HESI Leadership
Total Questions : 49
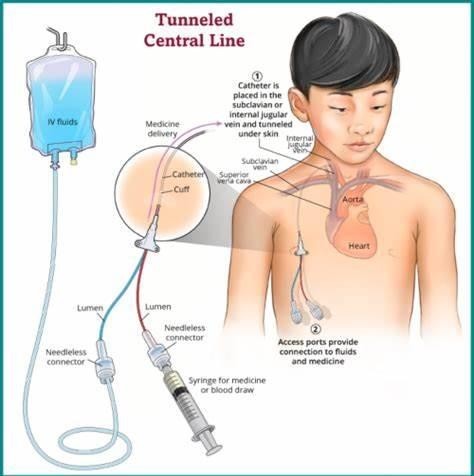
Showing 25 questions, Sign in for moreSeveral nurses who work on a postoperative surgical unit have reported to the charge nurse their concerns about a particular surgeon's treatment of clients during invasive procedures. Adult clients are often in tears after this particular physician performs central IV line insertions or other invasive procedures. After the charge nurse confronts the healthcare provider who dismisses the concerns, the charge nurse reports the surgeon's behavior to the nurse manager who listens but does nothing about the situation. What action is most important for the charge nurse to take?
Explanation
Choice A reason: Confronting the nurse manager as a group may not be effective or appropriate, as it may create more conflict and resentment. The charge nurse should follow the chain of command and escalate the issue to a higher authority if the nurse manager fails to act.
Choice B reason: Attending procedures performed by the surgeon and demanding halting of the procedure if the client becomes distressed may be seen as insubordination and interference by the surgeon, who may have legal authority to perform the procedure. It may also jeopardize the client's safety and outcome.
Choice C reason: Documenting client reactions to invasive procedures performed by the physician in their medical record is important, but not sufficient. It does not address the root cause of the problem, which is the surgeon's lack of empathy and respect for clients' pain and dignity.
Choice D reason: Reporting the physician's lack of concern for clients' pain during invasive procedures to the Director of Nursing is the most important action for the charge nurse to take, as it may lead to an investigation and corrective measures. The Director of Nursing has more power and responsibility than the nurse manager to deal with such issues and protect clients' rights and welfare.
The nurse receives a change-of-shift report from the prior nurse assigned to a group of clients on a post-surgical unit. Which client requires the most immediate intervention by the nurse?
Explanation
Choice A reason: This client may have an infection or sepsis, which are life-threatening complications of surgery. The nurse should assess the client's vital signs, wound appearance, and laboratory results, and notify the physician immediately.
Choice B reason: This client has a chest tube to drain the pleural fluid and re-expand the lung. The amount of drainage is within normal limits and does not indicate an emergency. The nurse should monitor the client's respiratory status, oxygen saturation, and chest tube function.
Choice C reason: This client has a gunshot wound that may have caused tissue damage and bleeding. The dressing with 2 cm-sized dark red drainage may indicate fresh bleeding, but it is not excessive. The nurse should check the dressing for signs of infection, change it as ordered, and report any changes to the physician.
Choice D reason: This client has a Jackson-Pratt drain to collect the fluid from the surgical site after a mastectomy. The amount of serosanguineous fluid is expected and does not indicate a problem. The nurse should empty and measure the drain output, record it, and report any abnormalities to the physician.
Four clients are scheduled to receive IV infusions, but there are only three intravenous (IV) pumps available. Which prescribed infusion can most safely be administered without an IV infusion pump?
Explanation
Choice A reason: Ceftriaxone is an antibiotic that can be given by gravity infusion without an IV pump, as long as the nurse monitors the flow rate and adjusts the roller clamp as needed. The dose and duration of ceftriaxone are usually fixed and not affected by minor fluctuations in the infusion rate.
Choice B reason: Heparin is an anticoagulant that requires a precise and constant infusion rate to prevent bleeding or clotting complications. An IV pump is essential to deliver heparin safely and accurately.
Choice C reason: Magnesium is an electrolyte that can cause serious adverse effects such as cardiac arrhythmias,
respiratory depression, and muscle weakness if infused too rapidly or too slowly. An IV pump is necessary to control the infusion rate and prevent magnesium toxicity or deficiency.
Choice D reason: Regular insulin is a hormone that regulates blood glucose levels and requires careful titration based on frequent blood glucose monitoring. An IV pump is required to deliver insulin at a consistent and adjustable rate to avoid hypoglycemia or hyperglycemia.

A newly hired unlicensed assistive personnel (UAP) expresses fear to the charge nurse about collecting a sputum specimen from a client who is HIV positive. Which action should the charge nurse take first?
Explanation
Choice A reason: Demonstrating the proper use of personal protective equipment is important, but not the first action. The charge nurse should first assess the UAP's level of understanding and address any misconceptions or fears about HIV transmission.
Choice B reason: Offering to assist the UAP with the collection of the specimen may be helpful, but not the first action. The charge nurse should first educate the UAP about HIV transmission and infection control measures, and then evaluate the UAP's competence and confidence in performing the task.
Choice C reason: Providing the UAP with the infection control policy is relevant, but not the first action. The charge nurse should first explain the rationale and principles of infection control to the UAP, and then refer to the policy as a guideline and resource.
Choice D reason: Determining the UAP's knowledge about HIV transmission is the first and most appropriate action for the charge nurse to take, as it will help identify any gaps or misinformation that may cause fear or anxiety in the UAP. The charge nurse should then provide accurate and evidence-based information about HIV transmission, prevention, and treatment, and answer any questions or concerns that the UAP may have.
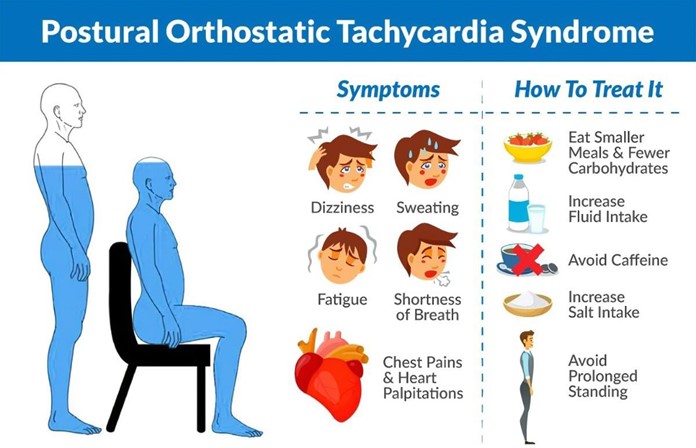
A client with tachycardia and hypotension presents to the emergency department (ED) reporting severe vomiting and diarrhea for three days. Which action is most important for the nurse to implement?
Explanation
Choice A reason: This client has signs of dehydration and fluid volume deficit, which can lead to shock, a life-threatening condition that occurs when the body's organs are not receiving enough blood flow. The nurse should monitor the client's vital signs, urine output, skin color, and level of consciousness, and report any changes to the physician.
Choice B reason: Initiating enteric precaution procedures is important to prevent the spread of infection, as vomiting and diarrhea may be caused by a contagious pathogen. However, this is not the most important action for the nurse to implement, as it does not address the client's immediate risk of shock.
Choice C reason: Reducing light, noise and temperature may help the client feel more comfortable and reduce nausea, but it is not the most important action for the nurse to implement, as it does not address the client's fluid volume deficit and potential shock.
Choice D reason: Encouraging electrolyte supplements may help replenish the electrolytes lost through vomiting and diarrhea, but it is not the most important action for the nurse to implement, as it may not be enough to restore the fluid balance and prevent shock. The client may need intravenous fluids and medications to correct the dehydration and hypotension.
The nurse manager overhears an older female nurse complaining to a co-worker about the time being used to attend an in-service session for bioterrorism preparedness. How should the nurse manager respond?
Explanation
Choice A Reason: Choosing to send another nurse who is more receptive is not a good option, as it may create
resentment and conflict among the staff. The older nurse may feel discriminated against or excluded, and the other nurse may feel burdened or pressured. The nurse manager should try to engage and motivate the older nurse to attend the in-service session, as it is important for her professional development and patient safety.
Choice B Reason: Asking the nurse why she thinks there is no need for an in-service program about these emergencies may sound confrontational or accusatory and may put the nurse on the defensive. The nurse manager should avoid making assumptions or judgments about the nurse's attitude or beliefs, and instead try to understand her perspective and address any barriers or misconceptions.
Choice C Reason: Informing the older nurse that inservice is not optional and her scheduled attendance is mandatory may be true, but it may also sound authoritarian or coercive, and may undermine the nurse's autonomy or dignity. The nurse-manager should avoid using threats or ultimatums, and instead try to explain the rationale and benefits of the inservice session, and solicit the nurse's input or feedback.
Choice D Reason: Encouraging the nurse to share her concerns and discuss ways to prepare for such emergencies is the best option, as it shows respect and empathy for the nurse, and fosters a collaborative and supportive
relationship. The nurse-manager should use active listening and open-ended questions, and provide relevant information and resources to help the nurse overcome her fears or doubts, and enhance her confidence and competence.
After reviewing the morning laboratory findings for four clients, which client should the nurse follow up with first? Reference Range:
International Normalized Ratio [0.8 to 1.1]
Blood Glucose 74 to 106 mg/dL (4.1 to 5.9 mmol/L)]
Potassium [3.5 to 5 mEq/L (3.5 to 5 mmol/L)]
Brain Natriuretic Peptide (BNP) [less than 100 pg/mL (less than 100 ng/L)]
Explanation
Choice A Reason: This client has a very high BNP level, which indicates severe heart failure and fluid overload. The nurse should follow up with this client first, as they may need urgent interventions such as oxygen therapy, diuretics, and vasodilators.
Choice B Reason: This client has an INR within the therapeutic range for warfarin therapy, which is usually between 2 and 3. The nurse should monitor this client for signs of bleeding or clotting, but they do not require immediate follow-up.
Choice C Reason: This client has a mildly elevated glucose level, which may be caused by the corticosteroids that
increase blood sugar. The nurse should check the client's blood glucose regularly and administer insulin as ordered, but they do not require immediate follow-up.
Choice D Reason: This client has a normal potassium level, which is within the reference range of 3.5 to 5 mEq/L. The nurse should ensure that the client is ready for dialysis and avoid foods high in potassium, but they do not require immediate follow-up.
To help prevent by a dissatisfied client, which objective is most important to include in the orientation classes for staff nurses? New nursing staff members will
Explanation
Choice A Reason: Demonstrating how to complete an adverse occurrence or variance report is important, but not the most important objective. This report is a tool for quality improvement and risk management, but it does not prevent litigation by itself. The nurse should also communicate effectively with the client and/or their family, and document the incident and the actions taken.
Choice B Reason: Discussing how to handle complaints from clients and/or their families is the most important objective, as it can help prevent or resolve conflicts, and avoid escalation to legal action. The nurse should listen empathetically, acknowledge the client's feelings and concerns, apologize if appropriate, explain the situation and the plan of care, and involve the supervisor or other resources if needed.
Choice C Reason: Describing how to obtain legal services if needed is relevant, but not the most important objective.
This objective implies that litigation is inevitable or expected, which may create a negative or defensive attitude in the staff nurses. The nurse should focus on preventing litigation by providing safe and quality care and building trust and rapport with the clients and/or their families.
Choice D Reason: Maintaining personal malpractice insurance is advisable, but not the most important objective. This objective may protect the nurse's personal assets in case of a lawsuit, but it does not prevent litigation from occurring. The nurse should follow the standards of practice and the policies and procedures of the organization, and document accurately and thoroughly.
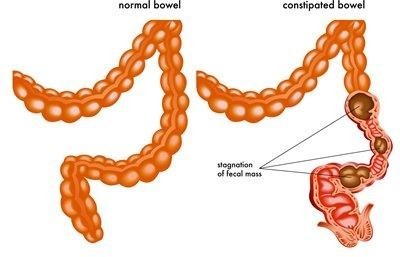
The home health aide caring for a home bound hospice client calls to inform the nurse that the client has reported feeling constipated. Which task should the nurse instruct the home health aide to perform?
Explanation
Choice A Reason: Listening for the presence of bowel sounds is not a task that the home health aide can perform, as it requires a stethoscope and clinical judgment. This task is within the scope of practice of the nurse, who should assess the client's bowel function and abdominal status.
Choice B Reason: Teaching the client about foods high in fiber is not a task that the home health aide can perform, as it requires knowledge and education skills. This task is within the scope of practice of the nurse, who should provide dietary advice and counseling to the client and their family.
Choice C Reason: Administering a prescribed dose of a laxative is not a task that the home health aide can perform, as it requires medication administration skills and authority. This task is within the scope of practice of the nurse, who should check the medication order, verify the dosage and route, and document the administration.
Choice D Reason: Assisting the client to drink warm prune juice is a task that the home health aide can perform, as it requires basic care and assistance skills. This task is appropriate for the home health aide, who should encourage fluid intake and offer natural remedies for constipation, such as prune juice, which has laxative effects.
A group of nurse managers is asked to engage in a needs assessment for a piece of equipment that will be expensed to the organization's budget. Which question is most important to consider when analyzing the cost-benefit for this piece of equipment?
Explanation
Choice A Reason: The ability to update the equipment each year may be desirable, but not the most important question to consider. Updating the equipment may incur additional costs and may not be necessary or feasible depending on the type and function of the equipment.
Choice B Reason: The number of departments that can use the equipment is the most important question to
consider, as it reflects the potential impact and benefit of the equipment for the organization. The more departments that can use the equipment, the more efficient and cost-effective it will be.
Choice C Reason: The cost of equipment is an important question to consider, but not the most important one. The cost of equipment should be compared with the expected benefits and outcomes of using the equipment, not just in terms of monetary value, but also in terms of quality of care and patient satisfaction.
Choice D Reason: The need for annual repair is an important question to consider, but not the most important one. The need for annual repair may indicate the reliability and durability of the equipment, but it may also depend on the frequency and intensity of use, and the availability and accessibility of maintenance services.
Several nurses are elected by their peers to serve on a negotiating committee to recommend new healthcare benefits. After the new benefits plan is developed and approved, which action is most important for the nurses working on this committee to implement?
Explanation
Choice A Reason: Announcing the new plan at a special employee wellness event may be a good way to promote the plan and celebrate the achievement, but it is not the most important action. The nurses working on the committee should first communicate the plan to their colleagues and address any questions or concerns they may have.
Choice B Reason: Determining staff opinion of current healthcare insurance costs may be useful for evaluating the need and feasibility of the new plan, but it is not the most important action. The nurses working on the committee should have done this before developing and approving the new plan, not after.
Choice C Reason: Surveying the nurses to see who wants to keep the old benefits plan may be helpful for assessing the satisfaction and acceptance of the new plan, but it is not the most important action. The nurses working on the committee should have considered the preferences and needs of their colleagues during the development and approval of the new plan, not after.
Choice D Reason: Being available to all shifts to discuss the changes in health benefits is the most important action for the nurses working on the committee to implement, as it shows respect and transparency for their colleagues, and fosters a collaborative and supportive work environment. The nurses working on the committee should explain the rationale and benefits of the new plan, and provide feedback and guidance to their colleagues.
In evaluating a staff nurse who demonstrates inconsistent performance, which intervention should the nurse- manager employ?
Explanation
Choice A Reason: This intervention is the most appropriate and effective for the nurse-manager to employ, as it provides clear and objective feedback to the staff nurse based on professional criteria, and encourages a positive and constructive approach to enhance the nurse's performance and development.
Choice B Reason: This intervention is not advisable, as it may create a false impression of the staff nurse's performance and fail to address the underlying issues or problems. Documenting the nurse's negative behaviors is important for accountability and improvement purposes, and avoiding it may expose the nurse manager to legal or ethical risks.
Choice C Reason: This intervention is not optimal, as it may demoralize or discourage the staff nurse and create a negative or hostile work environment. Focusing only on the areas of weakness may overlook the strengths and potential of the staff nurse, and may not foster a supportive and collaborative relationship between the nurse- manager and the staff nurse.
Choice D Reason: This intervention is not relevant, as it may divert the attention from the staff nurse's performance and shift the blame to external factors. Discussing how the inconsistency in the staff nurse's performance disrupts the routine of all of the staff members on the unit may not help the staff nurse identify and address their own areas of improvement, and may cause resentment or conflict among the team.
A fire is reported in the kitchen on the first floor of a three-floor community hospital, and the operator notifies the charge nurse on the third floor to start evacuation procedures. Which intervention should the charge nurse
implement?
Explanation
Choice A Reason: Instructing UAPs to transfer all non-ambulatory clients via wheelchairs is not a good intervention, as it may expose the clients and the UAPs to smoke and fire, and cause panic and congestion in the hallways. The charge nurse should follow the RACE protocol (Rescue, Alarm, Contain, Extinguish), which means rescuing only those clients who are in immediate danger, and containing the fire by closing doors and windows.
Choice B Reason: Instructing the nursing staff to evacuate ambulatory clients to the nearest fire exits is not a good intervention, as it may also expose the clients and the staff to smoke and fire, and interfere with the fire
department's efforts. The charge nurse should follow the RACE protocol, which means evacuating only as a last resort, and only after receiving instructions from the fire department.
Choice C Reason: Shutting all doors to client rooms and telling everyone to stay in their rooms until the fire
department arrives is the best intervention, as it follows the RACE protocol, which means containing the fire by closing doors and windows, and extinguishing it if possible with a fire extinguisher. This intervention also helps protect the clients and staff from smoke inhalation and fire spread, and allows the fire department to access and control the fire.
Choice D Reason: Announcing in a calm voice that all visitors should proceed immediately to the first floor via the service elevators is not a good intervention, as it may endanger the visitors and cause more damage. The charge nurse should follow the RACE protocol, which means alarming others by activating the fire alarm system and calling 911. The charge nurse should also instruct visitors not to use elevators during a fire, as they may malfunction or trap them inside.
The nurse manager observes that the staff nurse has used wrist restraints to help secure an elderly female in her
wheelchair. The client is pleading for the nurse to release her arms. The nurse explains to the nurse manager that the client needs to be restrained in the wheelchair so that the nurse can change her bed linens. Which is the priority action by the nurse manager?
Explanation
Choice A Reason: Contacting the healthcare provider is not the priority action because restraints should only be used as a last resort and not for staff convenience. The nurse manager should first ensure that the client's safety and dignity are respected.
Choice B Reason: This is the correct answer because restraints are not indicated for this situation and violate the client's rights. The nurse manager should educate the staff nurse about the ethical and legal implications of using restraints without proper justification and documentation.
Choice C Reason: Closing the door to the room is not a priority action because it does not address the issue of restraints. It also may isolate the client and increase her anxiety and distress.
Choice D Reason: Determining if the client has a PRN prescription for an antianxiety agent is not a priority action because it does not address the issue of restraints. It also may not be appropriate to medicate the client without assessing her condition and obtaining her consent.

A client with influenza is admitted to the medical unit. The nurse observes an unlicensed assistive personnel (UAP) preparing to enter the client's room to take vital signs and assist with personal care. The UAP has applied gloves and a gown. Which action should the nurse take?
Explanation
Choice A Reason: Reviewing the need for the UAP to wear a face mask is not enough because influenza is transmitted by respiratory droplets that can be inhaled by anyone within 6 feet of the infected person. A face mask does not provide adequate protection from inhalation of droplets.
Choice B Reason: This is the correct answer because a fitted respirator mask (such as N95) can filter out at least 95% of airborne particles and prevent exposure to the influenza virus. The UAP should wear a respirator mask along with gloves and a gown when providing care for a client with influenza.
Choice C Reason: Assigning the UAP to provide care for another client and assuming full care of the client is not necessary or feasible because it would increase the workload of the nurse and reduce the quality of care for both clients. The UAP can still assist with care for clients with influenza as long as they follow proper infection control measures.
Choice D Reason: Instructing the UAP to notify the nurse of any changes in the client's respiratory status is important but not a priority action because it does not address the issue of preventing transmission of influenza. The nurse should first ensure that the UAP wears appropriate personal protective equipment before entering the client's room.
The unlicensed assistive personnel (UAP) reports to the nurse that a male client with fluid volume overload will not allow the UAP to obtain his daily weight. Which action should the nurse implement?
Explanation
Choice A Reason: Asking the client why he does not want to be weighed is not a priority action because it does not address the need to obtain his daily weight. The nurse should first try to find a way to weigh the client without causing him discomfort or distress.
Choice B Reason: This is the correct answer because weighing the client using a bed scale can avoid the need for
transferring him from the bed to a standing scale, which may be difficult or painful for him. The bed scale can provide an accurate measurement of his weight and help monitor his fluid status.
Choice C Reason: Directing the UAP to delay weighing the client until later is not an appropriate action because it may result in missing or inaccurate data. The nurse should ensure that the client is weighed at the same time every day, preferably in the morning, before any fluid intake or output.
Choice D Reason: Documenting that the client refused daily weights is not an adequate action because it does not reflect the nurse's responsibility to provide quality care for the client. The nurse should try to resolve the issue of weighing the client and documenting the outcome and any interventions.

A staff nurse has been tardy for morning shift assignments for the past three days and provides no explanation for arriving late. Which approach is best for the nurse manager to use when addressing this staff member's tardiness?
Explanation
Choice A Reason: Cautioning the nurse that one more tardiness will result in probational employment is not the best approach because it is too punitive and does not address the underlying cause of the tardiness. The nurse manager should first try to understand why the nurse is late and offer support or guidance if needed.
Choice B Reason: Offering to switch the nurse's shift assignments to afternoons or evenings is not the best approach because it may not solve the problem of tardiness and may create resentment among other staff members who have to adjust their schedules. The nurse manager should respect the nurse's preferences and availability but also hold the nurse accountable for fulfilling their responsibilities.
Choice C Reason: This is the best approach because it communicates clearly and respectfully what is expected of the nurse and why it is important for them to be punctual. The nurse manager should also provide feedback and recognition when the nurse improves their attendance.
Choice D reason: Having the nurse sign a copy of the hospital employee attendance policy is not the best approach because it may imply that the nurse is unaware or indifferent to the policy. The nurse manager should assume that the nurse knows and agrees with the policy, but may need some assistance or motivation to follow it.
It is most important to assign which client to a registered nurse rather than a practical nurse (PN)?
Explanation
Choice A Reason: This client may need another dose of hydromorphone if the pain is not relieved by the previous one. A PN can administer this medication under the supervision of a RN and monitor the client's response.
Choice B Reason: This client's vital signs are within normal limits and indicate that the morphine is effective and not causing respiratory depression. A PN can assess and document the client's vital signs and pain level.
Choice C Reason: This is the correct answer because this client has acute and severe pain that may require immediate intervention and reassessment. An RN can evaluate the cause and severity of the pain, administer additional analgesics as prescribed, and implement nonpharmacological measures to relieve the pain.
Choice D Reason: This client has chronic and stable pain that is managed by a fentanyl patch. A PN can replace the patch according to the schedule and instructions provided by the RN.

Which staff assignment, made by the primary nurse, requires the most immediate follow-up action by the charge nurse on a medical unit?
Explanation
Choice A Reason: This assignment does not require immediate follow-up action by the charge nurse because a practical nurse can transport a stable postoperative client to another unit and report any changes or concerns to the primary nurse.
Choice B Reason: This assignment does not require immediate follow-up action by the charge nurse because a practical nurse can monitor the blood pressure of a client with hypertension and administer antihypertensive medications as prescribed and delegated by the primary nurse.
Choice C Reason: This assignment does not require immediate follow-up action by the charge nurse because a graduate nurse can obtain a unit of packed red blood cells from the blood bank and verify the compatibility and identification with another registered nurse before transfusing it to the client.
Choice D Reason: This is the correct answer because checking a client for fecal impaction is beyond the scope of practice of unlicensed assistive personnel. It involves inserting a finger into the rectum and assessing for hard stool, which can cause injury or infection to the client. The charge nurse should intervene and assign this task to a registered nurse or a practical nurse.
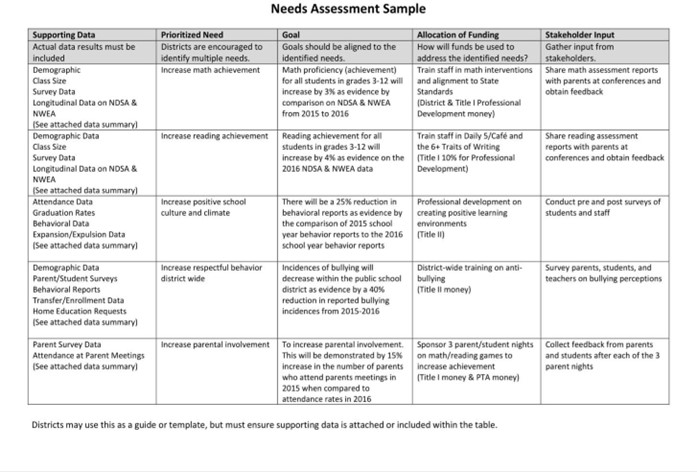
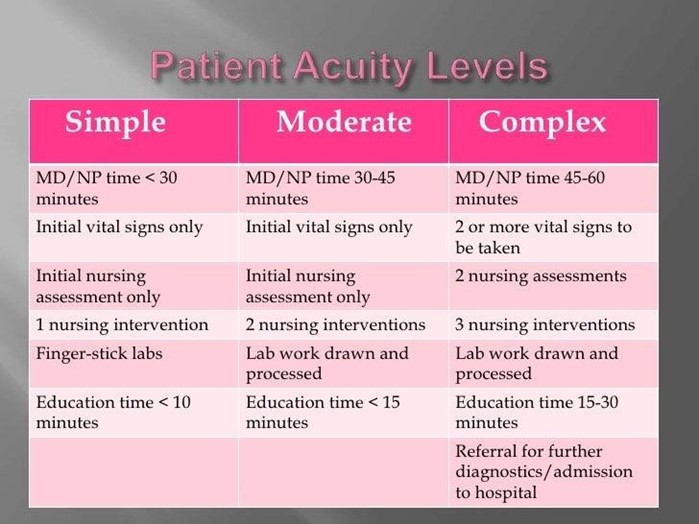
The charge nurse needs to determine if an additional nurse should be called to help staff the unit for the next shift. Which information is most important for the charge nurse to consider when making this decision?
Explanation
Choice A Reason: This is the correct answer because the acuity level of the clients reflects their complexity and intensity of care needs. The higher the acuity level, the more time and resources are required to provide safe and quality care. The charge nurse should consider the acuity level of the clients when determining the appropriate nurse-to-client ratio and staffing needs.
Choice B Reason: The physicians' plans to perform procedures on the unit is not the most important information for the charge nurse to consider because it does not directly affect the nursing workload or staffing requirements. The charge nurse should coordinate with the physicians and other departments to ensure that the procedures are scheduled and performed safely and efficiently.
Choice C Reason: The number of clients leaving the unit for diagnostic tests is not the most important information for the charge nurse to consider because it does not indicate the level of care that the clients need or receive. The charge nurse should ensure that the clients are prepared and accompanied for their tests and that their care is continued and monitored on their return.
Choice D Reason: The skill level of the personnel staffing the unit is not the most important information for the charge nurse to consider because it does not reflect the actual demand or supply of nursing care. The charge nurse should assign and delegate tasks according to the personnel's skill level and scope of practice but also consider other factors such as client acuity, availability, and preference.
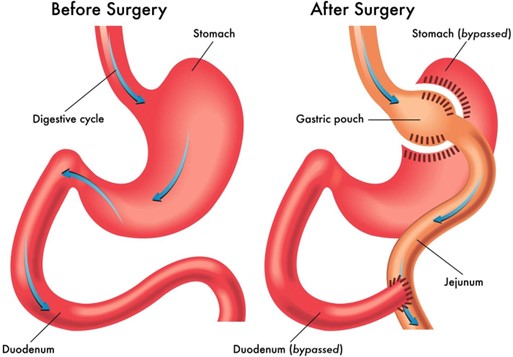
An adult woman who had gastric bypass surgery two weeks ago is admitted because she is exhibiting signs of anastomosis leakage. Her vital signs are: temperature 100°F (37.8°C), blood pressure 98/50 mm Hg, heart rate 135 beats/minute, and respiratory rate 24 breaths/minute. Which intervention is most important for the nurse to include in this client's plan of care?
Explanation
Choice A Reason: This is the correct answer because the client's vital signs indicate that she is hypovolemic and dehydrated due to the leakage of gastric contents from the anastomosis site. The nurse should replace fluids intravenously to prevent shock and electrolyte imbalance.
Choice B Reason: Recording the amount of daily wound drainage is important but not the most important intervention for this client because it does not address the immediate problem of fluid loss and hypovolemia. The nurse should monitor the wound drainage for signs of infection and report any changes to the physician.
Choice C Reason: Assessing skin condition and turgor for breakdown is important but not the most important intervention for this client because it does not address the immediate problem of fluid loss and hypovolemia. The nurse should assess the skin for signs of dehydration and pressure ulcers and provide appropriate skin care.
Choice D Reason: Turning every 2 hours around the clock from side-to-side is important but not the most important intervention for this client because it does not address the immediate problem of fluid loss and hypovolemia. The nurse should turn the client to prevent complications such as pneumonia and atelectasis but also consider the client's comfort and pain level.
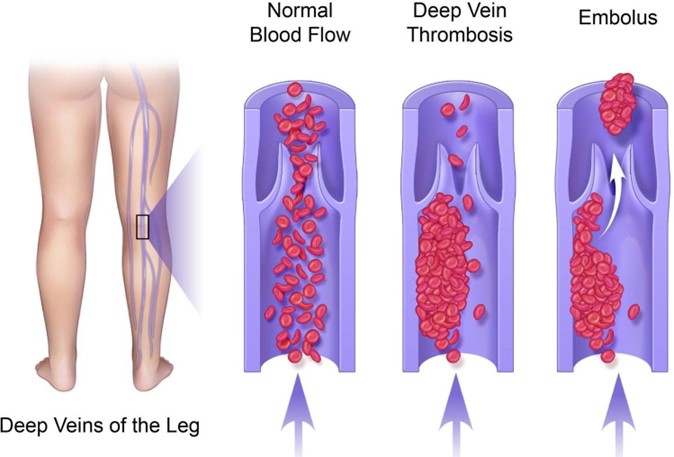
The practical nurse reports that a client with a deep vein thrombosis (DVT) was mistakenly given heparin in addition to the prescribed warfarin. Which priority action should the nurse take?
Explanation
Choice A Reason: This is the correct answer because the nurse should immediately inform the healthcare provider of the medication error and the client's condition. The healthcare provider may order antidotes, such as protamine sulfate for heparin and vitamin K for warfarin, to reverse the anticoagulant effects and prevent bleeding complications.
Choice B Reason: Monitoring for signs of bleeding is important but not the priority action for the nurse because it does not address the cause of the problem or prevent further harm. The nurse should monitor the client's vital signs, hemoglobin, hematocrit, and urine output, as well as check for any signs of bleeding, such as bruising, petechiae,
hematuria, hematemesis, melena, or epistaxis.
Choice C Reason: Completing an adverse occurrence report is important but not the priority action for the nurse because it does not provide immediate intervention or treatment for the client. The nurse should complete an
adverse occurrence report after notifying the healthcare provider and implementing appropriate actions. The report should include the details of the error, such as the time, dose, route, and name of the medications involved, as well as the client's response and outcome.
Choice D Reason: Obtaining blood for coagulation studies is important but not the priority action for the nurse because it does not provide immediate intervention or treatment for the client. The nurse should obtain blood
samples for coagulation studies, such as prothrombin time (PT), international normalized ratio (INR), and activated partial thromboplastin time (aPTT), after notifying the healthcare provider and following their orders. The results of these tests can help determine the extent of anticoagulation and guide further therapy.
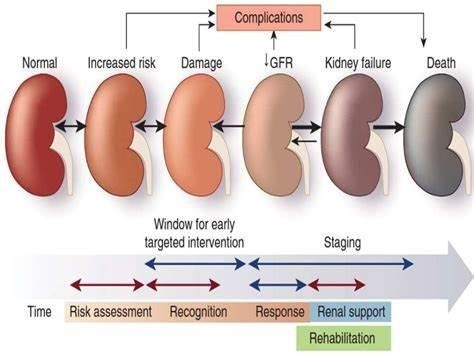
Which client requires the most immediate intervention by the nurse?
Explanation
A) This client has a mild fever, which may indicate an infection or inflammation. This is a potential complication of enteral feedings, but it is not the most urgent situation. The nurse should monitor the client's vital signs, assess the feeding tube site, and notify the provider if the fever persists or worsens.
B) This client has signs of uremic encephalopathy, which is a life-threatening condition caused by the accumulation of toxins in the brain due to impaired renal function. The nurse should intervene immediately to prevent further
neurological damage and possible coma or death. The nurse should assess the client's level of consciousness, check the blood pressure and urine output, and prepare to administer dialysis or other treatments as ordered by the provider.
C) This client has heat stroke, which is a serious condition that can lead to dehydration, electrolyte imbalance, and organ damage. However, the client is receiving a normal saline IV fluid bolus, which is an appropriate intervention to restore fluid volume and correct sodium levels. The nurse should continue to monitor the client's vital signs, skin
temperature, and urine output, and watch for signs of fluid overload or cerebral edema.
D) This client has hyperemesis gravidarum, which is a severe form of nausea and vomiting during pregnancy that can lead to dehydration, malnutrition, and electrolyte imbalance. However, the client is receiving an infusion of Ringer's Lactate, which is an isotonic solution that can replenish fluid and electrolyte losses. The nurse should continue to monitor the client's vital signs, weight, and intake and output, and administer antiemetics or other medications as ordered by the provider.
An experienced, female practical nurse (PN) is hired to work on the surgical unit of a tertiary hospital. The first day she is working on the unit, the PN tells the charge nurse that she has excellent wound care skills. It is a busy day and a postoperative client needs to have a sterile dressing change. Which action is best for the charge nurse to take?
Explanation
A) This action is not the best because it does not directly evaluate the PN's wound care skills in practice. A skill checklist may not reflect the current or actual abilities of the PN, especially if it is outdated or based on self-
reporting. The charge nurse should observe the PN's performance in person to ensure that she follows the proper procedures and protocols for sterile wound care.
B) This action is the best because it allows the charge nurse to verify the PN's wound care skills and provide feedback or guidance if needed. The charge nurse has a responsibility to ensure that the PN delivers safe and effective care to the clients on the unit. By watching the PN perform sterile wound care, the charge nurse can assess her competence, confidence, and compliance with standards of practice.
C) This action is not the best because it is disrespectful and discouraging to the PN. The charge nurse should not dismiss or undermine the PN's past experience, which may have contributed to her wound care skills. The charge nurse should acknowledge and appreciate the PN's expertise, but also verify her skill level through direct
observation.
D) This action is not the best because it exposes the client to potential harm and liability. The charge nurse should not delegate a task that requires assessment and evaluation to a PN without first confirming her skill level and competency. The charge nurse should also not ask the PN to perform a task while she is busy with other duties, as this may compromise the quality and safety of care.

A client with life-threatening injuries from a gunshot wound to the abdomen is mechanically ventilated and sedated. The client has a large family present who are asking multiple and repetitive questions. Which intervention should the nurse implement first?
Explanation
A) This intervention is not the best because it may take too much time and energy from the nurse, who needs to focus on the client's critical condition. The nurse may also have to repeat the same information multiple times, which can be frustrating and confusing for both the nurse and the family.
B) This intervention is not the best because it may not be feasible or appropriate at this time. The healthcare provider may be busy with other clients or procedures, and may not be able to speak with the family right away. The healthcare provider may also need to obtain the client's consent or permission before disclosing any information to the family, which may not be possible if the client is sedated.
C) This intervention is the best because it can help reduce the number and frequency of questions, and facilitate clear and consistent communication between the nurse and the family. The nurse can ask the family to choose one person who will act as their representative and spokesperson, and who will relay any information or updates to the rest of the family. This can also help respect the client's privacy and confidentiality, and prevent any conflicting or contradictory messages.
D) This intervention is not the best because it may not address the family's informational needs or preferences. The chaplain on call may provide spiritual or emotional support to the family, but may not be able to answer any medical or technical questions. The family may also have different religious or cultural beliefs that may not align with the chaplain's role or perspective.
Sign Up or Login to view all the 49 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

