RN > Exit Exams
Exam Review
HESI RN Exit 2023
Total Questions : 150
Showing 10 questions, Sign in for moreA male preoperative client who has already signed the informed consent for a surgical procedure confides in the practical nurse (PN) that he is really frightened and unsure about undergoing the surgery. Which priority action should the PN take?
Explanation
When a preoperative client expresses fear and uncertainty about undergoing surgery, the priority action for the practical nurse (PN) is to notify the charge nurse of the client's concerns. This is important because the charge nurse can coordinate appropriate interventions and support for the client, ensuring their emotional well-being and addressing their fears.
Let's evaluate the other options:
a) Encourage the client to continue with the scheduled surgery.
While it is important to provide support and reassurance to the client, simply encouraging them to continue with the scheduled surgery may not adequately address their specific concerns and fears. The charge nurse and the healthcare team should be involved to provide the necessary support and information to help alleviate the client's anxiety.
b) Document that the client has expressed concerns about the surgery.
Documenting the client's concerns is important for accurate record-keeping and continuity of care. However, it should not be the only action taken. Notifying the charge nurse is crucial to ensure appropriate follow-up and support for the client.
d) Remind the client that the consent has already been obtained.
Reminding the client that they have already signed the informed consent may not effectively address their fears and concerns. Reassurance and support should be provided, and involving the charge nurse and healthcare team is essential to address the client's emotional well-being.
In summary, when a preoperative client confides in the practical nurse (PN) about being frightened and unsure about undergoing surgery, the priority action is to notify the charge nurse of the client's concerns. This allows for appropriate interventions, support, and coordination of care to address the client's fears, ensure their emotional well-being, and provide necessary information about the surgical procedure.
The parents of a one-year-old child with the diagnosis of hypospadias informed the practical nurse (PN) that they plan to delay corrective surgery to see if the child will outgrow the problem. Which information should the PN provide to these parents?
Explanation
This is the correct answer because it allows the practical nurse (PN) to assess the parents' knowledge and understanding of hypospadias, and to provide accurate and relevant information based on their needs.
Hypospadias is a birth defect in boys in which the opening of the urethra is not located at the tip of the penis, but on the underside of the penis or in the scrotum²³. It is a common condition that affects about one in every 250 males at birth². Hypospadias does not resolve on its own and usually requires surgical correction to prevent complications such as urinary tract infections, difficulty with urination and sexual function, and psychological distress¹². The PN should explain these facts to the parents and encourage them to discuss their concerns and questions with the health care provider. The PN should also provide emotional support and empathy to the parents, as they may feel anxious or guilty about their child's condition.
a) Whatever the parents decide, the staff will be available to support the decision.
This is not the correct answer because it does not address the parents' lack of information and understanding about hypospadias. While it is important to respect the parents' autonomy and decision- making, it is also the PN's responsibility to educate them about the benefits and risks of surgery, and to correct any misconceptions or myths they may have about hypospadias. The PN should not be passive or indifferent about the parents' choice, but rather help them make an informed decision based on evidence- based practice.
b) The child's prognosis will not develop complications if surgery is delayed.
This is not the correct answer because it is not true. Delaying surgery for hypospadias may increase the risk of complications such as infection, scarring, fistula formation, urethral stricture, curvature of the penis, and impaired sexual function¹². The optimal timing for surgery depends on several factors, such as the severity of hypospadias, the child's age and health status, and the surgeon's preference, but it is generally recommended to perform surgery before 18 months of age¹². The PN should not give false reassurance or misinformation to the parents, but rather explain the potential consequences of postponing surgery.
c) Some children do outgrow this type of problem and waiting may be beneficial.
This is not the correct answer because it is also not true. Hypospadias is a congenital condition that does not improve or disappear over time. Waiting for surgery may not be beneficial, but rather harmful, as it may increase the risk of complications and psychological distress for the child¹². The PN should not give false hope or unrealistic expectations to the parents, but rather inform them about the nature and treatment of hypospadias.
Before administering an antibiotic that can cause nephrotoxicity, which laboratory value is most important for the practical nurse (PN) to review?
Explanation
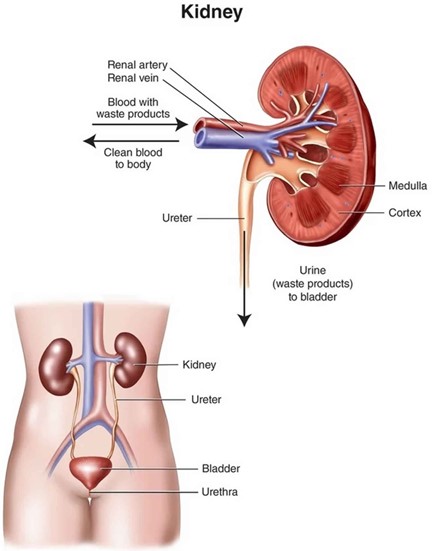
This is the correct answer because BUN and creatinine are the most important laboratory values to monitor for nephrotoxicity, which is the damage or injury to the kidneys caused by certain drugs or chemicals.
Nephrotoxicity can impair the kidneys' ability to filter waste products from the blood, resulting in elevated levels of BUN and creatinine. The normal range for BUN is 7 to 20 mg/dL, and for creatinine is 0.6 to 1.2 mg/dL. The practical nurse (PN) should review these values before administering an antibiotic that can cause nephrotoxicity, such as aminoglycosides, cephalosporins, vancomycin, or sulfonamides. The PN should also monitor the client for signs and symptoms of nephrotoxicity, such as decreased urine output, edema, hypertension, fatigue, nausea, and confusion.
a) Serum calcium
This is not the correct answer because serum calcium is not directly related to nephrotoxicity. Serum calcium is the amount of calcium in the blood, which is important for bone health, muscle contraction, nerve function, and blood clotting. The normal range for serum calcium is 8.5 to 10.2 mg/dL. Serum calcium may be affected by kidney disease, but it is not a reliable indicator of nephrotoxicity.
b) Hemoglobin and hematocrit
This is not the correct answer because hemoglobin and hematocrit are not directly related to nephrotoxicity. Hemoglobin is the protein in red blood cells that carries oxygen, and hematocrit is the percentage of red blood cells in the blood. The normal range for hemoglobin is 13.5 to 17.5 g/dL for men and 12 to 15.5 g/dL for women, and for hematocrit is 38.8 to 50% for men and 34.9 to 44.5% for women.
Hemoglobin and hematocrit may be affected by kidney disease, but they are not reliable indicators of
nephrotoxicity.
c) White blood cell count (WBC)
This is not the correct answer because WBC is not directly related to nephrotoxicity. WBC is the number of white blood cells in the blood, which are part of the immune system and fight infections. The normal range for WBC is 4,500 to 10,000 cells per microliter of blood. WBC may be elevated in response to an infection or inflammation, but it is not a reliable indicator of nephrotoxicity.
The practical nurse (PN) is assessing an older client with left-sided heart failure (HF). What intervention is most important for the PN to implement?
Explanation
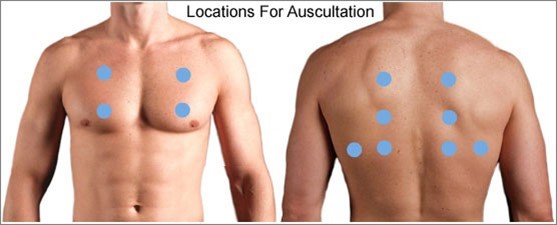
When assessing an older client with left-sided heart failure (HF), the most important intervention for the practical nurse (PN) to implement is to auscultate all lung fields. Left-sided heart failure is characterized by the inability of the left ventricle to effectively pump blood, leading to fluid accumulation in the lungs. Auscultating all lung fields allows the PN to assess for the presence of abnormal lung sounds such as crackles, indicating pulmonary congestion.
Let's evaluate the other options:
a) Inspect for sacral edema.
Sacral edema is commonly associated with right-sided heart failure, not left-sided heart failure. While it is important to assess for edema in clients with heart failure, inspecting for sacral edema may not be the most immediate and crucial intervention in this specific case.
b) Measure urinary output.
Measuring urinary output is a valuable assessment in many clinical situations, but it may not be the most vital intervention in the context of left-sided heart failure. Monitoring urinary output is more relevant in assessing kidney function and fluid balance rather than directly assessing the severity of left-sided heart failure.
d) Check mental acuity.
Checking mental acuity is important in assessing the overall condition of the client, but it is not the most crucial intervention specifically related to left-sided heart failure. Mental status evaluation is more useful in identifying signs of altered mental status or potential complications, rather than directly assessing the impact of left-sided heart failure.
In summary, when assessing an older client with left-sided heart failure, the most important intervention for the practical nurse (PN) to implement is to auscultate all lung fields. This allows for the detection of abnormal lung sounds associated with pulmonary congestion, a hallmark sign of left-sided heart failure.
The practical nurse (PN) receives a report of a stable client who experienced partial-thickness burns over 30% of the body surface area (BSA) 3 days ago.
Which complication is most important for the PN to anticipate?
Explanation
This is the most important complication for the practical nurse (PN) to anticipate because it is a common and potentially life-threatening condition that can occur in clients with severe burns. Curling's ulcer, also known as stress ulcer, is a type of peptic ulcer that develops in the stomach or duodenum as a result of stress, shock, trauma, or burns.
It is caused by decreased blood flow and increased acid secretion in the gastrointestinal tract, which damages the mucosal lining and leads to ulceration and bleeding. The PN should anticipate Curling's ulcer in a client who experienced partial-thickness burns over 30% of the body surface area (BSA) 3 days ago, as this is a major risk factor for developing stress ulcers.
The PN should monitor the client for signs and symptoms of Curling's ulcer, such as abdominal pain, nausea, vomiting, hematemesis, melena, and anemia. The PN should also administer prophylactic medications such as antacids, histamine-2 blockers, or proton pump inhibitors as prescribed by the health care provider.
a) Elevated blood pressure.
This is not the most important complication for the PN to anticipate because it is not directly related to burns. Elevated blood pressure, also known as hypertension, is a condition in which the force of blood against the artery walls is too high. It can be caused by various factors, such as genetics, lifestyle, medications, or underlying diseases. The PN should monitor the blood pressure of a client with burns, as it may reflect changes in fluid status, pain level, or infection. However, elevated blood pressure is not a common or specific complication of burns.
c) Compartment syndrome.
This is not the most important complication for the PN to anticipate because it is more likely to occur in clients with full-thickness burns than partial-thickness burns. Compartment syndrome is a condition in which increased pressure within a closed space (such as a muscle or limb) compromises blood flow and tissue perfusion. It can be caused by trauma, swelling, inflammation, infection, or tight dressings. The PN should assess for compartment syndrome in a client with burns, especially if the burn involves a circumferential area or an extremity. The PN should look for signs and symptoms of compartment syndrome, such as severe pain, pallor, paresthesia, paralysis, and pulselessness. The PN should also loosen or remove any constrictive dressings or splints and notify the health care provider immediately if compartment syndrome is suspected.
d) Excruciating pain.
This is not the most important complication for the PN to anticipate because it is not a complication but rather an expected outcome of burns. Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage. It can be caused by various stimuli, such as heat, cold, pressure, or chemicals. The PN should expect excruciating pain in a client who experienced partial-thickness burns over 30% of the BSA 3 days ago, as this type of burn involves damage to the epidermis and dermis layers of the skin, which contain many nerve endings. The PN should assess the pain level of the client using a valid and reliable pain scale and administer analgesics as prescribed by the health care provider. The PN should also provide nonpharmacological interventions such as distraction, relaxation techniques, music therapy, or massage to help reduce pain.
The practical nurse (PN) is providing care for a client who is receiving an aminoglycoside to treat a bacterial infection.
To assess for signs of ototoxicity, which action should the PN take?
Explanation
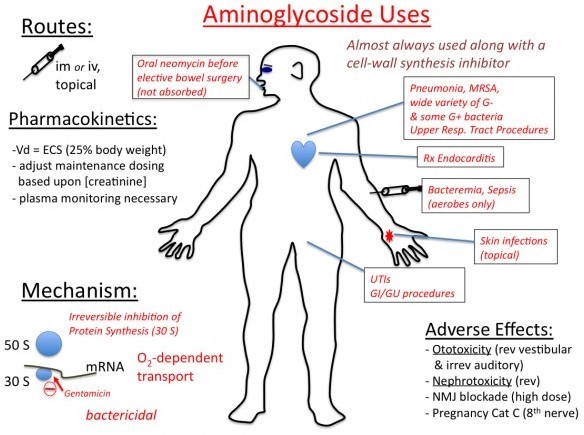
This is the correct answer because it is the best way to assess for signs of ototoxicity, which is a potential adverse effect of aminoglycosides. Ototoxicity is the damage or injury to the inner ear or auditory nerve caused by certain drugs or chemicals. It can result in hearing loss, tinnitus, vertigo, or balance problems. Aminoglycosides are a class of antibiotics that are effective against gram-negative bacteria, but they can also cause ototoxicity by interfering with the function of the hair cells in the cochlea. The practical nurse (PN) should monitor the client's hearing by asking about any changes in hearing acuity, ringing in the ears, or difficulty understanding speech. The PN should also perform a hearing test using a tuning fork or an audiometer if available. The PN should report any signs of ototoxicity to the health care provider and discontinue the aminoglycoside as ordered.
a) Check for changes in vision.
This is not the correct answer because it is not related to ototoxicity. Vision is the ability to see and perceive objects and colors using the eyes and the brain. Vision may be affected by various factors, such as age, genetics, eye diseases, injuries, infections, or medications. However, aminoglycosides do not cause vision problems or impairments. The PN should check for changes in vision in a client who is receiving other drugs that can cause ocular toxicity, such as ethambutol, chloroquine, or digoxin.
c) Observe the skin for a rash.
This is not the correct answer because it is not related to ototoxicity. A rash is a change in the color, texture, or appearance of the skin that may be caused by various factors, such as allergies, infections, inflammation, or medications. A rash may present as redness, itching, swelling, blisters, bumps, or scales.
Aminoglycosides can cause skin reactions such as rash or urticaria in some clients who are hypersensitive or allergic to them. The PN should observe the skin for a rash in a client who is receiving an aminoglycoside and report any signs of an allergic reaction to the health care provider. However, a rash is not a sign of ototoxicity.
d) Measure the urinary output.
This is not the correct answer because it is not related to ototoxicity. Urinary output is the amount of urine produced and excreted by the kidneys and bladder. It is an indicator of renal function and fluid balance. The normal range for urinary output is 0.5 to 1 mL/kg/hour for adults. Urinary output may be affected by various factors, such as fluid intake, dehydration, diuretics, kidney disease, or medications. Aminoglycosides can cause nephrotoxicity, which is another potential adverse effect of these drugs. Nephrotoxicity is the damage or injury to the kidneys caused by certain drugs or chemicals. It can impair the kidneys' ability to filter waste products from the blood, resulting in reduced urine production and oliguria. The PN should measure the urinary output in a client who is receiving an aminoglycoside and report any signs of nephrotoxicity to the health care provider. However, urinary output is not a sign of ototoxicity
A client who is reaching saturation with medication reports the onset of muscle soreness and fatigue, and the practical nurse (PN) notes that the client's skin is warm to the touch.
Which action by the PN is a priority?
Explanation
This is the priority action by the practical nurse (PN) because it can help identify and prevent a potential adverse reaction to the medication. A client who is reaching saturation with medication means that the client has reached the maximum level of medication in the blood that can produce the desired therapeutic effect. However, this also means that the client is at a higher risk of developing toxicity or side effects from the medication. The PN should report the findings of muscle soreness, fatigue, and warm skin to the charge nurse, as these may indicate signs of inflammation, infection, or allergic reaction to the medication. The PN should also monitor the client's vital signs, oxygen saturation, and laboratory values, and document the findings. The charge nurse should notify the health care provider and adjust the medication dosage or regimen as ordered.
a) Administer a PRN dose of acetaminophen.
This is not the priority action by the PN because it does not address the underlying cause of the client's symptoms. Acetaminophen is an analgesic and antipyretic medication that can help reduce pain and fever. However, it does not treat inflammation, infection, or allergy, which may be the reasons for the client's muscle soreness, fatigue, and warm skin. The PN should administer a PRN dose of acetaminophen only after reporting the findings to the charge nurse and obtaining an order from the health care provider.
b) Encourage the client to drink fluids.
This is not the priority action by the PN because it does not address the underlying cause of the client's symptoms. Drinking fluids can help maintain hydration and electrolyte balance in the body, which are important for normal functioning of cells and organs. However, it does not treat inflammation, infection, or allergy, which may be the reasons for the client's muscle soreness, fatigue, and warm skin. The PN should encourage the client to drink fluids only after reporting the findings to the charge nurse and obtaining an order from the health care provider.
d) Monitor the client's serum lipid levels.
This is not the priority action by the PN because it is not related to the client's symptoms. Serum lipid levels are measures of fats and cholesterol in the blood, which are important for energy production, hormone synthesis, and cell membrane structure. However, they are not related to inflammation, infection, or allergy, which may be the reasons for the client's muscle soreness, fatigue, and warm skin. The PN should monitor the client's serum lipid levels only if they are prescribed a medication that can affect lipid metabolism, such as statins or fibrates.
A college student brings his roommate to the clinic because the roommate has been talking to someone who is not present. The student tells the practical nurse (PN) that his roommate is acting strange.
Which question should the PN ask the client next?
Explanation
This is the correct answer because it is the most relevant and respectful question to ask the client next. Asking about the onset of the voices can help the practical nurse (PN) determine the possible causes and triggers of the client's hallucinations, which are sensory perceptions that occur without external stimuli. Hallucinations can be caused by various factors, such as mental disorders, substance abuse, medication side effects, physical illnesses, sleep deprivation, or stress. The PN should ask about the frequency, duration, and content of the voices, as well as the client's response to them. The PN should also assess the client's mood, behavior, cognition, and insight. The PN should use a calm, supportive, and nonjudgmental approach when communicating with the client who is experiencing hallucinations.
a) "Are you planning to obey the voices?"
This is not the correct answer because it is not a priority question to ask the client next. Asking about the client's intention to obey the voices can help the PN assess the risk of harm to self or others, which is an important aspect of safety. However, this question may also imply that the PN believes or validates the voices, which may reinforce the client's delusions or false beliefs. The PN should ask about the client's plan to obey the voices only after establishing rapport and trust with the client, and after assessing the nature and content of the voices.
b) "Have you taken any hallucinogens?"
This is not the correct answer because it is not a respectful question to ask the client next. Asking about the client's substance use can help the PN identify the possible causes of hallucinations, as some drugs such as LSD, psilocybin, or ketamine can induce hallucinogenic effects. However, this question may also sound accusatory or confrontational, which may offend or alienate the client. The PN should ask about the client's substance use in a sensitive and nonthreatening manner, and after obtaining informed consent and ensuring confidentiality.
d) "Do you believe the voices are real?"
This is not the correct answer because it is not a helpful question to ask the client next. Asking about the client's belief in the reality of the voices can help the PN assess the level of insight or awareness that the client has about their condition. However, this question may also challenge or invalidate the client's perception, which may cause defensiveness or resistance. The PN should avoid arguing or disagreeing with the client about their hallucinations, as this may damage the therapeutic relationship. The PN should acknowledge and accept the client's experience without endorsing or reinforcing it.
The practical nurse (PN) notices that one of the unlicensed assistive personnel (UAP) working in the long- term care facility consistently records subnormal temperatures when using the thermometer.
Which action should the PN take first?
Explanation
When the practical nurse (PN) notices that one of the unlicensed assistive personnel (UAP) consistently records subnormal temperatures when using the thermometer, the first action the PN should take is to observe how the UAP obtains temperatures. This allows the PN to directly assess the UAP's technique and determine if any errors or inaccuracies are occurring during temperature measurement. By observing the process, the PN can identify any potential issues, such as incorrect placement of the thermometer or improper technique, and provide appropriate guidance and education.
Let's evaluate the other options:
a) Show the UAP how to chart temperatures.
While accurate charting of temperatures is important, it is not the primary concern in this situation. The PN should first focus on assessing the UAP's temperature measurement technique before addressing charting skills.
b) Return the thermometer for recalibration.
Returning the thermometer for recalibration may be necessary if there is evidence or suspicion of a malfunctioning thermometer. However, before assuming that the thermometer is the issue, it is important to first observe how the UAP obtains temperatures to rule out any human error in the measurement process.
d) Demonstrate how to use the equipment.
Demonstrating how to use the equipment may be beneficial, but it should not be the first action taken in this scenario. The PN should first observe the UAP's technique to identify any potential errors or issues in temperature measurement. Based on the observation, the PN can provide specific guidance and demonstrate the correct technique if necessary.
In summary, when a practical nurse (PN) notices that a UAP consistently records subnormal temperatures when using the thermometer, the first action the PN should take is to observe how the UAP obtains temperatures. This allows for direct assessment of the UAP's technique and identification of any potential errors or issues. Based on the observation, the PN can provide appropriate guidance, education, and intervention as needed to ensure accurate temperature measurement.
At the first dressing change, the practical nurse (PN) tells the client that her mastectomy incision is healing well, but the client refuses to look at the incision and refuses to talk about it.
Which response by the PN to the client's silence is best?
Explanation
When a client refuses to look at their mastectomy incision and refuses to talk about it, the best response by the practical nurse (PN) is to respect the client's autonomy and validate their feelings. Option a) acknowledges the client's discomfort and provides reassurance that it is okay for them to decline looking or talking about the incision at the moment. It also offers support by letting the client know that the incision will be available for examination when they feel ready to do so.
Let's evaluate the other options:
b) "Would you like me to call another nurse to be here while I show you the wound?"
This response assumes that the client needs someone else present to address their refusal to look at the incision. While having another nurse present may be helpful for some clients, it is not the appropriate first response. Respecting the client's autonomy and providing support should be the initial approach.
c) "Part of recovery is accepting your new body image, and you will need to look at your incision."
This response may come across as directive and insensitive. It implies that the client must look at their incision as part of their recovery process, disregarding their feelings and personal choices. It is important to respect the client's autonomy and allow them to navigate their own healing journey at their own pace.
d) "You will feel beter when you see that the incision is not as bad as you may think."
This response invalidates the client's feelings and assumes that their concerns about the incision are unfounded. It is essential to respect the client's emotions and validate their experience rather than dismissing or minimizing their concerns.
In summary, when a client refuses to look at their mastectomy incision and refuses to talk about it, the best response by the practical nurse (PN) is to acknowledge the client's discomfort, respect their autonomy, and provide reassurance that it is okay for them to decline looking or talking about the incision at that moment. The client's readiness to address the incision should be honored, and support should be offered when they are ready.
Sign Up or Login to view all the 150 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

