the wafer or barrier, of an ostomy appliance should typically be changed every 3 to 5 days. This timeframe allows for regular maintenance of the stoma and surrounding skin, ensuring proper hygiene and minimizing the risk of skin irritation or infection. However, it's important to note that individual circumstances may vary, and the frequency of faceplate changes can be adjusted based on the patient's specific needs, the type of ostomy, and the condition of the skin. Regular assessment of the stoma and peristomal skin is essential to determine the optimal timing for faceplate changes.
A nurse is caring for a patient with a colostomy. The ostomy drainage bag should be emptied whenever it is
Explanation
The ostomy drainage bag should be emptied whenever it is full. It is important to prevent the bag from becoming too full, as it can put pressure on the ostomy and the skin surrounding it, potentially causing leakage or discomfort for the patient. Regular emptying of the drainage bag ensures proper hygiene and prevents overflow. It is also a good practice to monitor the bag's filling level periodically throughout the day to prevent it from reaching full capacity.
B, C. 1/4 full, and D. % full are not accurate guidelines for emptying the ostomy drainage bag. Waiting until the bag is full is the best practice to avoid overfilling and potential leakage. However, if the patient experiences a high volume of output or the bag fills up quickly, more frequent emptying may be necessary.
It is important for the nurse to educate the patient on how to monitor the bag and recognize signs of fullness, as well as provide instructions on proper bag emptying techniques to maintain good ostomy care.
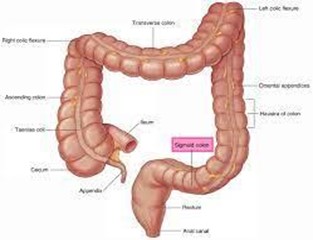
The nurse would expect the least formed stool to be present in which portion of the digestive tract?
Explanation
The least formed stool is expected to be present in the sigmoid colon. As stool passes through the large intestine (colon), it undergoes further water absorption, which gradually increases its firmness and forms it into its characteristic shape. The sigmoid colon is the last portion of the colon, located just before the rectum, and it is where stool is concentrated and becomes more solid before being eliminated from the body.
Let's briefly review the other options:
Ascending colon in (option B) is incorrect because it is the portion of the colon that comes after the cecum and goes up the right side of the abdomen. In this region, water absorption from the stool begins, but the stool is not yet fully formed.
Descending colon in (option C) is incorrect because it is the portion of the colon that comes after the transverse colon and descends along the left side of the abdomen. By this point, more water absorption has occurred, and the stool becomes even more formed.
Transverse colon in (option D) is incorrect because it is the portion of the colon that goes horizontally across the abdomen, between the ascending and descending colon. In this region, significant water absorption occurs, contributing to the further formation of the stool.
In summary, the least formed stool is found in the sigmoid colon, while the stool becomes progressively more formed as it passes through the ascending, transverse, and descending colon.
A patient is having trouble defecating into a bed pan while lying in bed. Which action by the nurse would assist the patient in having a successful bowel movement?
Explanation
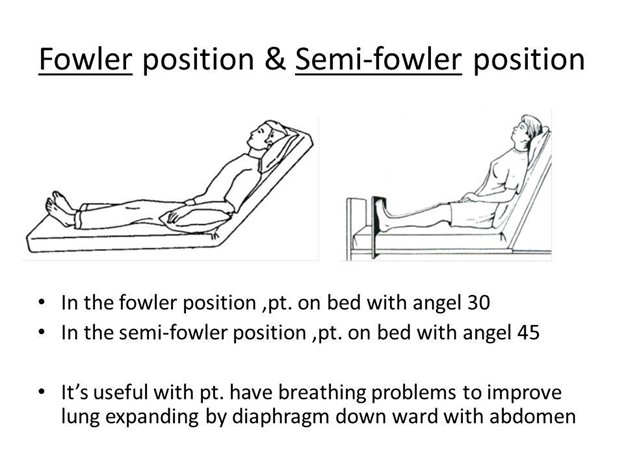
Raising the head of the bed to a semi or high Fowler's position (sitting up at a 30-45-degree angle) can assist the patient in having a successful bowel movement while using a bedpan. This position helps to facilitate gravity, making it easier for the patient to bear down and evacuate their bowels.
Administering laxatives to the patient in (option A) is incorrect because laxatives are medications that help promote bowel movements. While they may be used in some cases of constipation, they might not be the immediate solution for a patient having difficulty using a bedpan.
Preparing to administer a cleansing enema in (option B) is incorrect because Enemas involve introducing liquid into the rectum to stimulate bowel movements. They are typically used for more severe cases of constipation or as part of a bowel preparation before certain medical procedures. For a patient who is simply having trouble using a bedpan while lying in bed, an enema may not be necessary or appropriate at this time.
Withholding narcotic pain medication for at least 2 hours until the patient had a bowel movement successfully in (option C) is incorrect because, while some pain medications, particularly opioids, can cause constipation as a side effect, withholding pain medication solely for this purpose may not be appropriate or safe. Pain management is essential for patient comfort and recovery, and the nurse should find other interventions to assist with bowel movements while maintaining appropriate pain control.
A patient expresses concerns over having bright red stool. Which response by the nurse is most appropriate?
Explanation
Bright red stool can be a sign of gastrointestinal bleeding, and it is essential to take this symptom seriously and investigate its cause. Requesting a stool sample can help identify the presence of blood and determine the possible source of bleeding. Additionally, notifying the Charge RN ensures that the appropriate healthcare professionals are informed, and further evaluation and treatment can be initiated promptly. The nurse should not dismiss or downplay the concern, as it real. Suggesting that severe stress can cause bright red stool may not be accurate and could potentially dismiss the patient's concern without proper investigation.
Option A, "Sometimes severe stress can make the stool bright red," is not an appropriate response. While stress can affect bowel movements, it is important not to dismiss the presence of bright red stool without further investigation.
Option B, "This is probably nothing. Just let me know if it happens again," is not an appropriate. The nurse should not downplay the symptom without further assessment and investigation.
Option D, "You should schedule a colonoscopy as soon as possible," is not an appropriate response. While bright red stool should be investigated, scheduling a colonoscopy would be a more extensive procedure and should be considered based on the findings of the initial assessment and stool sample analysis.
The nurse knows that a bowel training schedule would be most beneficial in the plan of care for which patient?
Explanation
Bowel training programs are typically implemented for patients with fecal incontinence or impaired bowel control. Incontinence refers to the inability to control bowel movements, leading to unintentional passage of stool. Bowel training involves establishing a regular bowel movement routine, which may include scheduled toileting, dietary modifications, and exercises to strengthen the pelvic floor muscles. The aim is to promote regular bowel movements and improve control over bowel function.
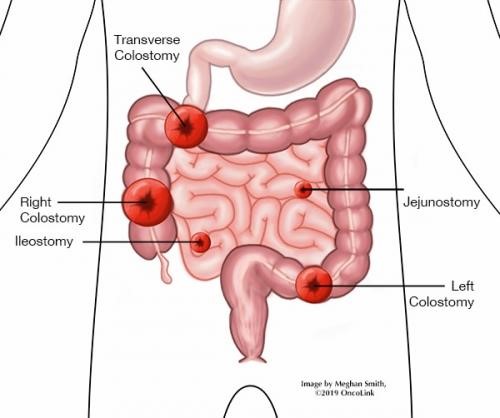
Option A, a 40-year-old patient with an ileostomy, may not benefit from a bowel training schedule because they have a surgically created opening in the ileum, bypassing the colon, and the stool is expected to be liquid and not under voluntary control.
Option C, a 30-year-old patient with C. difficile infection may not be beneficial from bowel training because it would require treatment to eliminate the infection, but a bowel training schedule may not be the primary focus of care for this condition.
Option D, a 25-year-old patient with Crohn's disease, may require management strategies such as medication, dietary adjustments, and lifestyle modifications to control symptoms and promote bowel health, but a bowel training schedule may not be the primary intervention for this condition unless there is associated bowel control impairment.
Which doctor's order should be questioned?
Explanation
Enemas are administered for various reasons, such as bowel preparation, constipation, or to administer certain medications. However, the choice of enema solution should be carefully considered based on the patient's condition and needs.
In this case, giving a hypertonic solution enema to a patient with fluid volume excess (fluid overload) could potentially worsen the patient's condition. Hypertonic solutions draw water from surrounding tissues into the bowel, which could lead to further fluid retention and exacerbate the fluid volume excess.
An oil retention enema for a patient using mineral oil laxatives in (option A) should not be questioned and it is acceptable since the oil retention enema helps lubricate the stool, making it easier to pass. It does not interact negatively with mineral oil laxatives.
A normal saline enema to be repeated every 4 hours until stool is produced in (option B) should not be questioned and it is appropriate if the patient is constipated, and the goal is to help produce a bowel movement. However, the frequency of repeating the enema every 4 hours should be questioned, as frequent enemas can lead to electrolyte imbalances and irritation of the bowel lining.
A Kayexalate enema for a patient with hypokalaemia in (option D) should not be questioned and it is appropriate since Kayexalate is used to treat hyperkalaemia (high potassium levels). The enema helps eliminate excess potassium from the body, thus improving the patient's hypokalaemia condition.

A nurse is educating a patient on how to irrigate an ostomy bag. Which statement by the patient indicates the need for further instruction?
Explanation
Using just any solution that is convenient for irrigating and cleaning an ostomy stoma is not safe and can lead to complications. It is essential to use a specific solution recommended by the healthcare provider for ostomy irrigation. Typically, a healthcare professional will prescribe a sterile irrigation solution that is appropriate for use with the ostomy, and it's crucial to follow their instructions.
Options A, B, and D are all do not indicate a need for further instruction:
In option A, "I should never attempt to reach into my stoma to remove fecal material." - This is a statement that does not require further instruction because reaching into the stoma can cause damage and should be avoided.
In option B, "Using warm enema will reduce cramping and discomfort during the procedure." - This is a statement that does not require further instructions because using a warm solution can help relax the muscles and reduce discomfort during ostomy irrigation.
In option D, "Sitting on the toilet lets the ostomy bag and irritant drain into the toilet bowl." - This is a statement that does not require further instructions because sitting on the toilet allows for easy drainage of both the ostomy bag and the irritant into the toilet bowl during the irrigation process.
The nurse knows that the best way to clean around a colostomy stoma is to use the following
Explanation
Cleaning the area around a colostomy stoma with mild soap and water is the recommended method. This helps to effectively remove any debris, residue, or stool around the stoma while being gentle on the skin. It is important to use a mild, non-irritating soap and lukewarm water.
Option A, cleaning with alcohol swab and letting it air dry, is not recommended as alcohol can be drying and irritating to the skin around the stoma.
Option B, cleaning with tap water, may not be sufficient to remove debris or bacteria effectively. Mild soap is needed to ensure proper cleaning.
Option C, cleaning with iodine only, is not recommended as iodine may be too harsh and can irritate the skin.
An older adult's perineal skin appears to be dry and thin with mild excoriation. When providing hygiene after a bowel movement, the nurse should
Explanation
Option A is the most appropriate choice. Applying a skin protective lotion after cleaning the backside can help moisturize and nourish the dry and thin perineal skin. It creates a barrier that helps protect the skin from further irritation and excoriation. It is important to choose a skin protective lotion specifically formulated for perineal care and suitable for older adults.
Let's go over the other options:
Option B is incorrect because taping an occlusive moisture barrier pad to the skin may not be necessary for mild excoriation and can potentially further irritate the skin. It is not the most appropriate intervention in this situation
Massage the skin with deep kneading pressure in (option C) is incorrect because deep kneading pressure may cause further irritation to the already dry and thin perineal skin, potentially worsening the excoriation. Gentle and cautious care should be taken to avoid excessive pressure or friction
Thoroughly scrub the skin with a washcloth and hypoallergenic soap in (option D) is incorrect because thoroughly scrubbing the skin with a washcloth and hypoallergenic soap can be too harsh for the already compromised perineal skin. It may cause further dryness, irritation, and damage to the skin. Gentle cleansing using mild, non-irritating soap and soft cloths or disposable wipes is more appropriate.
The nurse is caring for an anxious patient who is scheduled for surgery for colostomy placement. While the nurse is talking to the patient, the patient states, "I am so scared."
Explanation
In this situation, the nurse's priority should be addressing the patient's anxiety and fear. The patient has expressed their fear and it is important for the nurse to provide emotional support and reassurance. By acknowledging the patient's fear and addressing it, the nurse can help alleviate anxiety and promote a sense of calmness before the surgery.
Assessing bowel sounds and the presence of gas (option B) is incorrect because it is only important in preoperative assessment. Addressing the patient's anxiety should take precedence as it directly affects the patient's emotional well-being.
The family's questions about the procedure (option C) is incorrect because it can only be addressed after attending to the patient's immediate emotional needs.
Assessing lung sounds and respiratory rate (option D) is incorrect because it is not the immediate priority in this scenario. Addressing the patient's anxiety should take precedence over respiratory assessment unless there are specific indications suggesting a respiratory issue.
The nurse is emptying an ileostomy pouch for a patient. Which assessment finding would the nurse report immediately?
Explanation
Finding blood in the stool from an ileostomy is an abnormal and potentially concerning finding. It could indicate bleeding from the digestive tract, which requires prompt evaluation and medical intervention. The nurse should notify the healthcare provider immediately to ensure appropriate assessment and management of the situation.
Liquid consistency of stool in (option A) will not be reported immediately although it is typical for an ileostomy as it involves the output of liquid stool from the small intestine.
Unpleasant odor from the stool in (option B) is a common characteristic of stool output from an ileostomy. It is important for the nurse to address odor control measures, but it may not require immediate reporting unless accompanied by other concerning symptoms.
Continuous output from the stomach in (option D) is not an expected finding for an ileostomy, as the ileostomy bypasses the stomach. However, this option seems unrelated to the given scenario and is not as urgent as the presence of blood in the stool.
A patient has stools that are foul smelling and that float on water. The nurse documents that this patient is having
Explanation
Steatorrhea refers to the presence of excess fat in the stool, resulting in stools that are foul smelling and float on water. It is often associated with malabsorption or impaired digestion of fats. When fats are not properly digested and absorbed in the intestines, they can pass through the stool, leading to these characteristic features. Steatorrhea can be caused by various conditions such as pancreatic insufficiency, celiac disease, Crohn's disease, or other gastrointestinal disorders that affect fat digestion and absorption.
Rhinorrhea in (option A) is incorrect because it refers to a runny or excessive discharge from the nose.
Amenorrhea in (option B) is incorrect because it refers to the absence of menstruation in females.
Diarrhea in (option D) is incorrect because refers to the passage of loose or watery stools
What foods would increase colostomy odors?
Explanation
A and B. Turnips and Beets are known to contribute to increased colostomy odors. These vegetables contain compounds that can cause a strong odor in the stool and subsequently in the colostomy bag.
B. Buttermilk is also known to increase colostomy odors. It is a fermented dairy product that can have an impact on the smell of stool.
D. Yogurt, on the other hand, is not typically associated with increased colostomy odors. In fact, consuming yogurt can sometimes help regulate bowel movements and reduce odor in the stool due to its probiotic properties.
It is important to note that individuals may respond differently to certain foods, and the impact on colostomy odor can vary from person to person. It is advisable for individuals with a colostomy to work with a healthcare professional or a registered dietitian who can provide personalized dietary recommendations based on their specific needs and preferences.

Sign Up or Login to view all the 21 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

