HESI Pharmacology
Total Questions : 46
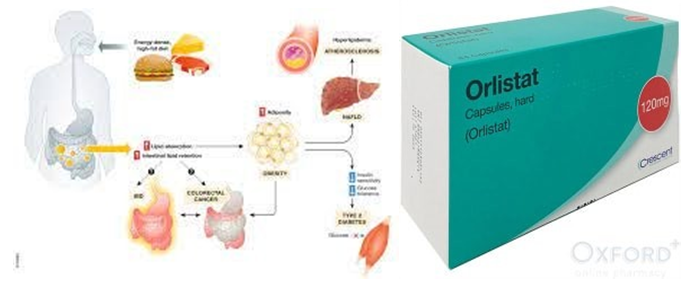
Showing 25 questions, Sign in for moreAfter taking orlistat for one week, a female client tells the home health nurse that she is experiencing increasingly frequent faty stools and flatus. Which action should the nurse take?
Explanation
Orlistat works by inhibiting the absorption of dietary fat in the intestines. The side effects of faty stools and flatus can be managed by reducing the intake of dietary fat. The nurse should ask the client to describe her dietary intake history for the last several days to determine if she has been consuming a diet high in fat.
Based on this information, the nurse can provide appropriate dietary advice to help manage these side effects.
The nurse is preparing a discharge teaching plan for a client who is taking ciprofloxacin hydrochloride tablets which were prescribed because of a suspected anthrax exposure. Which instructions should be included in the teaching plan?
(Select all that apply.)
Explanation
Ciprofloxacin hydrochloride is an antibiotic used to treat bacterial infections. It has been associated with an increased risk of tendonitis and tendon rupture. Therefore, the client should be instructed to report any tendon pain or swelling to the healthcare provider immediately [a]. Ciprofloxacin can also increase the skin’s sensitivity to sunlight, so the client should be advised to limit exposure to sunlight and avoid tanning beds [d]. Increasing fluid intake while taking the medication can help prevent the formation of crystals in the urine [e].
Option b is incorrect because NSAIDs can interact with ciprofloxacin and increase the risk of central nervous system stimulation and seizures.
Option c is incorrect because ciprofloxacin tablets should not be crushed or chewed as this can affect the medication’s effectiveness.

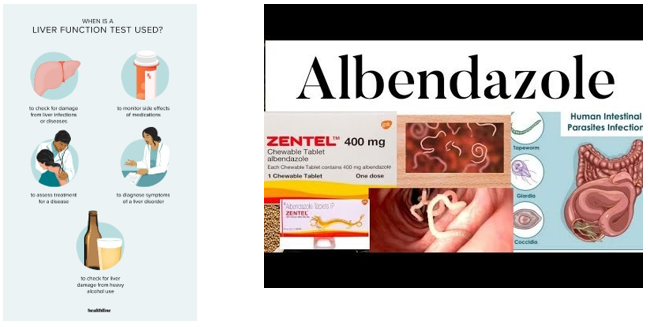
A client who is taking albendazole reports experiencing fatigue, nausea, and dark urine. The nurse observes a yellowing of the client’s skin and sclera. Which lab results should the nurse review?
Explanation
The client's symptoms suggest liver dysfunction, which is a known adverse effect of albendazole. Albendazole is primarily metabolized in the liver, and its use can cause liver damage in some cases. Therefore, it is essential to review liver function test results to assess the severity of liver damage and to determine if the medication should be discontinued or the dosage should be adjusted.
The renal function panel (a) measures the levels of various substances, such as creatinine and blood urea nitrogen, in the blood to assess kidney function.
The thyroid function test (b) evaluates the levels of thyroid hormones in the blood to diagnose thyroid disorders.
The basic metabolic panel (c) includes several tests that assess the levels of electrolytes, glucose, and other substances in the blood to evaluate metabolic function. However, these lab tests are not directly related to the symptoms and adverse effects associated with albendazole use
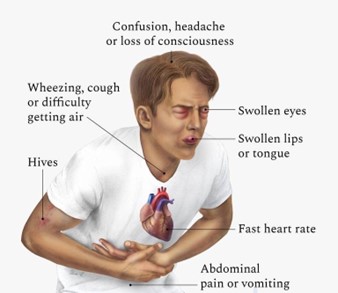
Which assessment data indicated to the nurse that a client is having an anaphylactic reaction to a medication?
Explanation
Anaphylaxis is a severe and potentially life-threatening allergic reaction that occurs rapidly after exposure to an allergen. The symptoms of anaphylaxis can vary but usually involve multiple organ systems, including the skin, respiratory, cardiovascular, and gastrointestinal systems.
Wheezing and dyspnea are two common symptoms of anaphylaxis that indicate the respiratory system's involvement.
Urticaria and pruritis are skin manifestations that can also be present in anaphylaxis, but they are not specific to this condition.
Insomnia and irritability are not typical symptoms of anaphylaxis.
Tinnitus and diplopia are also not common symptoms of anaphylaxis.
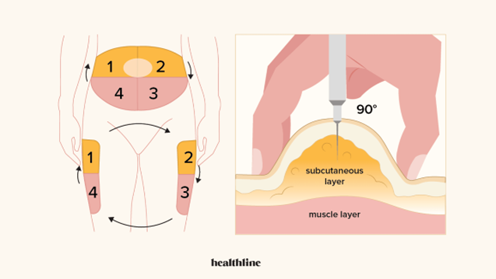
The nurse is planning to discharge teaching for a client with diabetes mellitus who has a new prescription for insulin glargine. Which action should the nurse include in the discharge teaching?
Explanation
Insulin glargine is a long-acting insulin that is given once daily at the same time every day via subcutaneous injection. Therefore, it is essential to teach the client self-injection skills for daily subcutaneous administration to ensure proper administration of insulin.
Option b is incorrect because insulin glargine is typically given at the same dose every day, not based on before meal blood sugar readings.
Option c is incorrect because insulin glargine is not used for the treatment of severe hypoglycemia, and it should not be administered by someone who is not trained to do so.
Option d is incorrect because ketoacidosis is a serious complication of diabetes mellitus that requires urgent medical atention, and increasing medication dosage is not appropriate for this condition.
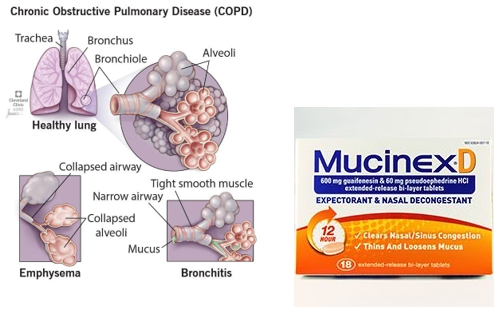
The nurse is preparing a client with Chronic Obstructive Pulmonary Disease (COPD) and a chronic productive cough for discharged home.
Which prescribed medication should the nurse review with the client to manage this symptom?
Explanation
Guaifenesin is an expectorant that helps to loosen and thin mucus in the airways, making it easier to cough up. It is commonly used to manage symptoms of a chronic productive cough in conditions such as COPD.
Salmeterol and Tiotropium are both bronchodilators that help to open up the airways and improve breathing in COPD, but they are not specifically indicated for managing a chronic productive cough.
Prednisone is a corticosteroid that can help reduce inflammation in the airways and improve breathing in COPD exacerbations, but it is not typically used for managing a chronic productive cough.
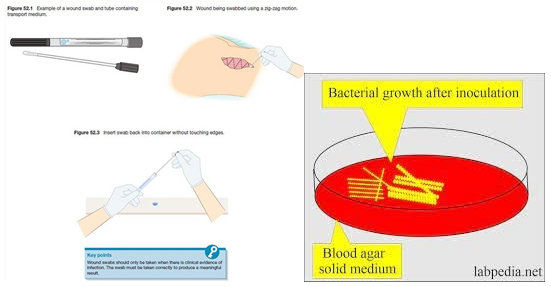
On admission, the healthcare provider describes a broad spectrum of antibiotic, ticarcillin for a client with a gram-negative infection. Before administering the first dose, it is most important for the nurse to implement which prescription?
Explanation
Before administering the first dose of any antibiotic, it is essential to obtain a culture and sensitivity test to identify the causative organism and determine the most effective antibiotic to use. Administering a broad- spectrum antibiotic before obtaining a culture and sensitivity test may lead to the development of antibiotic-resistant strains of bacteria, making it more difficult to treat the infection in the future.
Options a, c, and d are not as important as obtaining a culture and sensitivity test. Monitoring for signs of sodium and fluid retention, irrigation and topical antibiotic application to the wound area, and completing blood count and serum electrolytes are important, but obtaining a culture and sensitivity test is the priority.
The nurse is planning care for a patient with major depression who is receiving a new prescription for duloxetine.
Which information is most important for the nurse to obtain?
Explanation
Duloxetine is an antidepressant medication that belongs to a class of drugs known as serotonin- norepinephrine reuptake inhibitors (SNRIs). When combined with other antidepressants, including selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants (TCAs), and monoamine oxidase inhibitors (MAOIs), there is an increased risk of developing serotonin syndrome, a potentially life-threatening condition that can cause symptoms such as confusion, agitation, rapid heart rate, high blood pressure, and hyperthermia.
Therefore, it is essential for the nurse to determine whether the patient has recently used any other antidepressant medications before initiating duloxetine therapy. If the patient has taken other antidepressants, the nurse should consult with the healthcare provider to determine the appropriate course of action, which may include discontinuing the previous antidepressant and monitoring the patient closely for signs of serotonin syndrome.
While all of the options listed may be relevant to the patient's care, obtaining information about recent use of other antidepressants is the most crucial consideration for patient safety and medication management.

An older adult client with restless legs syndrome begins taking melatonin at bedtime. When evaluating the effectiveness of the herb which client assessment should the nurse complete?
Explanation
Restless legs syndrome is a condition that causes an uncomfortable sensation in the legs and an uncontrollable urge to move them. Melatonin is a natural hormone that helps regulate the sleep-wake cycle and can be used as a sleep aid. Therefore, when evaluating the effectiveness of melatonin in an older adult client with restless legs syndrome, the nurse should assess the client's sleep patterns to determine if the herb is improving their ability to fall and stay asleep.
Assessing anxiety level (a) may be useful in other contexts, but it is not directly relevant to evaluating the effectiveness of melatonin for restless legs syndrome. Observing for peripheral edema (b) and palpating pedal pulse volume (d) are important assessments in clients with peripheral vascular disease or other circulatory disorders, but they are not directly related to restless legs syndrome or the use of melatonin.

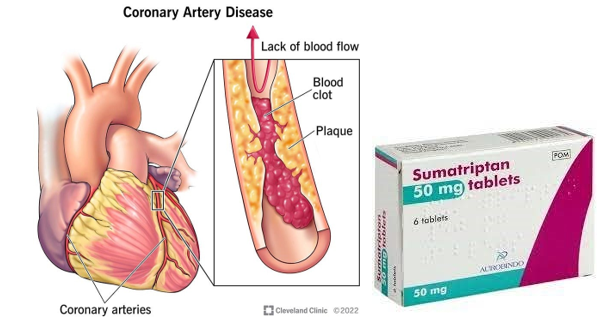
Before administering initial dose of sumatriptan succinate to a client with a migraine headache, it is most to determine if the client’s history includes which problem?
Explanation
Sumatriptan succinate is a medication used to treat migraine headaches by narrowing blood vessels in the brain. It is important to determine if the client has a history of coronary artery disease before administering the initial dose because the medication can also cause narrowing of the coronary arteries and potentially lead to a heart attack or other cardiac events.
Type 2 diabetes mellitus (a), seasonal allergic rhinitis (c), and irritable bowel syndrome (d) are not directly related to the use of sumatriptan succinate. However, it is still important to consider the client's medical history and overall health status when prescribing or administering any medication.
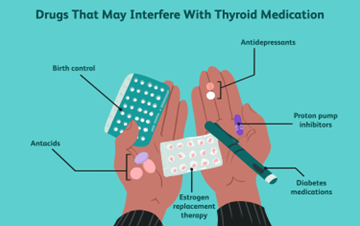
A client receives a new prescription for levothyroxine. Which statement made by client indicates to the nurse that the education was effective?
Explanation
Levothyroxine is a thyroid hormone replacement medication used to treat hypothyroidism. To ensure proper absorption and effectiveness of the medication, it should be taken on an empty stomach, preferably in the morning, and at least 30 minutes before eating. Therefore, when the client indicates that they understand the need to take the medication on an empty stomach, it indicates that the education was effective.
Option b, "Avoid the use of iron supplements," is also important education for clients taking levothyroxine because iron supplements can interfere with the absorption of the medication. However, it is not the best indicator of effective education because the question asks for the statement that indicates education was effective, and option a is a more direct and specific response to the medication.
Option c, "Administer levothyroxine at bedtime," is not accurate information because the medication should be taken in the morning on an empty stomach.
Option d, "Consume foods that are high in iodine," is not recommended for clients taking levothyroxine because high amounts of iodine can interfere with thyroid function. Therefore, this statement indicates a need for further education.
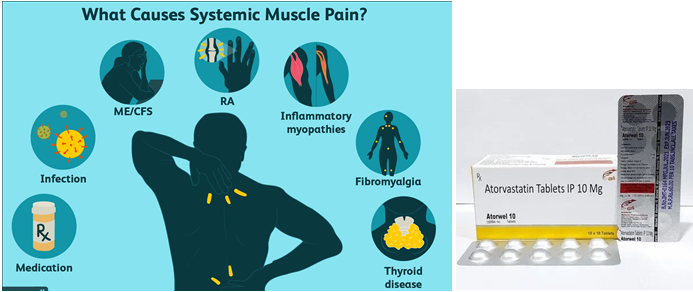
A client taking atorvastatin becomes an increased serum creatine phosphokinase (CK) level.
The nurse should assess the client for the onset of which problem?
Explanation
Atorvastatin is a medication used to lower cholesterol levels in the blood. One of its side effects is muscle damage, which can result in an increase in serum creatine phosphokinase (CK) levels. Creatine phosphokinase is an enzyme found in muscles, and when muscles are damaged, CK is released into the bloodstream. Therefore, an increased serum CK level indicates muscle damage, and the nurse should assess the client for muscle tenderness or weakness, which are symptoms of this side effect. Nausea and vomiting, excessive bruising, and peripheral edema are not typically associated with atorvastatin use.
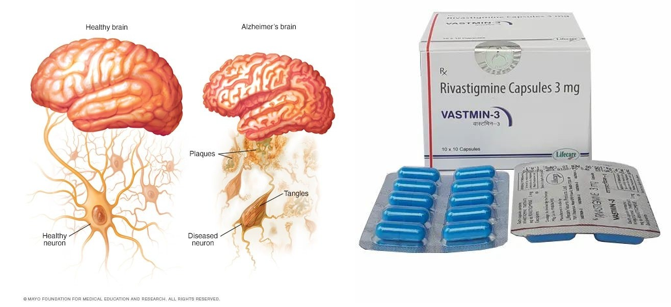
Rivastigmine, a cholinesterase inhibitor, is prescribed for a female client with early-stage Alzheimer’s disease. The client’s daughter tells the nurse that she plans to start administering the drug when her mothers’ symptoms are no longer manageable, in hopes that her mother will not have to go to a nursing home. How should the nurse respond?
Explanation
The nurse should explain to the client's daughter that Rivastigmine is most effective when used early during Alzheimer's disease. Delaying the use of the medication until the symptoms are no longer manageable may result in the drug being less effective.
The nurse should emphasize the importance of following the healthcare provider's instructions for administering the medication to maximize its therapeutic effect. It is important to educate the client's daughter about the progressive nature of Alzheimer's disease and the need for ongoing monitoring and care.
The home health nurse observes a client self-administering an epinephrine injection using an auto-injector pen.
Which client action requires intervention by the nurse?
Explanation
The correct answer is Choice B: Inserts the injection pen through clothing.
Choice B rationale:
- Ineffective delivery of medication:Inserting the injection pen through clothing can impede the needle from reaching the muscle and delivering the medication effectively.Clothing can act as a barrier,absorbing or deflecting the medication,potentially leading to a suboptimal dose or delayed absorption.
- Risk of infection:Clothing may harbor bacteria or other contaminants that could be introduced into the injection site,increasing the risk of infection.This is particularly concerning in a home setting where clothing may not be as sterile as in a healthcare facility.
- Difficulty assessing injection site:If the injection is given through clothing,it can be challenging to accurately assess the injection site for any signs of redness,swelling,or other potential complications.This could delay identification and treatment of any adverse reactions.
Choice A rationale:
- Appropriate injection site:The fleshy outer thigh is a common and recommended injection site for epinephrine auto-injectors.It provides a large muscle mass with adequate blood flow for rapid absorption of the medication.
Choice C rationale:
- Ensures full dose delivery:Holding the pen in place for several seconds after injection is essential to ensure that the full dose of medication is delivered.This allows time for the medication to be fully expelled from the pen and absorbed into the muscle tissue.
Choice D rationale:
- Not a reusable device:Epinephrine auto-injector pens are designed for single use only and should not be cleaned for re-use.Cleaning a used pen can compromise its sterility and functionality,potentially leading to infection or medication errors.
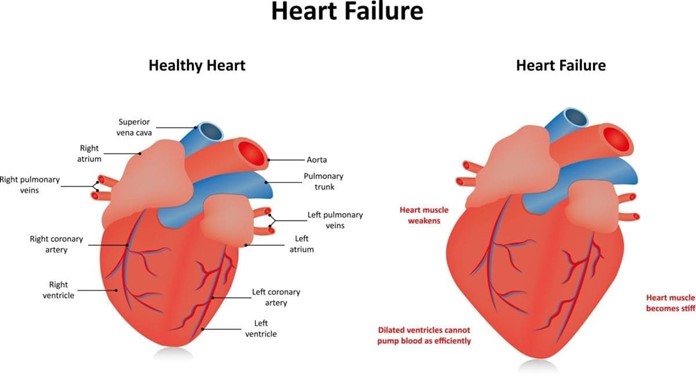
A client with heart failure (HF) develops hyperaldosteronism and spironolactone is prescribed. Which instruction should the nurse include in this patient’s plan of care?
Explanation
Spironolactone is a potassium-sparing diuretic that works by blocking the actions of aldosterone, a hormone that can lead to potassium loss in the urine. However, in some cases, spironolactone can cause hyperkalemia (high levels of potassium in the blood), which can be dangerous for patients with heart failure. Therefore, it is important to instruct the patient to limit their intake of high-potassium foods such as bananas, oranges, tomatoes, spinach, and salt substitutes containing potassium.
Option a (Replace salt with a salt substitute) is incorrect because salt substitutes often contain potassium, which can further increase the risk of hyperkalemia.
Option c (Cover your skin before going outside) is unrelated to the use of spironolactone and hyperkalemia.
Option d (Monitor skin for excessive bruising) is not directly related to the use of spironolactone and hyperkalemia, although it is a potential side effect of other medications used to treat heart failure.
A client who received a renal transplant three months ago is readmitted to the acute care unit with signs of graft rejection. While taking the client’s history, the nurse determines that the client has been self-administering St. John's Wort, an herbal preparation on the advice of a friend.
Which information is most significant about this finding?
Explanation
Cyclosporine is an immunosuppressive medication commonly used to prevent graft rejection after organ transplantation. St. John's Wort is known to induce cytochrome P450 enzymes, which can increase the metabolism and decrease the effectiveness of many medications, including cyclosporine. This interaction can lead to decreased plasma concentrations of cyclosporine, which can increase the risk of graft rejection. Therefore, it is important to advise the client to discontinue the use of St. John's Wort and inform their healthcare provider about any herbal or supplement use to prevent potential interactions with prescribed medications. Options a, c, and d are not directly related to the client's current condition and are not as significant as option b.

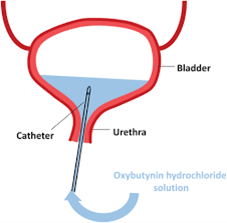
A female client starts a new prescription, oxybutynin, for symptoms of an overactive bladder. The client tells the nurse that she is training to run in a marathon. Which instruction should the nurse emphasize?
Explanation
Oxybutynin is a medicine used to treat symptoms of an overactive bladder. One of the side effects of oxybutynin is that it can cause dry mouth, constipation, and dry skin21. These side effects can increase the risk of dehydration. Additionally, oxybutynin can cause flushing and heat stroke. Therefore, it is important for the client to take measures to avoid dehydration and over-heating while training for a marathon.
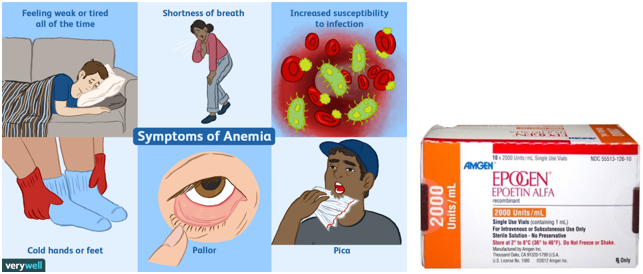
A client with anemia secondary to chronic kidney disease started a prescription for epoetin alfa two months ago. Which client finding best indicates that the medication is effective?
Explanation
Epoetin alfa is a medication that stimulates the production of red blood cells and is commonly used to treat anemia in patients with chronic kidney disease. Hemoglobin level is the most important parameter to monitor the effectiveness of epoetin alfa therapy. An increase in hemoglobin level indicates an improvement in the patient's anemia and suggests that the medication is effective.
While options a, b, and d are also important considerations in the management of anemia, they do not provide a definitive indication of the effectiveness of epoetin alfa therapy. Reports of increased energy levels and decreased fatigue can be subjective and influenced by many factors. Taking concurrent iron therapy without adverse effects is important to support the production of red blood cells but does not confirm the effectiveness of epoetin alfa. Increased consumption of iron-rich foods can be helpful in managing anemia, but it does not provide a direct indication of the effectiveness of epoetin alfa therapy.
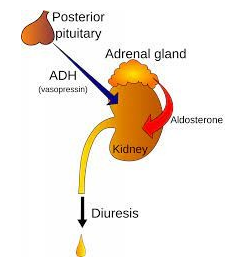
When caring for a client with diabetes insipidus who is receiving antidiuretic hormone intranasally, which serum lab test is most important for the nurse to monitor?
Explanation
Diabetes insipidus is a condition in which the kidneys are unable to conserve water, leading to excessive thirst and urination. It is treated with antidiuretic hormone (ADH), which helps the kidneys retain water and reduce urine output. When caring for a client with diabetes insipidus who is receiving ADH intranasally, it is important for the nurse to monitor the client’s serum osmolality.
Osmolality is a measure of the concentration of particles in a solution and can provide information about the client’s hydration status.
Monitoring serum osmolality can help determine if the ADH therapy is effective in managing the client’s diabetes insipidus.
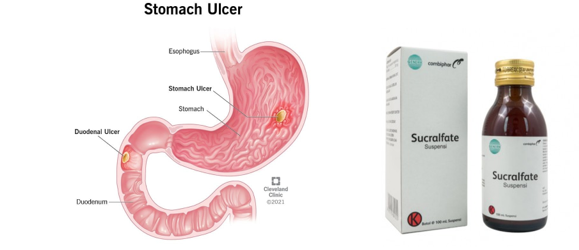
The nurse is planning to administer the antiulcer GI agent sucralfate to a client with a peptic ulcer disease. Which action should the nurse include in this client’s plan of care?
Explanation
Sucralfate is a medication used to treat and prevent the return of duodenal ulcers. It is important to take sucralfate on an empty stomach, either 1 hour before meals or 2 hours after meals. This allows the medication to work effectively by sticking to damaged ulcer tissue and protecting against acid and enzymes so healing can occur.
Two months after taking nitrofurantoin for a bacterial infection, a client reports the onset of severe, watery diarrhea to the home care nurse. How should the nurse respond?
Explanation
Nitrofurantoin is an antibiotic commonly used to treat urinary tract infections. One of the adverse effects of nitrofurantoin is diarrhea, which may be severe and watery. Therefore, it is important for the home care nurse to inform the client that the diarrhea may be a side effect of the medication and requires further evaluation. The nurse should instruct the client to stop taking the medication and contact their healthcare provider for further assessment and treatment. The nurse should also assess the client's fluid and electrolyte status and monitor for signs of dehydration.
Option a is important to consider, but it does not address the potential adverse effect of the medication.
Option c may be appropriate in some cases, but it is not the priority intervention at this time.
Option d is not necessarily true and may cause unnecessary alarm to the client.
An elderly client with heart failure comet to the emergency room because of nausea, vomiting, and anorexia. Based on the client’s signs and symptoms, which data from the medical history has the most significance when planning this client’s care?
Explanation
Digoxin is a medication commonly used to treat heart failure by strengthening the heart's contractions and slowing down the heart rate. However, it can also cause nausea, vomiting, and loss of appetite, especially when levels in the body are too high. Furosemide is a diuretic medication that helps to remove excess fluid from the body, which is often necessary in heart failure. However, it can also cause electrolyte imbalances, such as low potassium levels, which can contribute to nausea and vomiting.
Therefore, in a client with heart failure who is experiencing these symptoms, it is important to assess their medication regimen, including dosages and serum levels, to ensure that they are not experiencing medication side effects or toxicity.
Adjustments may need to be made to the client's medication regimen to manage symptoms effectively and prevent further complications. Options (a), (b), and (d) do not have as direct a correlation to the current symptoms and would not have the same level of significance when planning care for this client.
A client with chemotherapy induced nausea receives a prescription for metoclopramide. Which adverse effect is most important for the nurse to report?
Explanation
Metoclopramide is a medication used to treat nausea and vomiting, including those caused by chemotherapy. However, it has a potential adverse effect of causing extrapyramidal symptoms (EPS), which are involuntary movements of the body, such as muscle spasms, twitching, or restlessness. These symptoms can be distressing for patients and can interfere with their quality of life. EPS can be a sign of tardive dyskinesia, a serious and irreversible neurological disorder.
Therefore, it is essential for the nurse to monitor the client for any signs of EPS and report them immediately to the healthcare provider to prevent further complications. Unusual irritability, diarrhea, and nausea are also potential adverse effects of metoclopramide, but they are not as concerning as EPS.

A client with a history of chronic obstructive pulmonary disease (COPD) receives a new prescription for an ipratropium inhaler. Which action indicates to the nurse that additional teaching is needed?
Explanation
Ipratropium is a medication used to treat chronic obstructive pulmonary disease (COPD)1. When using an ipratropium inhaler for the first time or if it has not been used for a while, it is important to prime the inhaler by spraying it into the air away from your face1. However, the inhaler only needs to be primed with 2 sprays, not 71. If the client primes the inhaler with 7 pumps, it indicates that additional teaching is needed.
Prior to administering oral doses of calcitriol and calcium carbonate to a client with hypoparathyroidism, the nurse notes that the total level of calcium is 14 mg/dL (3.5 mmol/L). Which action should the nurse implement?
Explanation
A total calcium level of 14 mg/dL (3.5 mmol/L) is higher than the normal range of 2.2 to 2.6 millimoles per liter (mmol/L)1. Calcitriol and calcium carbonate are both medications used to increase calcium levels in the blood2. Since the client’s calcium level is already high, it would be important for the nurse to hold both medications and contact the healthcare provider for further instructions.

Sign Up or Login to view all the 46 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

