Hesi RN Fundamentals of Nursing
Total Questions : 44
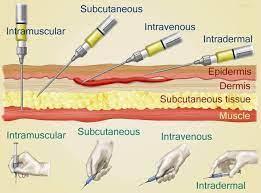
Showing 25 questions, Sign in for moreThe nurse is teaching a client how to self-administer low-molecular-weight heparin subcutaneously. Which instruction should the nurse include?
Explanation
Choice A Reason: Massaging the injection site can cause bruising and bleeding, and is not recommended for subcutaneous heparin injections.
Choice B Reason: Rotating injections between different body sites can increase the risk of hematoma formation and skin irritation, and is not advised for subcutaneous heparin injections.
Choice C Reason: Expelling the air in the prefilled syringe can result in a loss of medication dose, and is not necessary for subcutaneous heparin injections.
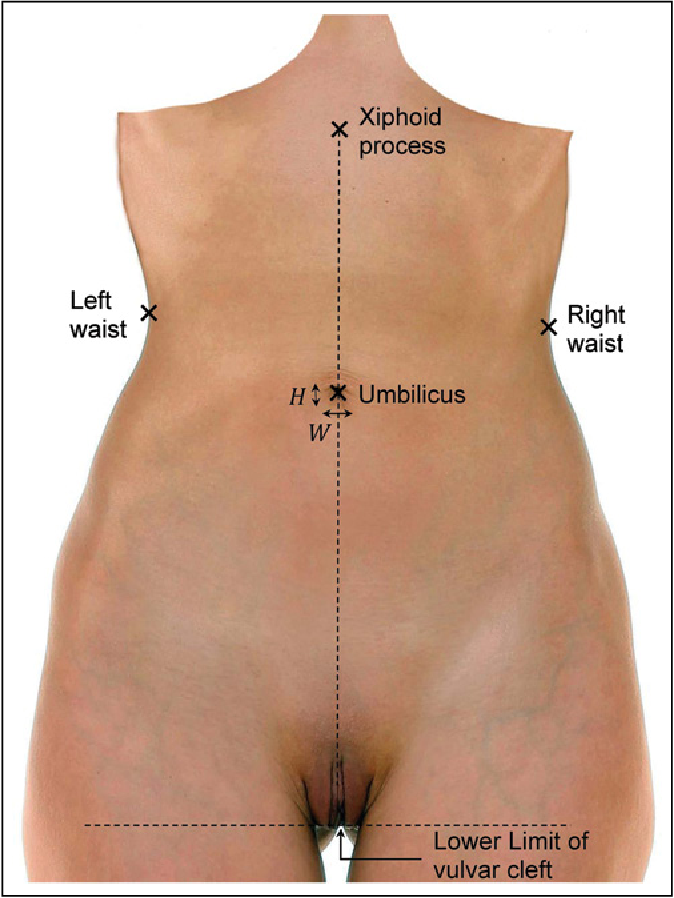
Choice D Reason: Injecting in the abdominal area at least 2 inches from the umbilicus is the correct technique for subcutaneous heparin injections, as it reduces the risk of injury to blood vessels and nerves, and ensures consistent absorption of the medication.
Patient Data
History and Physical
The client is a 56-year old woman who had an anteroposterior spinal fusion 2 days ago. She tolerated the procedure well and has been progressively increasing her walking distance.
Nurses Notes
1200
- Heart rate: 98 bpm
- Pain rating: 5/10
- Morphine 2.5 mg given
- The client did ambulation exercises with physical therapy
1300
- Heart rate: 78 bpm
- Pain rating: 3/10
- Ibuprofen 800 mg given
- The client is resting in bed
1400
Orders
- Heart rate 118 bpm
Based on the trending heart rate and pain score, what should the nurse do? Select all that apply.
Explanation
Choice A: Lead the client in guided imagery
This is a correct choice because guided imagery is a non-pharmacological intervention that can help reduce pain and anxiety by creating a relaxing mental image for the client. Guided imagery can also lower the heart rate and blood pressure by activating the parasympathetic nervous system.
Choice B: Give a dose of 2.5 mg of Morphine
This is an incorrect choice because morphine is an opioid analgesic that can cause respiratory depression, hypotension, and bradycardia. The client's heart rate is already elevated, which could indicate inadequate pain relief or anxiety. Giving more morphine could worsen the client's condition and mask the underlying cause of the pain.
Choice C: Assist the client to walk around the room
This is an incorrect choice because walking around the room could increase the client's pain and heart rate by stimulating the sympathetic nervous system. The client has already done ambulation exercises with physical therapy at 1200, so there is no need to repeat them at 1400. The client should be allowed to rest in bed and conserve energy.
Choice D: Assess for sources of pain other than the surgical site
This is a correct choice because the nurse should always assess the client holistically and rule out any other potential causes of pain, such as infection, inflammation, or ischemia. The nurse should also check the surgical site for any signs of bleeding, hematoma, or infection. The nurse should use a comprehensive pain assessment tool that includes the location, intensity, quality, duration, frequency, and aggravating and relieving factors of the pain.
Choice E: Consult with the surgeon about the pain level
This is a correct choice because the nurse should collaborate with the surgeon and other members of the health care team to provide optimal pain management for the client. The nurse should report the client's pain score, vital signs, medication administration, and response to interventions. The surgeon may order additional tests or medications to address the cause of the pain and improve the client's comfort.
The nurse is caring for a client who is postoperative and receiving supplemental oxygen at 2 L/minute via nasal cannula. The oxygen saturation is 89%. Which action should the nurse implement?
Explanation
Choice A: Switching to a non-rebreather mask is not appropriate for this client. A non-rebreather mask delivers a high concentration of oxygen (up to 100%) and is used for clients who are critically ill or have very low oxygen saturation levels. This client has a mild hypoxemia and does not need such a high flow of oxygen.
Choice B: Removing the nasal cannula is not advisable for this client. The client is postoperative and may have impaired gas exchange due to anesthesia, pain, or decreased mobility. Removing the supplemental oxygen may worsen the client's hypoxemia and increase the risk of complications.
Choice C: Increasing the oxygen to 3 L/minute is the best action for this client. The client has a mild hypoxemia (normal oxygen saturation is 95% or higher) and may benefit from a slight increase in oxygen delivery. A nasal cannula can deliver oxygen at a low flow rate (1 to 6 L/minute) and is suitable for clients who are stable and need mild to moderate oxygen therapy.
Choice D: Verifying the placement of the pulse oximeter is not a priority for this client. The pulse oximeter measures the oxygen saturation of hemoglobin in arterial blood by using a sensor attached to the finger, toe, earlobe, or forehead. The placement of the sensor may affect the accuracy of the reading, but it is not likely to cause a significant change in the oxygen saturation level. The nurse should verify the placement of the pulse oximeter after increasing the oxygen flow rate and reassessing the client's condition.
Which assessment is most important for the nurse to perform prior to the application of a heating pad?
Explanation
Choice A: Limitations to range of motion are not directly related to the application of a heating pad. A heating pad may help reduce pain and stiffness, but it does not affect the range of motion itself.
Choice B: Muscle strength and tone are also not directly related to the application of a heating pad. A heating pad may relax tense muscles, but it does not affect the strength or tone of the muscles.
Choice C: Degree of neurosensory impairment is the most important assessment for the nurse to perform prior to the application of a heating pad. A heating pad can cause burns or tissue damage if the patient has impaired sensation and cannot feel the heat or pain. The nurse should check the patient's ability to perceive temperature, pressure, and pain before applying a heating pad.
Choice D: Presence of rebound phenomenon is not relevant to the application of a heating pad. Rebound phenomenon refers to the worsening of symptoms after discontinuing a medication or treatment. A heating pad does not cause rebound phenomenon.
After an intravenous antibiotic is started, the nurse determines that the medication is not prescribed for the client and stops the infusion. Which action should the nurse implement next?
Explanation
Choice A: Notify the healthcare provider is the correct action because it is the nurse's responsibility to report any medication errors or adverse reactions to the prescriber as soon as possible.
Choice B: Document the event on the chart is not the next action because it should be done after notifying the healthcare provider and completing an incident report.
Choice C: Complete an incident report is not the next action because it should be done after notifying the healthcare provider and before documenting the event on the chart.
Choice D: Inform the nurse on the next shift is not the next action because it should be done after documenting the event on the chart and during handoff.
A hospitalized client who has an advance directive and healthcare power of attorney is receiving enteral nutrition through a nasogastric (NG) tube. The client vomits and appears to be choking. Which action should the nurse take?
Explanation
Choice A: Irrigating the nasogastric tube with water is not the correct action because it may worsen the choking and increase the risk of aspiration.
Choice B: Reviewing the advance directive document is not the correct action because it is not a priority in this situation. The nurse should act quickly to relieve the choking and prevent complications.
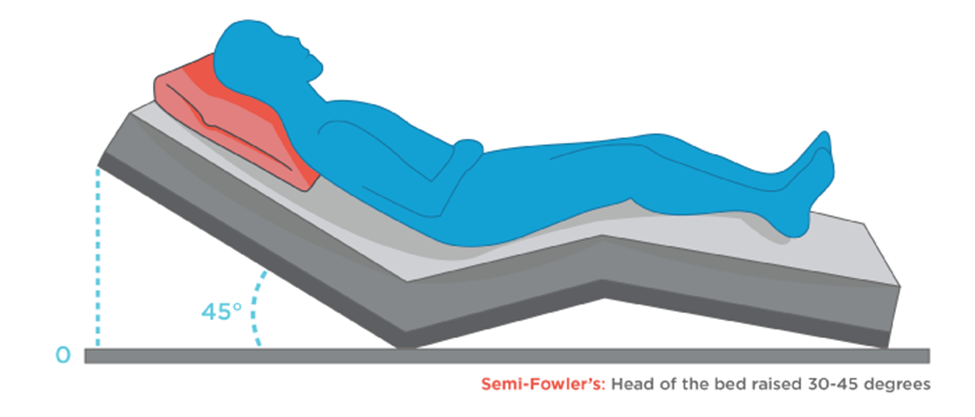
Choice C: Elevating the head of the bed 45 degrees is the correct action because it helps clear the airway and reduce vomiting.
Choice D: Performing oropharyngeal suctioning is not the correct action because it may stimulate gagging and vomiting. The nurse should suction only if there are visible secretions or vomitus in the mouth.
A client with a family history of cardiac disease is seeking information to control risk factors. Which lifestyle modification is most important for the nurse to encourage?
Explanation
Choice A: Regular exercise is a good lifestyle modification, but it is not as important as smoking cessation. Exercise can help lower blood pressure, cholesterol, and weight, but it cannot reverse the damage caused by smoking.
Choice B: Stress reduction is a good lifestyle modification, but it is not as important as smoking cessation. Stress can trigger or worsen cardiac problems, but it cannot cause them as directly as smoking.
Choice C: Smoking cessation is the most important lifestyle modification because smoking is a major risk factor for cardiac disease. Smoking damages the blood vessels, increases blood pressure, reduces oxygen supply, and promotes clot formation.
Choice D: Low-fat diet is a good lifestyle modification, but it is not as important as smoking cessation. A low-fat diet can help lower cholesterol and prevent plaque buildup, but it cannot undo the effects of smoking.
The nurse observes a decrease in a client's level of consciousness. Which vital sign should the nurse obtain first?
Explanation
Choice A: Blood pressure is not the first vital sign to obtain because it is not as sensitive to changes in the level of consciousness as respiratory rate. Blood pressure may be normal or elevated in some cases of decreased consciousness, such as stroke or head injury.
Choice B: Temperature is not the first vital sign to obtain because it is not as relevant to the level of consciousness as respiratory rate. Temperature may be normal or slightly elevated in some cases of decreased consciousness, such as infection or dehydration.
Choice C: Respiratory rate is the first vital sign to obtain because it reflects the adequacy of oxygenation and ventilation, which are essential for brain function. Respiratory rate may be increased, decreased, or irregular in cases of decreased consciousness, depending on the cause and severity.
Choice D: Pulse rate is not the first vital sign to obtain because it is not as indicative of the level of consciousness as respiratory rate. Pulse rate may be normal, fast, or slow in cases of decreased consciousness, depending on the cause and compensatory mechanisms.
Patient Data
History and Physical
The client is a 44-year-old with cerebral palsy who is non-verbal and has a severe intellectual disability. He requires total care at home, which is provided by his two sisters, a home health nurse, and an unlicensed home health aide. The client is currently in the hospital for a lower respiratory infection.
Nurses Notes
1000
- Noted the client's clothes and sheets are wet. The client voided approximately 75 mL of urine. The client's sister says that he usually wears adult diapers at home as he is unable to communicate when he needs to void.
Review H and P and nurse's notes.
Identify from the choices area to specify which condition the client is most likely experiencing, two actions the nurse should take to address that condition, and two parameters the nurse should monitor to assess the client's progress.
Explanation
Potential Conditions
Overflow urinary incontinence
This is the correct choice because overflow urinary incontinence is the involuntary loss of urine due to a distended bladder that cannot empty completely. The client has cerebral palsy, which can affect the bladder muscles and nerves, causing them to lose coordination and contractility. The client is also non-verbal and has severe intellectual disability, which can impair his ability to sense or communicate the need to void. The client's clothes and sheets are wet, indicating that he has leaked urine. The client voided approximately 75 mL of urine, which is a small amount for an adult male. These signs suggest that the client has overflow urinary incontinence.
Actions to Take
Provide skin care
This is a correct choice because the nurse should provide skin care to the client who has overflow urinary incontinence. The nurse should cleanse the perineal area with mild soap and water, pat dry, and apply a barrier cream or ointment to protect the skin from moisture and irritation. The nurse should also change the client's clothes and sheets as needed to keep him dry and comfortable.
Place an incontinence containment product under the client
This is a correct choice because the nurse should place an incontinence containment product under the client who has overflow urinary incontinence. An incontinence containment product is a device or material that absorbs or collects urine, such as a diaper, pad, or catheter. The nurse should choose an appropriate product based on the client's preferences, needs, and abilities. The nurse should also monitor the product for leakage, odor, or infection, and change it regularly.
Parameters to Monitor
Intake and output
This is a correct choice because the nurse should monitor the intake and output of the client who has overflow urinary incontinence. The nurse should measure and record the amount and type of fluids that the client consumes and excretes. The nurse should also note the color, clarity, odor, and specific gravity of the urine. The nurse should compare the intake and output with the normal ranges for the client's age, weight, and condition. The nurse should report any abnormal findings or changes to the health care provider.
Post-void residual
This is a correct choice because the nurse should monitor the post-void residual of the client who has overflow urinary incontinence. Post-void residual is the amount of urine left in the bladder after voiding. The nurse can measure it by using a bladder scanner or inserting a catheter after the client voids. A normal post-void residual is less than 50 mL for an adult male. A high post-void residual indicates that the bladder is not emptying completely, which can lead to overflow urinary incontinence. The nurse should report any high post-void residual to the health care provider.
A client who had surgery 3 days ago is sitting with head of bed at 75 degrees and requests to be repositioned. Which instruction is most important for the nurse to provide to the unlicensed assistive personnel (UAP)?
Explanation
Choice A: Have the client hold a pillow over the abdomen to cough and deep breathe is not the most important instruction because it is not related to repositioning. This is a good practice to prevent respiratory complications after surgery, but it can be done at any time.
Choice B: Encourage the client to eat all of the meals that are sent is not the most important instruction because it is not related to repositioning. This is a good practice to promote nutrition and healing after surgery, but it can be done at any time.
Choice C: Offer fruit juice at least twice during both the day and evening shifts is not the most important instruction because it is not related to repositioning. This is a good practice to prevent dehydration and constipation after surgery, but it can be done at any time.
Choice D: Lower the bed prior to helping the client to move up in bed is the most important instruction because it reduces the risk of injury and falls for both the client and the UAP. This is a safety measure that should be done before any repositioning.
The nurse is teaching a client how to self-administer low-molecular-weight heparin subcutaneously. Which instruction should the nurse include?
Explanation
Choice A: Massage the injection site to increase absorption is not a correct instruction because it may cause bruising and bleeding. Low-molecular-weight heparin is absorbed quickly without massaging.
Choice B: Rotate injections between the abdomen and gluteal areas is not a correct instruction because it may increase the risk of hematoma and infection. The abdomen is preferred over other sites for low-molecular-weight heparin injections.
Choice C: Expel the air in the prefilled syringe prior to injection is not a correct instruction because it may result in loss of medication and inaccurate dosing. The air bubble in the prefilled syringe should be left intact.
Choice D: Inject in abdominal area at least 2 inches from the umbilicus is a correct instruction because it ensures adequate subcutaneous tissue and avoids major blood vessels and organs.
A 16-year-old emancipated client is being seen in the emergency department following a minor automobile accident. The client's parents arrive and are asking questions about the client's laboratory results. Which response is best for the nurse to provide?
Explanation
Choice A: "I'm sorry, but your child's medical information is none of your business." is not a good response because it is rude and disrespectful. The nurse should maintain professionalism and empathy when dealing with parents.
Choice B: "I can give you those results as soon as I get them back from the lab." is not a good response because it violates confidentiality and privacy. The nurse should not share any medical information with anyone without the client's consent.
Choice C: "The healthcare provider will share this information with you." is not a good response because it implies that the parents have a right to know their child's medical information. The nurse should not make promises or assumptions that may not be true.
Choice D: "I can only give medical information to your child because they are legally an adult." is a good response because it explains the legal status of an emancipated minor and respects their autonomy. The nurse should inform the parents that their child has the right to make their own decisions regarding their health care.
The nurse observes an unlicensed assistive personnel (UAP) who is providing a total bed bath for a confused and lethargic client. The UAP is soaking the client’s foot in a basin of warm water placed on the bed. Which action should the nurse take?
Explanation
Choice A: Remind the UAP to dry between the client’s toes completely is not the best action because it does not address the risk of spillage and wetness on the bed. Drying between the toes is important to prevent fungal infections, but it can be done after removing the basin.
Choice B: Advise the UAP that this procedure is damaging to the skin is not the best action because it is not accurate and may cause confusion. Soaking the foot in warm water is not harmful to the skin, unless it is too hot or too long.
Choice C: Add skin cream to the basin of water while the foot is soaking is not the best action because it does not solve the problem and may waste the cream. Skin cream should be applied after drying the foot, not mixed with water.
Choice D: Remove the basin of water from the client’s bed immediately is the best action because it prevents potential hazards such as soaking, infection, or electric shock. The nurse should ensure that the bed is dry and clean before continuing with the bath.
While assessing a client’s blood pressure using an aneroid sphygmomanometer, the nurse inflates the cuff to an initial reading of 160 mm calibration. Upon release of the air valve, the nurse immediately hears loud Korotkoff sounds. Which action should the nurse implement next?
Explanation
Choice A reason: This is the correct action to take when the nurse hears loud Korotkoff sounds immediately after releasing the air valve. This indicates that the cuff was not inflated high enough to occlude the arterial blood flow and the initial systolic reading was inaccurate. The nurse should release the air, wait for 15 to 30 seconds, and then reinflate the cuff to 30 mm Hg above the first systolic sound. This will ensure a more accurate measurement of the blood pressure.
Choice B reason: This is not the correct action to take when the nurse hears loud Korotkoff sounds immediately after releasing the air valve. Continuing the blood pressure assessment until the last Korotkoff sound is heard will result in a lower systolic reading and a higher diastolic reading than the actual blood pressure of the client. The nurse should release the air and reinflate the cuff to 30 mm Hg above the first systolic sound.
Choice C reason: This is not the correct action to take when the nurse hears loud Korotkoff sounds immediately after releasing the air valve. Repositioning the stethoscope in the antecubital fossa over the palpable brachial pulse point will not change the fact that the cuff was not inflated high enough to occlude the arterial blood flow. The nurse should release the air and reinflate the cuff to 30 mm Hg above the first systolic sound.
Choice D reason: This is not the correct action to take when the nurse hears loud Korotkoff sounds immediately after releasing the air valve. Inflating the cuff quickly to a higher mm Hg reading than the previously auscultated systolic sound will cause discomfort and pain to the client and may damage the blood vessels. The nurse should release the air and reinflate the cuff to 30 mm Hg above the first systolic sound.
After administering oxycodone to a client one hour ago, the client is reporting severe pain. Which intervention should the nurse implement next?
Explanation
Choice A: Reassess the client and the level of pain is the correct intervention because it helps the nurse evaluate the effectiveness of the medication and plan further actions. The nurse should use a valid and reliable pain scale and check for any signs of adverse effects or complications.
Choice B: Tell the client the medication needs more time to work is not a correct intervention because it may dismiss the client’s pain and delay appropriate treatment. The nurse should acknowledge the client’s pain and explain the expected onset and duration of the medication.
Choice C: Ask the UAP to offer a backrub to the client is not a correct intervention because it may not be sufficient or appropriate for the client’s pain. The nurse should assess the client’s pain before delegating any nonpharmacological interventions to the UAP.
Choice D: Encourage the client to focus on taking deep breaths is not a correct intervention because it may not be effective or feasible for the client’s pain. The nurse should assess the client’s pain and offer other complementary therapies that are suitable and acceptable for the client.
The nurse observes the unlicensed assistive personnel (UAP) securing a client’s wrist restraints to the bedside rails. Which action is most important for the nurse to implement?
Explanation
Choice A: Complete an adverse occurrence/incident report is not the most important action because it does not correct the immediate problem or prevent harm to the client. The nurse should report the incident after ensuring the safety and comfort of the client.
Choice B: Ensure that the restraints are not too tight is an important action, but it is not enough to address the issue of improper securing of the restraints. The nurse should also teach the UAP how to secure the restraints correctly and safely.
Choice C: Demonstrate proper securing of the restraints is the most important action because it educates the UAP and prevents potential complications such as injury, infection, or circulation impairment. The nurse should show the UAP how to secure the restraints to a movable part of the bed frame, not to the rails.
Choice D: Initiate the facility’s restraint flow sheet is an important action, but it is not urgent or critical in this situation. The nurse should document and monitor the use of restraints according to the facility’s policy, but only after ensuring that they are applied correctly and appropriately.
The nurse plans to administer naloxone 1 mg. The label of the 10 mL vial indicates that the drug concentration is 0.4 mg/mL. How many mL should the nurse administer? (Enter numeric value only. If rounding is required, round to the nearest tenth.)
Explanation
To find the volume of the solution needed, the nurse can use the formula:
Volume (mL) = Dose (mg) / Concentration (mg/mL)
Substituting the given values, we get:
Volume (mL) = 1 mg / 0.4 mg/mL
Simplifying, we get:
Volume (mL) = 2.5 mL
Therefore, the nurse should administer 2.5 mL of naloxone to give a dose of 1 mg.

The nurse is assessing a client in the clinic who is frightened and does not understand English. Which intervention should the nurse implement first?
Explanation
Choice A: Request a family member to remain with the client is not the best intervention because it may compromise the confidentiality and accuracy of the assessment. The family member may not be able to translate correctly or may influence the client’s responses.
Choice B: Ask for the support of one of the client’s friends is not the best intervention because it may also violate the privacy and validity of the assessment. The friend may not be qualified or willing to translate or may have a conflict of interest with the client.
Choice C: Use drawings that are universal for all cultures is not the best intervention because it may not be sufficient or appropriate for the assessment. Drawings may not convey all the information needed or may be misinterpreted by the client.
Choice D: Obtain a staff member who is a bilingual interpreter is the best intervention because it facilitates the communication and understanding between the nurse and the client. The interpreter should be trained and certified in medical terminology and cultural sensitivity.
A male client with a nasogastric tube connected to low intermittent suction tells the nurse that his mouth is very dry. Which action should the nurse implement?
Explanation
Choice A Reason: This is incorrect because instilling normal saline solution into the nasogastric tube can cause fluid overload, electrolyte imbalance, or aspiration. Clamping the tube for one hour can also increase the risk of aspiration and gastric distension.
Choice B Reason: This is incorrect because turning the suction off can cause gastric distension and discomfort. Rinsing the mouth with cool water can also increase the risk of aspiration if the client swallows some of the water.
Choice C Reason: This is correct because oral sponge toothettes are soft and gentle on the oral mucosa and can help moisten and cleanse the mouth without causing irritation or aspiration.
Choice D Reason: This is incorrect because teaching the client that the oral mucosa must remain dry is false and can lead to further dryness, cracking, bleeding, and infection. The oral mucosa should be kept moist and clean to prevent these complications.
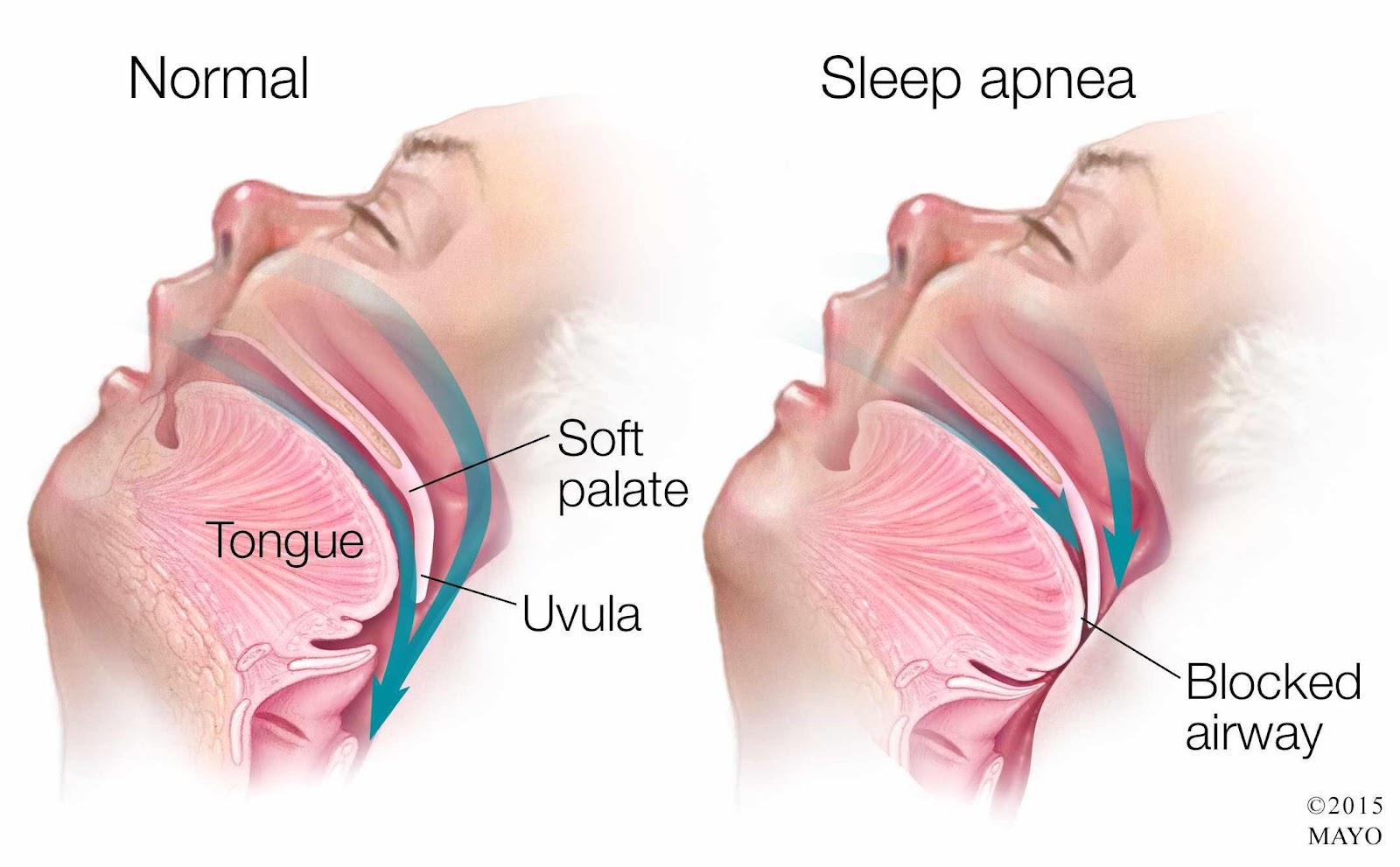
The nurse administers morphine to a client for chest pain who also has obstructive sleep apnea (OSA). Which intervention is most important for the nurse to implement before leaving the client alone?
Explanation
Choice A Reason: This is incorrect because lifting and locking the side rails in place is a standard safety measure for all clients, but it does not address the specific risk of respiratory depression caused by morphine and OSA.
Choice B Reason: This is correct because applying the client's positive airway pressure device can help maintain airway patency and prevent hypoxia and hypercapnia, which are common complications of OSA and opioid use.
Choice C Reason: This is incorrect because elevating the head of the bed to a 45-degree angle can help reduce chest pain and dyspnea, but it does not prevent airway obstruction or respiratory depression.
Choice D Reason: This is incorrect because removing dentures or other oral appliances can help prevent aspiration, but it does not affect the client's breathing pattern or oxygenation.
Prior to initiating digital removal of a fecal impaction, it is most important for the nurse to perform which client assessment?
Explanation
Choice A Reason: This is incorrect because abdominal girth can indicate the presence of fecal impaction, but it does not reflect the client's hemodynamic status or potential complications of the procedure.
Choice B Reason: This is incorrect because bowel sounds can indicate the level of bowel motility, but they do not provide information about the client's cardiovascular or respiratory function.
Choice C Reason: This is correct because vital signs can indicate the client's baseline condition and any changes during or after the procedure. Digital removal of a fecal impaction can stimulate the vagus nerve and cause bradycardia, hypotension, or cardiac arrest.
Choice D Reason: This is incorrect because breath sounds can indicate the client's respiratory status, but they are not directly affected by the procedure. However, breath sounds should be monitored for signs of aspiration if the client receives sedation or analgesia.
The nurse identifies several nursing problems for a client with paraplegia who has been having fecal incontinence and diarrhea. The client's parent is the primary caregiver. In planning care, the nurse should determine which problem is the highest priority?
Explanation
Choice A Reason: This is correct because fluid volume deficit is a life-threatening condition that can result from diarrhea and fecal incontinence. The nurse should monitor the client's fluid intake and output, electrolytes, weight, urine specific gravity, and skin turgor.
Choice B Reason: This is incorrect because bowel incontinence is a significant problem that can affect the client's dignity, comfort, and skin integrity, but it is not as urgent as fluid volume deficit. The nurse should implement a bowel management program and provide appropriate hygiene and skin care.
Choice C Reason: This is incorrect because caregiver role strain is a potential problem that can affect the parent's well-being and ability to provide care, but it is not as critical as fluid volume deficit. The nurse should assess the parent's coping skills, support system, and respite needs.
Choice D Reason: This is incorrect because impaired bed mobility is a chronic problem that can affect the client's functional status and quality of life, but it is not as serious as fluid volume deficit. The nurse should assist the client with positioning, turning, transferring, and exercising.
A client who is on complete bedrest frequently calls the nurse for the bedpan to urinate. Which action should the nurse take to evaluate the client for urinary retention?
Explanation
Choice A Reason: This is incorrect because palpating the suprapubic region for distention can be inaccurate and unreliable, as it can be affected by factors such as obesity, abdominal muscle tone, and bowel gas.
Choice B Reason: This is correct because scanning the client's bladder after voiding can measure the post-void residual urine volume, which indicates the amount of urine left in the bladder after urination. A high post-void residual urine volume can indicate urinary retention.
Choice C Reason: This is incorrect because reviewing the chart for number of voids over last 24 hours can provide information about the frequency of urination, but not the amount or completeness of urination.
Choice D Reason: This is incorrect because evaluating the client for urinary incontinence can assess the involuntary loss of urine, but not the ability to empty the bladder completely.
The nurse observes that there are reddened areas on the cheekbones of a client receiving oxygen per nasal cannula at 3 L/minute, and the client's oxygen saturation level is 92%. Which intervention would the nurse implement?
Explanation
Choice A Reason: This is incorrect because decreasing the flow rate to 1 L/minute can compromise the client's oxygenation and worsen hypoxia. The client's oxygen saturation level is below the normal range of 95% to 100%.
Choice B Reason: This is correct because placing padding around the cannula tubing can prevent pressure ulcers and skin breakdown caused by friction and irritation from the tubing.
Choice C Reason: This is incorrect because applying lubricant to the cannula tubing can increase the risk of infection and inflammation of the nasal mucosa. Lubricant should be applied sparingly to the nares only if needed.
Choice D Reason: This is incorrect because discontinuing the use of the nasal cannula can endanger the client's life and cause respiratory failure. The client needs supplemental oxygen to maintain adequate oxygenation.

After reviewing the admission assessment of a client with chronic pain, which intervention(s) should the nurse include in this client's plan of care? (Select all that apply.)
Explanation
Choice A Reason: This is correct because providing comfort measures such as topical warm application and tactile massage can help reduce pain perception and promote relaxation by stimulating non-painful sensory receptors.
Choice B Reason: This is incorrect because assisting the client to ambulate as much as possible during waking hours can increase pain intensity and fatigue by aggravating inflamed or injured tissues. The nurse should encourage moderate physical activity within the client's tolerance level.
Choice C Reason: This is correct because determining client's subjective measure of pain using a numerical pain scale can help assess pain severity and effectiveness of pain management interventions. Pain is a subjective experience that varies among individuals.
Choice D Reason: This is incorrect because encouraging increased fluid intake and measuring urinary output every 8 hours are not directly related to pain management. These interventions are more relevant for clients with fluid imbalance or renal impairment.
Choice E Reason: This is correct because implementing a 24-hour schedule of routine administration of prescribed analgesic can help maintain a steady level of analgesia and prevent breakthrough pain. Chronic pain requires continuous treatment rather than on-demand administration.
Sign Up or Login to view all the 44 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

