Exam Review
HESI Exit LPN Exam 1
Total Questions : 75
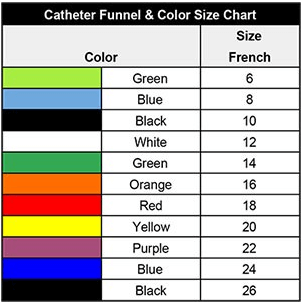
Showing 10 questions, Sign in for moreThe practical nurse (PN) is observing a newly hired PN who is preparing to administer a liquid medication via a client's feeding tube system as seen in the picture. What action should the PN take?
Explanation
Demonstrate how to administer medication via a feeding tube.The picture shows that the newly hired PN is about to make a serious error by adding the medication directly to the feeding bag, which can cause clogging, contamination, or inaccurate dosing of the medication. The PN should demonstrate how to administer medication via a feeding tube correctly, which involves stopping the feeding, flushing the tube with water, instilling the medication, flushing again, and resuming the feeding.
The other options are not correct because:
- Confirming that the medication is only administered once daily is not relevant or helpful, as it does not address the error or teach the correct technique of administering medication via a feeding tube.Determining if the medication is compatible with the solution is not necessary or appropriate, as the medication should not be mixed with the solution in the first place, but given separately through the feeding tube.
- Offering to assist in calculating the rate of flow for the mixture is not relevant or helpful, as there should be no mixture of medication and solution in the feeding bag, but separate administration of each through the feeding tube.
A client with obsessive-compulsive disorder (OCD) reports, "Thoughts stick in my mind and the rituals I use are stupid, but I cannot control them. People laugh at me, but they do not understand how awful it is. I am a burden to my family because I cannot hold a job. I do not know how much longer I can live this way." Which information is most important for the practical nurse (PN) to ask in response to the client's statements?
Explanation
This is the most important information for the PN to ask because it assesses the client's risk for self-harm and suicidal ideation. The client's statements indicate hopelessness, low self-esteem, and impaired functioning, which are potential warning signs of suicide. The PN should ask the client directly about any thoughts or plans of harming themselves and provide support and safety measures as needed.

The practical nurse (PN) is assisting in a community center clinic when four clients simultaneously arrive seeking help. In which order should the PN prioritize care to be provided based on the client needs? (Arrange the client with the highest priority first, on top, and lowest priority last, on botom.)
Explanation
A 12-year-old child with history of asthma who is wheezing and complaining of shortness of breath.
This client has the highest priority, as he or she may be experiencing an acute asthma atack that can compromise the airway and oxygenation. The PN should assess the client's respiratory status, administer bronchodilators, and monitor for improvement or deterioration.
A 7-year-old child who has type 1 diabetes mellitus and is experiencing extreme hunger and shakiness.
This client has the second highest priority, as he or she may be experiencing hypoglycemia, which is a low blood glucose level that can cause neurologic symptoms such as confusion, seizures, or coma. The PN should check the client's blood glucose level, provide a source of glucose, and monitor for recovery or complications.
A 10-year-old child with bleeding lacerations on both knees after falling on the playground.
This client has the third highest priority, as he or she may have a risk of infection or blood loss from the wounds. The PN should clean and dress the lacerations, apply pressure if needed, and check for signs of infection or inflammation.
A 5-year-old child who is crying uncontrollably because of an incontinent bowel episode.
This client has the lowest priority, as he or she does not have a life-threatening or urgent condition, but a psychosocial or emotional issue. The PN should provide comfort and reassurance to the child, change his or her clothes, and explore the possible causes of the incontinence.
An elderly client is 12-hours postoperative for a hernia repair and suddenly becomes agitated, staggers out into the corridor, and demands to be set free.
After assisting the client back to bed and administering pain medication, which intervention is best for the practical nurse (PN) to implement?
Explanation
c. Raise the side rails and notify the family to come and stay until the client is reoriented and cooperative.
The client may be experiencing postoperative delirium, which is a transient state of confusion, disorientation, agitation, or hallucinations that can occur after surgery, especially in elderly clients. The PN should raise the side rails and notify the family to come and stay with the client, as this can provide safety, comfort, and reassurance for the client.
The other options are not correct because:
- Administering a prescribed narcotic antagonist may not be appropriate or necessary, as the client's agitation may not be caused by analgesic accumulation, but by other factors such as hypoxia, infection, electrolyte imbalance, or sensory deprivation.
- Notifying the healthcare provider and requesting a prescription for restraints may not be the best intervention, as restraints can increase the client's agitation, anxiety, or injury. Restraints should be used only as a last resort when other measures have failed or when there is an imminent risk of harm.
d. Instructing a UAP to keep the upper side rails up and check on the client every 15 minutes may not be sufficient or effective, as the client may still try to get out of bed or become more agitated by being left alone. The PN should involve the family or stay with the client until he or she is calm and oriented.
Which actions should the practical nurse (PN) include when assessing a client for signs and symptoms of fluid volume excess? (Select all that apply.)
Explanation
The PN should palpate the rate and volume of the pulse, measure body weight at the same time daily, and observe the color and amount of urine when assessing a client for signs and symptoms of fluid volume excess. These actions can help detect changes in the cardiovascular, renal, and fluid balance systems that may indicate fluid overload, such as tachycardia, bounding pulse, weight gain, edema, oliguria, or dark urine.
The other options are not correct because:
b. Checking fingernails for the presence of clubbing is not relevant for assessing fluid volume excess, as clubbing is a sign of chronic hypoxia or lung disease that causes enlargement of the fingertips and nails.
e. Comparing muscle strength of both arms is not relevant for assessing fluid volume excess, as muscle weakness is not a specific sign of fluid overload, but may be caused by various factors such as electrolyte imbalance, nerve damage, or fatigue.
The charge nurse brings a #18 urinary catheter with a 30 mL balloon to the practical nurse (PN) who is preparing to insert a catheter in a female client who weighs 50 kg. Which action should the PN take first?
Explanation
This is the first action that the PN should take because the catheter size and balloon volume are inappropriate for the client. A #18 urinary catheter is too large for a female client who weighs 50 kg, and a 30 mL balloon may cause bladder trauma or discomfort. The PN should consult with the charge nurse and obtain a smaller catheter (such as #14 or #16) with a 10 mL balloon.
The birth weight of an infant delivered by a woman with gestational diabetes is 10.1 pounds (4,581 grams). The infant is jitery and has a heel stick glucose level of 40 mg/dL (2.2 mmol/L) 30 minutes after birth. Based on this information, which intervention should the practical nurse (PN) implement first?
Reference range:
Blood glucose neonate: [30 to 60 mg/dL or 1.7 to 3.3 mmol/L]
Explanation
b. Begin frequent feedings of breast milk or formula.
The infant has hypoglycemia, which is a low blood glucose level that can cause jiteriness, lethargy, seizures, or coma. Hypoglycemia is common in infants of mothers with gestational diabetes, as they produce excess insulin in response to high maternal glucose levels. The PN should begin frequent feedings of breast milk or formula, as this can provide a source of glucose and stimulate the infant's own glucose production.
The other options are not correct because:
a. Offering nipple feedings of 10% dextrose may be indicated in some cases of severe hypoglycemia, but it is not the first intervention. The PN should try oral feedings of breast milk or formula first, as they are more natural and less invasive.
c. Repeating the heel stick for glucose in one hour may be necessary to monitor the infant's glucose level, but it is not the first intervention. The PN should treat the hypoglycemia first, as it can have serious consequences if left untreated.
d. Assessing for signs of hypocalcemia may be important, as hypocalcemia is another possible complication in infants of mothers with gestational diabetes, but it is not the first intervention. The PN should address the hypoglycemia first, as it is more urgent and more likely to cause jiteriness.
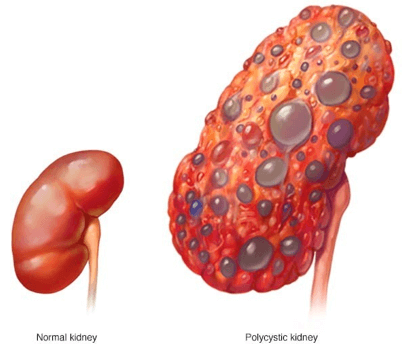
A client is being treated for chronic kidney disease (CKD). On examination, the client has an elevated blood pressure (BP) and is exhibiting changes in mental status. Which intervention in the plan of care should the practical nurse (PN) implement?
Explanation
This is the best intervention for the PN to implement because it monitors the client's fluid status and helps detect fluid overload, which can cause hypertension and neurological changes. The PN should weigh the client at the same time, on the same scale, and with the same clothing every day.
The practical nurse (PN) prepares to remove a client's saline lock. Which supplies should the PN gather? (Select all that apply.)
Explanation
They are needed to remove the saline lock safely and prevent bleeding or infection. The PN should wear exam gloves to protect themselves and the client from contamination, apply a small gauze pad over the insertion site, and secure it with paper tape after removing the saline lock.
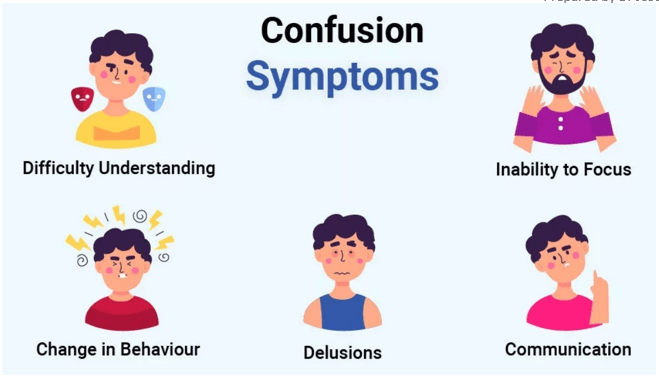
An older female adult who was admited to a long-term care facility yesterday is confused about what day of the week it is. Her history does not indicate that she was confused prior to admission. What action should the practical nurse (PN) take?
Explanation
it provides reality orientation and helps the client cope with the change in environment. The client may be experiencing acute confusion or delirium due to stress, medication, infection, or other factors. The PN should remind the client of the date, time, and place frequently and use other strategies such as calendars, clocks, and familiar objects to reduce confusion.
Sign Up or Login to view all the 75 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

