Fall 2022 N 517 Mental Health Exam 2
Total Questions : 24
Showing 24 questions, Sign in for moreA nurse is caring for a client following a suicide attempt. The client has a history of depression, substance abuse, and anorexia nervosa. Which of the following actions is the nurse's priority?
Explanation
In this scenario, the nurse's priority should be initiating suicide precautions. Safety is of utmost importance when caring for a client following a suicide attempt. By implementing suicide precautions, the nurse can take steps to ensure the client's physical and emotional well-being, such as removing potential means of self-harm and closely monitoring the client's behavior. This action aims to prevent further harm and promote a safe environment for the client.
Incorrect:
B- Administering the Hamilton Depression Scale: While assessing the client's level of depression is important, it is not the priority in this situation. The client has just attempted suicide, indicating a high level of risk. Therefore, the nurse should prioritize safety measures and immediate interventions rather than administering a depression scale.
C- Making a contract with the client for eating behavior: While addressing the client's eating behavior is important, it is not the priority in this situation. The client has just attempted suicide, indicating a significant risk to their life. Ensuring their safety and providing appropriate mental health support take precedence over addressing their eating behavior.
D- Reviewing the client's toxicology laboratory report: While reviewing the client's toxicology report may provide valuable information about substance abuse, it is not the priority in this scenario. The immediate concern is the client's safety following a suicide attempt. The nurse should focus on implementing suicide precautions and addressing the client's emotional and physical well-being.

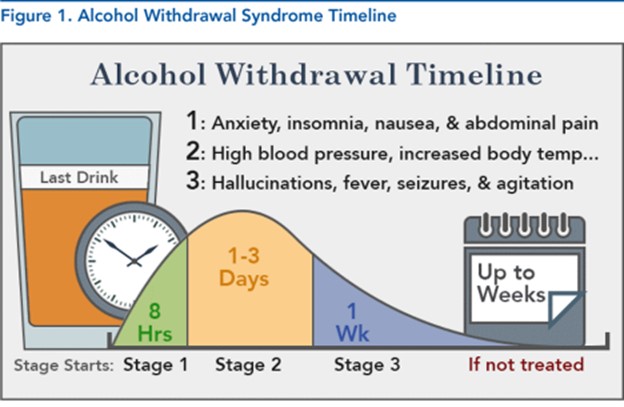
A nurse is caring for a client who is experiencing alcohol withdrawal. Which of the following findings should the nurse expect?
Explanation
Anxiety and diaphoresis: Alcohol withdrawal commonly presents with symptoms of anxiety, restlessness, and excessive sweating (diaphoresis). These symptoms are due to the central nervous system's hyperactivity caused by the sudden cessation of alcohol intake.
Incorrect:
B- Muscle aches and chills: Muscle aches and chills are not typical manifestations of alcohol withdrawal. These symptoms are more commonly associated with opioid withdrawal rather than alcohol withdrawal.
C- Fatigue and depression: Fatigue and depression are common symptoms during alcohol withdrawal. The client may feel tired, lack energy, and experience a low mood due to the neurochemical imbalances that occur during withdrawal.
D- Arrhythmia and respiratory depression: While alcohol withdrawal can lead to some cardiovascular and respiratory symptoms, such as increased heart rate and blood pressure, severe arrhythmia and respiratory depression are not typical findings. These more severe symptoms may indicate a more severe withdrawal syndrome or coexisting medical conditions that require immediate medical attention.
A nurse on the psychiatric unit is assessing a client who has moderate anxiety disorder. Which of the following findings should the nurse expect?
Explanation
Rapid speech: Rapid speech is a common finding in individuals with moderate anxiety. It may manifest as pressured speech, where the client talks quickly, feels a sense of urgency, and may have difficulty pausing or slowing down their speech.
Incorrect:
A- Urinary frequency: Urinary frequency is not typically associated with moderate anxiety disorder. However, in some cases, anxiety can cause an increase in urination due to the body's physiological response to stress. This response is more commonly observed in severe anxiety or panic disorder rather than moderate anxiety.
C- Chills: Chills are not typically associated with moderate anxiety disorder. Chills are more commonly seen in conditions such as infections or fever.
D- Distorted perceptual field: Distorted perceptual field, also known as perceptual disturbances, is not typically associated with moderate anxiety disorder. Perceptual disturbances refer to sensory experiences such as hallucinations or illusions, which are more commonly seen in severe mental health conditions like psychosis or substance-induced disorders.
A nurse in a clinic is caring for a client who is 3 weeks postpartum following the birth of a healthy newborn. The client reports feeling "down" and sad, having no energy, and wanting to cry. Which of the following is a priority action by the nurse?
Explanation
In this scenario, a priority action for the nurse is to ask the client if she has considered harming her newborn. The client's symptoms of feeling "down," sadness, lack of energy, and wanting to cry raise concerns about the possibility of postpartum depression, which is a serious mental health condition that can affect new mothers. In some cases, postpartum depression can lead to thoughts of harming oneself or the newborn. Therefore, it is crucial for the nurse to assess the client's risk and ensure the safety of both the client and her baby.
Incorrect:
A- Reinforce postpartum and newborn care discharge teaching: While reinforcing postpartum and newborn care discharge teaching is an important aspect of care, it is not the priority in this situation. The client's symptoms of feeling "down," sadness, lack of energy, and wanting to cry suggest the possibility of postpartum depression. The nurse should prioritize addressing the client's emotional well-being and assessing for potential risks, rather than focusing on routine postpartum and newborn care teaching.
B- Anticipate a prescription by the provider for an antidepressant: While medication may be part of the treatment plan for postpartum depression, it is not the priority action at this stage. The nurse should first assess the client's condition, including the severity of her symptoms and any potential risk of harm to herself or her newborn. Initiating a discussion about medication can come later, in collaboration with the healthcare provider and based on a comprehensive assessment.
C- Assist the family to identify prior use of positive coping skills in family crises: While supporting the client's family and identifying positive coping skills are important, they are not the priority in this scenario. The immediate concern is addressing the client's symptoms and assessing for potential risks associated with postpartum depression. Once the client's immediate safety and emotional needs are addressed, the nurse can involve the family in the care plan and help them identify and utilize positive coping strategies.
A nurse is assessing a client who is experiencing chronic stress. Which of the following findings should the nurse expect?
Explanation
Increased cognitive awareness: Chronic stress can lead to increased cognitive awareness, but it is important to note that this is not a universal finding. Some individuals may experience difficulty concentrating and impaired cognitive function due to chronic stress, while others may become hypervigilant and more aware of their surroundings.
Incorrect:
A- Hypotension: Hypotension, or low blood pressure, is not typically associated with chronic stress. In fact, chronic stress often leads to increased sympathetic nervous system activity, which can result in elevated blood pressure.
B- Viral infection: While chronic stress can have an impact on the immune system, it does not necessarily mean the client will have a viral infection. Prolonged stress may weaken the immune system, making individuals more susceptible to infections, but it does not guarantee the presence of a viral infection.
D- Increased energy: Chronic stress typically leads to a state of exhaustion and fatigue rather than increased energy. Prolonged stress can drain a person's physical and mental energy, resulting in feelings of fatigue, lethargy, and a lack of motivation.
A nurse is caring for a client admitted to a mental health facility who asks, "Can I refuse the electroconvulsive therapy (ECT) treatment so for tomorrow?" Which of the following should be the nurse's response?
Explanation
Informed consent is an essential ethical principle in healthcare, including mental health treatment. Even if the client has previously signed a consent form for electroconvulsive therapy (ECT), they have the right to change their mind and refuse the treatment at anytime. Respecting the client's autonomy and their right to make decisions about their own healthcare is crucial.
The nurse's response should support the client's right to refuse the treatment, rather than attempting to persuade or convince them otherwise. It is important to provide information, answer questions, and discuss the client's concerns or reasons for refusing the treatment. The client's decision should be respected and further discussions can be held with the healthcare provider to explore alternative treatment options or address any concerns the client may have.
A- "You have given signed consent for the treatments after they were explained to you." - This response does not acknowledge the client's right to refuse the treatment. Even if the client previously provided consent, they still have the right to change their mind and refuse the treatment. Informed consent is an ongoing process, and the client's autonomy should be respected throughout their care.
B- "You can refuse them, but the provider believes they are necessary." - While it may be true that the healthcare provider believes ECT is necessary, this response does not fully acknowledge the client's autonomy. It is important to emphasize the client's right to make decisions about their own healthcare, independent of the provider's opinion. The decision to refuse or accept the treatment should ultimately be made by the client.
C- "You will feel better after the course of treatments." - This response does not address the client's concerns or their right to refuse the treatment. It is essential to respect the client's autonomy and their ability to make decisions about their own care, even if their decision may not align with the potential benefits of the treatment. The nurse should focus on providing information, addressing the client's concerns, and supporting their decision-making process.
A nurse is assessing a client who has a history of alcohol use disorder. Which of the following questions should the nurse include to deter the use of alcohol affects the client's psychosocial behaviors?
Explanation
This question directly addresses the impact of alcohol use on the client's work-related behaviors and performance, which is an essential aspect of their psychosocial functioning. It can provide valuable information about potential impairments in work productivity, relationships with colleagues, and overall job stability.
While the other questions are also relevant and important in assessing a client with a history of alcohol use disorder, they focus on different aspects of the client's history and treatment. For example:
B- "Do you receive treatment for any mental health disorders?" helps to assess if there are coexisting mental health issues that may be contributing to or affected by alcohol use.
C- "At what age did you begin drinking alcohol?" helps to understand the timeline of the client's alcohol use and potential early risk factors for developing alcohol use disorder.
D- "Have you received prior treatment for substance use disorder?" provides insights into the client's past attempts at addressing their alcohol use and any prior experiences with treatment.
A nurse observes that a client who has depression is sitting alone in the room crying. As the nurse approaches, the client states, "I'm feeling really down and don't want to talk to anyone right now." Which of the following responses should the nurse make?
Explanation
This response acknowledges the client's feelings and respects their desire for space and silence. By offering to sit with the client, the nurse provides a comforting presence without pressuring the client to talk or share their emotions. It shows understanding and support for the client's current emotional state.
The other options may not be as helpful in this situation:
A- "Why are you feeling so down?" can be seen as intrusive and may make the client feel defensive or overwhelmed. It's important to respect the client's boundaries and not push them to explain their feelings if they are not ready.
B- "It might help you feel better if you talk about it." While talking about feelings can be beneficial for some individuals, it should be done on the client's terms. Pressuring the client to talk about their emotions may create additional distress.
C- "I understand. I've felt like that before, too." While sharing personal experiences can be a way to establish rapport, it should be done cautiously and with consideration for the client's unique situation. In this case, the focus should be on the client's needs rather than the nurse's experiences.
A school nurse is talking with a 13-year-old female at her annual health-screening visit. Which of the following comments made by the adolescent should be the nurse's priority to address?
Explanation
This comment indicates that the adolescent is concerned about a developmental milestone and comparing herself to her peers. It is important for the nurse to address this issue as it relates to the adolescent's physical and emotional well-being.
Menarche (the onset of menstruation) is a significant milestone in a girl's life, and the timing can vary among individuals. Some girls may start their periods earlier or later than their peers, and this can lead to feelings of insecurity or worry. The nurse should provide education and reassurance to the adolescent, explaining that the timing of menarche can vary and that it is a normal part of development.
The other comments, while important, may not require immediate attention:
B- "My parents treat me like a baby sometimes." This comment suggests a possible issue with parent-child dynamics, but it does not indicate an immediate health concern. The nurse may explore this further during a counseling session or refer the adolescent to a school counselor if necessary.
C- "There's a big pimple on my face, and I worry that everyone will notice it." While acne can impact an adolescent's self-esteem, it is not a priority issue from a health perspective. The nurse can provide support, discuss basic skincare practices, and offer guidance on managing acne if appropriate.
D- "None of the kids at this school like me, and I don't like them either." While social interactions are important for an adolescent's well-being, this comment does not indicate an immediate health concern. The nurse can explore this further during a counseling session or refer the adolescent to a school counselor for additional support
A nurse is caring for a client who is experiencing acute manifestations of withdrawal from alcohol. Which of the following medications should th nurse expect to administer to the client?
Explanation
Diazepam belongs to the benzodiazepine class of drugs and is commonly used to manage the symptoms of alcohol withdrawal. It helps alleviate anxiety, agitation, tremors, and seizures that can occur during alcohol withdrawal. Diazepam has sedative effects and helps prevent and treat alcohol withdrawal seizures by acting on the central nervous system.
Incorrect:
A- Disulfiram is a medication used to support alcohol abstinence by creating unpleasant reactions if alcohol is consumed. It is not typically administered during acute alcohol withdrawal.
B- Naltrexone is used to help individuals with alcohol dependence reduce their alcohol cravings and drinking behavior. It is not typically used during the acute phase of alcohol withdrawal.
D- Acamprosate is a medication used to maintain abstinence from alcohol in individuals who have already stopped drinking. It is not typically used during the acute phase of alcohol withdrawal.
A nurse caring for a client who has depression observes the client comes to breakfast freshly bathed wearing clean clothes, and styled hair. Which of the following responses by the nurse is therapeutic?
Explanation
This response acknowledges the client's effort and self-care without making assumptions or imposing judgment. It is an open and non-intrusive statement that shows the nurse is paying attention to the client's appearance and recognizing their positive action of self-grooming. It allows the client to share their feelings or thoughts if they choose to without feeling pressured or judged. This response demonstrates empathy and understanding, creating a supportive and non-threatening environment for the client to express themselves if they wish to do so.
Incorrect:
A- "Why are you all dressed up today?" This question may put the client on the spot and make them feel self-conscious or defensive. It assumes that there must be a specific reason for the client's appearance, which may not be the case. It can also imply that the client's usual appearance is different or not as desirable.
C- "Everyone feels better after showering." While it is true that personal hygiene can have a positive impact on one's mood, this statement may come across as dismissive or oversimplifying the client's experience. It may invalidate any underlying emotions or struggles the client is facing with their depression. It is important to acknowledge and address the client's feelings rather than making broad generalizations.
D- "You must be getting better. You look great." This statement assumes that physical appearance is directly correlated with the client's mental health and suggests that improvement in appearance equates to improvement in mental well-being. However, a person's outward appearance may not accurately reflect their internal struggles or progress in managing depression. Additionally, it can create pressure for the client to maintain a certain appearance to be perceived as "better."
A nurse is planning care for a client who has depression. The nurse notes that the client has weight loss, an inability to concentrate, an inability to complete everyday tasks, and a preference to sleep all day. Which of the following interventions should be included in the plan of care?
Explanation
Clients with depression may experience cognitive difficulties, such as trouble concentrating or articulating their needs. Giving the client extra time to express themselves and communicate their needs allows them to feel heard and understood. It also helps establish a therapeutic relationship with the client, promoting trust and collaboration in their care.
The other interventions listed may not be appropriate or effective in addressing the client's specific symptoms of depression:
A- Instructing the family to avoid visiting during mealtimes may not be necessary unless there are specific reasons related to the client's preferences or distractions during meals. It's important to involve the family in the client's care and support, including mealtime interactions, unless there are specific concerns or circumstances.
C- Offering three or four large meals daily may not be appropriate for all clients with depression. Some individuals may have a decreased appetite or experience changes in their eating patterns. It is important to assess the client's nutritional needs and preferences and provide a balanced meal plan tailored to their specific situation.
D- Discouraging rest periods during the daytime may not be helpful, as individuals with depression may experience fatigue, lack of energy, and a desire to sleep more. Adequate rest and sleep are important for overall well-being, and it is crucial to support the client in maintaining a regular sleep schedule and addressing any sleep disturbances they may be experiencing.
A nurse is assessing a client who is experiencing acute cocaine toxicity. Which of the following findings should the nurse expect?
Explanation
Tremors: This choice is correct. Tremors or muscle twitching can be expected in a client experiencing acute cocaine toxicity. Cocaine is a central nervous system stimulant that can cause overstimulation of muscles, resulting in tremors.
Incorrect:
A- Hypothermia: This choice is incorrect. Acute cocaine toxicity is associated with an increase in body temperature (hyperthermia) rather than a decrease (hypothermia). Cocaine is a stimulant that can cause the body to overheat, leading to hyperthermia, which is a dangerous condition that requires immediate medical attention.
B- Hypotension: This choice is incorrect. Cocaine is a stimulant that increases blood pressure and heart rate, leading to hypertension (high blood pressure), not hypotension (low blood pressure). Hypertension is a common cardiovascular effect of cocaine use.
D- Respiratory depression: This choice is incorrect. Respiratory depression, which is a slowing of the respiratory rate and depth, is more commonly associated with depressant drugs like opioids or benzodiazepines. As a stimulant, cocaine tends to have the opposite effect, leading to increased respiratory rate (tachypnea) and sometimes hyperventilation.

A nurse on an inpatient mental health unit is admitting a client who has panic-level anxiety. After showing the client to his room, which of the following nursing actions is most therapeutic at this time?
Explanation
Remaining with the client provides them with a sense of security, reassurance, and support. It shows the client that they are not alone and that the nurse is there to provide assistance and care. By being present and offering a calming presence, the nurse can help the client feel more at ease and gradually reduce their anxiety.
It's important to note that the other options are not the most appropriate actions in this situation:
A- Having the client join a therapy group may be overwhelming and may not be suitable during the acute phase of panic-level anxiety.
B- Suggesting that the client rest in bed may not address their immediate anxiety and may not be feasible if the client is experiencing intense anxiety symptoms.
D- Medicating the client with a sedative should be done based on a healthcare provider's order and assessment of the client's condition. It is not the initial therapeutic intervention and should only be considered if other non-medication interventions are ineffective or if the client's anxiety becomes severe and unmanageable.
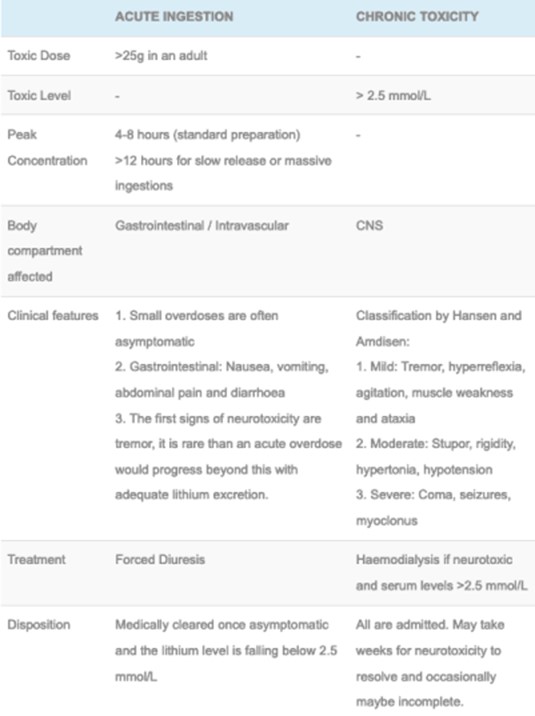
A nurse is providing discharge teaching to a client who has bipolar disorder and will be discharged with a prescription for lithium. The nurse should teach the client that which of the following factors puts her at risk for lithium toxicity?
Explanation
Excessive sodium intake can increase the risk of lithium toxicity because it affects the balance of electrolytes in the body and can interfere with lithium excretion. Clients taking lithium should maintain a consistent level of sodium intake and avoid sudden or excessive changes in their sodium consumption.
The other options listed are not directly related to the risk of lithium toxicity: A- Running 4 miles outdoors every afternoon is not a risk factor for lithium toxicity.
B- Drinking 2 liters of liquids daily is actually beneficial as it helps maintain hydration and can aid in flushing out the lithium from the body.
D- Eating foods high in tyramine is not associated with lithium toxicity. Tyramine-rich foods are typically a concern when taking certain medications, such as monoamine oxidase inhibitors (MAOIs), but not lithium.
A charge nurse is providing teaching to a staff nurse about assisting the provider with electroconvulsive therapy (ECT). Which of the following responses by the staff nurse indicates understanding of the teaching?
Explanation
Obtaining informed consent is a crucial step before administering electroconvulsive therapy (ECT). Informed consent ensures that the client is fully informed about the procedure, its potential risks and benefits, and any alternative treatments available. It allows the client to make an autonomous decision regarding their treatment.
The other responses are not accurate:
A- "ECT is an effective treatment for personality disorders." While ECT may be used in certain cases of severe mental illness, it is not primarily indicated for personality disorders.
B- "It is a myth that clients experience seizures during ECT." Seizures are a common and expected effect of ECT. ECT involves the induction of controlled seizures under anesthesia.
D- "Should monitor the client closely for hypotension following ECT." While monitoring the client for various physiological changes is important, hypotension is not a primary concern following ECT. The nurse would typically monitor for potential adverse effects such as confusion, memory loss, headache, and muscle soreness.
A charge nurse is discussing suicide interventions with nursing staff. Which of the following should the nurse identify as an example of secondary intervention?
Explanation
Secondary interventions are aimed at reducing the harm or preventing further complications in individuals who have already engaged in suicidal behavior. In this case, performing life-saving measures after a suicide attempt, such as cardiopulmonary resuscitation (CPR) or administering first aid, falls under the category of secondary intervention.
The other options are examples of primary and tertiary interventions:
A- Recognizing the warning signs of suicide: This is an example of primary intervention, which focuses on preventing suicidal behavior before it occurs by raising awareness, promoting mental health, and identifying risk factors and warning signs.
B- Identifying individuals who are at higher risk for attempting suicide: This is also an example of primary intervention, as it involves assessing and identifying individuals who may be at greater risk for suicidal behavior and implementing preventive measures.
D- Providing support for family and friends following a suicide: This is an example of tertiary intervention, which aims to provide support and care to those who have been affected by a suicide, including family and friends. Tertiary interventions focus on postvention, addressing the aftermath and providing support for survivors.
A nurse is caring for a client who is having difficulty sleeping and is pacing the floor. The client's head down, and he is wringing his hands. Which of the following actions should the nurse take?
Explanation
Remaining with the client demonstrates a supportive and therapeutic presence. It can help provide a sense of safety, reassurance, and comfort to the client who is experiencing difficulty sleeping and exhibiting signs of anxiety or restlessness. By staying with the client, the nurse can actively listen, observe, and assess the client's needs, allowing for prompt intervention if necessary.
A- Giving a PRN (as-needed) sleeping medication should not be the first response, as it is important to explore non-pharmacological interventions and address the underlying cause of the client's difficulty sleeping.
B- Exploring alternatives to pacing the floor with the client may be an appropriate intervention after assessing the client's needs and preferences.
C- Encouraging the client to go back to bed may not be effective if the client is experiencing significant anxiety or restlessness.
A nurse notices that a client who has moderate anxiety is pacing the hall and mumbling As the nurse approaches the client, he states, "I am at the end of my rope. I don't think I can take any more bad news." Which of the following responses should the nurse make?
Explanation
This response demonstrates a therapeutic and empathetic approach to the client's distress. By offering to talk in a private area without interruption, the nurse provides the client with a safe space to express their feelings and concerns. It also allows the nurse to conduct a more in-depth assessment of the client's current emotional state and any specific triggers contributing to their anxiety.
A- Encouraging the client to lie down assumes that all clients with anxiety benefit from this approach, which may not be the case for everyone.
B- Simply suggesting medication may not address the underlying concerns or provide an opportunity for the client to express themselves.
C- While relaxation exercises can be beneficial for managing anxiety, suggesting them right away may not be the best response when the client is in a heightened state of distress.
A nurse is admitting a client who has multiple injuries following a motor vehicle crash. Shortly after admission, the client's partner distraught and blames himself for the accident. Which of the following responses should the nurse make?
Explanation
This response acknowledges the client's distress and invites them to share their thoughts and feelings about the situation. It shows empathy and demonstrates active listening, allowing the nurse to gather more information about the client's emotional state and concerns. By giving the client an opportunity to express themselves, the nurse can provide appropriate support and address any guilt or self-blame the client may be experiencing.
Dismissing the client's concerns and redirecting the conversation to their partner's condition (Option A) may invalidate the client's feelings and prevent them from processing their own emotions.
Telling the client to calm down (Option B) may come across as dismissive and insensitive.
Asking the client why they think the crash is their fault (Option C) may put the client on the defensive and hinder open communication. The best approach is to actively listen to the client's concerns and create a supportive environment for them to share their feelings.
A nurse is caring for a client who reports acute, moderate anxiety. Which of the following is the priority nursing action?
Explanation
By remaining with the client, the nurse provides a sense of support and security. This presence can help alleviate the client's anxiety and provide reassurance. It also ensures that the nurse is available to assess the client's condition, offer therapeutic communication, and intervene if the anxiety escalates or the client becomes overwhelmed.
While the other options are also beneficial interventions for managing anxiety, they are not the priority in this situation. Instructing the client to remember past coping mechanisms (Option A) can be helpful, but the immediate presence of the nurse is more important to provide immediate support.
Providing a diverting activity (Option B) can be beneficial to distract the client from their anxiety, but it does not address the underlying anxiety or provide direct support.
Encouraging verbalization of feelings (Option C) is important for therapeutic communication, but it may not be the initial priority when the client is experiencing acute anxiety.
A nurse is teaching a community education course about the physical complications related to substance use disorder. Which of the following findings should the nurse include in the discussion as a health risk of heroin use?
Explanation
Heroin is an opioid drug that depresses the central nervous system, which can lead to respiratory depression. This means that heroin can slow down a person's breathing rate, potentially leading to shallow breathing or even stopping of breathing altogether. This is a life-threatening complication and one of the most significant dangers of heroin use.
The other options listed are associated with other substances or conditions:
A- Nasal septum perforation is commonly associated with the use of cocaine, not heroin.
C- Acute pancreatitis is not a commonly reported complication of heroin use.
D- Permanent short-term memory loss is not a specific complication of heroin use, though chronic substance abuse can lead to cognitive impairments and memory problems in general.

A nurse is caring for an adolescent female who has an eating disorder. The client is 162.6 cm (64 in) tall and weighs 38.56 kg (85 lb). Upon assessment, which of the following manifestations should the nurse expect? (Select all that apply.)
Explanation
When caring for an adolescent female with an eating disorder, the nurse should expect the following manifestations:
A- Amenorrhea: Amenorrhea refers to the absence of menstruation, which is commonly seen in individuals with eating disorders, particularly in cases of severe weight loss or malnutrition.
B- Altered body image: Individuals with eating disorders often have a distorted perception of their body shape and size. They may see themselves as overweight or have a negative body image, even when they are significantly underweight.
C- Hyperactivity: Some individuals with eating disorders may exhibit excessive physical activity or restlessness. This hyperactivity can be a result of increased energy expenditure, driven by a fear of weight gain or a compulsive need to burn calories.
E- Bradycardia: Bradycardia, or a slow heart rate, is a common finding in individuals with severe malnutrition or very low body weight. It can be a result of the body's adaptive response to conserve energy in a state of limited food intake.
Incorrect:
D- Verbalized desire to gain weight is not typically expected in individuals with eating disorders. They may express a desire to lose weight or have a fear of gaining weight instead.
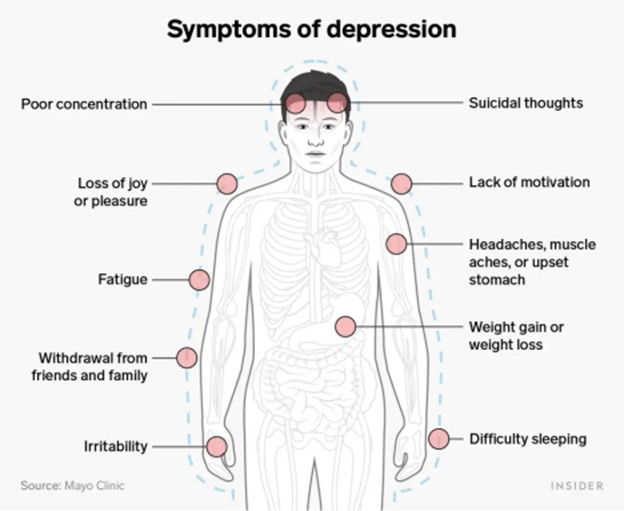
A nurse is caring for an adolescent who is experiencing indications of depression. Which of the following findings should the nurse expect? all that apply.)
Explanation
When caring for an adolescent experiencing indications of depression, the nurse should expect the following findings:
A- Irritability: Depression can manifest as increased irritability or anger, especially in adolescents. They may become easily annoyed or frustrated.
B- Insomnia: Sleep disturbances are common in depression. Adolescents may experience difficulty falling asleep, staying asleep, or have restless and disturbed sleep.
C- Chronic pain: Depression can be associated with physical symptoms, including chronic pain. Adolescents may complain of headaches, stomachaches, or other unexplained physical discomfort.
D- Low self-esteem: Depression often involves feelings of worthlessness, guilt, and low self-esteem. Adolescents may have negative thoughts about themselves, feel inadequate, or have a distorted self-perception.
Incorrect:
E- Euphoria, on the other hand, is not a typical finding in depression. It refers to an intense state of happiness or excitement, which is not consistent with the overall mood of depression.
Sign Up or Login to view all the 24 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

