RN > Exit Exams
Exam Review
HESI Exit II
Total Questions : 119
Showing 10 questions, Sign in for moreA client who is hypotensive is receiving dopamine, an adrenergic agonist, IV at the rate of 8 mcg/kg/min. Which intervention should the nurse implement while administering this medication?
Explanation
Choice A: Assessing pupillary response to light hourly is not related to dopamine administration. Dopamine does not affect the pupils or the cranial nerves that control them.
Choice B: Initiating seizure precautions is not necessary for a client receiving dopamine. Dopamine does not lower the seizure threshold or cause convulsions.
Choice C: Measuring urinary output every hour is an important intervention for a client receiving dopamine. Dopamine increases blood pressure and cardiac output, which improves renal perfusion and urine production. Urinary output is an indicator of the effectiveness of dopamine therapy and renal function.
Choice D: Monitoring serum potassium frequently is not directly related to dopamine administration. Dopamine does not affect potassium levels or cause hyperkalemia or hypokalemia. However, potassium levels may be affected by other factors such as fluid balance, renal function, and medications.

Explanation
Choice A: Assessing pupillary response to light hourly is not related to dopamine administration. Dopamine does not affect the pupils or the cranial nerves that control them.
Choice B: Initiating seizure precautions is not necessary for a client receiving dopamine. Dopamine does not lower the seizure threshold or cause convulsions.
Choice C: Measuring urinary output every hour is an important intervention for a client receiving dopamine. Dopamine increases blood pressure and cardiac output, which improves renal perfusion and urine production. Urinary output is an indicator of the effectiveness of dopamine therapy and renal function.
Choice D: Monitoring serum potassium frequently is not directly related to dopamine administration. Dopamine does not affect potassium levels or cause hyperkalemia or hypokalemia. However, potassium levels may be affected by other factors such as fluid balance, renal function, and medications.
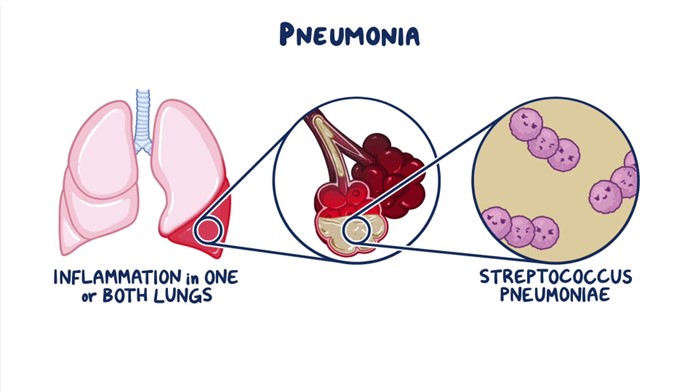
In caring for a client who is receiving linezolid IV for nosocomial pneumonia, which assessment finding is most important for the nurse to report to the health care provider?
Explanation
Choice A: Yellow-tinged sputum is not a serious adverse effect of linezolid. It may indicate an infection or inflammation in the respiratory tract, but it does not require immediate attention from the health care provider.
Choice B: Nausea and headache are common side effects of linezolid. They are usually mild and self-limiting, and they can be managed with supportive measures such as hydration, rest, and analgesics.
Choice C: Watery diarrhea is a sign of pseudomembranous colitis, a potentially life-threatening complication of linezolid. It is caused by an overgrowth of Clostridium difficile bacteria in the colon, which produce toxins that damage the intestinal mucosa. It can lead to dehydration, electrolyte imbalance, sepsis, and perforation. The nurse should report this finding to the health care provider immediately and stop the linezolid infusion.
Choice D: Increased fatigue is not a specific or serious adverse effect of linezolid. It may be related to the underlying infection, anemia, or other factors. It does not require urgent intervention from the health care provider.
Explanation
Choice A: Increasing oral fluids may help with hydration, but it will not reduce skin flushing caused by lisinopril. Lisinopril is an angiotensin-converting enzyme (ACE. inhibitor that dilates blood vessels and lowers blood pressure. Flushing occurs due to increased blood flow to the skin.
Choice B: Nitroglycerin is a vasodilator that relaxes smooth muscle in blood vessels and reduces chest pain caused by angina. It is not indicated for skin flushing caused by lisinopril. Moreover, nitroglycerin can lower blood pressure further and cause hypotension, headache, dizziness, and fainting.
Choice C: Going to an emergency department is not necessary for skin flushing caused by lisinopril. Flushing is not a sign of an allergic reaction or anaphylaxis, which would require immediate medical attention. Flushing is also not a symptom of a heart attack or stroke, which would present with other signs such as chest pain, shortness of breath, arm numbness, or slurred speech.
Choice D: Reassuring the client that facial flushing is a common side effect of lisinopril is the best action for the nurse to take. Flushing is not harmful or dangerous, and it usually subsides within a few hours. The nurse should explain the mechanism of action of lisinopril and its benefits for lowering blood pressure and preventing angina. The nurse should also advise the client to monitor his blood pressure regularly and report any signs of hypotension, such as dizziness, lightheadedness, or fainting.
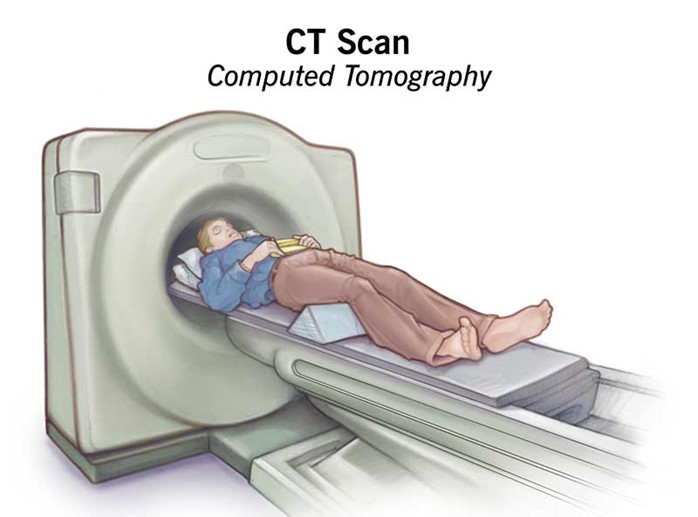
A client is being urgently transported to radiology for a Computerized Tomography (CT scan) after a sudden decrease in level of consciousness. The client is orally intubated and has a left lateral chest tube to 20 cm suction. Which action is most important for the nurse to take?
Explanation
Choice A: Securing chest tube to the stretcher for transport is a good practice, but it is not the most important action. The chest tube should be secured to prevent accidental dislodgement or kinking, but it does not affect the function of the chest tube or the drainage system.
Choice B: Administering PRN pain medication prior to transport is a compassionate action, but it is not the most important action. The client may experience pain due to the chest tube, the intubation, or the underlying condition, but pain relief is not a priority over maintaining adequate ventilation and drainage.
Choice C: Marking the amount of chest drainage on the container is a useful action, but it is not the most important action. The amount of chest drainage should be recorded and reported to monitor the client's status and detect any complications, such as hemorrhage or infection, but it does not affect the immediate function of the chest tube or the drainage system.
Choice D: Keeping the chest tube container below the site of insertion is the most important action for the nurse to take. The chest tube container should be kept below the level of the client's chest to maintain a gravity-dependent pressure gradient that allows air and fluid to drain from the pleural space. If the container is raised above the site of insertion, it can cause backflow of air or fluid into the pleural space, which can compromise ventilation and cause tension pneumothorax.
Explanation
Choice A: Administering a half dose now is not advisable, because it may result in underdosing or overdosing of digoxin. Digoxin has a narrow therapeutic range and a high risk of toxicity, especially in infants and children. The amount of digoxin absorbed by the infant before vomiting is unknown, so giving a partial dose may not achieve therapeutic levels or may exceed safe levels.
Choice B: Giving another dose is not advisable, because it may result in overdosing of digoxin. Digoxin has a narrow therapeutic range and a high risk of toxicity, especially in infants and children. The amount of digoxin absorbed by the infant before vomiting is unknown, so giving a full dose may exceed safe levels and cause adverse effects such as nausea, vomiting, bradycardia, arrhythmias, or visual disturbances.
Choice C: Mixing the next dose with food is not advisable, because it may affect the absorption and bioavailability of digoxin. Digoxin should be taken on an empty stomach or at least one hour before or two hours after meals, because food can interfere with its absorption from the gastrointestinal tract and reduce its effectiveness.
Choice D: Withholding this dose is the best instruction for the nurse to provide to this mother. Digoxin has a long half-life and accumulates in tissues, so missing one dose will not significantly affect its therapeutic effect. Withholding this dose will avoid overdosing and toxicity of digoxin, which can be life-threatening in infants and children. The nurse should also advise the mother to resume the regular dosing schedule and monitor the infant's pulse rate and signs of digoxin toxicity.
Explanation
Choice A: Observing insertion site is an essential assessment for a client who has a suprapubic catheter. The insertion site is located in the lower abdomen, where urine drains from an opening in the bladder through a catheter into a drainage bag. The nurse should inspect the site for signs of infection, inflammation, bleeding, or leakage. The nurse should also clean the site with soap and water and apply a sterile dressing as needed.
Choice B: Palpating flank area is not a relevant assessment for a client who has a suprapubic catheter. The flank area is located on the sides of the back, where the kidneys are located. Palpating the flank area can detect tenderness or pain that may indicate kidney infection or stones, but it does not provide information about the suprapubic catheter or its function.
Choice C: Measuring abdominal girth is not a relevant assessment for a client who has a suprapubic catheter. The abdominal girth is the circumference of the abdomen at the level of the umbilicus. Measuring abdominal girth can detect changes in fluid balance, ascites, or bowel obstruction, but it does not provide information about the suprapubic catheter or its function.
Choice D: Assessing perineal area is not a relevant assessment for a client who has a suprapubic catheter. The perineal area is located between the anus and the genitals. Assessing perineal area can detect signs of infection, irritation, or injury in the genital or anal regions, but it does not provide information about the suprapubic catheter or its function.
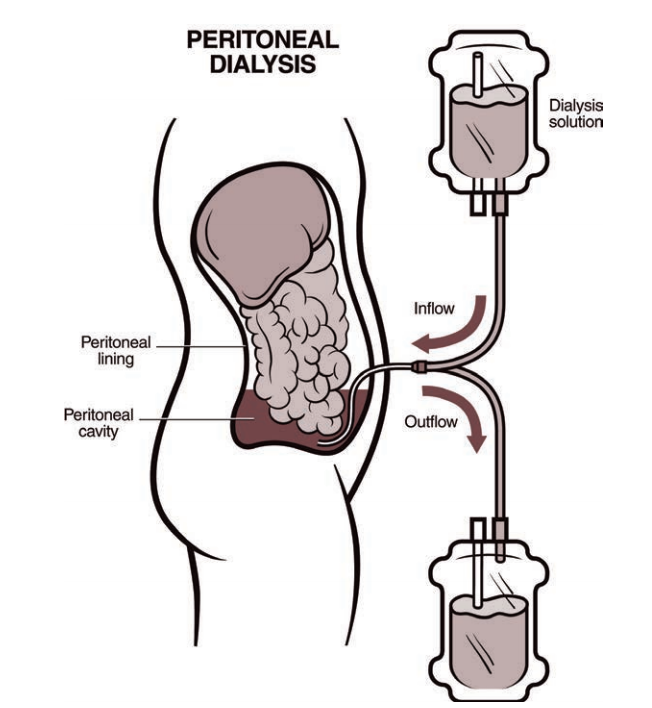
A client is receiving continuous ambulatory peritoneal dialysis since the arteriovenous (AV) graft in the right arm is no longer available for use for hemodialysis. The client has lost weight, has increasing peripheral edema, and has a serum albumin level of 1.5 g/dL (15 g/L). Which intervention is the priority for the nurse to implement?
Serum Albumin Reference Range: 3.5 to 5.5 g/dL (35 to 55 g/L)
Explanation
Choice A reason: Support stockings may help with peripheral edema, but they are not the priority intervention for this client. The client's low serum albumin level indicates malnutrition and increased risk of infection and poor wound healing.
Choice C reason: Evaluating patency of the AV graft is not the priority intervention for this client because the client is receiving peritoneal dialysis, not hemodialysis. The AV graft may be used in the future if peritoneal dialysis fails, but it is not an immediate concern.
Choice D reason: Instructing the client to follow fluid restriction amounts is important for peritoneal dialysis patients, but it is not the priority intervention for this client. The client's low serum albumin level indicates that fluid restriction alone is not sufficient to manage fluid balance and prevent edema.
Text 1:
The nurse is providing lifestyle change education for a client to slow the progression of coronary artery disease. Which statement(s) made by the client should the nurse recognize as needing additional education? (Select all that apply.)
Explanation
Choice A reason: Consuming foods with saturated fats can increase the level of low-density lipoprotein (LDL) cholesterol in the blood, which can contribute to plaque formation and narrowing of the coronary arteries.
Choice B reason: Walking 30 minutes per day can help lower blood pressure, improve blood circulation, and reduce the risk of heart attack and stroke.
Choice C reason: Using a salt substitute can help lower sodium intake, which can reduce fluid retention and lower blood pressure.
Choice D reason: Keeping a food diary can help the client monitor their calorie intake, portion size, and nutritional balance.
Choice E reason: Eating more canned vegetables can increase sodium intake, which can worsen fluid retention and blood pressure. Fresh or frozen vegetables are preferable.
Choice F reason: Including oatmeal for breakfast can provide soluble fiber, which can lower LDL cholesterol and prevent plaque formation in the coronary arteries.
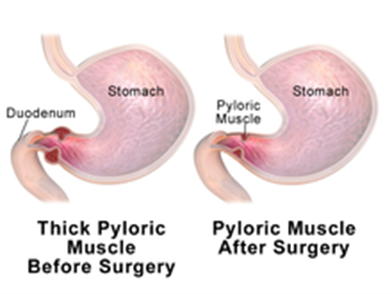
A 6-week-old infant with poor weight gain is scheduled for a pyloromyotomy. Which pre-operative nursing action has the highest priority?
Explanation
Choice A reason: Marking an outline of the "olive-shaped" mass in the right epigastric area is not a priority nursing action. The mass is caused by hypertrophy of the pyloric sphincter, which obstructs gastric emptying and causes projectile vomiting. The mass may not be palpable in all cases.
Choice C reason: Monitoring amount of intake and infant's response to feedings is important, but not the highest priority. The infant may have difficulty feeding due to nausea, vomiting, and abdominal pain.
Choice D reason: Instructing parents regarding care of the incisional area is a post-operative nursing action, not a pre-operative one. The parents will need to learn how to keep the incision clean and dry, monitor for signs of infection, and administer pain medication as prescribed.
Sign Up or Login to view all the 119 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

